Abstract
Background
Skull calvarium and dura mater are rare sites of distant metastasis, and mostly have been reported in lung, breast, and prostate malignancies. However, the calvarial and dural metastases from papillary thyroid cancer (PTC) are rare entities and pose diagnostic and therapeutic challenges. To date, only seven cases of calvarial metastasis with intracranial extension from PTC have been reported in literature. However, true dural metastasis from PTC has not yet been reported.
Case presentation
A 65-year-old Saudi woman presented with 6 months history of painful posterior scalp lump, 7 years after initial diagnosis of PTC. Computed tomography and magnetic resonance imaging showed occipitoparietal calvarial lesion with massive intracranial extension. Another para-sagittal lesion was found at the top of corpus callosum mimicking a meningioma. Histopathology of para-sagittal lesion and the biopsy of calvarial mass confirmed the diagnosis of metastatic PTC. After surgical resection, residual tumors were treated with postoperative intensity-modulated radiation therapy. At 13 months of follow-up, patient was alive and without any signs of recurrence.
Conclusion
Calvarial and dural metastases from PTC are extremely rare clinical entities. Surgical resection followed by postoperative radiotherapy is the treatment of choice. However, for such cases, multidisciplinary approach can prolong the treatment outcome and survival.
Introduction
Differentiated thyroid cancer, especially papillary thyroid cancer (PTC), commonly metastasizes to regional lymph nodes, lungs, and bones. However, the skull is uncommon site of metastasis, being involved only in 2.5%–5.8% of the cases.Citation1 Skull metastasis from PTC is frequently reported in the skull base, and the calvarial metastasis is a rare entity.Citation2 Calvarial metastasis from PTC usually presents as painless extracranial soft tissue mass, and in a few cases with intracranial extension, which is considered as indicator of poor prognosis.Citation3 So far, true dural metastasis from PTC is not known in the literature; however, only one case of true dural metastasis mimicking a meningioma from follicular thyroid carcinoma has been reported previously.Citation4 Symptoms of calvarial and dural metastases may vary from asymptomatic to recurrent headaches, seizures, sensory-motor dysfunction, and stroke, depending on the site of dural metastasis and extent of intracranial extension in calvarial metastasis.Citation5,Citation6
In this study, we describe a 65-year-old female with occipitoparietal calvarial metastasis with massive intracranial extension and para-sagittal dural metastasis from PTC.
Case presentation
In December 2013, a 65-year-old Saudi woman presented to us with the complaint of painful lump over the occipital region of scalp. She had noticed this lump for 6 months and it was increasing in size over 2 months; she was taking nonsteroidal anti-inflammatory drugs but with minimal improvement. Her previous medical history was not significant, and she denied any history of trauma, smoking, or weight loss. Past surgical history revealed that she had undergone total thyroidectomy and lymph node dissection for follicular variant papillary thyroid carcinoma pT2N1bM0 in June 2006. Postoperative thyroglobulin (TG) was 2.4 ng/mL. Subsequently, the patient was given radioactive iodine ablation 150 mCi in August 2006.
On physical examination, she was found to be in good general condition, and her vitals were stable. Head and neck examination revealed a hard fixed and tender mass of size 4 cm × 4 cm in the occiput without any ulceration of overlying skin, and the rest of the systemic examination was unremarkable. Clinical differential diagnosis was meningioma, sarcoma, giant cell tumor, or metastasis.
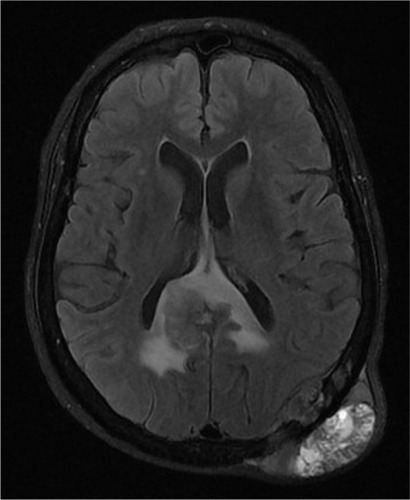
Hematology, renal and liver function tests, serum electrolytes, thyroid-stimulating hormone, and thyroxin were found to be within normal limits. Serum TG levels were markedly elevated, ie, 3,064 ng/mL (normal: 5–25 ng/mL). Whole body iodine scintigraphy was nonavid. Head and neck computed tomography (CT) showed a large left occipital bone mass of size 5.7 cm × 1.9 cm with intracranial extension and was extending superiorly to involve the parietal bone. Another intracranial dural-based lesion of size 2.6 cm × 2.3 cm was also found at the top of the splenium of corpus callosum (). Magnetic resonance imaging () and CT–positron emission tomography confirmed the findings of CT imaging. Fine needle aspiration of calvarial lesion confirmed the malignant follicular cells of PTC.
Figure 1 Head and neck computed tomography.
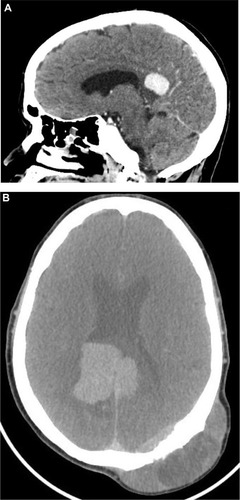
Figure 2 Magnetic resonance imaging (T2-weighted axial image) showing diffuse dural mass and another large lesion in the left occipitoparietal bone with intracranial extradural, intraosseous, and subgaleal soft tissue components.
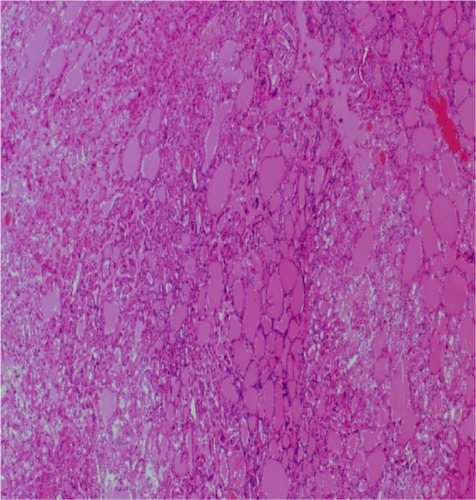
The patient was operated in January 2014; however, surgical attempt for complete resection of both lesions was foiled by perioperative profuse bleeding. Histopathology of the dural lesion revealed follicular pattern with numerous colloid-filled follicles with characteristic nuclear features of papillary carcinoma (enlarged and elongated nuclei and nuclear grooves), and immunopositivity for thyroid transcription factor-1 and cytokeratin 19 confirmed the diagnosis of metastatic follicular variant PTC (). Genetic testing revealed a BRAF V600E mutation. After successful recovery, patient was treated with intensity-modulated radiation therapy. Total dose of 5,400 cGy in 27 fractions over 6 weeks was given to both lesions. The treatment course was completed without any significant acute toxicity. Due to radioactive iodine refractory disease, the patient was started on sorafenib (Nexavar; Onyx Pharmaceuticals, Emeryville, CA, USA, and Bayer Healthcare, Wayne, NJ, USA) 400 mg orally twice daily after the completion of radiation therapy. At 8 months of follow-up period, the patient was doing well with stable skull mass and decreasing pattern of TG levels (37 ng/mL).
Discussion
Calvarium and dura as initial sites of distant metastasis from PTC is extremely rare. To date, only seven cases of calvarial metastasis with massive intracranial extension to involve dura from PTC have been published ().Citation3,Citation5,Citation7–Citation11 In our patient, calvarial metastasis with intracranial extension was seen during the sixth decade of life, and mean duration between initial diagnosis and calvarial metastasis was 72 months, which is in agreement with the previously published reports.Citation3,Citation8–Citation11 Also, similar to the reported literature, follicular variant of PTC was seen in our patient.Citation3,Citation5,Citation8,Citation10 Follicular variant PTC is known to have higher tendency to metastasize via hematogenous pathway than classic PTC.Citation12
Table 1 Previously published cases with calvarial skull metastasis with intracranial extension and dural metastasis from papillary thyroid carcinoma
Calvarial metastasis with direct dural involvement is not uncommon. In one autopsy series, dural involvement secondary to calvarial metastasis with intracranial extension was seen in 25%, and true dural metastases were observed only in 1% of cases.Citation13 To date, true dural metastasis from PTC is not known, and to the best of knowledge, our patient is the first case with true dural metastasis from PTC.
Diagnosis of calvarial and true dural metastases is challenging as these lesions are often mistaken as meningiomas. Noninvasive diagnostic techniques, including CT/magnetic resonance imaging, are essential for detecting, localizing, and assessing the extension of these lesions. However, an incorrect diagnosis is also likely to occur if it is based on the radiological findings, without a tumor biopsy.Citation8 In such cases, histopathological diagnosis along with immunohistochemistry should be made for definitive diagnosis.
The optimal management of calvarial and dural metastases is yet to be outlined. There does, however, appear to be a clear consensus that surgical resection is advantageous. However, complete surgical resection is often difficult in some cases because of risk of bleeding from these hypervascular lesions, presence of adjacent vital structures (brainstem, cochlea, cranial nerves, and corpus callosum), and risk of cerebrospinal fluid leak. Radical radiation therapy is another treatment modality that has been employed to control the calvarial and dural diseases either as an alternative to surgery for unfit patients or as an adjunct as in our patient. The effectiveness of radiation therapy is yet to be properly defined.Citation9 Our patient was treated with sorafenib, as recent trials have shown that tyrosine kinase inhibitors (TKIs) produce progression-free survival of ~1 year (range: 7.7–19.6 months), especially in patients with BRAF V600E mutations.Citation14
Conclusion
In conclusion, calvarial and dural metastases from PTC are extremely rare clinical entities. Surgical resection followed by postoperative radiotherapy is the treatment of choice. However, for such cases, multidisciplinary approach can prolong the disease-free and overall survival rates in patients with PTC.
Acknowledgments
Written consent was given from the guardian and the patient before publication.
Disclosure
The authors report no conflicts of interest in this work. No grants or funds were received for this study.
References
- MiyawakiSYamazakiRHaradaTSkull metastasis of thyroid papillary carcinomaJ Clin Neurosci200714548148417386370
- JouharFSQuadriAAfandiBAl RawiSOccult papillary thyroid carcinoma metastasis to the sacrum and the skull: an unusual presentationCase Rep Med2014201451654925544844
- Portocarrero-OrtizLGarcia-LopezRRomero-VargasSThyroid follicular carcinoma presenting as skull and dural metastasis mimicking a meningioma: a case reportJ Neurooncol200995228128419449147
- HamidHAGeeKYMuhammadRAbd RahmanZADasSDural metastasis mimicking meningioma: an interesting caseActa Medica (Hradec Kralove)2009521192219754003
- Tazi elMEssadiIErrihaniHThyroid carcinoma presenting as a dural metastasis mimicking a meningioma: a case reportN Am J Med Sci201131394222540062
- KutluhanAYalcınerGBozdemirKOzdemirETarlakBBilgenASPapillary thyroid carcinoma with metastasis to the temporooccipital skull: a case reportKulak Burun Bogaz Ihtis Derg201222316016322663926
- NigamASinghAKSinghSKSinghNSkull metastasis in papillary carcinoma of thyroid: a case reportWorld J Radiol20124628629022778883
- LiXZhaoGZhangYSkull metastasis revealing a papillary thyroid carcinomaChin J Cancer Res201325560360724255586
- HouraKVucicMCupicHKovacDCerinaVOsteolytic skull metastasis with dural involvement from a papillary thyroid carcinomaColl Antropol201135391992222053578
- SissonJCDewarajaYKWizauerEJGiordanoTJAvramAMThyroid carcinoma metastasis to skull with infringement of brain: treatment with radioiodineThyroid200919329730319207003
- LinKDLinJDHuangHSJengLBHoYSSkull metastasis with brain invasion from thyroid papillary microcarcinomaJ Formos Med Assoc19979642802829136516
- SalajeghehAPetcuEBSmithRALamAKFollicular variant of papillary thyroid carcinoma: a diagnostic challenge for clinicians and pathologistsPostgrad Med J200884988788218322127
- TaglePVillanuevaPTorrealbaGHueteIIntracranial metastasis or meningioma? An uncommon clinical diagnostic dilemmaSurg Neurol20025824124512480230
- GruberJJColevasADDifferentiated thyroid cancer: focus on emerging treatments for radioactive iodine-refractory patientsOncologist201520211312625616432