Abstract
Lichenoid reaction (LR) is clinically and histopathologically similar to lichen planus (LP), which involves the skin and mucous membrane. LR has identifiable etiology and can be triggered by systemic drug exposure or any other agents. LR occurs in all racial groups and is predominantly observed in young adults aged 20–40 years, but can occur in any age group. Typically, the clinical manifestation of LR is an itchy rash of small (±3–5 mm) shiny, raised, reddish-purple papules. The rash appears suddenly and commonly affects the anterior surface of the arm and hand and the back part of the body. We report a rare case of LR to antihistamines (cetirizine, loratadine) and corticosteroid (methylprednisolone): an adult female 32-year-old patient, with a chief complaint of burning sensation, a few small rashes and itching on the anterior surface of the arm after eating seafood and eggs 7 days prior to admission. From the detailed and chronologic anamnesis of her dietary habits, routine use of drugs and oral hygiene, and from the histopathological results, we concluded the patient has lichenoid reaction caused by drugs (antihistamines and corticosteroids).
Introduction
Lichenoid reaction (LR) is an adverse effect which may be caused by systemic administration of drugs including antihistamine, corticosteroid and some other triggers.Citation1,Citation2 The prevalence of LR has been reported to be approximately 2.4% in the general population and occurs in women three times more than in men.Citation3 Despite the tolerability and safety of H1 antihistamines in humans having been widely established, hypersensitivity reactions have been reported since the 1940s.Citation4–Citation6 But LR induced by antihistamines and corticosteroids is rarely reported.Citation7,Citation8 Here, we report a rare case of LR in a 32-year-old adult female, caused by antihistamines (cetirizine, loratadine) and corticosteroid (methylprednisolone) that were given to the patient for food allergy (seafood, eggs) treatment.
To participate in this study, the patient specifically provided written informed consent for the publication of the case details and any accompanying images. The study procedure was approved by the Ethical Committee of Wangaya Hospital in Denpasar, Bali, Indonesia with register number 08/RSUDW/Litbang/2020 and has permission to publish this study. The study was conducted in accordance with the Declaration of Helsinki.
Case Presentation
A 32-year-old adult female patient reported with a chief complaint of burning sensation, a few small rashes and itching on the anterior surface of the arm after eating seafood and eggs 7 days prior to admission ().
Past medical history; generally the patient felt fit with a previous history of food allergy caused by seafood and eggs. No family history of experienced allergic diseases. On physical (skin) examination were observed on the anterior surface of the arm a few red papules and itching, with no local change in temperature.
Progress Note
The patient consulted the general medical practitioner and was treated with antihistamine (10 mg cetirizine once a day, orally) and corticosteroid (4 mg methylprednisolone twice a day, orally) for food allergy treatment. Whenever she was exposed to antihistamine (10 mg cetirizine) and corticosteroid (4 mg methylprednisolone), she felt her skin lesions and itching abruptly increased, which were predominantly on the anterior surface of the left arm and hand (unilateral) ().
Figure 2 Rash and itching on the anterior surface of the left arm and hand, which the patient felt worsen.

This made the patient come back to the private clinic. She received another antihistamine (10 mg loratadine once a day, orally) to increase the therapeutic effect of antihistamines, but the skin lesions and itching were worse and full blown immediately. The papules began over the anterior surface of the left arm and hand asymmetrically, and spread upwards on the back part of the body, and she also felt chest discomfort. She was referred to Wangaya Hospital in Denpasar, Bali, Indonesia when the skin lesions were worse and she got chest discomfort. On physical examination, she was fully alert, her axillary temperature was 37.2 °C, blood pressure 110/70 mmHg, and pulse rate 88 times/minute regularly. Multiple papules appeared all over the body, predominantly on the anterior surface of the left arm and hand (asymmetric/unilateral), and the back part of the body was itchy ().
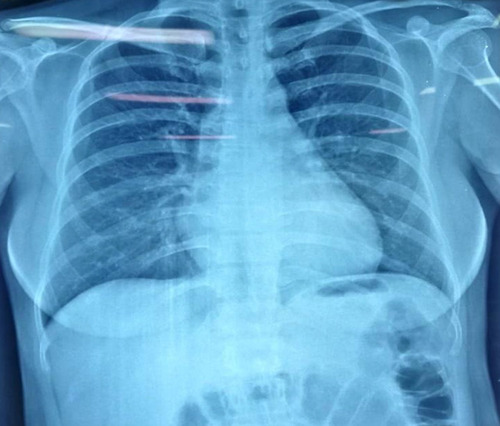
The laboratory data on admission were as follows: white blood count (WBC)=10.39×103/μL; with differential count: neutrophiles, 69.3%; lymphocytes, 23.8%; eosinophils, 6.9% (increasing the eosinophil plasma level), without any other abnormalities found in the blood chemistry panel. She felt chest discomfort, but the chest radiograph showed no cardiac, pleural or pulmonary abnormalities ().
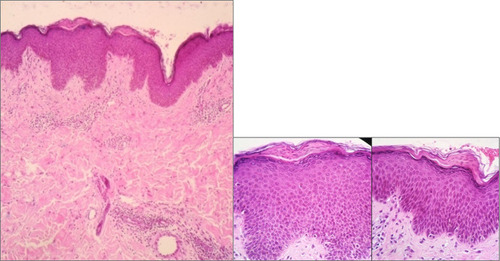
A skin biopsy was taken from the area with severe skin lesions on the anterior surface of the left arm. The histopathological examination showed findings consistent with a lichenoid drug reaction. The epidermis with focal parakeratosis and the epidermis with superficial and deeper extension are full of inflammatory infiltrates, numerous lymphocytes and a few eosinophils. The epidermis had focal parakeratosis ().
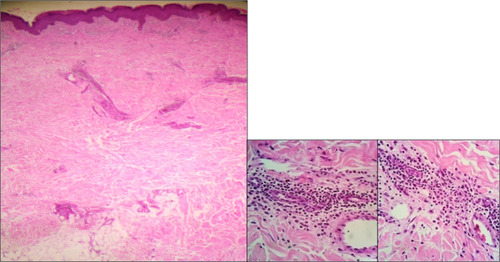
Detailed histopathological examination revealed the epidermis with superficial and deeper extension of inflammatory infiltrates, numerous lymphocytes and a few eosinophils ().
Figure 6 The epidermis with superficial and deeper extension full of inflammatory infiltrates, numerous lymphocytes and a few eosinophils.
Based on the clinical history and histopathological review, the final diagnosis was lichenoid reaction in a 32-year-old adult female, caused by antihistamines (cetirizine, loratadine) and corticosteroid (methylprednisolone).
The therapeutic approach is discontinuing the previous drugs (cetirizine, loratadine, methylprednisolone). At a screening, she was tested with other antihistamines by rapid desensitization protocol. The Chlor Tri Method (CTM) was tolerable. Other medicine given was shown to be not tolerable, such as azithromycin and gentamycin. Finally, the patient was treated by antihistamine (4 mg CTM) 3 times a day, orally. In a week follow-up, the patient had better condition day by day gradually.
Discussion and the Literature Review
Lichenoid reaction (LR) may associate with systemic drug exposure involving the skin, oral mucosa or both.Citation9–Citation11 Despite this, the tolerability and safety of H1 antihistamines in humans have been widely established. The case of hypersensitive reactions has been reported since the 1940s.Citation12
The patient came to consult the general medical practitioner with a complaint of the presence of small papules and itching on the anterior surface of the arm after eating seafood and eggs. The clinical finding suggested that her complaint was caused by food allergy. She was treated with antihistamine (10 mg cetirizine once a day, orally) and corticosteroid (4 mg methylprednisolone twice a day, orally).
Systemic adverse effects of antihistamines are caused by inhibition of peripheral and central cholinergic and serotoninergic receptors by antihistamines, inducing dizziness, drowsiness, nausea, restlessness, dry mouth, problems with memory, tinnitus, sometimes difficulty of urination and defecation.Citation13,Citation14
Also, adverse effects caused by short-term low-dose corticosteroids such as of the gastrointestinal system (gastric irritation) and endocrine-metabolic system (hyperglycemia) are frequent.Citation15–Citation17
But LR reported in association with many systemic medications (antihistamines and corticosteroids) are very rare. This patient, whenever she was exposed to the drugs (cetirizine and methylprednisolone) during food allergy treatment, felt the skin lesions and itching abruptly were worse. This made the patient come back to the private clinic. Then, she was treated with another antihistamine (10 mg loratadine once a day, orally) to increase the therapeutic effect of antihistamines, but the skin lesions and itching were worse and full blown immediately. The papules began over the anterior surface of the left arm and hand asymmetrically, and spread upwards on the back part of the body, and she also felt chest discomfort. Based on the clinical findings, the clinical adjustment was suspicion of lichenoid reaction caused by antihistamines (10 mg cetirizine, 10 mg loratadine) and corticosteroid (4 mg methylprednisolone). She was referred to Wangaya Hospital in Denpasar, Bali, Indonesia.
Lichenoid reactions reported in association with many systemic medications are now known such as ACE inhibitors, interferon alfa, antihistamines, lithium, antimalarials, methyldopa, beta-blockers, NSAIDs, carbamazepine, penicillamine, furosemide, penothiazines, gold, phenytoin, hydroxycarbamide, proton pump inhibitors, corticosteroids and sulphonylureas.Citation3,Citation18
In this case, the suspicious systemic drug administration triggers were antihistamines (cetirizine 10 mg and loratadine 10 mg) and corticosteroid (methylprednisolone 4 mg).
Theoretically, the histopathologic feature of lichenoid reaction is that subepithelial infiltrate is more diffuse and less band like, with deeper extension into the connective tissue and a more mixed cell population, including eosinophils and plasma cells, perivascular infiltrate and parakeratosis.Citation7,Citation19–Citation21
Lichenoid reaction and lichen planus on the microscope characteristics are no different, so detailed anamnesis is more important.Citation22
In this case, from detailed and chronologic anamnesis of her dietary habits, routine use of drugs and oral hygiene, and from the histopathological results – epidermis with focal parakeratosis and the epidermis with superficial and deeper extension of inflammatory infiltrates, and numerous lymphocytes with a few eosinophils – we concluded the patient had a lichenoid reaction caused by drugs (antihistamines and corticosteroids).
The comparison between the literature review and case are: Citation20
1. Clinically
a. Literature review, the lichenoid reaction is unilateral lesion / asymmetric; in this case we found rash and itchy predominance raised on anterior surface of left arm, hand (asymetric)
b. In less well-established sites like gingiva, lips, palate; in this case we found Rash and itchy on back part of the body
c. Association with the triggers; in this case we found the suspicient triggers: antihistamines and corticosteroids
2. The histopathological features
Literature reviews are focal parakeratosis, lymphocytes infiltration, eosinophils; in this case we found the epidermis with focal parakeratosis, superficial and deeper extension of inflammatory infiltrates, numerous lymphocytes with few eosinophils.
The principle therapy of LR first requires identification or recognition of the triggering factor, and it is necessary to avoid these triggering factors. The symptoms typically reduce after elimination of the suspected drug or other triggers and one should suppress symptoms as optimally as possible until there is spontaneous remission.Citation23–Citation25
Before starting the treatment with the new regimen, we performed a drug provocation test. She was tested with other antihistamines by rapid desensitization protocol, and the Chlor Tri Method (CTM) was tolerable. Another medicine given was not tolerable or showed a hypersensitivity reaction, such as azithromycin or gentamycin. Finally, the patient was treated by antihistamine (4 mg CTM) 3 times a day, orally. The patient was observed and the condition was better day by day gradually.
Conclusions
The adverse drug reactions of antihistamines and corticosteroid are common but lichenoid reaction is very rare. There are many challenges that should be solved step by step and simultaneously with observation. The problems can occur due to the diagnostic approach and/or management cases. It is important for the practitioner to use antihistamines and corticosteroids in case of cutaneous reactions before obtaining a certain diagnosis to avoid improper use of drugs.
Acknowledgment
The author appreciates all of the doctors who are in duty at the Emergency Unit, the Intensive Care Unit Crew and other colleagues; I. B. Wiyasa, Surgeon, Novitasari Pathologist at Wangaya Hospital in Denpasar, Bali, Indonesia.
Disclosure
The author reports no conflicts of interest in this work.
References
- Giudice A, Liborio F, Averta F, Barone S, Fortunato L. Oral lichenoid reaction: an uncommon side effect of rituximab. Case Rep Dent. 2019;1–3.
- Pangsomboon K, Kintarak S. Oral lichenoid reaction to herbal medicine: a case report. Songklanakar in Dent J. 2017;5:44–56.
- Hosseini FA, Samami M, Tavakol F, Hoseini EG. Oral lichen planus or oral lichenoid reaction? A literature review. J Islam Dent Assoc. 2019;31:40–57.
- Kataria G, Saxena A, Sharma S. Levocetirizine induced fixed drug erupion: a rare case report study. Int J Sci. 2014;4:228–229.
- Lee J, Kim YU, Kim SH. Drug hypersensitivity to various antihistamines with cross-reactions: a case report. Clin Trad Allergy. 2014;4(S3):P132. doi:10.1186/2045-7022-4-S3-P132
- Kim MH, Lee SM, Lee SH, et al. A case of chlorpheniramine maleate-induced hypersensitivity with aspirin intolerance. Allergy Asthma Immunol Res. 2011;3(1):62–64. doi:10.4168/aair.2011.3.1.6221217928
- Stipetic MM, Brzak BL, Hodak IB, et al. Clinicopathologic correlation of oral lichen planus and oral lichenoid lesions: a preliminary study. Sci World J. 2014;2014:1–6. doi:10.1155/2014/746874
- Torres RF, Almagro M, Pozo JD, et al. Lichenoid drug eruption induced by olanzapine. Actas Dermosifiliogr. 2008;99(3):221–224.18358199
- Katsoulas N, Tosios K, Andrikopulou AS. Lichenoid lesions of the upper lip: a retrospective study of 24 cases. Med Oral Patol Oral Cir Bucal. 2018;23(3):e302–7. doi:10.4317/medoral.2230329680851
- Akbas A, Kilinc F. Analysis of the patients with lichenoid drug reactions: a retrospective study. Med Sci Discovery. 2018;5:153–160. doi:10.17546/msd.407370
- Ismail SB, Kumar SKS, Zain RB. Oral lichen planus and lichenoid reactions: etiopathogenesis, diagnosis, management and malignant transformation. J Oral Sci. 2007;49:89–106. doi:10.2334/josnusd.49.8917634721
- Choi YW, Jung MJ, Kim HO, Chung BY, Park CW. Anaphylaxis to chlorpheniramine maleate and literature review. Ann Dermatol. 2019;31(4):438–441. doi:10.5021/ad.2019.31.4.438
- Shahid M, Tripathi T, Sobia F, Moin S, Siddiqui M, Khan RA. Histamine, histamine receptors, and their role in immunomodulation: an updated systematic review. Open Immunol J. 2009;2(1):9–41. doi:10.2174/1874226200902010009
- Rio PRD, Gutierrez G, Lopez JS, Acevedo BN, Alvarez JMB, Cocera CM. Urticaria caused by antihistamines: report of 5 cases. J Investig Allergol Clin Immunol. 2009;19(4):317–320.
- Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoid-induced side effects: a comprehensive review. J Am Acad Dermatol. 2017;76(1):1–9. doi:10.1016/j.jaad.2016.01.06227986132
- Oray M, Samra KA, Ebrahimiadib N, Meese H, Foster S. Long-term side effects of glucocorticoids. Expert Opin Drug Saf. 2016;15(4):457–465. doi:10.1517/14740338.2016.114074326789102
- Thondprasom K, Dhanuthai K. Steroids in the treatment of lichen planus: a review. J Oral Sci. 2008;50:377–385. doi:10.2334/josnusd.50.37719106464
- Lee A, Thomson J. Drug-induced skin reaction In: Lee A, editor. Adverse Drug Reactions. 2nd ed. London: Pharmaceutical Press; 2005:125–156.
- Sareen C, Pathak A, Ahuja P, Kohli M. A diagnostic dilemma: oral lichen planus or lichenoid reaction – a series of case reports. J Adv Med Dent Scie Res. 2015;3:98–102.
- Kamath VV, Setlur K, Yerlagudda K. Oral lichenoid lesions – a review and update. Indian J Dermatol. 2015;60(1):102. doi:10.4103/0019-5154.147830
- Gupta M, Gupta H, Gupta A. Tenofovir induced lichenoid drug eruption. Avicenna J Med. 2015;5(3):95–97. doi:10.4103/2231-0770.16025026229762
- Do Prado RF, Marocchio LS, Felipini RC. Oral lichen planus versus oral lichenoid reaction: difficulties in the diagnosis. Indian J Dent Res. 2009;20(3):361–364. doi:10.4103/0970-9290.5737519884724
- Sanchez PS, Bagan JV, Soriano J, Sarrion G. Drug-induced oral lichenoid reactions. a literature review. J Clin Exp Dent. 2010;2:e71–5. doi:10.4317/jced.2.e71
- Kadam NS, Patil RA, Gurav AN, et al. Duloxetine hydrochloride-induced oral lichenoid reaction: a case report. Med Prin Pract. 2015;24:394–397.
- Barbosa MO, Da Silva AF, De Carvalho Tarquinho SBC, Demarco FF. Oral lichenoid lesions associated with amalgam restorations: report of two cases1. Rev Odanto Cienc. 2011;26:258–261. doi:10.1590/S1980-65232011000300012