Abstract
Little is known about the features of asthma and allergy in the elderly. A significant number of elderly patients with asthma have uncontrolled and severe asthma. This review aims to provide an analysis of the literature on the assessment and phenotype of severe allergic asthma in the elderly. Gaps and pitfalls in diagnostic and therapeutic approaches, as well as management of severe allergic asthma in the elderly, are also discussed.
Introduction
Asthma is a common chronic disease that affects ≈300 million people worldwide.Citation1 Prevalence of asthma among countries varies from 1% to 28% and affects people of all races and age groups.Citation1 Adult-onset or late-onset asthma is considered if asthma symptoms appear in adulthood.Citation2 Age at diagnosis can vary from 12 years to ≥65 years.Citation3,Citation4 Recent epidemiologic studies have shown that asthma is prevalent in the elderly (4.5%–12.7%).Citation5 One study demonstrated the rate of newly diagnosed asthma in patients aged ≥65 years to be 0.1% per year.Citation6 The number of people aged ≥60 years is growing rapidly in developed countries. By 2030, it is estimated that this group will be ≈20% of the total population.Citation7 This expected increase in the prevalence of asthma in the elderly has led to increased interest in the phenotyping of asthma in this population based on severity, age at diagnosis, spectrum of symptoms, treatment response, triggering factors, and level and type of inflammation.
Some data suggest that asthma in older adults is phenotypically different from that in younger patients.Citation1,Citation8 That is, a significant number of older people with asthma have uncontrolled and severe asthma, which leads to increased morbidity and mortality.Citation1 Several factors in older patients with asthma contribute to the risk of uncontrolled disease: a low level of education; poor memory and coordination; and hearing, visual, and neuromuscular difficulties in learning inhaler-use methods and asthma self-management plans.Citation8 Older patients with asthma also have an increased likelihood of comorbidities and polypharmacy, which can lead to worsening of asthma.Citation8
Asthma management in the elderly follows the same steps as that for younger adults.Citation1 Nevertheless, asthma in the elderly is being underdiagnosed and undertreated.Citation1 Usually, the term older adults is applied to persons aged ≥65 years, but the definition of older persons in the asthma literature is not homogeneous. Many reports on asthma in the elderly are findings from general surveys in adults and have not focused primarily on asthma characteristics in the elderly. Hence, more studies are needed to ascertain the prevalence and features of asthma and allergy in the elderly.
This review aims to provide analyses of the literature on the assessment and phenotype of severe allergic asthma in the elderly. Gaps and pitfalls in diagnostic and therapeutic approaches, as well as management of severe allergic asthma in the elderly, are also discussed.
Phenotype of allergic asthma in the elderly
Asthma in the elderly is a mixture of childhood-onset and adult-onset disease.Citation9 Asthma may persist from childhood or start in adult life. Hence, elderly patients with asthma can be grouped as patients with long-standing asthma or patients with late-onset disease.Citation9 Atopy is more frequent in early-onset asthma than in late-onset asthma.Citation9 Atopy increases the risk of asthma in children and younger adultsCitation9 and may also increase the risk of asthma in the elderly. Recent studies have suggested that allergic sensitization in patients with asthma aged ≥55 years might be more common than reported.Citation10 Busse et alCitation11 found that sensitization to indoor allergens was strongly associated with asthma in elderly patients. Sensitization to house dust mites, mold, and cockroaches can increase the prevalence of asthma in the elderly.Citation12,Citation13 Studies also suggest that sensitization and exposure to pollen allergens result in persistent and severe asthma in adults.Citation14 Parietaria is more important than Olea and Gramineae as a risk factor for the development of nonspecific bronchial hyperresponsiveness.Citation14 Celikel et alCitation15 analyzed the records of 922 patients diagnosed with seasonal allergic rhinitis retrospectively to determine the risk factors for asthma in adults. They divided patients with seasonal allergic rhinitis into four groups: 1) no sensitization, 2) monopollen sensitization, 3) polypollen sensitization, and 4) mite sensitization. Compared with the polypollen sensitization group, groups with no sensitization and mite sensitization had a higher risk of asthma, whereas the monopollen sensitization group was unlikely to have any other allergic disease (including asthma).Citation15 Data support an association between pollen sensitization and adult-onset asthma, but sensitization to pollen is not significantly associated with asthma symptoms in the elderly.Citation12,Citation13 Recently, we showed that the prevalence of atopy was 21% in an elderly population with asthma; these patients were most commonly sensitized to Dermatophagoides pteronyssinus (44.4%), followed by Blattella germanica (27.7%), Aspergillus fumigatus (27.7%), Dermatophagoides farinae (22.2%), and a grass mix (11.1%).Citation16 Our results were similar to those of Busse et al,Citation11 who found that sensitization to house dust mites, mold, and cockroaches was an important factor in elderly patients with asthma. Of these patients, 44% had mild, 41% had moderate, and 5% had severe persistent asthma. In all, 93.9% of patients had late-onset disease (age >18 years).Citation16 Atopy seems to be closely linked with late-onset asthma as well as long-standing asthma. Wolfe et alCitation17 found that an atopic condition (defined as rhinitis, eczema, or positive skin reactions to rye grass or house dust mite in childhood) increased the risk of more severe asthma in adult life.
Presentation of allergic asthma in the elderly is not different to that in younger patients. Ozyigit Pur et alCitation18 found that older individuals with allergic asthma had similar clinical and laboratory characteristics to those of a younger age group. In that report, asthma severity was not different between older and younger patients with allergic asthma. However, older patients with asthma had worse control of asthma and lower values for forced expiratory volume in 1 second (FEV1) and forced vital capacity when compared with younger patients with allergic asthma.Citation18 A study by Inoue et alCitation19 elicited similar results to those by Ozyigit Pur et al,Citation18 with no significant differences in blood or sputum cells, exhaled nitric oxide, or airway responsiveness to methacholine between older and younger patients with asthma. However, based on analyses of spirometry, computed tomography, and impulse oscillation, elderly patients with asthma had greater involvement of small and large airways than nonelderly patients with asthma.Citation19
Clinical characteristics of severe asthma in the elderly have been reported to be complex and considerably distinct. In particular, late-onset asthma appears to be more severe and less atopic in nature.Citation20 In the Cardiovascular Health Study,Citation21 respiratory symptoms in patients with late-onset asthma (cough, phlegm, wheezing, and dyspnea) were more prevalent compared with patients whose asthma began before the age of 20 years. Elderly individuals with asthma reported that the most common trigger was a viral infection or animal allergies.
Patients with long-standing asthma have worse and more frequent respiratory symptoms, an increased number of hospitalizations and emergency medical interventions, and lower parameters of lung function.Citation22 Park et alCitation23 established a prospective, observational cohort of elderly Korean patients with asthma to identify elderly patients with asthma with distinct clinical phenotypes. Four clusters of elderly patients with asthma were identified: 1) long duration of symptoms and marked obstruction of airways, 2) female dominance and normal lung function, 3) male dominance for smoking and reduced lung function, and 4) high body mass index and borderline lung function. Prevalence of atopy among the four clusters was 15.6%–26.4%. Cluster 3 (male dominance for smoking and reduced lung function) had a significantly higher prevalence of atopy. Cluster 1 had a significantly longer duration of symptoms, severe obstruction of airways, and a higher number of exacerbations. Park et alCitation23 found long duration of symptoms and smoking to be related to reduced lung function in elderly patients with asthma even after bronchodilator inhalation.
Management challenges
Many patients with adult-onset asthma have a poor prognosis, with a faster decline in lung function and more severe, persistent limitation of airflow.Citation2 Compared to younger adults, a significant number of older individuals with asthma have poorly controlled asthma, which can lead to increased numbers of prescriptions of asthma medications, hospitalizations, and deaths.Citation4 If asthma develops at an advanced age, symptoms are much like those among younger adults. However, greater amounts of medication are needed to maintain asthma control in elderly populations because they may be more likely to have respiratory failure with other diseases, such as chronic obstructive pulmonary disease (COPD) and congestive heart failure. Tsai et alCitation24 published the results of analyses of a large, USA-wide database for emergency-department visits. They found that of those who visited the emergency department for asthma problems, those aged ≥55 years had a higher prevalence of hospitalization and near-fatal asthma events, longer duration of hospital stay, and higher overall mortality than adults aged 18–54.9 years. Talreja and BaptistCitation25 compared younger patients with asthma with older patients with asthma and found that the latter were more likely to be obese, to be smokers, and to have worse control of asthma. As stated earlier, several factors in older patients with asthma contribute to the risk of uncontrolled disease: a low level of education; poor memory and coordination; and hearing, visual, and neuromuscular difficulties in learning inhaler-use methods and asthma self-management plans. Older patients with asthma also receive several types of medications for different health problems that can react with asthma treatments.Citation7
Asthma management in the elderly is beset with problems. The goal of asthma therapy is to reduce the frequency and severity of symptoms and exacerbations, maintain normal levels of activity, and achieve optimal lung function. Management of severe allergic asthma in the elderly follows the same steps as that in younger adults to achieve these goals.Citation1 The European Respiratory Society and American Thoracic Society Task Force on severe asthmaCitation26 has defined the following three main steps in the management of severe allergic asthma in the elderly.
Step 1: definition
Confirmation of the diagnosis
Classic symptoms of asthma in the elderly are similar to those of younger individuals with asthma.Citation27 Most patients complain of episodic wheezing, dyspnea, and a feeling of chest tightness. These symptoms are often worse at night and upon exertion in younger patients with asthma.Citation27 Asthma symptoms can be triggered by infections of the respiratory tract, aeroallergens, irritants, and the medications commonly used by this patient population (aspirin, nonsteroidal anti-inflammatory agents, angiotensin-converting enzyme inhibitors, and beta-blockers).Citation27 The diagnosis of asthma may be more difficult in the elderly because of the high prevalence of other disorders that can have similar symptoms (congestive heart failure, emphysema, COPD, chronic aspiration, gastroesophageal reflux disease (GERD), and tracheobronchial tumors).Citation27,Citation28 Comorbidities and the psychosocial effects of aging may also affect the diagnosis profoundly. Differentiation of chronic asthma from COPD can be very challenging, and in some patients, asthma cannot be distinguished from COPD with the available diagnostic tests. COPD management may have similarities with that of asthma.Citation27 In elderly patients (as for younger adults), careful history-taking is necessary to identify symptoms and triggers. Physical examination should include examination of upper airway and chest auscultation, and alternative causes of respiratory symptoms should be considered and investigated fully, including use of pre- and postbronchodilator spirometry.Citation1 Further diagnostic tests are needed to exclude other conditions or comorbidities (eg, parenchymal lung disease, COPD, GERD, sleep apnea, and congestive heart failure).Citation1
Differentiation between severe asthma and mild asthma
Severe asthma can be defined as asthma that requires treatment with high-dose inhaled corticosteroids and a second controller (and/or systemic corticosteroids) to prevent it from becoming uncontrolled, or which remains uncontrolled despite such therapy.Citation26 Severe asthma involves almost-continuous symptoms, frequent exacerbations, frequent night-time awakenings, limited activities, peak expiratory flow or FEV1 baseline <60% predicted, and peak expiratory flow variation of 20%–30%. Therefore, this definition includes patients at steps 4 and 5 of guidelines set by the Global Initiative for Asthma (GINA).Citation1 Severe asthma in the elderly can be accompanied by the presence or absence of a significant irreversible component of obstruction.Citation29 There is considerable variation in the duration and severity of asthma, and many of these patients have severe, irreversible obstruction unrelated to asthma duration.Citation29 The degree of irreversible obstruction is unrelated to pack-years of cigarette smoking, suggesting that there are additional causes. Coexisting COPD and bronchiectasis with segmental pulmonary fibrosis can also cause irreversible obstruction in cases with severe asthma.Citation29
Determination of whether severe asthma is controlled or uncontrolled
Any one of the following four criteria can be used to define uncontrolled asthma: poor control of symptoms (ie, asthma control questionnaire >1.5 consistently or asthma control test <20); frequent severe exacerbations (defined as ≥2 bursts of systemic corticosteroids [>3 days each] in the previous year); serious exacerbations (defined as at least one hospitalization stay in the intensive care unit, or mechanical ventilation in the previous year); and airflow limitation (ie, FEV1 <80% predicted after withholding of short- and long-acting bronchodilators).Citation26 A significant number of older people with asthma have uncontrolled and severe asthma, which can lead to increased morbidity and mortality.Citation1 Compared to young adults with asthma, elderly adults with asthma have worse short-term (symptoms within the previous week, day-and-night symptoms during the previous 30 days, and corticosteroid use in the previous 3 months) and long-term (asthma attack, emergency-department visit, hospitalization, and activity limitations in previous year) control.Citation24 Recently, we showed that 52% of elderly patients had uncontrolled asthma.Citation16 In a recent multicenter observational study, 39% of elderly patients with asthma had uncontrolled asthma despite receiving high-level GINA-based therapy (steps 3–4).Citation30
Step 2: patient evaluation
Assessment of contributory factors
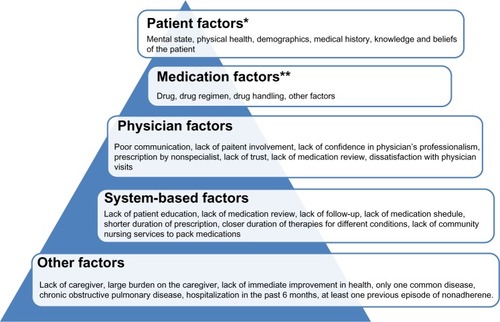
If the diagnosis of asthma has been confirmed, coexisting conditions must be determined and addressed. Adherence to asthma medications (as well as poor methods of inhalation of medications) presents problems in all age groups.Citation1 However, it has been suggested that older people are less likely to adhere to medications and to use their inhaler devices appropriately when compared to younger adults.Citation16,Citation18,Citation31 Detection of poor adherence can be challenging. Yap et alCitation32 reviewed the barriers affecting medication adherence in older adults. They categorized the barriers into five main factors: patient, medication, physician, system-based, and other (). The attending physician should focus and address all factors affecting medication adherence in older adults. Improper use of inhaler devices in older people is very common. Recently, we showed that 52% of patients had uncontrolled asthma and, of these elderly patients with asthma, only 48.7% used their inhaler devices properly.Citation16 Arthritis of the hands, tremors, low inspiratory flow rates, and problems in hearing, seeing, and neuromuscular coordination can result in difficulties with inhaler manipulation.Citation31 Atopy and allergy, rhinosinusitis, nasal polyps, GERD, obesity, concurrent smoking, anxiety, and depression are important coexisting conditions that may contribute to asthma severity.Citation25 In adults, chronic disease in the upper airways (particularly sinusitis) is very often associated with poor outcomes. In the Severe Asthma Research Program study,Citation33 54% of patients with severe asthma had a history of sinusitis. Cluster analyses in the Severe Asthma Research Program study showed that sinus disease was significantly more frequent in patients with a severe asthma phenotype in the oldest patients.Citation34
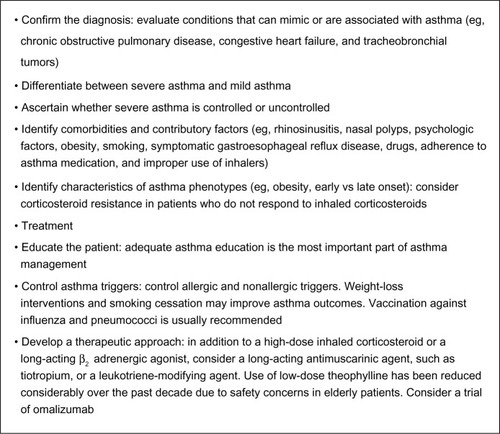
Figure 1 Factors effecting medication adherence.
Interactions among the effects of aging, asthma, and coexisting disease
Elderly patients with asthma frequently have coexisting diseases.Citation5 Coexisting disease and disease-related treatments should be considered in the diagnosis and management of asthma. Elderly individuals with asthma have an increased prevalence of respiratory diseases, such as chronic bronchitis, COPD, chronic sinusitis as well as stomach ulcers, cardiovascular disease, osteoporosis, diabetes mellitus, depression, and cancer when compared to younger patients with asthma.Citation35 Individuals with severe asthma have a higher prevalence of sinusitis, GERD, hypersensitivity to non-steroidal anti-inflammatory drugs, pneumonia, obstructive sleep apnea syndrome, recurrent respiratory infections, and neuropsychological problems when compared to patients with nonsevere asthma.Citation26,Citation35 A recent study reported that elderly patients with asthma had a significantly higher mean number of chronic comorbidities (8.4) than those in younger patients (3.4).Citation35 In the elderly, differentiating age-related normal physiological and neuropsychological changes from asthma-related abnormal changes can be very difficult. Normal aging-associated changes in lung structure probably worsen asthma symptoms.Citation36 Such changes sometimes make it difficult to distinguish clearly between asthma and COPD, especially in patients who have smoked tobacco. Initially, asthma symptoms may be masked by or misdiagnosed as other disorders, such as congestive heart failure.Citation36 In particular, elderly patients are exposed to the negative effects of polypharmacy, and some treatments taken for coexisting diseases may worsen asthma control by inducing bronchospasm.Citation36 It is important to ask which other medications elderly asthma patients are using. Clinicians need to be aware of the potential for interactions among the effects of aging, asthma, coexisting diseases, and various medications in elderly patients. Patient education and asthma management plans for elderly patients should take into account all the following possible conditions: loss of coordination and muscle strength, hearing and visual difficulties, sleep disturbances, impaired cognitive function, neuropsychological diseases, and depression.
Special groups
Asthma in patients with neuropsychological diseases
Memory changes are common in the elderly. A loss of neurons in certain areas of the brain can increase reaction times and reduce the ability to respond to multiple complex stimuli in the elderly.Citation36 In addition, pathologic conditions, such as stroke, dementia, anemia, electrolyte imbalance, thyroid dysfunction, and poor cardiac function, are more frequent in the elderly.Citation36 All these contributory factors can lead to confusion and affect the ability to learn and use new information.Citation36 The most common psychoneurological problems are depression and dementia in elderly asthmatic patients.Citation36 Studies have suggested an association between asthma and dementia, but the results are inconsistent.Citation37 Untreated asthma could be also associated with declining cognitive function. A recent study by Bozek and JarzabCitation38 reported that, after 1 year of antiasthmatic treatment, some cognitive and instrumental activities increased significantly in asthma patients with Alzheimer’s disease. However, ≈10% of elderly patients are mentally debilitated,Citation36 and getting asthma symptoms under control in such patients is very difficult. Clinicians often face challenges in maintaining asthma control in elderly patients with mental problems. Many of these patients with dementia do not present with typical symptoms (eg, breathlessness and cough). Mental status and neuropsychiatric disorders can cause aspiration, which can exacerbate asthma symptoms.Citation36 These patients are often hypoxic, and most of them cannot take medication of any type by themselves. Family members, friends, or special nurse care for an impaired elderly person may be needed. Education and support programs for caregivers of patients with dementia could be effective in reducing treatment problems and improving the management of asthma and dementia. Nebulizers can also replace inhalers in such patients.
Prevalence of concomitant depression in elderly patients with asthma is 17%. Depression can also be caused by commonly used medications in the elderly, such as corticosteroids, antihypertensive agents, and anti-Parkinsonian drugs.Citation34 The association among depression, psychiatric disorders, and asthma is stronger in females than in males.Citation39 There is a close relationship with asthma, mortality, and depression.Citation36 Depression may also reduce compliance with treatment plans and patient motivation to engage in normal activities.Citation36 Hence, depression should be treated for the maintenance of asthma control in these patients. Several studies have reported on various aspects of the coexistence of asthma, multiple sclerosis, and Parkinson’s disease, but the results are contradictory.Citation40,Citation41
Asthma–COPD overlap syndrome (ACOS)
ACOS is the definition for a condition in which a person has the clinical features of asthma and COPD.Citation1,Citation42 ACOS is common among elderly asthmatic people with a history of smoking or long-term asthma.Citation43,Citation44 Women are more likely to have ACOS than men.Citation43 ACOS has been estimated to be present in 15%–45% of patients with obstructive airway disease, and the prevalence increases with age.Citation44 Patients with ACOS have a high prevalence of mortality, frequent exacerbations, more severe attacks, and decreased pulmonary function when compared to those with asthma alone or COPD alone.Citation45 They have also more comorbidities, such as diabetes mellitus and malignant disease.Citation45,Citation46 The most frequent cause of death in these patients is malignant disease.Citation46 Distinguishing between asthma with a component of fixed airflow obstruction and COPD is important, especially in current and exsmokers. However, sometimes distinguishing clearly between asthma and COPD can be difficult. Reversibility of airway obstruction in elderly asthmatics is often reduced because of irreversible structural changes, and conversely, in patients with COPD, a significant response to bronchodilators can be observed.Citation36,Citation42 In addition to pulmonary function tests, assessment of inflammatory markers by induced sputum and the degree of airway remodeling by imaging methods might be useful to characterize patients with ACOS by phenotype. Other comorbidities such as malignant disease should also be evaluated in these patients. Little is known about the characteristics of these patients and how best to treat them. Different treatment options are recommended, such as symptom-based approaches and ACOS phenotyping-based approaches, for patients with ACOS.Citation1,Citation44,Citation47
Approaches to asthma phenotyping
Widely accepted definitions of the phenotypes of severe allergic asthma in an elderly population are lacking. Late-onset asthma, early-onset asthma, corticosteroid insensitivity, and obesity characteristics can be helpful when considering specific therapies.
Step 3: treatment
Nonpharmacologic interventions
Asthma education
Considerable evidence suggests that patient education is very important for successful control of asthma.Citation1 Adequate asthma education is particularly important in the elderly owing to the often complex treatments involved, comorbidities, and sometimes reduced memory and cognitive functions.Citation4 Inappropriate methods for using inhaler devices are another problem in elderly patients with respect to uncontrolled disease.Citation4 Recently, we found that older patients with asthma had limited knowledge of self-management and worse control of asthma and showed improper use of inhaler devices. Educational levels in these elderly patients were low; they did not use the Internet for asthma education, and the only source of asthma knowledge for such patients was physician-managed asthma care.Citation16 Our study showed that standard asthma care is largely insufficient for older patients and that asthma education programs should be developed for older adults based on education level and asthma characteristics. Effective education programs for elderly patients with asthma would lower the prevalence of uncontrolled asthma in this population.Citation16
Controlling triggers
Controlling triggers is the main step in the management of allergic asthma, but elderly asthmatics have little knowledge about asthma triggers. Wolfenden et alCitation48 investigated factors associated with hospitalization and revealed that 40% of older people with asthma reported that they did not know everything they needed to know to manage flare ups, adjust their medications, or avoid asthma triggers. Weight-loss interventions and smoking cessation can also improve asthma outcomes.Citation1 Vaccination against influenza and pneumococci is usually recommended in the elderly population. However, less evidence is available on the preventative role of influenza vaccination on asthma control in elderly patients with asthma.Citation4 Pneumococcal vaccination is recommended in patients with COPD, but its value in adult patients with asthma is less certain.Citation4
Pharmacologic interventions
Severe allergic asthma includes patients at steps 4 and 5 of GINA guidelines.Citation1 General rules of pharmacotherapy for the elderly are not different from those for adult patients.Citation1 GINA recommends add-on tiotropium if there is a history of exacerbation and a high-dose corticosteroid plus long-acting β2 adrenergic agonist and extra controllers, such as leukotriene-modifying agents and theophylline for patients at step 4.Citation1 Factors such as arthritis, inspiratory flow rate, and complexity of treatment regimens should be considered when choosing medication and inhaler devices.Citation1 Treatment response must be monitored carefully because elderly patients may have discordant correlations between changes in symptoms and lung function. Side effects, polypharmacy, and drug interactions should also be considered in the elderly.Citation49
Leukotriene-modifying agents have been shown to be effective in the prevention of allergen-induced asthma, but studies on their use in the elderly are limited.Citation4 Inhaled β-agonists can induce tremor or tachycardia in susceptible patients.Citation4 Tiotropium has an excellent safety profile in the elderly and may be a good option in age-related reduction in lung function and the frequent overlap between asthma and COPD in the elderly.Citation4,Citation49 Theophylline is an effective bronchodilator and has some anti-inflammatory properties,Citation4 but its use has been reduced considerably over the past decade due to safety concerns, especially in the elderly. The narrow therapeutic range, frequency of concomitant illnesses that alter kinetics, and many drug interactions that affect the clearance of theophylline show that theophylline levels in the blood of elderly patients with asthma must be monitored closely.Citation4 Anti-IgE (omalixumab) is a treatment option for patients with severe allergic asthma uncontrolled upon step 4 treatment.Citation1 Korn et alCitation50 confirmed that the efficacy of omalixumab in patients with severe allergic asthma is similar in younger and older patients. Long-term treatment with oral corticosteroids may be required for some patients with severe allergic asthma. However, older individuals experience more adverse drug effects and have comorbidities such as diabetes mellitus and hypertension that can worsen because of corticosteroid use. Antiplatelet therapy with aspirin for the management of cerebrovascular disease or cardiovascular disease can be challenging in aspirin-sensitive patients with asthma. If aspirin therapy is indicated in an asthmatic patient with aspirin sensitivity, aspirin desensitization could be a treatment option. Key points in the management of severe allergic asthma are shown in .
Conclusion
Some data suggest that allergic asthma in older adults is phenotypically different from that observed in younger patients. Asthma management in the elderly follows the same steps as that in younger adults, but asthma in the elderly is underdiagnosed and undertreated. Attending physicians must take into account the factors in elderly patients with severe allergic asthma that contribute to the risk of uncontrolled disease: a low level of education; poor memory and coordination; hearing, visual, and neuromuscular difficulties in learning inhaler-use methods and asthma self-management plans; and nonadherence to asthma medication.
Disclosure
The authors report no conflicts of interest in this work.
References
- Global Initiative for Asthma (GINA) [homepage on the internet]Global Strategy for Asthma Management and Prevention Available from: http://www.ginasthma.org/local/uploads/files/GINA_Report_2015_Aug11.pdfAccessed April 24, 2015
- de NijsSBVenekampLNBelEHAdult-onset asthma: is it really different?Eur Respir Rev201322445223457164
- MirandaCBusackerABalzarSTrudeauJWenzelSEDistinguishing severe asthma phenotypes: role of age at onset and eosinophilic inflammationJ Allergy Clin Immunol200411310110814713914
- GibsonPGMcDonaldVMMarksGBAsthma in older adultsLancet201037680381320816547
- YáñezAChoSHSorianoJBAsthma in the elderly: what we know and what we have yet to knowWorld Allergy Organ J201471825152804
- BauerBAReedCEYungingerJWWollanPCSilversteinMDIncidence and outcomes of asthma in the elderly. A population-based study in Rochester, MinnesotaChest199711123033109041973
- CardonaVGuilarteMLuengoOLabrador-HorrilloMSala-CunillAGarrigaTAllergic diseases in the elderlyClin Transl Allergy201111122409889
- MelaniASManagement of asthma in the elderly patientClin Interv Aging20138913e92223885171
- Di LorenzoGDi BonaDLa PianaSDittaVStefania Leto-BaroneMBronchial asthma-emerging therapeutic strategiesSapeyEAllergic Asthma and AgingRijekaInTech201290116
- VenturaMTScichiloneNGelardiMPatellaVRidoloEManagement of allergic disease in the elderly: key considerations, recommendations and emerging therapiesExpert Rev Clin Immunol201511111219122826483075
- BussePJCohnRDSaloPMZeldinDCCharacteristics of allergic sensitization among asthmatic adults older than 55 years: results from the National Health and Nutrition Examination Survey, 2005–2006Ann Allergy Asthma Immunol2013110247e25223535087
- JaakkolaMSIeromnimonAJaakkolaJJAre atopy and specific IgE to mites and molds important for adult asthma?J Allergy Clin Immunol2006117642e64816522465
- ArrudaLKVailesLDFerrianiVPSantosABPomésAChapmanMDCockroach allergens and asthmaJ Allergy Clin Immunol2001107419e42811240940
- Di LorenzoGMansuetoPMellusoMNon-specific airway hyperresponsiveness in mono-sensitive Sicilian patients with allergic rhinitis. Its relationship to total serum IgE levels and blood eosinophils during and out of the pollen seasonClin Exp199727910521059
- CelikelSIsikSRDemirAUKarakayaGKalyoncuAFRisk factors for asthma and other allergic diseases in seasonal rhinitisJ Asthma200845871071418951265
- OzturkABOzyigit PurLKostekOKeskinHAssociation between asthma self-management knowledge and asthma control in the elderlyAnn Allergy Asthma Immunol2015114648048425935432
- WolfeRCarlinJBOswaldHOlinskyAPhelanPDRobertsonCFAssociation between allergy and asthma from childhood to mid-adult life in an Australian cohort studyAm J Respir Crit Care Med20001622177218111112134
- Ozyigit PurLOzturkABKeskinHAllergic asthma: differences in characteristics between younger and older patientsRev Fr Allergol2015555379381
- InoueHNiimiATakedaTPathophysiological characteristics of asthma in the elderly: a comprehensive studyAnn Allergy Asthma Immunol2014113552753325216975
- BramanSSKaemmerlenJTDavisSMAsthma in the elderly. A comparison between patients with recently acquired and long-standing diseaseAm Rev Respir Dis199114323363401990949
- EnrightPLWardBJTracyRPLasserECAsthma and its association with cardiovascular disease in the elderly. The Cardiovascular Health Study Research GroupJ Asthma199633145538621370
- ParkHWKwonHSKimTBCOREA Study GroupDifferences between asthma in young and elderly: results from the COREA studyRespir Med20131071509151423927852
- ParkHWSongWJKimSHClassification and implementation of asthma phenotypes in elderly patientsAnn Allergy Asthma Immunol20151141182225455518
- TsaiC-LLeeW-YHananiaNCamargoCAJrAge-related differences in clinical outcomes for acute asthma in the United States, 2006–2008J Allergy Clin Immunol20127152158
- TalrejaNBaptistAPEffect of age on asthma control: results from the National Asthma SurveyAnn Allergy Asthma Immunol201110624e2921195941
- ChungKFWenzelSEBrozekJLInternational ERS/ATS guidelines on definition, evaluation and treatment of severe asthmaEur Respir J20144334337324337046
- HananiaNAKingMJBramanSSLedfordDKAsthma in Elderly Workshop ParticipantsAsthma in the elderly: current understanding and future research needs – a report of a National Institute on Aging (NIA) workshopJ Allergy Clin Immunol20111283 supplS4S2421872730
- MathurSKAllergy and asthma in the elderlySemin Respir Crit Care Med201031558759520941659
- ReedCEAsthma in the elderly: diagnosis and managementJ Allergy Clin Immunol201012668168720673985
- MilaneseMDi MarcoFCorsicoAGELSA Study GroupAsthma control in elderly asthmatics. An Italian observational studyRespir Med201410881091109924958604
- GoemanDPDouglasJAOptimal management of asthma in elderly patients. Starategies to improve adherence to recommended interventionsDrugs Aging200724538139117503895
- YapAFThirimoorthyTKwanYHSystematic review of the barriers affecting medication adherence in older adultsGeriatr Gerontol Int Epub20151020
- MooreWCBleeckerERCurran-EverettDNational Heart, Lung, Blood Institute’s Severe Asthma Research ProgramCharacterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute’s Severe Asthma Research ProgramJ Allergy Clin Immunol200711940541317291857
- MooreWCMeyersDAWenzelSENational Heart, Lung, and Blood Institute’s Severe Asthma Research ProgramIdentification of asthma phenotypes using cluster analysis in the Severe Asthma Research ProgramAm J Respir Crit Care Med201018131532319892860
- WardzyńskaAKubsikBKowalskiMLComorbidities in elderly patients with asthma: association with control of the disease and concomitant treatmentGeriatr Gerontol Int201515790290925243580
- National Heart, Lung, and Blood Institute [webpage on the Internet]NAEPP Working Group ReportConsiderations for Diagnosing and Managing Asthma in the Elderly Available from: http://msdh.ms.gov/msdhsite/_static/resources/2107.pdfAccessed March 20, 2013
- ChenMHLiCTTsaiCFRisk of dementia among patients with asthma: a nationwide longitudinal studyJ Am Med Dir Assoc2014151076376725037169
- BozekAJarzabJImproved activity and mental function related to proper antiasthmatic treatment in elderly patients with Alzheimer’s diseaseAllergy Asthma Proc201132534134522195685
- SorianoJBVisickGTMuellerovaHPayvandiNHansellALPatterns of comorbidities in newly diagnosed COPD and asthma in primary careChest200572099210716236861
- ManouchehriniaAEdwardsLJRoshanisefatHTenchCRConstantinescuCSMultiple sclerosis course and clinical outcomes in patients with comorbid asthma: a survey studyBMJ Open201555e007806
- ChengCMWuYHTsaiSJRisk of developing Parkinson’s disease among patients with asthma: a nationwide longitudinal studyAllergy201570121605161226310430
- Global Initiative for Chronic Obstructive Lung Disease [webpage on the Internet]Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease [updated April 2, 2015]. Avaliable from: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2015_Apr2.pdfAccessed January 30, 2016
- De MarcoRPesceGMacronAThe coexistence of asthma and chronic obstructive pulmonary disease (COPD): prevalence and risk factors in young, middle aged and elderly people from the general populationPLoS One201385e6298523675448
- PostmaDSRabeKFThe asthma-COPD overlap syndromeN Engl J Med2015373131241124926398072
- NielsenMBarnesCBUlrichCSClinical characteristics of the asthma-COPD overlap syndrome-a systemic reviewInt J Chron Obstruct Pulmon Dis2015101443145426251584
- HarataTYamasakiAFukishimaTCauses of death in patient with asthma and asthma-chronic obstructive pulmonary disease overlap syndromeInt J Chron Obstruct Pulmon Dis20151059560225834418
- BarnesPJTherapeutic approaches to asthma-chronic obstructive pulmonary disease overlap syndromeJ Allergy Clin Immunol201513653154526343937
- WolfendenLLDietteGBSkinnerEASteinwachsDMWuAWGaps in asthma care of the oldest adultsJ Am Geriatr Soc20025087788312028175
- SongWJChoSHChallenges in management of asthma in the elderlyAllergy Asthma Immunol Res20157543143926122503
- KornSSchumannCKropfCEffectiveness of omalizumab in patients 50 years and older with severe persistent allergic asthmaAnn Allergy Asthma Immunol2010105431331920934632