Abstract
Introduction
Severe neonatal hyperbilirubinemia can cause mortality and serious morbidities. When phototherapy fails, neonates with severe hyperbilirubinemia should undergo double volume blood exchange transfusion (BET). As this procedure carries a significant risk of mortality and morbidity, adopting guidelines for the treatment of neonatal hyperbilirubinemia is critical to avoid hyperbilirubinemia toxicity and also the complication of an unindicated procedure.
Methods
This study investigated the causes, complications, and trend of BET rate in our unit over a 13-year period. The medical charts and laboratory databases of all infants who underwent BET in Jordan University Hospital between 2003 and 2015 were retrospectively reviewed.
Results
The rate of exchange cases decreased significantly after adopting the guidelines of American Academy of Pediatrics (P<0.0001). Most neonates were term newborns (69%). Average birth weight was 2,800 g. The most common causes of exchange transfusion were non-hemolytic conditions. Late prematurity alone accounted for 20% of the cases. Thrombocytopenia was the most commonly encountered complication (33%). Chronic neurological complications were seen in 12% of those who were followed for >12 months of age.
Conclusions
This study showed a clear decline in the rate of BET after implementing the guidelines of American Academy of Pediatrics. In addition to improving the strategies for the identification and follow-up of at-risk newborns, we should intensify our efforts to prevent the progression of neonatal hyperbilirubinemia to the exchange level by enhancing parents’ awareness of this potentially harmful neonatal condition.
Introduction
Neonatal hyperbilirubinemia is a common phenomenon that is usually benign.Citation1 However, severe neonatal hyperbilirubinemia can cause mortality and serious morbidities.Citation2 When neonates with severe hyperbilirubinemia fail to respond to phototherapy, double volume blood exchange transfusion (BET) is the only option.Citation3 As this procedure carries a significant rate of complications,Citation4 neonatal hyperbilirubinemia guidelines are critical to avoid both hyperbilirubinemia toxicity and the complication of an invasive therapy.Citation3,Citation5
The present study was conducted to investigate the rate of BET and its complications. Furthermore, the effect of adopting the guidelines outlined by the American Academy of Pediatrics (AAP)Citation3 on the rate of BET in our institution was also investigated.
Patients and methods
This study examined neonatal exchange transfusion due to indirect hyperbilirubinemia. We aimed to study the causes, complications, and trend of the exchange transfusion rate in our unit over a 13-year period. The medical charts and laboratory databases of all infants who underwent BET in Jordan University Hospital between 2003 and 2015 were retrospectively reviewed. The study was approved by the Deanship of Scientific Research at the University of Jordan and was reviewed and approved by the Institutional Review Board Committee and the Ethical Committee at the University of Jordan. Patient’s consent to review medical charts was not required due to the retrospective nature of the study which does not include patient identifiers. To insure patient’s confidentiality, medical charts revision process is only allowed inside the medical charts department. All the authors in this study had the privilege to access files of pediatric patients in Jordan University Hospital.
Setting
Our university hospital is a tertiary center, with >4,000 deliveries/year. The neonatal unit provides care for premature infants and sick neonates, with a capacity of 30 beds. The hospital delivers post-discharge well-newborn services, including physical examination and neonatal screen within 72 hours of discharge.
Antenatal screening and management
All pregnant women followed in Jordan University Hospital have their blood tested for ABO grouping and RhD typing and for antibodies using the indirect antiglobulin test (IAT). Anti-D immunoglobulins are administered to Rh-negative women antenatally and postnatally accordingly. In case of sensitization, follow-up is performed by serial IAT titers and by monitoring the development of anemia in the infants using the middle cerebral artery Doppler measurement. Intrauterine blood transfusion is performed for severely anemic fetuses.
Neonatal screening protocol
Jordan University Hospital guidelines indicate that all neonates born to Rh-negative mothers, blood group type O mothers, positive IAT mothers, or to mothers with unknown blood group are screened by the direct antiglobulin test (DAT) and have their bilirubin level measured using cord blood. Cord blood DAT results were considered reliable and were not confirmed by peripheral blood samples. Any newborn whose DAT was positive or cord bilirubin level was ≥3 mg/dL immediately had their serum bilirubin level measured, and then serial measurements were performed every 4–6 hours, depending on the degree of rise. All other newborns had their serum bilirubin level measured whenever they developed jaundice.
Two years ago, regardless of their clinical jaundice status, we began screening all newborns prior to discharge using a transcutaneous bilirubinometer. Data from these 2 years have not been included in the current study.
Phototherapy
Phototherapy is initiated when newborns’ serum bilirubin reaches phototherapy level. Phototherapy level is affected by the newborn’s age, presence of risk factors that increase bilirubin toxicity such as hemolysis, glucose-6-phosphate dehydrogenase (G6PD) enzyme deficiency, sepsis, etc.Citation6 Prophylactic phototherapy is not routinely practiced in our unit. An intensive phototherapy 360° cradle was introduced to the service in 2009.
Intravenous immunoglobulin (IVIG) use
IVIGs are used only when the DAT of the infant is positive and there is evidence of ongoing hemolysis. The attending on-call in our unit refers to 2 protocols for the use of IVIG. This treatment is implemented either according to the AAP guidelines whenever the bilirubin level is 2 mg/dL below the exchange level in a newborn with hemolytic disease and a positive DAT, or whenever the newborn has a positive DAT and his/her bilirubin level reaches phototherapy level. The rationale of the second approach is that an increasing bilirubin level reaching the threshold of therapy means significant hemolysis. Furthermore, when following the AAP guidelines, the time required for IVIG transfusion might be too long to be of benefit when the rate of rise is rapid and the infant is only 2 mg/dL away from exchange. The dose of IVIG is 1 g/kg over 2 hours. During IVIG transfusion, the newborn infant is placed on continuous cardiorespiratory monitoring. and vital signs are documented every 15 minutes. If any reaction develops, the transfusion is stopped, and the physician is called to evaluate the newborn and administer medication if needed.
Exchange transfusion: threshold
Exchange transfusion is performed for infants presenting with acute bilirubin encephalopathy or whose bilirubin is at the exchange level and fails to respond to phototherapy. Prior to 2008, a serum bilirubin level of 20 mg/dL was the exchange level for healthy term infants.Citation7 At the end of 2008, the AAP guidelinesCitation3 for phototherapy and the exchange level were fully adopted.
Exchange transfusion: preparation
Once the bilirubin level is at, or approaching, the exchange level, a compatibility cross-matching is done using O RhD-negative or ABO-compatible RhD-negative packed red blood cells (PRBCs). The transfused blood is filtered as per our blood bank protocol. Blood irradiation is not available in Jordan University Hospital. A volume of 90 cc/kg is prepared and reconstituted with an equal volume of AB-positive fresh frozen plasma. Reconstitution is performed only when the decision for exchange is taken. The blood should not be >5 days old. If only older PRBCs are available, washed PRBCs should be used. Cytomegalovirus-negative blood is only requested when the newborn is premature, <34 weeks gestational age. The blood bank in Jordan University Hospital uses calcium citrate as a preservative. Parents are informed of the procedure and its benefits and potential complications.
Exchange transfusion: procedure
Exchange transfusion is performed using an umbilical venous catheter. A pre-prepared exchange set is employed. The provided data sheet is used for documenting the exchanged volumes of blood and should be kept in the newborn’s chart. Blood is exchanged in small aliquots (5–10 cc). During the exchange, the newborn is on continuous cardiorespiratory monitoring. If the newborn becomes bradycardic, the procedure is stopped, and the newborn receives resuscitation according to the neonatal resuscitation guidelinesCitation8,Citation9 and also receives 200 mg/kg calcium gluconate intravenously. Feeding is stopped, and intravenous fluid is started upon approaching the exchange level and this continues for 24 hours after the exchange transfusion, provided the bilirubin level is falling. The umbilical venous catheter is retained until 24 hours after the exchange or until the level of bilirubin continuously falls, whichever is later. Antibiotics are not routinely administered unless there is a suspicion of sepsis. Fluids are not routinely increased unless dehydration is present.
Laboratory investigations
The first 5 cc of blood withdrawn is sent to the laboratory for the following analyses: complete blood count, blood film, electrolytes, calcium, alanine transaminase, G6PD, and thyroid function test. The final 5 cc undergoes the same investigations except for G6PD and thyroid function test.
The bilirubin level is measured every 4–6 hours depending on the degree of rise, and the Hb level is measured at least every 12 hours.
Statistical analysis
Overall trends in exchange transfusion are presented for the period 2003–2015 (before and after adoption of the AAP guidelines) and assessed by χ2 for trend tests. Other data are presented as numbers and frequencies. A P-value <0.05 is considered statistically significant.
Results
The rate of exchange cases decreased significantly after adoption of the AAP guidelines at the end of 2008 (). There were 20,730 live newborns between 2003 and 2008, with 38 cases of BET. Between 2009 and 2015, there were 35,041 live newborns with 7 cases of BET (P<0.0001). Most neonates who underwent BET were term newborns (69%). Their average birth weight was 2,800 g. Most mothers had O blood group and were Rh positive. Most newborns were admitted due to hyperbilirubinemia. The demographic data and hospitalization characteristics are detailed in .
Figure 1 Number of exchange cases during the study period with the change in rate illustrated before and after the adoption of the AAP hyperbilirubinemia guidelines.
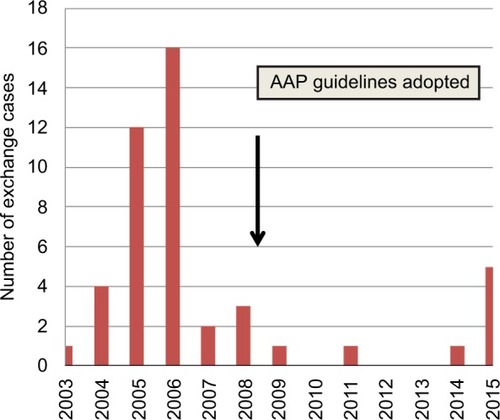
Table 1 Demographic and hospitalization data of neonates who underwent exchange transfusion in a tertiary care center in Jordan
The most common causes of exchange transfusion were non-hemolytic conditions. A 2×2 contingency table was used to compare the rate of severe hyperbilirubinemia between hemolytic and non-hemolytic cases; there was no significant difference with P-value of 0.2 and odds ratio of 0.4 (95% CI: 0.094–1.68). Late prematurity alone accounted for 9 cases (). Thrombocytopenia was the most commonly encountered complication (33%). Chronic neurological complications were seen in 12% of those who were followed for >12 months of age ().
Table 2 Causes of exchange transfusion in tertiary health care center in Jordan over a 13-year period
Table 3 Short- and long-term complications of neonates who underwent exchange transfusion in tertiary care center in Jordan
Discussion
Exchange transfusion for neonatal hyperbilirubinemia is an effective procedure for preventing chronic bilirubin encephalopathy.Citation10 However; it carries a significant risk of mortality and morbidity.Citation11
The rate of BET is declining worldwide.Citation12,Citation13 Many factors have contributed to this, mainly antenatal antibody screening, anti-D administration,Citation14,Citation15 intensive phototherapy,Citation16 and the use of IVIG.Citation17 The adoption of neonatal screening programs and the change in therapeutic thresholds have also contributed greatly to the improvement of neonatal severe hyperbilirubinemia outcomes and the decline in the BET rate.Citation3,Citation11
In this study, we investigated the trend of neonatal BET in our unit over a 13-year period, focusing on the stage of complete adoption of the AAP guidelines for the treatment of severe neonatal hyperbilirubinemia. A decrease in the rate of BET after adoption of the AAP guidelines has previously been reported.Citation5,Citation18 This finding was also clearly demonstrated in our cohort (). The AAP guidelines offered more structured approach to neonates approaching exchange level. The time of making the decision to perform exchange was a major change. The decision is based on the response to phototherapy and whether the treatment is successful in decreasing the bilirubin below exchange level, rather than the initial bilirubin prior to starting phototherapy.Citation3 Other major revisions that the AAP guidelines introduced into our practice were the change in the exchange level for healthy term newborns (which used to be 20 mg/dL) and IVIG administration for DAT-positive hemolytic diseases. The AAP guidelines were introduced earlier to our unit but were not adopted fully by all treating physicians; this might explain the earlier decline of exchange transfusion cases starting prior to the significant decline that happened in 2008.
During the time of AAP guidelines adoption, we also introduced a 360° phototherapy cradle unit. It is highly likely that this improved the rate of phototherapy response in infants with severe hyperbilirubinemia and played a role in the BET rate decline.Citation19,Citation20
In contrast to previous studies, hemolytic conditions were not the most common cause of severe hyperbilirubinemia that led to BET in our cohort.Citation12,Citation13 This might reflect the strict approach our institution applies during antenatal care to identify and follow-up at-risk newborns. All neonates with a positive DAT are identified pre-discharge and go home with a plan for bilirubin follow-up. Intensive phototherapy and IVIG treatment almost certainly contributed to the better outcomes in hemolytic situations.
The predisposition of late premature infants to severe hyperbilirubinemia has been previously documented.Citation21 In this study, there were 9 patients who did not have any identified cause of their severe hyperbilirubinemia except for being late premature newborns. This highlights the importance of close follow-up of late preterm newborns without apparent risk factors for severe hyperbilirubinemia.
Several side effects of BET have previously been reported, primarily thrombocytopenia and metabolic disturbances.Citation13 In our cohort, thrombocytopenia was the most commonly encountered short-term complication. None of the newborn infants had thrombocytopenia prior to exchange. Immune-mediated reactions due to the presence of platelet A immunoglobulin G in donor plasma may explain the severe thrombocytopenia cases that required platelet transfusions,Citation22 whereas dilution effects of transfused blood might explain the milder cases. There was no hemorrhagic complication encountered.
Outpatient clinic follow-up for >1 year of age was achieved in only 56% of the patients. Chronic neurological deficits were found in 3 (12%) of those patients. All were male newborns and had normal G6PD levels. The first patient was a late preterm newborn and had a bilirubin level of 40 mg/dL. The second patient was a small-for-gestational age late preterm newborn and had a bilirubin level of 15 mg/dL. Their hyperbilirubinemia cause was not identified. The third patient had hemolysis due to Rh isoimmunization and his highest bilirubin level was 34 mg/dL, and he received IVIG. In addition to sever hyperbilirubinemia, the first 2 infants were at higher risk for adverse neurodevelopment outcomes due to their gestational age.Citation23
This study showed a clear decline in the rate of BET after implementation of the AAP guidelines. In addition to improving the identification and follow-up strategies of at-risk newborns, we should intensify our efforts to prevent the progression of neonatal hyperbilirubinemia to the exchange level by enhancing parents’ awareness of this potentially harmful neonatal condition, which was recently shown to be lacking in our population.Citation24
Disclosure
The authors report no conflicts of interest in this work.
References
- BhutaniVKStarkARLazzeroniLCInitial Clinical Testing Evaluation and Risk Assessment for Universal Screening for Hyperbilirubinemia Study GroupPredischarge screening for severe neonatal hyperbilirubinemia identifies infants who need phototherapyJ Pediatr20131623477.e1482.e123043681
- SgroMCampbellDShahVIncidence and causes of severe neonatal hyperbilirubinemia in CanadaCMAJ2006175658759016966660
- American Academy of Pediatrics Subcommittee on HyperbilirubinemiaManagement of hyperbilirubinemia in the newborn infant 35 or more weeks of gestationPediatrics2004114129731615231951
- Abu-EkteishFDaoudARimawiHKakishKAbu-HeijaANeonatal exchange transfusion: a Jordanian experienceAnn Trop Paediatr2000201576010824215
- JangaardKAAllenAChanges in practice patterns for treatment of hyperbilirubinemia in healthy, full term infants in Nova Scotia, Canada following the AAP practice parametersPaediatr Child Health20027Suppl A22A23A
- BhutaniVKJohnsonLSivieriEMPredictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newbornsPediatrics199910316149917432
- MaiselsMJNewmanTBKernicterus in otherwise healthy, breast-fed term newbornsPediatrics1995964 Pt 17307337567339
- WyckoffMHAzizKEscobedoMBPart 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular CareCirculation201513218 Suppl 2S543S56026473001
- NANN Board of DirectorsPrevention of acute bilirubin encephalopathy and kernicterus in newborns: position statement #3049Adv Neonatal Care2011115 SupplS3S922123452
- OlusanyaBOOgunlesiTASlusherTMWhy is kernicterus still a major cause of death and disability in low-income and middle-income countries?Arch Dis Child201499121117112125123403
- ChessmanJCBowenJRFordJBNeonatal exchange transfusions in tertiary and non-tertiary hospital settings, New South Wales, 2001–2012J Paediatr Child Health201753544745028370676
- HakanNZencirogluAAydinMOkumusNDursunADilliDExchange transfusion for neonatal hyperbilirubinemia: an 8-year single center experience at a tertiary neonatal intensive care unit in TurkeyJ Matern Fetal Neonatal Med201428131537154125182682
- BujandricNGrujicJExchange transfusion for severe neonatal hyperbilirubinemia: 17 years’ experience from Vojvodina, SerbiaIndian J Hematol Blood Transfus2015322208214
- LiumbrunoGMD’AlessandroAReaFThe role of antenatal immunoprophylaxis in the prevention of maternal-fetal anti-Rh (D) alloimmunisationBlood Transfus20108181620104273
- HardingHLMartlewVJMcFadyenIRClarkeCAPreventing Rhesus D haemolytic disease of the newborn by giving anti-D immunoglobulin: are the guidelines being adequately followed?Br J Obstet Gynaecol19971041869870
- EdrisAAGhanyEARazekARZahranAMThe role of intensive phototherapy in decreasing the need for exchange transfusion in neonatal jaundiceJ Pak Med Assoc20146415824605703
- CorteyAElzaabiMWaegemansTRochBAujardYEfficacy and safety of intravenous immunoglobulins in the management of neonatal hyperbilirubinemia due to ABO incompatibility: a meta-analysisArch Pediatr2014219976983 French25125032
- SteinerLABizzarroMJEhrenkranzRAGallagherPGA decline in the frequency of neonatal exchange transfusions and its effect on exchange-related morbidity and mortalityPediatrics20071201273217606558
- Abd-EllatifMAAbd-EllatifDAThe use of intensive phototherapy in severe neonatal hyperbilirubinemiaJ Egypt Soc Parasitol201242248349323214225
- de CarvalhoMMochdeceCCSáCAMoreiraMEHigh-intensity phototherapy for the treatment of severe non haemolytic neonatal hyperbilirubinemiaActa Paediatr2011100462062321251060
- ReichmanNETeitlerJOMoullinSOstfeldBMHegyiTLate-preterm birth and neonatal morbidities: population-level and within-family estimatesAnn Epidemiol201525212613225481078
- ForsterJSchmidtBKünzerWUse of an immunoenzyme microtechnic for quantitative determination of platelet-associated IgG in pediatrics. Acute idiopathic thrombocytopenia purpura and thrombocytopenia following exchange transfusionMonatsschr Kinderheilkd198313131571606682933
- VohrBLong-term outcomes of moderately preterm, late preterm, and early term infantsClin Perinatol201340473975124182959
- Al-lawamaMAlbaramkiJKarajehDDmourHMaternal knowledge of neonatal jaundice and its relation to their level of education in Amman, JordanKasmera2017451118
