Abstract
The blood transfusion (BT) system in Pakistan is fragmented, demand-driven and depends on weakly regulated transfusion practices. There is a considerable possibility that transfusion-transmissible infections (TTIs) are contributing to the current epidemic of hepatitis B virus (HBV) and hepatitis C virus (HCV) (affecting 7.4% of the general population) in the country. To study this issue, we conducted a systematic review to identify articles related to TTIs and transfusion safety in Pakistan from January 1, 2010 to January 31, 2020. A review of 33 articles met the final criteria for qualitative synthesis. Analysis of these studies showed a cumulative frequency of HBV 2.04%, HCV 2.44%, HIV 0.038%, syphilis 1.1% and malaria 0.11%. The frequency of coinfections among blood donors varied from 0.0099% to 0.35%. The highest number of coinfections were HCV and syphilis, followed by HCV and HBV infections. Syphilis and malaria were tested in only 38% and 46% of all the blood donations in one study. The rate of voluntary non-remunerated donations (VNRDs) was less than 13%, and male donors were 95% to 100% in these studies. There was a significant difference in the frequency of HBV and HCV in VNRDs (0.48%) as compared to replacement donors (RDs) (4.15%). In short, this review shows a high frequency of TTIs, especially HBV, HCV and syphilis in the blood donor population in Pakistan. There is a high dependency on RDs, minimal use of healthy voluntary blood donation practices, inadequate screening of high-risk donors, repeated collections of the blood from RDs, poor quality of screening methods and limited knowledge of donor health. Without standardized safe transfusion practices, there will be an ongoing increase in transmission of TTIs, especially HBV, HCV, syphilis, and HIV leading to a significant adverse public health impact.
Introduction
Blood transfusion (BT) is an essential lifesaving treatment and is an integral part of the World Health Organization (WHO) list of essential medicines.Citation1 WHO recommends achieving self-sufficiency to meet the transfusion needs of a population with a safe supply of blood components based on voluntary, non-remunerated blood donations (VNRDs) along with a security of supply chain for providing safe end-product to patients.Citation1 An estimated 3.5 million blood donations are collected every year in Pakistan.Citation2 Blood transfusions are used mainly for chronically transfusion-dependent thalassemia patients, anemia due to poor health conditions, acute trauma, surgical procedures, hemorrhage and pregnancy-related complications.Citation5 An estimated one-fourth of the national annual blood collections are used for transfusion-dependent thalassemia patients.Citation6 Pakistan has one of the highest hepatitis B virus (HBV) and hepatitis C virus (HCV) prevalence (5 and 10 million, respectively) in the world and unsafe BT practices are further fueling this epidemic.Citation3 Blood-borne transmissions remain a crucial vector for transmission of HBV and HCV infections, affecting about 7.4% of the general population.Citation4 The maternal mortality rate in Pakistan is one of the highest in the world (276/100,000 live births) and the major causes of maternal deaths are due to complications of anemia and bleeding.Citation7
Major challenges for BT safety in Pakistan include the high prevalence of HBV and HCV infections in the general population, lower rates of voluntary donations, lack of standardized screening measures of donors and limited reporting of TTIs. In addition, blood banks (BBs) in Pakistan transfuse most blood as whole blood though the concept and facilities for blood component therapy (red blood cells, platelets, and plasma) is evolving in urban and tertiary care centers. Rural areas, however, face significant difficulty in accessing safe BT products. This leads to unsafe practices in the supply chain, lack of knowledge and adherence to the WHO guidelines and the use of improperly screened blood.
WHO strategy for universal safe blood transfusion places an emphasis on the development of a well-coordinated BT system with an exclusive collection of blood from VNRDs, quality-assured donor testing, evidence-based use of BT practices, development of universal quality and monitoring metrics.Citation8 To raise the standard of BT safety according to the WHO guidelines, Pakistan has developed the “Safe Blood Transfusion Program (SBTP)” which was launched in 2010 with financial support from the German government and technical aid from the WHO. Its role is that of a central coordinating body at the federal level. The purpose of this program includes the development of a nationwide infrastructure of a new BT system.Citation5 It led to the development of 10 modern Regional Blood Centers (RBCs) and modernization of 60 existing Hospital Blood Banks (HBBs) in Phase I. SBTP Phase II is currently underway with a 10 million euros grant through the German Development Bank (KfW). It includes the expansion of RBCs’ network and upgrades to existing HBBs.Citation5
In this review, we estimated the frequency of transfusion-transmissible infections (TTIs) in the donor population to estimate the burden of TTIs through blood transfusions and reviewed various safety challenges associated with the BT system in Pakistan.
Materials and Methods
Search Strategy
We carefully conducted a comprehensive search of PubMed and PakiMediNet from inception to January 31, 2020 with no language restriction. The search queries were transfusion-transmitted infections, transfusion-related infections, TTIs and blood transfusion infections in Pakistan. Two authors (AW/HE) screened titles and abstracts of all identified results independently. Another two authors (MAS/MKS) reviewed the full-text articles according to the predefined inclusion and exclusion criteria. Discrepancies were resolved through discussion. In addition, the reference lists of potentially eligible studies were hand-searched to avoid overlooking any eligible studies. Our research did not require IRB approval or written consent.
Inclusion and Exclusion Criteria
Inclusion criteria were: 1) studies with more than 50 participants and 2) studies that showed the frequency of common TTIs (HBV, HCV, HIV, malaria, syphilis) in donor populations.
Exclusion criteria: 1) case reports, abstracts without full-length articles, meta-analysis and systemic reviews, 2) studies with uncommon TTIs such as West Nile virus, dengue fever and human T-lymphocyte virus-1/2, 3) studies with the frequency of TTIs in chronically transfusion-dependent patients of thalassemia major and hemophilia.
Data Extractions
Two authors independently extracted data (HE/AW) from the included studies including author, number of patients, type of donors, seropositive status of HBV, HCV, HIV, malaria, syphilis and coinfection.
Eligible Studies
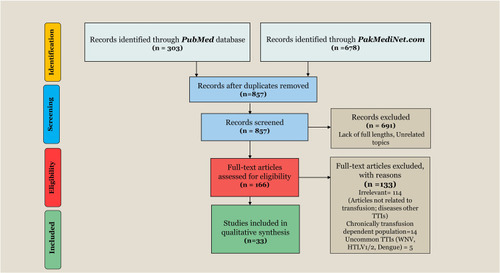
A total of 981 studies were identified based on initial database search and 857 studies remained after removing duplicates. After reviewing titles and abstracts, 166 studies were retrieved for full-length article review according to predefined inclusion and exclusion criteria. We excluded 133 studies for reasons indicated in the PRISMA flow chart (). Thirty-three studies were finally included in our systematic review.
Figure 1 PRISMA flow diagram showing a summary of selection process.
Definition for Positive Transfusion-Transmissible Infections
A blood donor was labelled positive for any particular TTI if reported reactive by the study irrespective of the type of investigation used.
Frequency of Transfusion-Transmissible Infections
The frequency (in percent) for any particular TTI in individual study was calculated as total number of donors with reactive TTI/total donor population screened multiplied by 100. We calculated the cumulative frequency of TTIs in the donor population, ie, the total number of donors reactive for a particular TTI in individual studies divided by the total donor population of all studies screened.
Diagnostic Methods for TTIs Used in Studies
Diagnostic methods used for detection of TTIs in these studies were diverse with variable sensitivity and specificity. Methods used included immunochromatographic methods (ICT), enzyme-linked immunosorbent assay (ELISA), microparticle enzyme immunoassay (MEIA), chemiluminescence assay (CIA) and nucleic acid amplification test (NAT).
Results
The characteristics of 33 studies included in the systemic review are given in . These studies used BBs’ data of large metropolitan cities in Pakistan such as Karachi, Hyderabad, Islamabad, Rawalpindi, Lahore, Faisalabad and Peshawar. Twenty-eight studies (n=672,199) evaluated the frequency of either HBV, HCV or both among donors (). Twenty-three studies (n=1,339,689) focused on the frequency of HIV, syphilis or malaria ().
Table 1 Characteristics of Studies (n=33) Included in a Systematic Review
Table 2 Summary of Data from Studies Reporting the Frequency of Hepatitis B and Hepatitis C Among Blood Donors
Table 3 Summary of Data from Studies Reporting Frequency of HIV, Syphilis, and Malaria in Blood Donors
Blood Transfusion Donors in Pakistan
Replacement donors (RDs) are the major type of donors in Pakistan with VNRDs ranging between 0.10%-13%.Citation11,Citation13,Citation19,Citation20,Citation22,Citation23,Citation28,Citation29,Citation33–Citation35 The proportion of blood donations by VNRDs varied between 0% and 91% across 19 BBs in one study, 8.25% of all donations were due to VNRDs and seven BBs had no donations by VNRDs.Citation19 Male donors comprised 95% to 100% of all blood donations. Donors were more prevalent in younger age groups.Citation12,Citation13,Citation22 Female donors ranged between 0% and 9.6% in individual studiesCitation9,Citation12,Citation13,Citation18,Citation20,Citation22 One study with data from both private and public BBs reported a higher proportion of female donors in private BBs versus public BBs, 29% vs 15%, p<0.01.Citation16
Transfusion-Transmissible Infections in Pakistan
The frequency of TTIs in blood donors varied among studies depending on donor types, number and types of TTI tested and screening methods. In 11 studies, authors screened donors for three or more TTIs (HBV, HCV, HIV,syphilis, and malaria) and cumulative frequency of TTIs was about 4% to 9% of all donors.Citation12,Citation13,Citation15,Citation18–Citation21,Citation25,Citation26,Citation28,Citation31 One study with 94% RDs reported the total frequency of TTIs to be 14.34%.Citation11 Three studies with 100% VNRDs reported a significantly lower frequency of TTIs, i.e., 3.54%, 4.9%, and 6.2%.Citation9,Citation17,Citation18 The frequency of TTI was significantly higher among RDs than in VNRDs in one study, 4.15% versus 0.48%.Citation13 TTIs, mainly HBV and HCV, were common causes of blood donation deferrals.Citation15,Citation23 Transfusion-related infections also resulted in discard of 5.01% of donated blood.Citation19 As the majority of studies had a smaller number of female donors, TTI frequency was exceptionally low among females.Citation12,Citation13,Citation17,Citation22,Citation24,Citation29 One study with the highest population (9.6%) of female donors (age range, 18–40, 67% females were 20–30 years-old) reported 22% (n=366) of reactive female donors.Citation20 Donors with a lower socioeconomic status had a higher frequency of TTIs.Citation35 According to Raza et al., the majority of reactive donors (69.5%) had a history of previous blood donations and had limited education.Citation31 When donors were educated it had a positive influence on their knowledge about TTIs. Odds of limited TTI knowledge were increased if donors had a secondary level of education versus tertiary level of education, OR: 4.04, CI: 1.567–10.435, p<0.01.Citation31 Overall, 48% of donors in the study had no knowledge that they could transmit an infection through blood transfusion. Donors with secondary education had better attitudes toward BT compared to those with primary education, OR: 2.019, CI: 1.190–3.426, p <0.01.Citation31 The notification of reactive donors about a positive test was also very low, i.e., 54.25% of all positive cases.Citation31 Major causes of a low notification rate were non-responses and failure to reach out to provided contact information.Citation31
Hepatitis B
The frequency of hepatitis B (HBsAg) in donors ranged from 0.81% to 4.22%.Citation9–Citation15,Citation17–Citation26,Citation28,Citation29,Citation31,Citation32,Citation34–Citation36 Cumulative frequency calculated from 24 studies published between 2010 and 2020 was 2.04% (n=16,203) and 20 studies had HBV frequency below 2% while 4 studies had frequency above 2%.Citation11,Citation12,Citation19,Citation36 Attaullah et al. recorded an upward trend in the frequency of HBV from 2.60% in 2008 to 5.03% in 2011.Citation12 Abdullah et al., however, documented a downward trend in the frequency from 1.78% in 2016 to 1.51% in 2017.Citation34 Sial et al recorded a higher HBV rate in males (63%) versus females (27%) but females accounted for 9.6% of all donors.Citation20 Similarly, Niazi et al. calculated a higher frequency among males (1.50%) versus females (0.37%) with females representing 1.5% of the donors.Citation22 Unmarried donors in one study were more likely to be reactive for HBsAg compared to married donors (p=0.001).Citation24
Hepatitis C
The frequency of hepatitis C (anti-HCV antibodies) in donors ranged from 1.29% to 10%. Cumulative frequency of HCV calculated from 26 studies was 2.44% (n=17,660).Citation9–Citation33,Citation35 Frequency of HCV was less than 2% in 8 studies,Citation9,Citation10,Citation19,Citation24,Citation30–Citation33 2–4% in 15 studies,Citation12–Citation15,Citation17,Citation20–Citation23,Citation25–Citation29,Citation35 and above 4% in 3 studies.Citation11,Citation16,Citation18 In 19 studies that investigated the reactivity of HBV and HCV within the same population, HCV was much more frequently detected than HBV.Citation10,Citation11,Citation13–Citation15,Citation17,Citation18,Citation20–Citation26,Citation28,Citation29,Citation31,Citation32,Citation35 HCV was the second most common cause (22.89%) of blood donation deferrals in one study.Citation15 In another study, HCV detection was the first most common cause (28.61%) of blood donation deferrals.Citation23 Irfan et al and Tufail et al. noted a higher number of reactive HCV cases in younger donors (less than 40 years).Citation13,Citation15 The number of HCV cases in male donors was higher than female donors in two studies, 74% vs 26% and 99.3% vs 0.7%.Citation20,Citation22 HCV-related risk factors were dental treatments (50%), traveling abroad (23.07%), history of surgery (11.53%) and blood transfusions in one study (7.69%).Citation30
HIV
The Frequency of HIV cases ranged between 0% and 0.18% in individual studies, with cumulative frequency equal to 0.038% (n=497) based on 18 studies.Citation11–Citation13,Citation15,Citation18–Citation22,Citation24–Citation26,Citation28,Citation29,Citation31,Citation32,Citation35,Citation39 Two studies had 0% of HIV-reactive cases.Citation2–Citation11 Another two studies had HIV frequency of 0.02% (N=26) and 0.07% (n= 20) of the screened population, all positive cases were men.Citation20,Citation22 Irfan et al. reported a low frequency (0.10%) of HIV-positive cases but faced difficulty in following up on reactive cases.Citation13 Among 30 reactive cases in this study, only a small number responded to follow-up calls, and 5 cases actually returned to the BB for a confirmatory test. All those who underwent a confirmatory test were reactive.Citation13 There was a downward trend in HIV frequency from 2008 to 2011 in one study with an overall frequency of 0.06%.Citation12 Another study published in 2014 found 16 HIV reactive cases (0.0057%) between 1998 and 2006, and 50 reactive cases (0.014%) between 2007 and 2013, showing an upward trend.Citation39 The causes of HIV contraction in this study were heterosexual high-risk sexual behavior (65%), intravenous drug use (39%) and blood transfusions (12%). The author reported “men who have sex with men – MSM” in only 1.5% of cases.Citation39
Syphilis
The frequency of syphilis in blood donors was between 0.11% and 3.01% in 17 studies with a cumulative frequency of 1.1% (n=6974).Citation11,Citation12,Citation18–Citation26,Citation28,Citation29,Citation31,Citation32,Citation35,Citation41 Seven studies reported syphilis in less than 1% of the donors,Citation11,Citation12,Citation18,Citation19,Citation22,Citation23,Citation32 six studies between 1% and 2%,Citation20,Citation21,Citation28,Citation29,Citation31,Citation35 and four studies in more than 2% of donors.Citation24–Citation26,Citation41 In one study, the author collected data from 19 BBs, 6 BBs did not routinely screen donors for syphilis and only 38% of all donations were screened for syphilis.Citation19 Syphilis reactivity also led to the rejection of 10.4% of donors.Citation23 In one study from Karachi, daily wage laborers and married donors were more likely to be syphilis reactive.Citation24 Zahoor et al. noted an upward trend of syphilis cases between 2016 (2.02%) to 2017 (2.46%). These donors were referred to their center from all over Pakistan.Citation41 Ghafoor et al.noted six out of seven (86%) total cases of syphilis being above 40.Citation18 Among 571 reactive syphilis donors reported by Sial et al., 93% were men and the majority of reactive donors (54%) were between the age of 20 and 30.Citation20 Similar to this, 99% of reactive donors were men in another study.Citation22
Malaria
The frequency of malarial parasite ranged from 0.005% to 1.2% with a cumulative frequency of 0.11% (n=368) of all blood donors that were screened.Citation11,Citation19,Citation21,Citation24–Citation26,Citation28,Citation29,Citation31,Citation32,Citation35,Citation37,Citation38,Citation40 All studies had a frequency of malaria less than 1% except one study by Waheed et al. with a frequency of 1.20%.Citation11 The malarial parasite was not routinely screened by six BBs in one study and only 46% of blood donations were screened.Citation19 Malaria was the least frequently detected TTI in those studies that screened donors for all major types of TTIs. According to a WHO report, the prevalence of malaria was 0.1%, 1.78% and 0.81% for the years 2011, 2012 and 2013 in Pakistan.Citation44
Coinfections
Co-infectivity has also been reported in many studies. Arshad et al. found 0.35% (n=58) of donors with coinfections.Citation24 Another study from Islamabad reported a very low frequency of co-infections, 0.039% (n=12).Citation32 Zameer et al. found 0.29% (n=29, 28 donors had 2 TTIs while 1 donor had 3 TTIs) cases of coinfections. The highest number of coinfections (n=13) were HCV and syphilis followed by HCV and HBV (n=12).Citation26 One study from Lahore documented 0.38% (n=71) of donors with coinfections; HCV and syphilis co-infectivity was the highest (n=46) followed by HBV and HCV coinfections (n= 22).Citation28 Another author reported a total co-infectivity of 0.09% (n=103) with the highest co-infectivity seen with HBV and HCV in 94 cases.Citation13 Sial et al. reported coinfections in 0.135% donors (n=400) with HCV and syphilis having the highest co-infectivity in this study, 0.09% (n=27).Citation20 Rauf et al. reported 15 cases (0.22%) of HBV and HCV coinfections as the highest co-infectivity.Citation35 Alarmingly, they reported 11 donors (0.16%) who were concomitantly reactive for HBV, HCV, HIV and syphilis.Citation35 Three concomitant TTIs were also reported in two donors by another author.Citation13
Discussion
Pakistan has a poorly regulated, demand-driven fragmented BT system based on more than 1800 public hospital-based or free-standing private blood banks (BBs).Citation42,Citation43 These units provide all services of the vein-to-vein transfusion chain, ranging from typing, cross-matching, donor screening, collection, storage and distribution of blood to the patients. There is inadequate initial screening of donors for high-risk behaviors due to inadequate training of BB staff. Limited knowledge of donors about their health and medical problems also increases the risk of TTIs. Pakistan lacks a universal quality-assured serological screening process. In many blood banks, poor quality, cheap and rapid manual methods are being used for quick screening along with poor laboratory practices.Citation44 This can lead to a significant probability of missing an infection in the donor population with a multifold increased risk of transmission to transfusion recipients. Rates of voluntary donations are meager accounting for less than 13% of all donations. This is due to a lack of infrastructure, poor educational status and cultural beliefs of the general population.Citation45
According to a global status report (2016) by the WHO on blood safety and availability, the proportion of donations that screened TTIs in Pakistan were 100% for HIV, HBV, HCV and only 66% for syphilis and malaria.Citation42 The seroprevalence of HBV in blood donors varied from 1.55% to 3.76%, HCV from 2.55% to 7.23%, HIV from 0 0.01% to 0.04% and syphilis varied from 0.59% to 1.16% %.Citation42–Citation47
Our review showed a cumulative frequency of 2.04% (n=16,203) for HBV and 2.44% (n=17,660) for HCV among blood donors. Transmission of HBV and HCV through blood transfusion is a significant concern. Pakistan falls in a low-intermediate prevalence area for HBV, with an estimated carrier rate of 2–4% and an estimated 5 million individuals with chronic HBV infection. It has the second-largest number of HCV infected population worldwide.Citation48 According to one estimate, almost 10 million people in the country are infected with chronic HCV, that being roughly 5.9% of the total population. There is a high prevalence of HCV (48.67%) in chronically transfusion-dependent thalassemia and hemophilia patients.Citation49 High prevalence of HBV and HCV in donors may be contributing to this high prevalence in the general population and among chronic transfusion recipients. WHO recommends donor screening of HCV through anti-HCV antibodies by rapid diagnostic immunoassay in resource-limited countries or a combination of HCV antigen-antibody immunoassay (EIA/CLIA). Samples reactive by CLIA/EIA should be further confirmed by nucleic acid amplification technology (NAT), which is the gold standard for HCV diagnosis. For HBV, blood donors should be screened using a highly sensitive and specific HBsAg immunoassay (EIA/CLIA). Routine screening for anti-HBc for transfusion purposes is not needed.Citation50
The concern of HIV spread is growing in the public health community of Pakistan. There are recent reports of isolated low-scale epidemics of HIV in rural areas.Citation51 Pakistan is one of the countries located in the WHO Eastern Mediterranean Region and HIV infections are spreading at an alarming rate in this region.Citation51 WHO considers the current HIV epidemic in Pakistan to be a concentrated one. The total prevalence of HIV is still less than 1% of the total adult population in Pakistan.Citation51 According to the UNAIDS 2018 report, there is an alarming increase of 57% in new HIV cases and a 369% increase in AIDS-related deaths since 2010.Citation52 In 2018, only 14% of people living with HIV in Pakistan knew their HIV status.Citation52 Given the lack of a centralized hemovigilance system, it is challenging to estimate a real-time risk of HIV infection in Pakistan due to BT. According to one article, the spread of HIV through blood transfusion in Pakistan was about 11.73%.Citation53 Seroconversion to HIV-positive could be as high as 98% after exposure to HIV infected blood products.Citation54 In developed countries such as the United States, the risk of contracting an HIV infection through transfusion is expected to be one in 1.5 million donations.Citation55 The rate of HIV infectivity with packed red blood cells is inversely related to its storage time. HIV infected blood products which are stored for less than 8 days are 96% infectious. Infectivity drops to 50% when stored for more than 3 weeks.Citation54 There is a steady increase in the prevalence of HIV in the donor population. On the other hand, there is a lack of standardized HIV donor screening. The cumulative frequency of HIV in our study was 0.038% (n=497).
An estimated 12 million new cases of syphilis are diagnosed each year globally, with an estimated global prevalence of 0.5% in men aged 15–49 years.Citation56,Citation57 In our review, the cumulative frequency of syphilis in the donor population was 1.1% (n=6974). Treponema pallidum is a relatively fragile bacterium which is sensitive to cold temperature and the risk of its transmission through BT is minimal if blood is stored below 20º centigrade for longer than 72 hours.Citation58,Citation59 However, in Pakistan, most transfusions are stored for less than 72 hours due to arrangement by family members on a needed basis. WHO recommends testing with Venereal Disease Research Laboratory (VDRL), rapid plasma reagin (RPR) and cold storage techniques to minimize the risk of syphilis through transfusion.Citation60
Malaria is endemic in Pakistan with 3.5 million cases every year.Citation61 In our review, we noticed a lack of universal screening of blood for malaria. According to the Federal Drug Administration (FDA) and the American Association of Blood Bank (AABB), people with malaria cannot donate blood for 3 years after becoming asymptomatic.Citation62,Citation63 Rate of malaria transmission in endemic countries such as Pakistan may be as high as 50 cases per million blood donations.Citation64 In our review, the cumulative frequency of malaria in blood donors was 0.11% (n=368). This seems to be an underestimation of the overall risk of transfusion-transmitted malaria due to a lack of uniform widespread testing protocols. The peripheral smear is the most widely used diagnostic test in Pakistan, but it is highly dependent on user technical skills and knowledge.Citation64 Asymptomatic blood donors have low levels of parasite count along with the low density of parasite in the blood which can lead to difficulty in the detection of the parasite.Citation65 The most effective way of screening donors is to take a proper history for any underlying disease, medications use, fever and high-risk exposure.Citation8 Donor criteria should be developed locally and implemented to exclude potentially high-risk individuals.
According to the WHO, the number of total blood donations and VNRDs decrease steeply from high-income countries to low-income countries.Citation66 Proportions of VNRDs in 2013 in high-income, upper-middle-income, lower-middle-income and low-income countries were 95%, 79%, 71% and 63%, respectively.Citation42 Therefore, there is limited access to safe blood, especially in low-income countries. WHO recommends blood donations to be collected mainly from VNRDs because of their lowest prevalence of TTIs.Citation66 Replacement/family donors (RDs) and paid (professional) or remunerated donors are less desirable than other types. With the aim of sufficient and sustainable blood supply, WHO envisions 100% of blood donations to be collected from VNRDs worldwide.Citation67 Contrarily, almost 85–90% of blood donations came from RDs in Pakistan in 2011–2013.Citation42 Despite efforts to decrease RDs and increase VNRDs, replacement donors accounted for 87% to 99.98% of all donors according to these studies.Citation11,Citation13,Citation19,Citation20,Citation22,Citation24,Citation28,Citation29,Citation33 According to a global status report of the WHO, less than 25% of Pakistan’s blood donations are by VNRDs. Development of the VNRDs-based collection system as recommended by the WHO is an important measure to ensure the availability of safe blood products.Citation42 In Pakistan, there is a need for donor education and registration campaigns for the development of voluntary donor base, registration of family RDs for future voluntary donations and development of a network of BBs that rely on voluntary donations only.
Establishment of a separate qualification and training program of transfusion medicine in Pakistan can help implement standardization of quality metrics and assurance of safe blood supply. It provides a skilled workforce that can implement good evidence-based transfusion practices.Citation68 WHO proposes the development of programs for integration of transfusion medicine education into the existing structure of medicine, nursing and laboratory technology institutions.Citation69
Hemovigilance is a concept of surveillance of the whole vein-to-vein transfusion chain. It includes follow-ups with transfusion recipients, collection and assessment of the data on unexpected or undesirable events related to the therapeutic use of blood products. It utilizes this information to prevent the occurrence or recurrence of such incidents in the future.Citation70 In developing countries, it can help to assess the risk of TTIs. There are challenges to achieve effective hemovigilance in Pakistan due to limited availability of TTIs epidemiology data, lack of a centralized reporting system for adverse events and follow-up services for donors and recipients. There is suboptimal donor testing which leads to missing the infections due to high false-negative results.Citation71,Citation72 Moreover, there is no mechanism for identifying the rate of transfusion-related infections in the general population. During our review, we were unable to find any large-scale surveillance and reporting data on TTIs.
The government of Pakistan has much more to do, but in 2010, they launched a series of initiatives, per the WHO guidelines, for an overall improvement of the BT system through national safe blood transfusion programs (SBTP). This led to the formulation of a national blood policy and strategic framework for the strengthening of the organizational structure of the transfusion system in Pakistan. Through the USAID, the WHO supplied blood-screening kits worth 84 million dollars.Citation73 There are considerable improvements regarding the development of regional public blood centers with accreditation standards, improved data collection and implementation of universal screening guidelines. There are training and educational opportunities devoted to improving the quality, data collection and evidence-based blood use. But these efforts are mainly centered in major urban institutions with limited outreach to rural areas where the problem is severe and needs urgent intervention and attention.
This review has limitations because we based the review on the data from studies focused on localized geographical locations due to lack of availability of large scale-multicenter structured data. We relied on data sources to find the most recent and consistent information that could lead to inherent reporting bias for studies and their ability to be published. Most of the studies are of variable quality and scope. The donor populations also vary among studies and comparison of the population among studies is difficult due to the inconsistency of information and data provided. The screening methods differ among studies and there is variable sensitivity and specificity of the methods. There is a risk of missing or omitting some publications due to reviewer bias. The use of grey literature like the WHO and local reports is also based on limited data and rely on information reported by the government agencies. Our study represents the best possible overview of the underlying problem with limitations. We recommend large multi-centered studies involving rural centers in Pakistan.
Conclusion
Our study shows the cumulative frequency of HBV of 2.04%, HCV of 2.44%, HIV of 0.038%, syphilis of 1.1% and malaria of 0.011% among screened donors. There is limited screening of syphilis (38%) and malaria (46%) in the donor population. The rate of co-infections is 0.35%, with HCV and syphilis as the most frequent co-infections. The blood donors in Pakistan are mostly RDs and the rate of VNRDs is low (0.10%-13%). There is a lack of widespread standardized testing and follow-up of donors who test positive on initial screening. Our findings highlight the need for promoting a culture of voluntary blood donations by creating awareness among the public to mobilize and motivate through media, professional medical societies, political factors, local governmental and non-governmental organizations. Moreover, our data endorse the need for a universal quality-assured donor screening, development of a hemovigilance system, uniform standard operating procedures and a trained workforce for BBs. There is a need for large prospective multi-center epidemiological studies in the country for a better understanding of the burden of TTIs, impact of testing procedures and influence of mitigation strategies such as hemovigilance system and TTI tracking networks.
Disclosure
The authors declare no conflicts of interest with this manuscript.
References
- WHO model lists of essential medicines. World Health Organization; 2019 Available from: https://www.who.int/medicines/publications/essentialmedicines/en. Accessed 816, 2020.
- Saqlain N, Ahmed N, Ahmed A, Hareem S. Blood donation; knowledge, attitude and beliefs of the female attendants. Professional Med J. 2017;24(12):1806–1811. doi:10.17957/TPMJ/17.4003
- Pakistan SBTPGo. National blood banks data collection report 2018. Available from: https://www.sbtp.gov.pk/wp-content/uploads/2019/10/National-Data-Collection-Report-2018.pdf. Accessed 816, 2020.
- Farhat M, Yasmeen A, Ahmad A. An overview of hepatitis B and C in Pakistan. Int J Microbiol Allied Sci. 2014;1:98–102.
- Zaheer HA, Waheed U, Nasir K Safe blood transfusion programme annual report 2019 2019. Available from: https://www.sbtp.gov.pk/wp-content/uploads/2020/02/Final-Report-2019.pdf. Accessed 816, 2020.
- Muazzam A, Javed S. Predictors of caregiver’s burden: interplay of physical and emotional health and perceived hope in children with thalassemia and hemophilia. Pak J Soci Clin Psychol. 2013;11(2):36.
- Pasha O, Saleem S, Ali S, et al. Maternal and newborn outcomes in Pakistan compared to other low and middle income countries in the Global Network’s Maternal Newborn Health Registry: an active, community-based, pregnancy surveillance mechanism. Reprod Health. 2015;12(S2):S15. doi:10.1186/1742-4755-12-S2-S1526062610
- WHO. Universal access to safe blood transfusion 2007. Available from: https://www.who.int/bloodsafety/StrategicPlan2008-2015AccessSafeBloodTransfusion.pdf. Accessed 816, 2020.
- Shah SM, Khattak IU, Ali A, Tariq M. Seropositivity for hepatitis B and C in voluntary blood donors. J Ayub Med Coll Abbottabad. 2010;22(3):149–151.22338442
- Ansari SH, Shamsi TS, Khan MT, et al. Seropositivity of Hepatitis C, Hepatitis B and HIV in chronically transfused ββ-thalassaemia major patients. J Coll Physicians Surg Pak. 2012;22(9):610–611.22980623
- Waheed U, Khan H, Satti HS, Ansari MA, Malik MA, Zaheer HA. Prevalence of transfusion transmitted infections among blood donors of a teaching hospital in Islamabad. Ann Pak Inst Med Sci. 2012;8(4):236–239.
- Attaullah S, Khan S, Khan J. Trend of transfusion transmitted infections frequency in blood donors: provide a road map for its prevention and control. J Transl Med. 2012;10(1):20. doi:10.1186/1479-5876-10-2022293125
- Irfan SM, Uddin J, Zaheer HA, Sultan S, Baig A. Trends in transfusion transmitted infections among replacement blood donors in Karachi, Pakistan. Turk J Hematol. 2013;30(2):163. doi:10.4274/Tjh.2012.0132
- Tunio SA, Bano S, Laghari ZA, Ali W, Shamim H, Afreen U. Seroprevalence of hepatitis B and hepatitis C among blood donors in Hyderabad, Pakistan. Gomal J Med Sci. 2013;11(2).
- Tufail S, Babar F, Ikram N, Raza M, Abdul-Shakoor H. Blood donors’ deferral-causes. J Rawalpindi Med Coll. 2013;17(1):119–121.
- Sulehri MA, Hussain SJ, Mehmood Q, Javed SH. Incidence of false sero-negative blood donor cases for Hepatitis-C in public and private hospitals of city district Faisalabad. Ann Punjab Med Coll. 2013;7(1):10–16.
- Chaudhry MA, Malik JR, Ashraf MZ. Seropositivity of hepatitis B and C in blood donors at CMH Lahore, Pakistan. Ann Punjab Med Coll. 2013;7(1):1–5.
- Ghafoor B, Hussain M, Leghari AR, Mehwish A, Zulfiqar S, Mustafa G. Major transfusion-transmissible infections among blood donors in Rahim Yar Khan, a district of Southern Punjab, Pakistan. Isra Med J. 2016;8(4).
- Waheed U, Hasan SI, Wazeer A, Zaheer HA. The status of blood safety in Islamabad, Pakistan. Ann PIMS. 2016;12(4):209.
- Sial GR, Khan S, Shahid SU, Bhatti S, Farooq F. Prevalence of transfusion transmitted infections in asymptomatic blood donors: is Syphilis alarming? Biomedica. 2016;32(1).
- Raza N. Revisiting reactive blood donor demographics-A single center experience. J Liaquat Univ Med Health Sci. 2016;15:208–212.
- Niazi SK, Mahmood A, Alam M, Ghani E. Seroprevalence of transfusion transmissible infections in blood donors: a three-year experience. Pak Armed Forces Med J. 2016;66(2):190–193.
- Nadeem A, Salamat N, Iqbal N, et al. Demographic features of donors and causes of blood donor deferral at Armed Forces Institute of Transfusion, Rawalpindi. Pak Armed Forces Med J. 2016;66(6):898–902.
- Arshad A, Borhany M, Anwar N, et al. Prevalence of transfusion transmissible infections in blood donors of Pakistan. BMC Hematol. 2016;16(1):27. doi:10.1186/s12878-016-0068-227891232
- Memon FA, Ujjan ID, Memon AI, Shaikh AR, Rao AR, Naz A. Seroprevalence of transfusion transmitted infections among different blood group donors at Blood Bank LUMHS, Hyderabad. Pak J Med Sci. 2017;33(2):443. doi:10.12669/pjms.332.1169128523053
- Zameer M, Shahzad F, Khan FS, Ali H, Saeed U, Farooq M. Transfusion transmissible infections among healthy blood donors at blood bank from Children’s Hospital & Institute of Child Health Lahore. Pak Armed Forces Med J. 2017;1(1):131.
- Maeesa W, Muhammad U, Khansa Q, Muhammad R, Iram N. Seroprevalence of hepatitis C among the apparently healthy blood donors of Karachi. Baqai J Health Sci. 2017;20(1):19–24.
- Saeed M, Hussain S, Rasheed F, Ahmad M, Arif M, Rahmani MT. Silent killers: transfusion transmissible infections-TTI, among asymptomatic population of Pakistan. J Pak Med Assoc. 2017;67(3):369–374.28303984
- Sultan S, Nasir MI, Rafiq S, Baig MA, Akbani S, Irfan SM. Multiplex real-time RT-PCR assay for transfusion transmitted viruses in sero-negative allogeneic blood donors: an experience from Southern Pakistan. Malays J Pathol. 2017;39(2):149.28866696
- Rehman N, Orakzai MB, Hayat A, et al. Prevalence of Hepatitis C virus and its risk factors in blood donors in district Peshawar. Pak J Pharm Sci. 2018;31(1):83–87.29348088
- Raza N, Qureshi H, Qureshi A. Reactive blood donor notification; their responses and perceptions: experience from southern Pakistan. J Ayub Med Coll Abbottabad. 2018;30(3):351–355.30465364
- Awan SA, Junaid A, Sheikh S. Transfusion transmissible infections: maximizing donor surveillance. Cureus. 2018;10(12).
- Naz A, Mukry SN, Naseer I, Shamsi TS. Evaluation of efficacy of serological methods for detection of HCV infection in blood donors: A single centre experience. Pak J Med Sci. 2018;34(5):1204.30344577
- Abdullah S, Zahoor S, Rao MA, et al. Seroprevalence of hepatitis B virus in blood donors at a large teaching hospital of Pakistan: a potential health policy concern. J Appl Hematol. 2019;10(1):29. doi:10.4103/joah.joah_10_19
- Rauf R, Cheema A. Potential risk of transfusion-transmissible infections among blood donors in district Faisalabad of Pakistan. Clin Med (Northfield Il). 2019;19(Suppl 3):27. doi:10.7861/clinmedicine.19-3-s27
- Masood I, Usman Waheed MA, Saeed M, et al. Molecular epidemiology of hepatitis B virus genotypes in blood donors in Islamabad, Pakistan. J Lab Physicians. 2019;11(3):240. doi:10.4103/JLP.JLP_150_1831579261
- Ali N, Ahmed J, Ali N, Jehan F, Saleem S. Transfusion transmitted malaria in three major blood banks of Peshawar, Pakistan. Afr J Biotechnol. 2010;9(33).
- Usman M, Mahmood H. Frequency of malarial parasite infection in healthy blood donors of Pakistan. Baqai J Health Sci. 2015;18(1).
- Ghani E, Rathore MA, Khan SA. Trends in human immunodeficiency virus seroprevalence in blood donors in northern Pakistan. Public Health. 2016;131:71–74. doi:10.1016/j.puhe.2015.10.010
- Kousar R, Saqlain N, Ahmed N. Malarial parasite screening in blood donors; experience at the Children’s Hospital & Institute of Child Health, Lahore. Pak Pediatr J. 2016;40(3):143–147.
- Zahoor S, Hameed S, Iqbal W, ur Rehman H, ur Rehman N, Jaral J. Seroprevalence of Syphilis in healthy blood donors of Lahore during year 2016 and 2017; An upcoming problem for Pakistan. Professional Med J. 2020;27(01):138–142. doi:10.29309/TPMJ/2019.27.01.3823
- Global status report on blood safety and availability 2016. Global database on blood safety. World Health Organization Available from: https://apps.who.int/iris/bitstream/handle/10665/254987/9789241565431-eng.pdf?sequence=1. Accessed 816, 2020.
- Zaheer HA, Waheed U. Blood safety system reforms in Pakistan. Blood Transfus. 2014;12(4):452–457.24960645
- Waheed U, Abdella YE, Saba NE, et al. Evaluation of screening effectiveness of hepatitis B surface antigen and anti-HCV rapid test kits in Pakistan. J Lab Physicians. 2019;11(4):369–372. doi:10.4103/JLP.JLP_172_1931929706
- Mumtaz Z, Bowen S, Mumtaz R. Meanings of blood, bleeding and blood donations in Pakistan: implications for national vs global safe blood supply policies. Health Policy Plan. 2012;27(2):147–155. doi:10.1093/heapol/czr01621372061
- Waheed U, Arshad M, Usman J, Farooq A, Wazeer A, Zaheer HA. Surveillance of HIV infection in blood donors in Pakistan: a systematic review. Pak Armed Forces Med J. 2017;67(5):860–867.
- Jefferies M, Rauff B, Rashid H, Lam T, Rafiq S. Update on global epidemiology of viral hepatitis and preventive strategies. World J Clin Cases. 2018;6(13):589–599. doi:10.12998/wjcc.v6.i13.58930430114
- Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi H. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol. 2014;61(1):S45–S57. doi:10.1016/j.jhep.2014.07.02725086286
- Waheed Y, Shafi T, Safi SZ, Qadri I. Hepatitis C virus in Pakistan: a systematic review of prevalence, genotypes and risk factors. World J Gastroenterol. 2009;15(45):5647. doi:10.3748/wjg.15.564719960560
- WHO. Screening donated blood for transfusion transmissible infections 2010. Available from: https://www.who.int/bloodsafety/ScreeningDonatedBloodforTransfusion.pdf. Accessed 816, 2020.
- WHO. HIV cases–Pakistan; 7 2019 Available from: https://www.who.int/csr/don/03-july-2019-hiv-cases-pakistan/en/. Accessed 816, 2020.
- UNAIDS. Country factsheets PAKISTAN 2018. Available from: https://www.unaids.org/en/regionscountries/countries/pakistan. Accessed 816, 2020.
- Bhurgri Y. HIV/AIDS in Pakistan. J Pak Med Assoc. 2006;56(1):1.16454124
- Donegan E, Lee H, Operskalski E, et al. Transfusion transmission of retroviruses: human T‐lymphotropic virus types I and II compared with human immunodeficiency virus type 1. Transfusion. 1994;34(6):478–483. doi:10.1046/j.1537-2995.1994.34694295061.x8023388
- Zou S, Dorsey KA, Notari EP, et al. Prevalence, incidence, and residual risk of human immunodeficiency virus and hepatitis C virus infections among United States blood donors since the introduction of nucleic acid testing. Transfusion. 2010;50(7):1495–1504. doi:10.1111/j.1537-2995.2010.02622.x20345570
- Newman L, Rowley J, Hoorn SV, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS One. 2015;10(12):e0143304. doi:10.1371/journal.pone.014330426646541
- Tagny CT. Syphilis and blood safety in developing countries In: Sato NS, editor. Syphilis - Recognition, Description and Diagnosis. InTech; 2011 Available from: http://www.intechopen.com/books/syphilis-recognition-description-and-diagnosis/syphilis-and-blood-safety-indeveloping-countries. Accessed 816, 2020.
- Orton S. Syphilis and blood donors: what we know, what we do not know, and what we need to know. Transfus Med Rev. 2001;15(4):282–291. doi:10.1053/tm.2001.2695611668435
- Kaur G, Kaur P. Syphilis testing in blood donors: an update. Blood Transfus. 2015;13(2):197–204.25545876
- Montoya PJ, Lukehart SA, Brentlinger PE, et al. Comparison of the diagnostic accuracy of a rapid immunochromatographic test and the rapid plasma reagin test for antenatal syphilis screening in Mozambique. Bull World Health Organ. 2006;84(2):97–104. doi:10.2471/BLT.04.01866316501726
- Malaria strategic plan, Pakistan – 2015–20. Directorate of Malaria Control Available from: http://dmc.gov.pk/index.php?option=com_content&view=article&id=84&Itemid=84. Accessed 816, 2020.
- Mungai M, Tegtmeier G, Chamberland M, Parise M. Transfusion-transmitted malaria in the United States from 1963 through 1999. N Engl J Med. 2001;344(26):1973–1978. doi:10.1056/NEJM20010628344260311430326
- Zoon K. Recommendations for Deferral of Donors for Malaria Risk: Letter to All Registered Blood Establishments. Rockville, Maryland: US Department of Health and Human Services. Food and drug administration; 1994.
- Moiz B. Prevention of transfusion transmitted malaria in an endemic area—a challenge for blood banks. Infect Dis J Pak. 2004;13(4):96–98.
- Choudhury N, Jolly J, Mahajan R, Ganguly N, Dubey M, Agnihotri S. Malaria screening to prevent transmission by transfusion: an evaluation of techniques. Med Lab Sci. 1991;48(3):206–211.1787779
- Blood safety and availability. World Health Organization Available from: https://www.who.int/en/news-room/fact-sheets/detail/blood-safety-and-availability. Accessed 816, 2020.
- Towards 100% voluntary blood donation, a global framework for action. World Health Organization Available from: https://www.who.int/bloodsafety/publications/9789241599696/en/. Accessed 816, 2020.
- Sibinga CTS, Oladejo MA, Adejumo OH, et al. A global survey of clinicians’ awareness, accessibility, utilization of e-continuous education, and quality of clinical blood use: policy considerations. Int J Clin Transfus Med. 2017;5:69. doi:10.2147/IJCTM.S136047
- Global collaboration for blood safety 2004. World Health Organization Available from: https://www.who.int/bloodsafety/GCBS_Report_NOV_2004.pdf?ua=1. Accessed 816, 2020.
- Faber JC. Haemovigilance procedure in transfusion medicine. Hematol J. 2004;5(Suppl 3):S74–S82. doi:10.1038/sj.thj.620042715190283
- Naz S, Umair MM, Hameed A. Evolution of blood banks of Islamabad in ten years (2006–2016). Ann PIMS. 2018;14(2):127–134.
- Luby S, Khanani R, Zia M, et al. Evaluation of blood bank practices in Karachi, Pakistan, and the government’s response. J Pak Med Assoc. 2006;56(1 Suppl 1):S25–S30.
- Blood safety in Pakistan 2018. World Health Organization Available from: http://www.emro.who.int/pak/programmes/blood-safety.html. Accessed 816, 2020.
