Abstract
Introduction
Gynecology and obstetrics are among the specialties where blood transfusion is most practiced. This situation requires the use of good transfusion practices. The objective of this study was to assess the quality of transfusion practice in the Gynecology and Obstetrics Department of the University Hospital of Kinshasa (UHK).
Methods
This is a prospective, evaluative and descriptive study performed at the Department of Gyneco-Obstetrics of the University Hospital of Kinshasa from February 25 to June 25, 2020; which dealt with patients who received at least one blood transfusion.
Results
About 498 patients, 54 patients were transfused and their average age was 36.4 years, with the extremes of 14 and 60 years, the transfusion rate was 10.8%. Most of patients (n=36: 2/3) were transfused during weekend days, sachets were used as delivery materials of blood product in 57.4% of cases (n = 31). Among the prescribers of blood products, 70.4% were nurses. All transfusions were carried out in type-specific and cross-matched Rh. All the transfused patients were not aware of the disadvantages of transfusion. Compatibility tests at the patient’s bedside were not performed in 61.1% of cases and the concordance control between the patient and the blood component to be transfused was not performed in 70.4% of cases. Close monitoring of blood transfusion in the first ten minutes was not performed in 59.3% of cases.
Conclusion
Transfusion encounters real practical problems in the gyneco-obstetrical environment of countries with limited resources. However, an assessment and multidisciplinary collaboration would be necessary to improve transfusion practice in medical field.
Introduction
The practice of transfusion is common in Gynecological and Obstetrical specialties, because of a high frequency of complications such as: disorders of parturition, incomplete abortions, cases of placenta accreta and rupture of the uterus, caesarean section, close-term anemia, ruptured ectopic pregnancy, evacuation of hydatid moles and cancer (uterus, breast, ovary).Citation1–3 As a result, blood transfusion remains a daily concern in these two specialties.Citation4 In addition, the transfusion and post-transfusion risk occurred requires the use of good transfusion practices.Citation5 Unfortunately, the act of transfusion is often marred by non-conformities confirmed by several studies carried out in SSA. These studies revealed non-conformities in relation to bedside compatibility tests (72.6%),Citation2,Citation6 the concordance control of the blood group mentioned on the patient’s file with the one mentioned on the blood product (15.5%)Citation1,Citation2 and close monitoring of blood transfusion during the first ten minutes (88.3%).Citation2
Then, to secure the act of transfusion in countries with limited resources, the World Health Organization (WHO) recommended in 2016 to strengthen the management of the quality system throughout the transfusion chain and to carry out training programs and performing internal and external assessment of quality systems.Citation7,Citation8 To carry out these assessments, collaboration between clinicians and biologists is necessary, but also strategies to reduce the inappropriate use of blood and blood components in all specialties.Citation8 These strategies include guidelines, monitoring of transfusion practice and self-assessment by clinicians.Citation3 The objective of this study was to assess the quality of transfusion practices in the Gynecology and Obstetrics Departments of the UHK.
Methods
This is a prospective, evaluative and descriptive study performed over a period of 4 months, from February 25 to June 25, 2020 in the Gyneco-Obstetrics Department of the University Hospital of Kinshasa. The study population is composed of patients admitted to the Gyneco-Obstetrics Department of the UHK and having been transfused at least once during the study period.
Sampling
An exhaustive and reasoned sampling of patients transfused during the study period was carried out (n=54).
Variables of Interest
The different variables of interest were obtained by direct observation of transfusion performed by the health agents who practiced transfusion on the one hand, and by questioning the patients or their members on the other hand.
The parameters of interest were as follows: age, profession, marital status, days of transfusion, materials for transporting blood components, information on the advantages and disadvantages of blood transfusion before transfusion act, the practitioners of the blood transfusion, the concordance control between the patient and the blood component to be transfused, the type of transfusion, the compatibility test at the patient’s bedside, monitoring of the blood transfusion in the first 10 minutes and the acute transfusion reactions.
Operational Definitions
Critical assessment was defined as a systematic and critical analysis of the quality of medical care by comparing procedures or services with the standard references, in order to make corrections.
Appropriate blood component was a blood component transfused solely to treat a condition leading to significant morbidity and mortality that cannot be prevented or effectively managed by other means.Citation5
Statistical Analyzes
Categorical data were presented by their numbers (n) and their percentages (proportions). Associations between categorial variables were sought by Pearson’s Chi-square test.
The normality of the quantitative variables was assessed by the Kolmogorov–Smirnov test. Quantitative variables were characterized by the mean ± standard deviation (X ± SD) or the median with its interquartile (Med (EIQ)). The average of the ages with normal distribution was compared by Student’s t-test between two groups but also with the analysis of variances (ANOVA) between ≥ 3 groups.
In univariate (bivariate) analysis, the association between two continuous or quantitative variables was determined by Pearson’s r coefficient in case of normal distribution but also by Spearman’s rho (ρ) coefficient in case of abnormal distribution.
The statistical significance threshold was set at p < 0.05.
All statistical analyzes were performed with SPSS 23 software.
Results
Transfusion Rate
Upon a total of 498 patients admitted to the Gynecology and Obstetrics Departments, 54 patients received at least one blood transfusion, about 10.8%.
Age of Patients
sums up the central tendency, the dispersion, the quartile and the retrospective distribution ages of the study population. In fact, the range of age extremes (minimum = 14 years and maximum = 60 years) was spread out and categorized according to the chronobiology of the following population: adolescent-young adult with age <34 years versus advancing into adulthood with age ≥34 years. Most of our patients (51.9%) were between 14 and 33 years old ().
Table 1 Distribution of Data Related to the Compliance Parameters of the Transfusion Rules
Table 2 Distribution of the Patients Related to the Age of the Study Population
Patient Profession
Among all patients 32, 8.1, 2.1, 2.3, 1.2 and 2 had reported the professions of housewife, student/pupil, demographer, policewoman, doctor, seamstress, trader, magistrate and nurse: most of the patients (close to 60% and 2/3) being less educated housewives than the other professions.
Transfusion Days
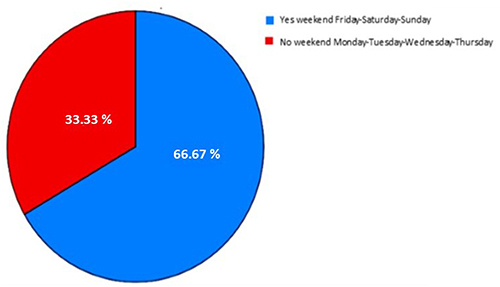
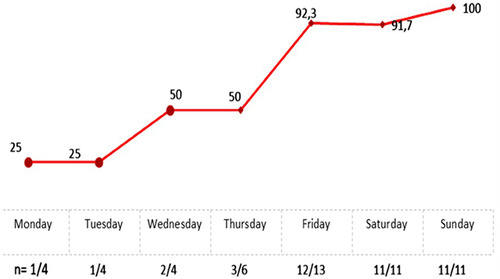
The days of blood transfusions characterized the frequencies of the study population: most of patients (n=36: 2/3) were transfused during weekend days (Friday-Saturday-Sunday) against 18 patients transfused during non-weekend days ().
Indicator for the Critical Assessment of Transfusion Practices
Materials for Transporting Blood Products
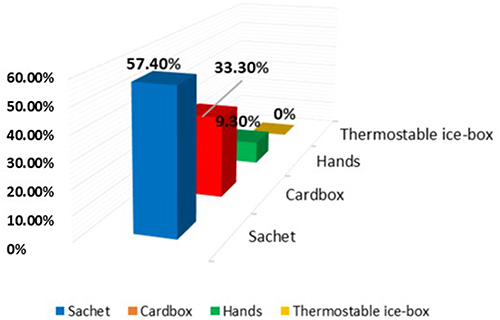
Materials for transporting blood products were in the form of a sachet in 57.4% of cases (n = 31), in the form of a cardboard box in 33.3% of cases (n = 18), by the hands of family members in 9.3% of cases (n=5) and with a thermo stable cooler in 0.0% of cases (n=0) ().
Haemorrhage was the main clinical indication for blood transfusions in the present study. This was dominated by postpartum haemorrhage (42.6%) of cases (n=23), followed by post oncological surgery haemorrhage (37.0%) of cases (n=20), and pre-intrapartum haemorrhage (20.4%) of cases (n=11).
Practitioners of the Blood Transfusion
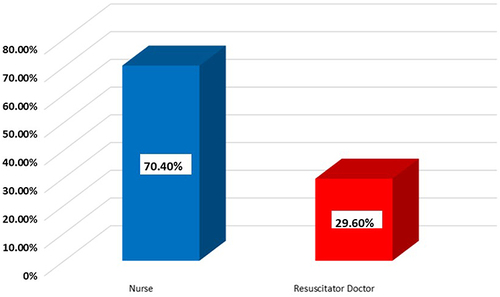
Among practitioners of Blood Transfusion, 70.4% of nurses (n=38) were comparable to 29.6% of resuscitator physicians (n=16) ().
Type of Transfusion
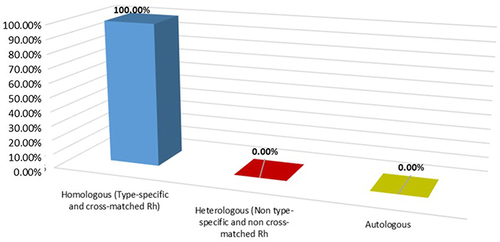
Homologous transfusion (type-specific and cross-matched Rh) as type of transfusion was performed in 100.0% of patients (n=54) ().
Observance of Haemovigilance Rules
The parameters of compliance with the rules of blood transfusion were summarized in . This consisted of information on the advantages and disadvantages of blood transfusion to patients before the transfusion procedure, the control of concordance between the patient and the blood component unit to be transfused, compatibility testing at the patient’s bedside, monitoring of blood transfusion in the first 10 minutes and adverse effects occurring during transfusions.
Univariate Analysis for the Adverse Effects as Predictor Occurring During Transfusions
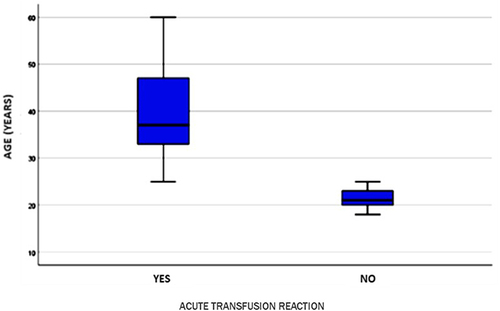
Age and Acute Transfusion Reactions
All patients with the age advancement presented an acute transfusion reaction (average age ≥ 34 years, 100% n=26). Patients with an acute transfusion reaction were statistically older (median age = 41.2 ± 11.2 years; P < 0.0001) than their partners without a minor or major acute transfusion reaction (average age = 21.6 ± 3.6 years) ().
Transfusion Days and Acute Transfusion Reaction
There was a highly significant association (P<0.001) between the rates of acute transfusion reaction and the days when blood transfusions were performed during the week in the form of an exponential curve. Then, the acute transfusion reaction rate was more frequent during weekend days (Friday-Saturday-Sunday) (94.4% n=34/36 RR 2.4 95% CI 1.4–4.4; P < 0.001) than during non-weekend working days (38.9% n=4/18) (). The most prevalent reaction was hyperthermia reaction ().
Table 3 Days, Months and Reactions Post Transfusion
Discussion
This is the first study that assessed practices of transfusion in a gyneco-obstetrics environment at the UHK.
Transfusion Rate
In the current study, transfusion was performed in 10.8% of patients admitted during the study period. This rate is more or less comparable to those found by ChowdhuryCitation9 in 2016 in India and by ZamanéCitation2 in Burkina Faso in 2014, which were respectively 9.2% and 11.1%. But it is higher than the rate indicated by Yung-Taek Ouh (1.9%)Citation10 in Korea in 2014 and by Matthew Cauldwell (0.3%)Citation11 in the United Kingdom in 2017 in patients transfused in Gyneco-Obstetrical environment.
The relatively high rate observed in this study testifies an increased transfusion activity in the Gyneco-Obstetrics Department of the UHK. Indeed, the low socio-economic standard of patients (74.1%) constitutes an impasse to the early diagnosis and management of pathologies with a high risk of bleeding. In addition, pathophysiological aspects are generally not taken into account when prescribing BT: transfusion decisions are often made by non-trained practitioners and are based on limited and often low quality evidence. In addition, there is no evidence practice about any level of anemia.Citation12 It is also important not to consider blood transfusion (transfusion of allogeneic red blood cells, platelet concentrates and plasma units) especially for patients with cancer, as a standard therapeutic arsenal used in the context of surgical and non-surgical treatment.Citation13
This rate is related to the organization of the night work services in GO/UHK during the weekend. At weekend, the number of doctors is less, supervisors on call are not on site most of the time, and consequently decisions are made without supervisors’ opinion. In addition, patients are admitted urgently at weekend (81.5%) in an unstable hemodynamic state leading to an urgent transfusion. All these facts justify the increased rate of BT during the three days of the weekend at the GO/UHK.
In intermediate- and high-resource countries, some reports indicate improvements in transfusion practices (mainly with respect to the hemoglobin thresholds at transfused patients).Citation3,Citation5,Citation14 These improvements are related to: the adoption of the restrictive strategy rather than the liberal strategy;Citation12 the personalization of the blood management (PBM); the mobilization of the means for training, the organization of mass voluntary blood donation campaigns and the organization of quality assessment.Citation15
Age of Patients
The average age of our patients was around 33.5 years, this result is comparable to that reported in other studies performed in some African countriesCitation1,Citation4,Citation6,Citation11,Citation16 but further low than that of patients transfused in the departments of Gynecology and Obstetrics of developed countries.Citation10,Citation17
Transport Equipment
The LBC transport equipment in the current study did not meet the recommendations of various standards in relation to the transport of LBC.Citation12 In a study carried out in Burkina Faso,Citation18 LBCs were transported in 100% of cases in thermo stable coolers without an “ice-box”.
Practitioners of the Blood Transfusion (BT)
As a medical procedure, BT must be performed by the doctor or his/her delegacy to the nurse or midwife and in the absence of any adverse effects.Citation19 In this study we noticed that most of the LBCs were administered by nurses (70.4%) and then by resuscitator doctors (29.6%). In Togo, Aboubakari’s study revealed that 73.2% of LBCs had been transfused by intern trainees, 26.2% by nurses and 0.6% by doctors. Sawadogo noted that all LBCs were transfused by nurses.Citation18
Type of Blood Transfusion
In the current approach, all transfusions were performed in type-specific (ABO) and cross-matched Rh with homologous blood. This result is similar to the one of LouatiCitation20 who noticed that all transfusions of Labile Blood Components were in cross-matched Rh. Similarly Kouakou et alCitation6 reported 98.6% of transfusions in type-specific and 98.6% in cross-matched Rh and with homologous blood in 97.28%. According to the rules of blood transfusion, compatible and identical transfusions (Type-specific and cross-matched Rh) should be preferred over non-identical compatible transfusions (Non-type specific and Non-cross-matched Rh).
Compliance with Transfusion Rules
All the information related to the BT is of a great importance of the acceptance of the patient or her family members. Indeed, before any prescription of a blood transfusion, it is essential to aware the patient or her family members of the necessity for the transfusion. The procedure of transfusion is governed by legislation and engages the responsibility of the prescriber. Any error that may lead to legal proceedingsCitation12. In the current study, no patient or a member of her family was made aware of the disadvantages of transfusion. On the other hand, 70.4% of patients or their companions were informed about the advantages of transfusion. In Burkina Faso, SawadogoCitation18 in 2014 noted that the necessity for BT had been explained to patients and/or their companions, although awareness of the disadvantages of TB was not exhaustive.
All non-conformities (absence of transfusion sheet, quantity of blood to be transfused not specified, the rate of transfusion not indicated, the concordance control between the patient and the BCs to be transfused, the compatibility test at the patient’s bedside, the close monitoring of blood transfusion during the first 10 minutes) were reported in a high proportions in the current study. This situation is recurrent in many countries with limited resourcesCitation2,Citation6 and reflects a lack of rigor, the urgent context of transfusion and interdisciplinary consultation (clinicians, anesthesiologists and biologists).
In any haemotherapy, the acute transfusion reactions are mainly immunological, often serious and deserve to be prevented in advance. Our survey shows that 75.9% of transfused patients presented a transfusion reaction. This rate is upper to previous studies carried out in Gyneco-Obstetrical in African countries.Citation4,Citation6 Transfusion incidents that occurred during transfusions were not recorded in patient’s file and were performed by nurses. This justifies the lack of rigorous follow-up of the transfusion procedure by doctors.
Strengths and Weakness of the Study
This study presented strengths but also weakness at a certain degree.
The weakness of this study is inherent to its methodological approach. Indeed, the presence of the principal investigator at all stages of the transfusion chain could have influenced the transfusion practice and therefore biased the results. In addition, the lack of training of those involved in transfusion practice has not made it possible to accurately assess the performance of the various stakeholders and may justify the high proportions of non-compliances in relation to the various studied parameters. The monocentric nature is another weakness of the present study. The results of this study cannot be extrapolated to other hospital institutions (gynecology and obstetrics department) in Kinshasa. Finally, this study did not consider the medium and long-term complications of the patients included in the study.
Nevertheless, the present study is the first to assess the transfusion practice in the Gyneco-Obstetrics environment of the University Hospital of Kinshasa, highlighting the shortcomings of all the practitioners of the transfusion procedure.
Conclusion
This work has shown that the practice of transfusion has real a problem in the Department of Gynecology and Obstetrics of the UHK in terms of the transport of blood components, the consideration of the rules of haemovigilance, and the transfusion procedure.
Continuing education for all the actors involved in transfusion practice and clinical-biologist collaboration are therefore important to ensure blood transfusion under optimal conditions.
Ethical Considerations Ethics Statement
The protocol for this study has been approved by the National Health Ethics Committee (CNES) of the Ministry of Public Health of the Democratic Republic of Congo under number 264/CNES/BN/PMMF/2020 of 02/11/2020 and the written consent of the patients was obtained. All participants were informed about the purpose of the study and were voluntary participant complies declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work”.
Disclosure
Dr Guy Ndelembo Baina Snr reports grants, personal fees from Cliniques universitaires de Kinshasa, during the conduct of the study. The authors declare no other conflicts of interest.
References
- Andriamandranto HU, Rajaonarison TJ, Rakoto Alison AO, Randriambelomanana JA. blood transfusion in obstetrical practice at the CHU de gynécologie et obstétrique de befelatanana. Cardiovasc Digit Health J. 2021;2:4. doi:10.1016/j.cvdhj.2020.11.004
- Zamané H, Dembelé A, Sawadogo KCC, et al. Evaluation de Ia pratique transfusionnelle en urgence obstetricale et gynecologique au Centre Hospitalier Universitaire Yalgado Ouedraogo, Ouagadougou (Burkina Faso). Science Et Technique. 2014;37(1–2):101–109.
- Biswas S, Rengaraj S. Pattern of Blood Transfusion among Women undergoing Caesarean Section in a Tertiary Health Care Centre in South India. BMC Complement Altern Med. 2002;2(1):4. doi:10.1186/1472-6882-2-4
- Bonkoungou P, Lankoande M, Kinda B. Indications for transfusion and prognosis of women transfused at the Department of Obstetrics and Gynaecology of the Yalgado Ouédraogo University Hospital in Ouagadougou. Révue Africaine d’Anesthésiologie et de Médecine d’Urgence. 2014;19(2):18–21.
- Singh S, Sinha P, Yadav G, Gupta U, Tyagi P. Transfusion practices in obstetrics and gynaecology in a tertiary care center. Int J Reprod Contracept Obstetr Gynecol. 2017;5(3):831–834. doi:10.18203/2320-1770.ijrcog20160593
- Kouakou F, Effoh D, Loué V, Adjoby R, N’guessan K, Koffi A. Transfusion practice in the gynaeco-obstetrical environment. About 753 transfusions performed at the CHU of Cocody (Abidjan-RCI). Révue Africaine d’Anesthésiologie et de Médecine d’Urgence. 2011;16(1):15–19.
- World Health Organization. Regional Office for the Eastern Mediterranean. Strategic Framework for Blood Safety and Availability 2016-2025. World Health Organization. Regional Office for the Eastern Mediterranean; 2016. Available from: https://apps.who.int/iris/handle/10665/250403. Accessed June 19, 2022.
- Puri V, Dhal I, Singh K, Sharma G, Rai P, Sharma S. Critical audit of fresh frozen plasma transfusion practices in obstetric and gynecology departments in a tertiary care hospital – where and what needs to be improved? Glob J Transfus Med. 2019;4(2):175. doi:10.4103/GJTM.GJTM_49_19
- Chowdhury F, Akhter S, Islam A, Rayen J, Begum N, Begum F. Evaluation of blood transfusion practices in obstetrics and gynecology in a tertiary hospital in Bangladesh. J Bangladesh Coll Phys Surg. 2016;34(1):9–14. doi:10.3329/jbcps.v34i1.29116
- Ouh YT, Lee KM, Ahn KH, et al. Predicting peripartum blood transfusion: focusing on pre-pregnancy characteristics. BMC Pregnancy Childbirth. 2019;19(1):477. doi:10.1186/s12884-019-2646-3
- Cauldwell M, Shamshirsaz A, Wong TY, et al. Retrospective surveys of obstetric red cell transfusion practice in the UK and USA. Int J Gynaecol Obstet. 2017;139(3):342–345. doi:10.1002/ijgo.12309
- Shander A, Gross I, Hill S, Javidroozi M, Sledge S. A new perspective on best transfusion practices. Blood Transfus. 2013;11(2):193–202. doi:10.2450/2012.0195-12
- Goubran HA, Elemary M, Radosevich M, Seghatchian J, El-Ekiaby M, Burnouf T. Impact of transfusion on cancer growth and outcome. Cancer Growth Metastasis. 2016;9:1–8. doi:10.4137/CGM.S32797
- Chhabra S, Namgyal A. Rationale use of blood and its components in obstetric-gynecological practice. J Mahatma Gandhi Inst Med Sci. 2014;19(2):93. doi:10.4103/0971-9903.138427
- Surbek D, Vial Y, Girard T, et al. Patient blood management (PBM) in pregnancy and childbirth: literature review and expert opinion. Arch Gynecol Obstet. 2020;301(2):627–641. doi:10.1007/s00404-019-05374-8
- Bassowa A, Douaguibe B, Ajavon D, Fiagnon K, Aboubakari S, Akpadza K. Satisfaction and time to obtain blood products in obstetric emergency situations at Sylvanus Olympio Teaching University Center of Lome. Int J Res Rep Gynaecol. 2020;25:1–8.
- Green L, Knight M, Seeney FM, et al. The epidemiology and outcomes of women with postpartum haemorrhage requiring massive transfusion with eight or more units of red cells: a national cross-sectional study. BJOG. 2016;123(13):2164–2170. doi:10.1111/1471-0528.13831
- Sawadogo A. Blood transfusion practice in the gynaecology and obstetrics department of the Yalgado Ouédraogo University Hospital (Burkina Faso). UNIVERSITE DE OUAGADOUGOU; 2012.
- Chand NK, Subramanya HB, Rao GV. Management of patients who refuse blood transfusion. Indian J Anaesth. 2014;58(5):658–664. doi:10.4103/0019-5049.144680
- Louati N, Rekik T, Chaabane R, Chaabane K, Mnif H, Gargouri EJ. Evaluation of transfusion practices in obstetrical environment. 2007.