Abstract
Stamford Hospital (SH) is a 305 bed Level II Trauma center located in Fairfield County, the epicenter of the coronavirus disease 2019 (COVID-19) pandemic in Connecticut. The COVID-19 pandemic was a fast paced, rapidly evolving crisis, presenting our leadership team with unique challenges related to resource availability, patient care, and staff safety. The existing Hospital Incident Command System (HICS) was activated in March 2020 to coordinate our operational emergency management planning, response, and recovery capability for this unplanned event. Although HICS lays the groundwork for hospital preparations and protocol implementation, it is not designed to withstand prolonged crisis circumstances. Given the conditions that the COVID-19 pandemic presented, the possibility for future waves became an impending reality, prompting the need for a long-term solution. To establish guidelines that promoted balance between necessary preparations in the case of additional surges of the pandemic and concurrent resumption then maintenance of routine hospital operations, the SH COVID-19 Playbook was created. The Playbook, presented here, is arranged in accordance with the evidence-based 4 S’s (Space, Staff, Systems, and Stuff) strategic critical care planning framework, to address surge capacity management within our hospital’s four main patient care areas and additional supportive services. Through feedback from frontline caregivers and leaders within SH, the Playbook captures our experience, best practices, and insight acquired during the first wave of the pandemic. Established with the intentions of equipping leadership and staff globally, guidelines are presented to aid in the navigation of future pandemic surges and successfully care for COVID-19 patients, ensure staff safety, allow for normal services to operate, and provide optimal communication and support for the community, patients, and staff.
Background
The emergence of COVID-19 has caused unprecedented challenges for healthcare systems internationally. Hospital emergency preparations for events of this nature incorporate the implementation of a Hospital Incident Command System (HICS) which exercises supplementary oversight to guide the hospital through crises. Simultaneously safeguarding system processes, staff, and patients while maintaining their institutions’ core mission and values is paramount.Citation1
HICS was established by the California Emergency Medical Services Authority,Citation2–5 allowing for common terminology and coordinated leadership decision-making, encompassing all phases of emergency response efforts in collaboration with stakeholders such as community leaders, frontline staff, and executives.Citation1,Citation6 HICS is grounded on the same principles as the Incident Command System (ICS) component of the National Incident Management System (NIMS), with HICS guiding hospital systems on response and recovery management for disaster events.
Healthcare leadership uses incident management principles regularly for Emergency Department (ED) surges, resource and staff scarcity, mass casualty events, with systems then resuming routine services after the emergency event.Citation7,Citation8 Nevertheless, the COVID-19 pandemic was drastically different than previous crisis encounters, demanding intense and long-term decision-making for executive leadership beyond those typically guided by HICS.
Setting
Stamford Hospital (SH) is a 305 bed Level II Trauma center located in Fairfield County, serving one of the largest cities in the state of Connecticut (CT). Due to the proximity to the New York (NY) metropolitan area, our county was inundated with COVID-19 infections. On March 11th, 2020, our community-based teaching hospital’s first COVID-19 patient was admitted. The first Intensive Care Unit (ICU) admission occurred within 48 hours, and we reached our peak inpatient census of 151 patients, including 61 ICU admissions by April 14th, 2020. The extent of the impending surge of critically ill patients was unknown and experts cautioned of an international threat due to COVID-19’s precarious and unknown virulence, with the potential to overwhelm healthcare institutions globally.Citation9
Battling the First Surge
HICS was officially activated on March 9th, 2020, as SH entered the critical response stage,Citation5 with executive leadership meeting at least three times per week to review the current state of the pandemic and its current effect on the healthcare system at large. As part of the HICS planning phase,Citation10 a COVID-19 Response Planning Team was created and responsible for continued and ongoing surveillance of cases within the community and the hospital, as well as monitoring the operational aspects of caring for COVID-19 patients system wide. The Team met daily or weekly and was responsible for activating the full HICS response if triggered to do so. outlines the standing agenda of these meetings and topics addressed.
Table 1 Agenda Breakdown for COVID-19 Response Planning Meetings
HICS command members comprised of leadership and caregivers across the organization, such as the Executive Team and key clinical and operational leaders. Once activated, command members met based on the Incident Commander’s recommendations and were responsible for: reviewing current data, providing public health and medical updates to stakeholders and the community, assessing operational and logistical needs, and addressing staff well-being.
Expanding Bed Capacity
While our newly constructed patient rooms among all units and floors were developed as single patient rooms,Citation11 leadership decided it was best to double room occupancy among two of our general medical floors to ensure that proper isolation and bed availability were achieved via the use of COVID-19 and non-COVID-19 care zones. These procedures and novel workflow changes have been cited in the literature as best practices and strategies implemented internationally,Citation12–14 although taking place at large medical centers with additional resources and organizational surge capacity.
Knowing that we had limited capacity and that some of our patients no longer required acute inpatient services but could not return home, the decision was made to open an Alternate Care Site (ACS) using our old, decommissioned hospital building on the same campus as the new hospital. The teams moved quickly to reactivate a designated area of the old hospital as beds and equipment were required as well as the necessary technology to support the continuation of care. The National Guard staffed this unit, which would be open to internal transfers from Stamford Health as well as neighboring healthcare organizations that needed a place to send discharged patients.Citation15–17
Workflow Augmentations
Guidelines and workflows were established by executive leadership to standardize our infection prevention and control practices during procedures that might expose staff to the virus.Citation10 Each workflow that was new or altered required collaboration and buy-in from clinical staff, and non-clinical staff to adequately and efficiently care for infectious patients, such as transporters, dietary and housekeeping. Other departments that provided essential input on these workflows included Information Services (to ensure we had the right technology in each new room and ensuring it was reflected in our Electronic Medical Records (EMR)), Facilities (to ensure the right equipment to care for these patients were being set up on the newly created COVID-19 units), Materials Management (to ensure all staff that were entering patient rooms wore the correct Personal Protective Equipment (PPE)), and Pharmacy.
As the global pandemic was quickly spreading, it became apparent that we needed to rapidly provide valuable data and insights to leaders and colleagues. In highlighting systems that were created or altered during the pandemic, it is important to mention our COVID-19 dashboard and various teams required for successful implementation of our augmented workflows and protocols.
By early April, staffing shortages, resources, and visitation restrictions were key stressors for our leadership team. Planning meetings during this time focused on augmenting the hospital’s infrastructure, as the COVID-19 positive patient population had to be safely isolated, thus creating entirely new or altering existing workflows. Every clinical area required at least one or multiple new patient care processes, which were continuously being modified, sometimes several times a day. Because many of our COVID-19 units were impromptu creations, such as standing up additional ICUs and converting private rooms to semi-private rooms, workflows needed to be established on how to do this efficiently and effectively.
Surveillance
Tracking and forecasting COVID-19 related data points was vital when monitoring staffing levels, available beds, equipment, and supplies. Using our current technology, HICS leadership and National Guard staff worked with our Analytics & Innovation (AI) team to delineate and locate the data sources required to populate our COVID-19 dashboard (). Surveillance of important metrics and census levels were already built within our system’s EMR, as some data points are for more than just our main inpatient health records system, a similar response strategy used by large medical systems.Citation18
Figure 1 Data sources specifically created for SH’s COVID-19 Dashboard.
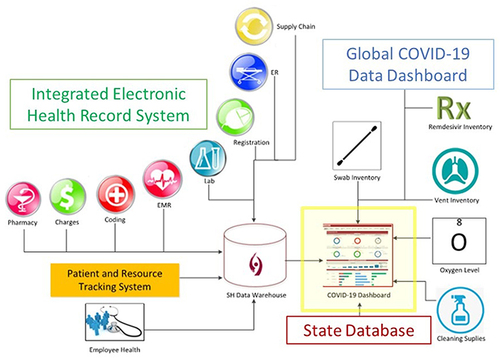
On March 29, 2020, the United States (US) federal government required hospitals to submit daily data reports to understand the burden, capacity, capabilities, and number of patients hospitalized due to COVID-19.Citation19 Our “all-hands-on-deck” approaches for this top priority task enabled us to create and test these new data sources in hours as opposed to weeks. Staffing levels, testing, and positivity rates were metrics captured by SH’s Employee Health department and displayed within the dashboard. Important metrics were continuously added to the dashboard based on the necessity to track items such as oxygen levels per room and supply inventory for both our system and when reporting to local and regional partners. New resources included a Teletracking system that displayed the inpatient positivity status, location of admission, and pertinent care information.
Much about the novel virus remained unclear to healthcare leaders, including if and when crisis proportions would be reached.Citation20 Efforts to monitor the national and global rates of morbidity and mortality were complex due to the lack of uniformity in reporting in care settings. Requiring only one link for full integration, the John Hopkins COVID-19 surveillance dashboard was added as an additional planning tool to view the ever-changing global, national, and state trends.Citation21
Support Services
Early on, the clinical treatments and procedures guidelines were recognized as first line, but when new recommendations and/or treatments failed to reduce morbidity, command members were required to make rapid protocol changes, similarly experienced among other institutions when battling the first surge.Citation22–24 For example, initially recommended medications for COVID-19 treatment, such as hydroxychloroquine and lopinavir/ritonavir were swiftly proven ineffective and thus no longer a frontline treatment for inpatients.Citation25 During the month of March 2020, while 89% of the ongoing clinical trials in the US paused enrollment due to the pandemic and related visitation barriers,Citation26–28 SH was one of the first sites in the US to obtain approval for Convalescent Plasma treatment. Once further treatments were approved through the expanded access program, they were added to our existing treatment protocols.
Moreover, when visitation was halted and to further support our ICU staff, a novel Family Liaison communication team was established to provide families status updates on their loved one admitted to the ICU, with other hospitals establishing similar ICU family communication teams.Citation29–31 Liaison’s increase capacity for ICU staff to focus on their complex patient care duties to alleviate their workload while still delivering a family-centered approach in palliative communication. The organization’s existing Cardiac Surgery Patient Navigation Workflow was adapted to train and recruit staff volunteers for the program and was initiated in under two weeks.
Additionally, to help shorten the hospital stay of COVID-19 patients requiring oxygen without compromising a safe discharge a comprehensive, multi-disciplinary home oxygen outpatient program was established. Prior to the pandemic, SH did not have an established post-discharge oxygen program. Leadership collaborated with an oxygen supplier, enabling us to purchase and provide portable pulse oximeters to these patients upon discharge. Before discharge, patients were educated and trained on proper home utilization. Follow-up and monitoring was provided by a designated Case Manager, who communicated the patients’ status with the care team.
The Ongoing Pandemic Response
Pandemic management focuses on minimizing the short and long-term impact on health systems utilizing emergency operation guidelines.Citation32 Important considerations include social distancing and strict cleaning measures, developing extensive workforce and community testing, implementing novel treatment measures and ensuring that adequate PPE and critical care equipment are readily available.Citation33–35 However, uncertainty of the pandemic’s surge potential, future pandemic waves, supply chain projections and the general novel and hazardous healthcare environment made it evident to executive leadership, critical care stakeholders, and patient care leaders that the HICS emergency response preparations were not sufficient to sustain the extended wave of the COVID-19 pandemic, similarly reported by both large medical centers and smaller healthcare systems.Citation22,Citation24,Citation36,Citation37 Lacking established response guidelines or treatment protocols to withstand the novelty and intensity of the circumstances required rapid decision-making on innovative system-wide emergency response plans, without knowledge or sufficient preparations for what was to come.
Development of the COVID-19 Playbook
A solution was crucial to provide transition points for long-term responses, prompting the creation of the SH COVID-19 Playbook (). Specifically designed by SH’s AI Team, the Playbook assists leadership and staff in the response to an additional surge in COVID-19 cases, while maintaining our ability to sustain normal and routine clinical and support operations. Essential protocols are defined to guide a sustained census period as well as during de-escalation of subsequent waves. The Playbook is structured to include pertinent information, inclusive of organizational triggers, incident command center infrastructure, emergency and critical care services, alternate care sites, testing capacity and capabilities, communication strategies and the responsibilities of supporting departments.
The 4 S’s: Space, Staff, Systems and Stuff surge capacity frameworkCitation32,Citation38,Citation39 allowed for integrated healthcare delivery versus the typical disease-specific vertical approach, while simultaneously identifying resources and potential gaps in our planning and response efforts. The surge capacity framework defines and incorporates healthcare crisis responses for conventional, contingency, and crisis phases, pertaining to space, stuff, systems, and stuff.Citation10 Threats to sustain normal operations are evaluated by leadership and the HICS Planning Team on a case-by-case basis, and when entering a critical stage of the pandemic, evaluating staffing needs, current professional and federal guidelines on clinical operations, and supply chain projections is recommended.Citation39 Determining and planning for adjustments that may be required to ensure the continuation of our normal operating procedures is pivotal and advised.Citation39,Citation40
The SH COVID-19 Playbook is organized by the 4 S’s and based on lessons learned during the first wave of the pandemic within SH’s four main patient care areas. To adequately guide leaders in pandemic management, SH’s COVID-19 Playbook details concurrent activities to be taken during subsequent surges.
Table 2 COVID-19 Playbook
Support Services
Staff
Hiring and onboarding supplemental staff is guided by the critical care staffing models,Citation10,Citation39 requiring novel inter-departmental and external collaborations, including the human resources (HR), nursing, and Information Security departments expedited clearance processes and instituting badge and network access privileges. When surging, nursing leadership designates a point person for onboarding, along with the division of the HR departments to allocate work groups based on individual strengths (COVID-19 team and day-to-day team). We partner with travel agencies who honored a short-term pandemic specific contract, helping to create “COVID-19” offer letters, and recruit staff. A separate Central Staffing Command Center is activated as soon as critical numbers are reached in each unit to manage the hiring and onboarding process of the clinical labor pool/travelers while HR manages the non-clinical labor pool. High school and college volunteers work throughout the hospital including in our ED. Planning teams determine when the volunteer program should halt all in-person volunteer activities, with an all-staff email sent alerting departments of this necessary change.
Marketing and Communications
Based on feedback after the initial surge, many novel communication and marketing strategies are incorporated into the Playbook. To improve the provision of pertinent information on the rapidly changing healthcare situation, leadership hosts live Town Hall and Q&A sessions on clinical, operational and staff well-being. Our new COVID-19 internal and external websites, house pandemic related materials and resources, to facilitate the provision of updates to staff and community members regarding the latest guidance and policies.
Partnerships
One example of regional partnerships includes SH’s Fairfield County Incident Command Collaborative (FCICC). The FCICC creates the broad and ongoing planning and policy considerations at the level of the Connecticut Hospital Association and state government. The FCICC was established early in the pandemic course to promote collaboration in preparedness, resource management, staffing, and patient care. Assisting and guiding patient transfers, optimizing resources to support the most critical needs across the region, and sharing the same operating protocols to ensure a collaborative environment to best meet the needs of our patients and communities continues to be a best practice. Core activities include sharing data on resources such as PPE, ventilator usage, staffing levels, inpatient census, and the development of clinical protocols when necessary.
During a surge, FCICC commanders organize safe and pre-defined routes when transferring medical and ICU patients between hospitals in the context of constantly changing bed availability and incident community level surges. We continue to communicate and work with key external organizations including local and state governments and health departments, skilled nursing facilities and hospital associations in CT and Greater NY.
Pandemic Decision-Making
There was a need for actionable tools for clinical decision-making to ensure consistent equitable care practices. SH established a mechanical ventilator allocation policy if another surge or public health emergency creates demand for ventilators that outstrips the total supply at SH. The allocation policy, guided by the literature, is enacted if ventilator capacity is, or will shortly be, overwhelmed despite taking all appropriate steps to increase the surge capacity to care for critically ill patients.Citation41 The allocation framework is grounded in ethical obligations that include the duty to care, the duty to steward resources to optimize population health, distributive and procedural justice, and transparency.Citation39 Allocation is based on available objective medical evidence and individualized patient assessments. The policy describes 1) the circumstances and process of instituting and terminating the ventilator allocation protocol; 2) the creation of Triage Teams to ensure consistent decision-making; 3) allocation criteria for initial allocation of ventilators; and 4) reassessment criteria to determine whether ongoing provision of scarce ventilators are justified for individual patients.
Discussion
The first surge of COVID-19 patients required the global community to implement and escalate disaster plans, not knowing these plans would soon be proven incapable of handling the impending pandemic’s circumstances. While the first wave of the pandemic hit our and other healthcare systems with ferocity and limited time to plan, subsequent downtime between future waves allowed us to create a planning tool utilizing the 4 S’s, Space, Staff, Systems and Stuff to provide continuity in patient care during the sustained crisis. To best utilize our current Space, we can rapidly convert non-clinical areas, such as conference rooms, to aid clinical operations and reduce exposure. Three additional ICUs can be created in non-critical areas to triple ICU capacity in addition to expanding from one to two Intermediate Care Units. Special considerations for those areas that can accommodate critically ill patients include determining the order to open the units in and establishing triggers for such; determining how to open each additional ICU (opening the entire unit versus in pods of 4); staffing critical care nurses, intensivists, and respiratory therapists; and availability of equipment, beds, negative pressure rooms, and medical gases.
To provide proper and prompt care to all patients admitted during an influx of patients, we have established rapid on-boarding and credentialing processes to mitigate a critical staffing shortage (Staff). Staff and care teams are supplemented by temporarily hiring external traveling healthcare professionals and recruiting SH staff possessing the knowledge to care for those with COVID-19. In addition, staff can be quickly reassigned to other COVID-19 specific roles to support other units with increased patient demand. Novel programs include the Home Oxygen program, Family Liaison program, Proning Teams,Citation60 and specialized COVID-19 care teams. To best utilize our system capacity, multiple workflows can be altered or newly created within the various clinical areas of the hospital to best suit the sustained pandemic demands. In addition to patient-related workflows, expansion plans were also created for critical care areas, forward triaging in the ED in the case that the military tents were used, as well as acute care units. Managing stuff is a centralized process to ensure all appropriate equipment and PPE needed to sustain and maintain staff safety and patient care.
The psychological and physical impact of caring for the surge of critically ill patients is cited in the literature as being extremely distressing, causing acute psychological stress among frontline staff.Citation42–44 A cross-sectional survey assessed our essential workers’ current state of welfare as well as motivators and coping strategies. Staff reported feeling burned out, emotionally distraught, and fearful for their own and loved one’s safety. Furthermore, peer support and teamwork, along with constant communications from leadership, were factors that helped motivate SH’s frontline staff to come back to work each day.Citation45,Citation46
To improve staff well-being and reduce their pandemic associated anxieties, numerous support programs became newly available such as calming “Peace Rooms”, teaching providers transcendental meditation and the 24/7 Resilience in Stressful Events (RISE)Citation47 crisis peer support hotline. Furthermore, our medical residents reported high burnout rates and negative mental health consequences before, during and after the first surge,Citation48 an issue among all trainees and frontline workers cited in the literature by many throughout the last two decades.Citation49–51 Support initiatives to improve well-being including wellness coaching, team building events, and lectures on wellness topics are additional services advised by the literature and provided at SH for this at risk group.Citation52–54
Importantly, partnerships with local and regional systems and coalitions aided in maximizing capacity and capabilities to provide regional consistency of care, cited as a best practice and a commonly used strategy during disasters and the COVID-19 pandemic.Citation10,Citation55–57 We also instituted strong communication strategies which have also been initiated by other institutions as a best practice to ensure staff feel supported and to ensure the surrounding community is apprised and informed.Citation37,Citation58,Citation59
Our experience, as well as others,Citation13,Citation22,Citation24 demonstrated that emergency planning is essential and even the best plans inevitably cannot foresee or anticipate every eventuality, as each emergency and crisis is unique. Due to the surge caused by the Omicron variant, our resources were pushed yet again as SH’s inpatient census reached a daily high census of 91 patients. We are confident that the creation of the Playbook and its continued use and refinement allowed us to maintain most if not all our routine services.
Conclusion
SH’s system wide response strategies greatly differed from previous disaster responses, as limited information on COVID-19 was available to guide executive leadership decision-making when leading through a disaster. Ultimately, our altered yet effective approaches to the pandemic enabled our 305-bed community-based teaching hospital to weather the first months of the pandemic, establishing a new normal for future practice and pandemic surges. As the pandemic continues, leadership must review their pre-defined HICS procedures and guidelines, ensure a HICS chain of command, designated surge teams with defined responsibilities, and amplified surveillance for an organized, timely, and effective response.
Although crisis management for the COVID-19 pandemic at SH was initially through the HICS approach, utilization was restricted due to its limited intrinsic capacity to fulfill the disparate needs a community hospital may face during an extended health disaster. The undulating nature of COVID-19 therefore required HICS to be refined to ensure long-term stability and sustainability. Vital operations and systems must be pre-defined and maintained through the face of an event of such destructive nature to not only preserve life but to also provide essential functions to those patients not affected by COVID-19. In creating the COVID-19 Playbook, leadership can proactively address key operational strategies during the next emergency, ensuring our hospital is equipped to effectively mitigate threats and continue to optimize care of the patients and communities we serve.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
We would like to acknowledge the leadership, staff, and care teams across Stamford Health, for tirelessly caring for our patients and the Stamford community during the pandemic.
References
- CHA. Hospital Incident Command System (HICS). Emergency Preparedness; 2019. Available from: https://www.calhospitalprepare.org/overview/hospital-incident-command-system-hics. Accessed October 5, 2020.
- EMSA. HICS history and background. EMSA; 2020. Available from: https://emsa.ca.gov/hics-history-and-background/. Accessed September 9, 2020.
- Nowell B, Steelman T. Beyond ICS: how should we govern complex disasters in the United States? J Homel Secur Emerg Manag. 2019;16(2). doi:10.1515/jhsem-2018-0067
- Hospital Safety Center. Take a hike, HEICS: new HICS takes over for incident command; 2007. Available from: http://hospitalsafetycenter.com/print/67722/topic/WS_HSC_HSC.html. Accessed October 24, 2021.
- Medicine I of. Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. Introduction and CSC Framework; 2012.
- CDPH. HICS guidebook 2014. CDPH - Emergency Preparedness Office; 2014. Available from: http://cdphready.org/hics-guidebook-2014/. Accessed September 9, 2020.
- Rüter A, Kurland L, Gryth D, Murphy J, Rådestad M, Djalali A. Evaluation of disaster preparedness based on simulation exercises: a comparison of two models. Disaster Med Public Health Prep. 2016;10(4):544–548. doi:10.1017/dmp.2015.176
- Cole D. The Incident Command System: A 25-Year Evaluation by California Practitioners. National Fire Academy; 2000:30.
- Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet Lond Engl. 2020;395(10223):470–473. doi:10.1016/S0140-6736(20)30185-9
- Hick JL, Einav S, Hanfling D, et al. Surge capacity principles: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. CHEST. 2014;146(4):e1S–e16S. doi:10.1378/chest.14-0733
- Rose SJ, Waggener L, Kiely SC, Hedge A. Postoccupancy evaluation of a neighborhood concept redesign of an acute care nursing unit in a planetree hospital. HERD Health Environ Res Des J. 2022;15(3):171–192. doi:10.1177/19375867221091318
- Peters AW, Chawla KS, Turnbull ZA. Transforming ORs into ICUs. N Engl J Med. 2020;382(19):e52. doi:10.1056/NEJMc2010853
- Bader MK, Braun A, Fox C, et al. A California hospital’s response to COVID-19: from a ripple to a tsunami warning. Crit Care Nurse. 2020;40(6):e1–e16. doi:10.4037/ccn2020799
- Koh HK, Shei AC, Bataringaya J, et al. Building community-based surge capacity through a public health and academic collaboration: the role of community health centers. Public Health Rep. 2006;121(2):211–216. doi:10.1177/003335490612100219
- Dire DJ, Suter RE, Robinson JD, Lynn WS. Army urban augmentation medical task forces for COVID-19: part 2—initial utilization. Mil Med. 2021;186(11–12):314–318. doi:10.1093/milmed/usab308
- Dire DJ, Suter RE, Robinson JD, Lynn WS. Army urban augmentation medical task forces for COVID-19: part 1-development. Mil Med. 2021;186(11–12):309–313. doi:10.1093/milmed/usab309
- ASPR TRACIE. The National guard’s response to COVID-19. ASPR TRACIE; 2022. Available from: https://asprtracie.hhs.gov/technical-resources/resource/10949/the-national-guards-response-to-covid-19. Accessed August 8, 2022.
- Satterfield BA, Dikilitas O, Kullo IJ. Leveraging the electronic health record to address the COVID-19 pandemic. Mayo Clin Proc. 2021;96(6):1592–1608. doi:10.1016/j.mayocp.2021.04.008
- CDC. COVID-19 public health reporting for laboratories that develop or use laboratory developed tests with intent to obtain EUA; 2020. Available from: https://www.cdc.gov/csels/dls/locs/2020/covid-19_public_health_reporting.html. Accessed August 7, 2022.
- D’Auria G Leadership in a crisis: responding to the coronavirus outbreak and future challenges. McKinsey - Organ Pract; 2020. Available from: https://www.mckinsey.com/business-functions/organization/our-insights/leadership-in-A-crisis-responding-to-The-coronavirus-outbreak-and-future-challenges#. Accessed November 9, 2022.
- Hopkins J. COVID-19 map. Johns Hopkins Coronavirus Resource Center; 2020. Available from: https://coronavirus.jhu.edu/map.html. Accessed December 7, 2020.
- Garg M, Wray CM. Hospital medicine management in the time of COVID-19: preparing for a sprint and a marathon. J Hosp Med. 2020;15(5):305–307. doi:10.12788/jhm.3427
- Matear D, Hunter R. Hospital incident command system: preparedness and application for COVID-19 response in California’s Central Valley. J Bus Contin Emerg Plan. 2021;14(3):288–304.
- Jain PN, Finger L, Schieffelin JS, Zerr DM, Hametz PA. Responses of three urban U.S. Children’s Hospitals to COVID-19: Seattle, New York and New Orleans. Paediatr Respir Rev. 2020;35:15–19. doi:10.1016/j.prrv.2020.06.002
- Rosenberg ES, Dufort EM, Udo T, et al. Association of treatment with hydroxychloroquine or azithromycin with in-hospital mortality in Patients with COVID-19 in New York State. JAMA. 2020;323(24):2493–2502. doi:10.1001/jama.2020.8630
- Irb WCG. Clinical trial insights from the WCG knowledge BaseTM. WCG IRB; 2020. Available from: https://www.wcgclinical.com/covid-19/covid-19-trial-insights/. Accessed April 5, 2022.
- Unger JM, Xiao H, LeBlanc M, Hershman DL, Blanke CD. Cancer Clinical Trial Participation at the 1-Year Anniversary of the Outbreak of the COVID-19 Pandemic. JAMA Netw Open. 2021;4(7):e2118433. doi:10.1001/jamanetworkopen.2021.18433
- Cramer G. How the pandemic has changed clinical trials. Rutgers University; 2021. Available from: https://www.newswise.com/coronavirus/how-The-pandemic-has-changed-clinical-trials. Accessed April 12, 2022.
- Wendel PK, Stack RJ, Chisholm MF, et al. Development of a communications program to support care of critically Ill coronavirus disease 2019 (COVID-19) patients. J Patient Exp. 2020;7(5):673–676. doi:10.1177/2374373520956865
- Lipworth AD, Collins EJ, Keitz SA, et al. Development of a novel communication liaison program to support COVID-19 patients and their families. J Pain Symptom Manage. 2021;61(1):e1–e10. doi:10.1016/j.jpainsymman.2020.11.016
- Gabbie S, Man K, Morgan G, Maity S. The development of a family liaison team to improve communication between intensive care unit patients and their families during the COVID-19 pandemic. Arch Dis Child Educ Pract Ed. 2020;106(6):367–369. doi:10.1136/archdischild-2020-319726
- Hick JL, Christian MD, Sprung CL. Chapter 2. Surge capacity and infrastructure considerations for mass critical care. Intensive Care Med. 2010;36(1):11–20. doi:10.1007/s00134-010-1761-4
- Jester B, Uyeki T, Jernigan D. Readiness for responding to a severe pandemic 100 years after 1918. Am J Epidemiol. 2018;187(12):2596–2602. doi:10.1093/aje/kwy165
- CDC. Public health preparedness capabilities: national standards for state and local planning. Public Health Emergency Preparedness and Response Capabilities: National Standards for State, Local, Tribal, and Territorial Public Health; 2021. Available from: https://www.cdc.gov/cpr/readiness/capabilities.htm. Accessed March 10, 2022.
- CDC. Space, staff, and stuff; 2021. Available from: https://www.cdc.gov/cpr/readiness/healthcare/SpaceStuf.htm. Accessed September 14, 2021.
- Boyle A, Dotson S, Ellison P, Hayanga H. Application of the principles of biomedical ethics to the labor and delivery unit during the COVID-19 pandemic. J Womens Health. 2020;29(11):1361–1371. doi:10.1089/jwh.2020.8812
- Ahern S, Loh E. Leadership during the COVID-19 pandemic: building and sustaining trust in times of uncertainty. BMJ Lead. 2020. doi:10.1136/leader-2020-000271
- Hick JL, Koenig KL, Barbisch D, Bey TA. Surge capacity concepts for health care facilities: the CO-S-TR model for initial incident assessment. Disaster Med Public Health Prep. 2008;2(S1):S51–S57. doi:10.1097/DMP.0b013e31817fffe8
- Hick JL, Hanfling D, Wynia MK, Pavia AT. Duty to plan: health care, crisis standards of care, and novel coronavirus SARS-CoV-2. NAM Perspect. 2020. doi:10.31478/202003b
- Dichter JR, Kanter RK, Dries D, et al. System-level planning, coordination, and communication: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4Suppl):e87S–e102S. doi:10.1378/chest.14-0738
- Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of covid-19. N Engl J Med. 2020;382(21):2049–2055. doi:10.1056/NEJMsb2005114
- Barzilay R, Moore TM, Greenberg DM, et al. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl Psychiatry. 2020;10(1):291. doi:10.1038/s41398-020-00982-4
- Bender AE, Berg KA, Miller EK, Evans KE, Holmes MR. “making sure we are all okay”: healthcare workers’ strategies for emotional connectedness during the COVID-19 pandemic. Clin Soc Work J. 2021;1–11. doi:10.1007/s10615-020-00781-w
- Bernstein CA, Bhattacharyya S, Adler S, Alpert JE. Staff emotional support at Montefiore Medical Center during the COVID-19 pandemic. Jt Comm J Qual Patient Saf. 2020;47(3):185–189. doi:10.1016/j.jcjq.2020.11.009
- Rose S, Hartnett J, Pillai S. Healthcare worker’s emotions, perceived stressors and coping mechanisms during the COVID-19 pandemic. PLoS One. 2021;16(7):e0254252. doi:10.1371/journal.pone.0254252
- Rose S, Hartnett J, Pillai S. A comprehensive dataset describing nurse’s emotions, perceived stressors and coping mechanisms during the first surge of the COVID-19 pandemic. Data Brief. 2022;40:107814. doi:10.1016/j.dib.2022.107814
- Connors C, Wu AW. RISE: an organized program to support health care workers. Qual Manag Healthc. 2020;29(1):48–49. doi:10.1097/QMH.0000000000000233
- Heluey C, Bahgat J, Hartnett J, Rose SJ, Newman RB, Homayounrooz F. The effects of the COVID-19 crisis on resident well-being in a community teaching hospital. South Med J. 2022;115(9):712. doi:10.14423/SMJ.0000000000001437
- Zoorob D, Shah S, Saevig DL, Murphy C, Aouthmany S, Brickman K. Insight into resident burnout, mental wellness, and coping mechanisms early in the COVID-19 pandemic. PLoS One. 2021;16(4):e0250104. doi:10.1371/journal.pone.0250104
- Aziz H, James T, Remulla D, et al. Effect of COVID-19 on surgical training across the United States: a National survey of general surgery residents. J Surg Educ. 2020;78(2):431–439. doi:10.1016/j.jsurg.2020.07.037
- Cabarkapa S, Nadjidai SE, Murgier J, Ng CH. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: a rapid systematic review. Brain Behav Immun Health. 2020;8:100144. doi:10.1016/j.bbih.2020.100144
- Melnyk BM, Kelly SA, Stephens J, et al. Interventions to improve mental health, well-being, physical health, and lifestyle behaviors in physicians and nurses: a systematic review. Am J Health Promot. 2020;34(8):929–941. doi:10.1177/0890117120920451
- Barbash IJ, Kahn JM. Fostering hospital resilience—lessons from COVID-19. JAMA. 2021;326(8):693–694. doi:10.1001/jama.2021.12484
- Pollock A, Campbell P, Cheyne J, et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst Rev. 2020;11:CD013779. doi:10.1002/14651858.CD013779
- Abir M, Nelson C, Chan EW, et al. Critical Care surge response strategies for the 2020 COVID-19 Outbreak in the United States. RAND Corporation; 2020. Available from: https://www.rand.org/pubs/research_reports/RRA164-1.html. Accessed October 27, 2021.
- ACEP. Health care system surge capacity recognition, preparedness, and response. ACEP; 2017. Available from: https://www.acep.org/patient-care/policy-statements/health-care-system-surge-capacity-recognition-preparedness-and-response/. Accessed September 14, 2021.
- Kim CS, Meo N, Little D, et al. Bracing for the storm: one health care system’s planning for the COVID-19 surge. Jt Comm J Qual Patient Saf. 2020. doi:10.1016/j.jcjq.2020.09.007
- Francisco C, Nuqui A. Emergence of a situational leadership during COVID-19 pandemic called new normal leadership. Online Submis. 2020;4. doi:10.17613/ETSV-NN43
- HariharanSiddharth WL, SmithWill AR. FergusonBrian, FussellChris. Improving health care leadership in the covid-19 era. NEJM Catal Innov Care Deliv. 2020;2020:15.
- Elharrar X, Trigui Y, Dols AM, et al. Use of Prone Positioning in Nonintubated Patients With COVID-19 and Hypoxemic Acute Respiratory Failure. JAMA. 2020;323(22):2336. doi:10.1001/jama.2020.825.
