Abstract
Purpose
Previous studies show that the hospital environment and the behavior of health care personnel may predict patients’ perceptions of care quality. The aim of the study was to explore changes in perceived care quality from the patients’ perspective (QPP) when hospital services are relocated from an old to a new high-tech hospital and to describe what is important for patients in the high-tech hospital.
Patients and methods
A comparative cross-sectional design was used. The questionnaire QPP, which is based on a theoretical model of the quality of care comprising four quality dimensions, was used. Data were collected in 2015 (old hospital) and 2016 (new hospital), with 253 and 324 respondents, respectively, by consecutive sampling. Comparative statistics was used to test differences between patients’ care quality perceptions (perceived reality [PR] and subjective importance [SI]) (P≤0.05).
Results
The patients rated PR of all four quality dimensions (the care organization’s physical-technical conditions and sociocultural approach and the caregivers’ medical-technical competence and identity-oriented approach) higher in the new hospital. However, only the two quality dimensions concerning the care organization were rated significantly more highly. On an item level, five of the 27 items scored significantly higher on patients’ SI than on patients’ PR of the care in the new hospital, indicating a quality deficiency from the patients’ perspective. This comprised receiving effective pain relief, receiving examination and treatment within an acceptable waiting time, receiving useful information on self-care, receiving useful information on which doctors were responsible for their medical care, and having a comfortable bed.
Conclusion
The increase in care QPP was associated with improved environmental conditions, and no significant improvement in care quality was associated with the health care personnel. The results indicate that being in a high-tech environment does not improve patients’ perceptions of care quality provided by health care personnel. The results gave valuable information for quality improvement in clinical practice, based on the patients’ perspective.
Introduction
Patients’ perceptions of care quality are one of the essential indicators of care quality, and as such important for quality improvement work.Citation1–Citation3 Patients in need of health care services wish for individualized, high-quality care, which is also the main goal for those providing the care.Citation2,Citation4,Citation5 Patients’ individual perceptions of care quality are important, because they may reflect patients’ perceptions of standards in hospital wardsCitation6 and also clarify how patients define quality.Citation7 The theoretical model of quality of care: The Quality of Care from the Patients’ Perspective (QPP) views care quality through the patient’s eyes and is used as the theoretical foundation in this study.Citation8 Quality of care in the QPP model is seen as a measure of patients’ experiences of the quality of health care encountering patients’ perceived reality (PR).Citation8 Patients’ perceptions of what constitutes quality of care are formed by their system of norms, expectations, and experiences and by their encounter with an existing care structure.Citation8
Previous research has shown that different factors may impact on the patients’ perceptions of care quality. These factors can be classified into the following two broad areas: person-related conditions and external objective care conditions. Person-related conditions, such as the patients’ sex,Citation9,Citation10 age,Citation9,Citation11 educational level,Citation9,Citation10 self-reported physical health and psychological well-being,Citation12,Citation13 and whether the patients are admitted to hospital as emergencies or by schedule,Citation9,Citation10 are found to be connected with patients’ perceptions of care quality.
External objective care conditions connected with patients’ perceptions of care quality are as follows: the hospital’s organization and structure of care,Citation14–Citation16 the competence of health care personnel,Citation17–Citation19 the nurse–physician relationship,Citation20 the general atmosphere on the wards,Citation4 the size of the hospital,Citation9 the number of beds on each ward,Citation21 inpatient stay,Citation22 and occupancy.Citation21 In addition, a comfortable environment, comprising such aspects as hotel servicesCitation18 and staying in newer hospital buildings,Citation23 has a positive impact on patients’ quality ratings. Patients have also identified cleanliness, good signs/information points, adequate seating, nonovercrowding, and privacy for conversations as important when they are hospitalized.Citation24 One recent study explored changes in patient’s satisfaction when clinical services were relocated to a new clinical building with patient-centered features.Citation25 The increase in satisfaction was associated with improved room and visitor-related facilities such as pleasant décor, visitor accommodation, and comfort. However, no significant improvement in satisfaction with clinical providers or ancillary staff was found.Citation25
As described earlier, previous research focuses on the impact of patients’ person-related and external objective conditions on their quality of care perceptions. However, few studies explore the role of the high-tech hospital environment and patients’ perception of care quality. Furthermore, research investigating what patients view as being important for experiencing high care quality in high-tech hospitals is scarce.
The aim of the study was to explore changes in perceived care QPP when hospital services are relocated from an old to a new high-tech hospital and to describe what is important to patients in the high-tech hospital.
Methods
Design
The design was comparatively cross-sectional to explore patient’s perceptions of care quality.
Setting
A Norwegian hospital trust was relocated to a new clinical building in November 2015. The hospital serves approximately 290,000 people and is viewed as a medium-sized hospital in Norway. However, the number of emergency beds makes the hospital the fourth largest emergency hospital in Norway. The hospital has also been recognized as a showcase of best practice in the implementation of health care information technology and placed in Europe’s Electronic Medical Record Adoption Model (EMRAM) Stage 6 of the 7 Stages Club by Healthcare Information and Management Systems Society (HIMSS) Europe, which is an organization that assesses and scores the clinical information technology systems in European hospitals.Citation26
In the old hospital, the number of beds on the wards varied between 14 and 30, depending on the architectural conditions of the building. There were mostly multibedded patient rooms with shared bathrooms, and single rooms were scarce on each ward. Each ward also had one living room with a television for the patients to use and a kitchen for preparing small extra meals if needed. The new hospital consists solely of single-bed rooms with private bathrooms and television. The wards in the new hospital are standardized to 36 beds organized in four bed courts consisting of nine beds located around a working station. On every ward, there is a dining room with buffet dining for the patients.
In addition to new physical buildings, the relocation should comprise a reorganization of staff’s working methods and services because of the increased implementation of technology. The technology was applied in order to streamline the hospital systems, so that the patients would have fewer staff to interact with throughout their stay. It includes electronic whiteboards, which allow patient self-check and ensure coordination and logistics of inpatients. It also includes a system for message alerts using smart phones facilitating easy and rapid communication across disciplines and clinical units. Using mobile solutions such as tablets and smart phones, doctors and nurses have real-time information where they need it. Advanced logistics systems have also been introduced in the new hospital. Blood samples and medicines are transported in pneumatic tubes, while automatic guided vehicles (AGVs) transport clothes, foods, and merchandise. These systems contribute to more efficient logistics while relieving health professionals from this job, allowing them the possibility of spending more quality time with the patients.
Participants and procedure
The population consisted of patients ready for discharge from hospital wards during 2 weeks in the autumn of 2015 (old hospital) and autumn of 2016 (new hospital). Consecutive sampling was used. Patients were included if 1) they were 18 years or older, 2) they understood Norwegian, 3) they were able to express themselves verbally, and 4) their mental and physical health were such that it was ethically justifiable to invite them to participate. The responsible nurse on each ward assessed the patients according to these inclusion criteria.
On the day of the patient’s discharge or the day before, the contact person (nurse or secretary) on each ward/bed court gave patients, who satisfied the inclusion criteria, both oral and written information about the study. Patients who agreed to take part in the study received the questionnaire. Patients were instructed to return their completed questionnaire in a sealed envelope to the contact person before discharge. Patients who were not physically able to fill in the answers were offered assistance by one of the researchers in the research team. The researchers collected the envelopes daily during the 2 weeks of the data collection period. A total of 253 patients answered the questionnaire in the old hospital, and 324 patients answered the questionnaire in the new hospital, that is, 22 and 28.4% of discharged patients, respectively.
Data collection – the questionnaire
The respondents’ perceptions of care quality were measured using the QPP questionnaire,Citation27 including one item concerning information on the use and effects of medicines.Citation10 Furthermore, two items about fellow patients were included. The questionnaire is patient centered and derived from a theoretical model of quality of care; The Quality of Care from the Patients’ Perspective.Citation27 The model states that patients’ perceptions of what constitutes quality of care are formed by their system of norms, expectations, and experiences and by their encounter with an existing care structure. Hence, the patients’ perception of care quality includes four dimensions and the questionnaire consists of 27 items covering the caregiver’s medical-technical competence, the caregiver’s identity-oriented approach, the care organization’s physical-technical conditions, and the care organization’s sociocultural atmosphere.
Each item was evaluated in two ways by the respondents: the perceived reality (PR) of the item and the subjective importance (SI) of the item.Citation27 Each item’s PR described how the respondent experienced various aspects of care. Items were evaluated with sentences related to the statement “This is what I experienced”, for example, “My care was determined by my own requests and needs rather than the staff’s procedure”. A 4-point response scale ranging from 1 (do not agree at all) to 4 (completely agree) was used. Each item also had a “not applicable” response. The SI of each item described how important patients considered various aspects of care to be and described their preferences. Items were evaluated with sentences related to the statement “This is how important it was for me”, for example “The nurses showed commitment: ‘cared about me’”. A 4-point response scale ranging from 1 (little or no importance) to 4 (very highest importance) was used. Each item also had a not applicable response. The index of each dimension was calculated by adding the item scores and dividing the sum by the number of items answered within that dimension. The Cronbach’s a coefficients for PR in this study were 0.66/0.78 for medical-technical competence, 0.90/0.90 for identity-oriented approach, 0.54/0.62 for physical-technical conditions, and 0.79/0.89 for sociocultural atmosphere for 2015 and 2016, respectively. The Cronbach’s a coefficients for SI were 0.75/0.78 for medical-technical competence, 0.87/0.91 for identity-oriented approach, 0.77/0.76 for physical-technical conditions, and 0.82/0.90 for sociocultural atmosphere.
An Index of Measures () was developed by Lars-son and Wilde-LarssonCitation28 based on scores on the item’s PR and SI at the group level. The idea behind the Index is that various combinations of responses to questions on PR and SI should prompt different measures on the part of the caregivers.Citation28
Figure 1 Illustration of the Index of Measures (Larsson and Wilde-Larsson, 2003).Citation28
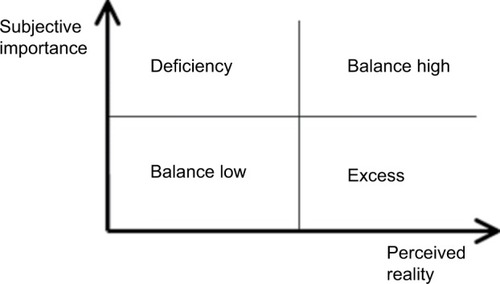
Care QPP is considered to be high when PR scores are higher than scores on SI and also when both scores on PR and SI are high and in balance. Previous studies have argued that high scores on QPP items range from about 3.30 to 4.0.Citation29,Citation30 Care quality is considered deficient from the patient’s perspective when scores on SI are higher than scores on PR. Finally, care quality is considered low when the balance is low on both SI and PR. Scores ranging between 3.30 and 3.00 are considered a modest rating,Citation29 and scores ranging from 3.00 and lower are considered a low quality rating.Citation29,Citation30
The questionnaire also included the respondents’ socio-demographic characteristics and health-related aspects comprising the following eight items: age, sex, education, inpatient stay, and respondent’s self-rated health condition in response to “How would you describe your present physical health condition?” and “How would you describe your present psychological well-being?” using a 5-point scale ranging from 1 (very poor) to 5 (very good). In addition, the respondents were asked about hospital admission (“scheduled” or “emergency”). In 2015, the respondents were asked whether they stayed in single rooms, multiple bed rooms, or the corridor. In 2016, the new hospital only had single rooms, consequently the question was changed, and the respondents were asked whether they stayed in single rooms or in a corridor during their stay. The questionnaire consisted of a total of 35 items.
Statistical analyses
Data were analyzed using SPSS Version 24.0 (IBM Corporation, Armonk, NY, USA).Citation31 The descriptive statistics frequency, percentage, mean, and standard deviation were used to describe the study sample and the respondents’ perceptions of quality of care, the PR and SI. Independent sample’s t-test was run on continuous variables, and Chi-squared test was run on categorical variables to explore potential differences in characteristics between the patient groups in the old and the new hospitals. The Mann–Whitney U-test was used to compare differences between the respondents’ care quality perceptions in the old and the new hospitals. Wilcoxon signed-rank test was used to test for potential differences between PR and SI in the 2016 sample (the new hospital). The Cronbach’s a was used to test the quality scales for internal consistency.Citation32,Citation33 Statistical significance was set at P≤0.05.
Results
Respondent characteristics
The characteristics of the two samples did not differ apart from significantly more men answering the questionnaire compared to women answering the questionnaire in the new hospital (2016). The median age in 2015 was 61 years, and the median age in 2016 was 65 years. Most respondents were admitted to hospital as emergencies. They rated their psychological well-being better than their physical health. The number of patients staying in a corridor in the new hospital was unchanged from the old hospital (refer for results).
Table 1 Respondents’ characteristics in the old hospital (N=253) compared with the new hospital (N=324)
The respondents’ Index of Measures
displays the respondents’ PR and SI at dimension level. In the old hospital, there was a care quality deficit in the two dimensions associated with the health care personnel. No care quality deficits were shown at dimension level in the new hospital. This indicates a balance between what is of importance to the respondents and how they experience the care quality while hospitalized. The scores on the PR of the dimensions associated with the care environment were significantly higher in the new hospital than in the old hospital. In addition, the scores on the SI of the physical-technical dimension were significantly higher in the new hospital than in the old hospital.
Table 2 The respondents’ Index of Measures (the difference between PR and SI at dimension level) in the old hospital and in the new hospital, respectively
The respondents’ perceptions of care quality in the old hospital compared with the new hospital
displays the comparison of the respondents’ scores on PR and on SI on item level in the old and in the new hospitals, respectively. In addition, shows the items with significantly different scores on PR from the old to the new hospital and significantly different scores on SI from the old to the new hospital. A total of 17 items showed statistically significant higher scores on PR in the new hospital compared with the old hospital, and no items were scored significantly lower. As for SI, five items were scored significantly higher in the new hospital than in the old hospital.
Table 3 Respondents’ PR and SI at item level in the old (2015) and the new high-tech hospital (2016), respectively
In the new hospital, a total of 12 items showed statistically significant differences in PR and SI scores. On five of these items, the respondents’ scores on SI are higher than the PR scores, which show a care quality deficient. On seven of these items, the respondents’ scores on PR are higher than the scores on SI and display a high-quality balance (refer for all results).
Discussion
Patients’ perceived care quality increased from the old to the new hospital in all four quality dimensions (the care environment’s physical-technical conditions and sociocultural atmo sphere and the care personnel’s medical-technical competence and identity-oriented approach) without a decrease in their scores on the SI of the care quality. This indicates that the quality of the health care received by the patients in the new hospital had increased and was in balance.Citation28 The two care quality environment dimensions’ physical-technical conditions and sociocultural atmosphere received significantly higher scores in the new hospital than in the old hospital. This is in line with results of a previous study that found that changes in patient satisfaction after hospital renovation were associated with improved room- and visitor-related satisfaction.Citation25 Previous results also show that patients with favorable impressions of the building design fared better on well-being-related outcomes relative to those with less favorable impressionsCitation23 and that the environment has a greater influence on patient’s satisfaction than just being clean and quiet.Citation34
The scores on the care personnel dimensions identity-oriented approach and medical-technical competence were higher in the new hospital, even though not significantly higher than in the old hospital. This was also the results from the study by Siddiqui et alCitation25 where no significant differences in relation to health care personnel were found. One might ask whether the technology gives the health professionals the opportunity of spending more time with the patients, which was one of the intentions with the introduction of technology. One explanation might be that when this study was conducted approximately 10 months after moving into the new, high-tech hospital health care professionals might still be struggling with adjusting to the changes in work processes. The personnel might have been less efficient in providing care while they adjust. A majority of the health care personnel in hospitals are registered nurses (RNs). A previous study found that there is a need to improve the quality of the nurse–patient interaction so as to facilitate individualized care independent of hospitals’ organizational variables.Citation35 This may be difficult, as RNs at the same time experience a conflict between their desire to provide nursing care based on the patients’ needs and preferences and factors such as cost-effectiveness policy and transparency goals for external accountability.Citation36 Future research ought to examine what health care personnel believe that the impact of the new technology has been on their provision of care and, in addition, examine the health care personnel’s views on how the systems could be improved to increase quality patient care.
On an item level, seven of the 27 items in the new hospital showed high-quality balance with PR scores significantly higher than the respective SI scores. Within the dimension of the identity-oriented approach, the patients showed high scores on the nurse and assistant nurse commitment toward them and doctors, nurses, and assistant nurses showed them respect. This study found higher perceived care quality compared to Muntlin et al’sCitation37 study from 2006 using the same questionnaire. They found that more than 20% of the patients felt that the nurses did not show any interest in their life situation. Our results are, however, in line with results from a Nordic study in which the patients showed high scores on nursing care.Citation38 Being respectful and showing commitment are important aspects of person-centered care.Citation39 Patients’ experiences of person centeredness were highlighted in one study as having an influential role in patients’ care quality experiences.Citation3 Our results are, therefore, promising for developing a more person-centered approach in hospital and hence increasing the quality of care from the patients’ perspective.
Within the environmental dimension physical-technical conditions, the patients showed high PR scores on having access to the apparatus and equipment that was necessary for their medical care and receiving food and drink that they liked. This is as expected, since the hospital trust is brand-new, with entirely new equipment, and also in line with previous research.Citation25 Within the environmental dimension sociocultural atmosphere, the patients showed high PR scores on the items concerning the fact that their relatives and friends were treated well and that they could talk to the nurse in private when they wanted to. In the new hospital, there are only single rooms and, as such, the patients can have families and friends staying and they can talk in private with the nurses and doctors. However, our results show that the number of patients staying in the corridor is the same in the new hospital as in the old one, that is, one in 10 patients. This may threaten the patients’ privacy. Results of a review on healing environment found that patients staying in multiple bed rooms and patients staying in a waiting area felt less secure and less able to control social encounters.Citation40 The main problem in the waiting area was overhearing conversations at the reception desk, which can be comparable to receiving information when staying in a bed in the corridor.
On five items, the patients scored significantly higher on SI than PR, indicating a deficit in care quality, and areas for quality improvement. Within the care personnel’s medical-technical competence dimension, the deficit concerned receiving effective pain relief and being given an examination and treatment within an acceptable waiting time. Muntlin et alCitation37 found that 20% of patients reported that they did not receive effective pain relief, and Fröjd et alCitation41 found the same, in addition to 22% not being given an examination and treatment within an acceptable waiting time. In contrast, an American study found that greater health information technology investments in hospitals were associated with shorter waiting times during hospitalization.Citation42 The hospital participating in our study is the most high-tech hospital in Norway, but at the same time, it is the fourth largest emergency hospital. This might be associated with an increase in waiting times, because critically ill patients must be prioritized.
Within the care personnel’s identity-oriented approach dimension, the quality deficit concerned receiving useful information on self-care and on which doctors were responsible for their care. This is in line with results from Muntlin et al’sCitation37 and Fröjd et al’sCitation41 studies. Both studies were made using the QPP questionnaire. Skudal et alCitation38 using the NOR-PEQ questionnaire found similar results in three different countries where the lowest scores were given to items relating to information on tests and examinations. These systems contribute to a more efficient logistics, while relieving health professionals from this job allowing them the opportunity to spend more quality time with the patients.
Having a comfortable bed received higher scores on SI than PR indicating a quality deficit. Fröjd et alCitation41 found that 22% of the patients were dissatisfied with the hospital beds in their study. One possible explanation might be that the hospital beds, old or new, are standard beds not adapted to the individual patient with their different body shapes and, therefore, different needs during rest and sleep. Another explanation might be the patients in the new hospital stay in single rooms with no other company than their own thoughts and feelings and with no natural common area to meet other patients for sharing worries and concerns. The bed can possibly be the one thing to concentrate on.
Methodological considerations
The analyses were run at a group level as the respondents were not the same in the two samples. Independent t-tests and Chi-squared tests were run to test for potential differences. The results showed no significant differences between the samples except for more men answering the questionnaire in 2016 than in 2015. The respondents in 2016 also showed an increase in their SI in the physical-technical conditions, which may reflect a general trend toward strengthened consciousness among patients as the hospital is new and modern.Citation43
The respondents were mostly younger people. The nurses on the wards/bed courts were responsible for asking patients to participate in the study. They assessed which patients could be asked based on the patient’s physical and mental health. Therefore, patients who were critically ill, or in a palliative phase, had mental disorders such as dementia and very poor mental health and were not invited to take part in the study. The results from our study cannot be generalized to these groups of patients. The problem concerning the inclusion of these groups of patients are well known from other studies.Citation13 The nurses may have assessed a patient’s condition differently, so that patients included on one ward/bed court may not have been included on another ward/bed court. The authors tried to make the nurses’ assessment as similar as possible by giving oral information and written guidelines about the inclusion criteria to the responsible nurses and further on to offer to assist the patient in completing the questionnaire.
The patients answered the questionnaire on the day before or on the day of discharge from hospital. This might be a threat to credible answers. Patients may have felt that they had to give more positive answers than they would have after discharge. They may have been unsure of possible consequences for their health care. To avoid this, the patients were asked to fill in the questionnaire when they were alone and return it in a sealed envelope. One positive aspect of answering the questionnaire before discharge is that the experiences of health care quality are still fresh and not biased by the passing of time or influenced by relatives and friends. Results that have studied the possible effect of survey timing show that the effect may also depend on the nature of the patients’ illness and the extent of their recovery.Citation6
The Cronbach’s a for the quality of care dimension scales in the questionnaire ranged between 0.54 and 0.91, which was quite similar with scores found in previous studies. The Cronbach’s a for the physical-technical dimension (0.54) was the exception. Previous studies have higher scores.Citation27,Citation29 The Cronbach’s a, however, is known to be lower for dimension scales that comprise fewer items.Citation44 The physical-technical dimension scale included only three items. It is important to collect data on the patients’ perceptions of the quality of the hospital’s physical-technical conditions, but the results must be interpreted with care. The questionnaire (QPP) is, however, validated and often used.Citation41,Citation45,Citation46
One potential limitation might be that the patients’ care quality ratings in 2015 were negatively affected by a sense of decay in the old hospital right before the move. The results from 2016 must therefore be interpreted with care, and it could be valuable to repeat the study after a year to see if the increase in patients’ care quality ratings continues.
Research shows that conducting a patient survey and using the results to improve the quality of health care are two different processes.Citation47 The usefulness of patient surveys depends on the interaction between these two processes, and there seems to be a need for developing guidelines on how to use these data in quality work on wards/bed courts.Citation48
Conclusion
Being a patient in a new high-tech hospital has increased patients’ perceptions of care quality, but the increase in care QPP was associated with improved environmental conditions, and no significant improvement in care quality was associated with the health care personnel. Health care personnel needs time to adjust to changes in work processes. Future quality improvement activities should examine how the features of a high-tech hospital can be utilized to support health care personnel to be more attentive to the individual care needs of each patient. The results gave valuable information for quality improvement in clinical practice based on the patients’ perspective.
Ethical considerations and approval
The study followed the principles of the Declaration of Helsinki.Citation49 The respondents were verbally informed and given written information stating the purpose of the study that the data would be handled confidentially and that they had the right to withdraw at any time without any consequences for them. Informed consent to participate was considered given when the respondent returned a completed questionnaire. The study was approved by the Norwegian Social Science Data Services (reference number 44034).
Author contributions
VAG and AKH designed the study. All authors collected the data, contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Acknowledgments
The authors are grateful to the respondents who participated and shared their experiences on health care quality when being hospitalized.
Disclosure
The authors report no conflicts of interest in this work.
References
- DonabedianAThe Definition of Quality and Approaches to its AssessmentAnn Arbor, MIHealth Administration Press1980
- Lov om spesialisthelsetjenesten m m592000OsloSosialog helsedepartementet2000
- EdvardssonDWattEPearceFPatient experiences of caring and person-centredness are associated with perceived nursing care qualityJ Adv Nurs201773121722727532230
- AikenLHSermeusWVan den HeedeKPatient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United StatesBMJ2012344e171722434089
- YouLMAikenLHSloaneDMHospital nursing, care quality, and patient satisfaction: cross-sectional surveys of nurses and patients in hospitals in China and EuropeInt J Nurs Stud201350215416122658468
- CrowRGageHHampsonSThe measurement of satisfaction with healthcare: implications for practice from a systematic review of the literatureHealth Technol Assess20026321244
- SofaerSFirmingerKPatient perceptions of the quality of health servicesAnnu Rev Public Health20052651355915760300
- WildeBStarrinBLarssonGLarssonMQuality of Care from a Patient PerspectiveScand J Caring Sci1993721131208248668
- DanielsenKGarrattAMBjertnaesØAPettersenKIPatient experiences in relation to respondent and health service delivery characteristics: a survey of 26,938 patients attending 62 hospitals throughout NorwayScand J Public Health2007351707717366090
- GrøndahlVAKarlssonIHall-LordMLAppelgrenJWilde-LarssonBQuality of care from patients’ perspective: impact of the combination of person-related and external objective care conditionsJ Clin Nurs20112017–182540255121749512
- JenkinsonCCoulterABrusterSRichardsNChandolaTPatients’ experiences and satisfaction with health care: results of a questionnaire study of specific aspects of careQual Saf Health Care200211433533912468693
- LarssonGWilde-LarssonBQuality of care and patient satisfaction: a new theoretical and methodological approachInt J Health Care Qual Assur201023222824721388102
- GrøndahlVAFagerliLBNursing home care quality: a cluster analysisInt J Health Care Qual Assur2017301253628105880
- ThorneLEllamushiHMtandariSMcEvoyAWPowellMKitchenNDAuditing patient experience and satisfaction with neurosurgical care: results of a questionnaire surveyBr J Neurosurg200216324325512201394
- VukmirRBCustomer satisfactionInt J Health Care Qual Assur Inc Leadersh Health Serv200619183116548396
- SjetneISVeenstraMEllefsenBStavemKService quality in hospital wards with different nursing organization: nurses’ ratingsJ Adv Nurs200965232533619040690
- AikenLHClarkeSPSloaneDMSochalskiJSilberJHHospital nurse staffing and patient mortality, nurse burnout, and job dissatisfactionJAMA2002288161987199312387650
- HendersonACaplanGDanielAPatient satisfaction: the Australian patient perspectiveAust Health Rev2004271738315362299
- OtaniKWatermanBFaulknerKMBoslaughSDunaganWCHow patient reactions to hospital care attributes affect the evaluation of overall quality of care, willingness to recommend, and willingness to returnJ Healthc Manag20105512537 discussion 3820210071
- ShenHCChiuHTLeePHHuYCChangWYHospital environment, nurse-physician relationships and quality of care: questionnaire surveyJ Adv Nurs201167234935821044136
- GrøndahlVAWilde-LarssonBHall-LordMLKarlssonIA pattern approach to analysing patients’ satisfaction and quality of care perceptions in hospitalInt J Person Center Med201114766775
- FindikUYUnsarSSutNPatient satisfaction with nursing care and its relationship with patient characteristicsNurs Health Sci201012216216920602687
- AlvaroCWilkinsonAJGallantSNKostovskiDGardnerPEvaluating intention and effect: The impact of healthcare facility design on patient and staff well-beingHERD20169282104
- LavelaSLEtingenBHillJNMiskevicsSPatient perceptions of the environment of care in which their healthcare is deliveredHERD201693314626597101
- SiddiquiZKZuccarelliRDurkinNWuAWBrotmanDJChanges in patient satisfaction related to hospital renovation: experience with a new clinical buildingJ Hosp Med201510316517125652720
- MønstedTFossumKBuilding for the Next Generation: Practical Challenges for Platformization at a Norwegian HospitalNorwayUniversity of Oslo2018
- Wilde LarssonBLarssonGDevelopment of a short form of the Quality from the Patient’s Perspective (QPP) questionnaireJ Clin Nurs200211568168712201896
- LarssonGWilde-LarssonBQuality improvement measures based on patient data: some psychometric issuesInt J Nurs Pract20039529429914531851
- LarssonBWPatients’ views on quality of care: age effects and identification of patient profilesJ Clin Nurs19998669370010827616
- HenochILövgrenMWilde-LarssonBTishelmanCPerception of quality of care: comparison of the views of patients’ with lung cancer and their family membersJ Clin Nurs2012213–458559422150995
- FieldADiscovering Statistics Using IBM SPSS Statistics4th edUKSage2013
- TabachnickBGFidellLSUsing Multivariate Statistics6th edBoston, MAAllyn & Bacon/Pearson Education2007
- PolitDFBeckCTNursing Research: Generating and Assessing Evidence for Nursing Practice8th edBaltimore, MDLippincott Williams & Wilkins2008
- MacAllisterLZimringCRyherdEEnvironmental variables that influence patient satisfaction: A review of the literatureHERD201610115516927492078
- SuhonenRVälimäkiMKatajistoJLeino-KilpiHHospitals’ organizational variables and patients’ perceptions of individualized nursing care in FinlandJ Nurs Manag200715219720617352703
- KieftRAde BrouwerBBFranckeALDelnoijDMHow nurses and their work environment affect patient experiences of the quality of care: a qualitative studyBMC Health Serv Res20141424924923663
- MuntlinAGunningbergLCarlssonMPatients’ perceptions of quality of care at an emergency department and identification of areas for quality improvementJ Clin Nurs20061581045105616879549
- SkudalKEGarrattAMErikssonBLeinonenTSimonsenJBjertnaesOAThe Nordic Patient Experiences Questionnaire (NORPEQ): cross-national comparison of data quality, internal consistency and validity in four Nordic countriesBMJ Open201223e000864
- McCormackBDewingJMcCanceTDeveloping person-centred care: addressing contextual challenges through practice developmentOnline J Issues Nurs20111623
- HuismanERCMMoralesEvan HoofJKortHSMHealing environment: A review of the impact of physical environmental factors on usersBuild Environ2012587080
- FröjdCSwenneCLRubertssonCGunningbergLWadenstenBPatient information and participation still in need of improvement: evaluation of patients’ perceptions of quality of careJ Nurs Manag201119222623621375626
- LeeJThe impact of health information technology on disparity of process of careInt J Equity Health2015141725566790
- LarssonGWilde-LarssonBChanges over time in the importance patients ascribe to different aspects of care: on the need to improve person-centerednessInt J Person Center Med201223482490
- StreinerDLNormanGRCairneyJHealth Measurement Scales: A Practical Guide to their Development and Use5th edUSAOxford University Press2015
- LarssonBWLarssonGChantereauMWvon HolsteinKSInternational comparisons of patients’ views on quality of careInt J Health Care Qual Assur Inc Leadersh Health Serv2005181627315819128
- RahmqvistMBaraACPatient characteristics and quality dimensions related to patient satisfactionInt J Qual Health Care2010222869220133477
- PatwardhanASpencerCHAre patient surveys valuable as a service-improvement tool in health services? An overviewJ Healthc Leadersh201243346
- HaugumMDanielsenKIversenHHBjertnaesOThe use of data from national and other large-scale user experience surveys in local quality work: a systematic reviewInt J Qual Health Care201426659260525142685
- MillumJWendlerDEmanuelEJThe 50th anniversary of the Declaration of Helsinki: progress but many remaining challengesJAMA2013310202143214424141885
