Abstract
Background:
Plantar fasciitis is a common condition routinely managed by podiatrists in the community and is widely treated conservatively. Two commonly used treatments for plantar fasciitis are customized functional foot orthoses and corticosteroid injections. While common to clinical practice, the evidence base underpinning these treatment strategies is unknown. Therefore, the aim of this systematic review was to assess the effectiveness and safety of customized functional foot orthoses and corticosteroid injections in the treatment of plantar fasciitis.
Methods:
A systematic literature search was conducted. Experimental studies, in English, from 1998 to 2010 were accepted for inclusion in this review. The PEDro quality assessment tool and the National Health and Medical Research Council’s hierarchy of evidence were used to assess the quality of the included studies.
Results:
Six randomized controlled trials which met the selection criteria were included in this review. Four reported on customized functional foot orthoses and 2 on corticosteroid injections. Current best available evidence highlights that both customized functional foot orthoses and corticosteroid injections can lead to a decrease in pain associated with plantar fasciitis. Additionally, customized functional foot orthoses may also provide an additional benefit in terms of increased functional ability in patients with plantar fasciitis. Corticosteroid injections may have side effects, especially pain (from the injection).
Conclusion:
Both customized functional foot orthoses and corticosteroid injections can lead to reduction in pain associated with plantar fasciitis. While customized functional foot orthoses may increase the functional outcomes in patients with plantar fasciitis, corticosteroid injections may have side effects (especially pain as a result of the injection), which may limit its acceptability.
Introduction
Evidence-based practice (EBP) is now a firmly entrenched philosophy for providing both safe and quality health care. Evidence based practice is defined as “the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients”Citation1 and is underpinned by 3 equally important concepts, namely, best research evidence, clinical expertise and patient values.Citation1 While the importance of EBP is universally recognized, EBP in podiatry is still in its infancy. Podiatry’s foray into EBP is shrouded by a lack of rigorous high quality evidence, limited research capability and/or opportunities for podiatrists, and barriers in accessing and implementing evidence into clinical practice.Citation2,Citation3 However, with increasing emphasis on EBP in health care, podiatrists too are required to ensure their practices are underpinned by current best research evidence.
Plantar fasciitis is a common condition routinely managed by many podiatrists in the community, as they are primary contact practitioners. Therefore, it is essential that podiatry management strategies for plantar fasciitis are underpinned by EBP principles to ensure that optimal outcomes are attained. Although most commonly described as an inflammatory condition (plantar fasci’itis), researchers have questioned the presence of inflammation in this condition.Citation4,Citation5 Plantar fasciitis is reported to commonly occur in runners and those who are overweight.Citation6–Citation9 Furthermore, research indicates that 10% of the general population will also experience this pathology at least once in their lifetime.Citation6,Citation7,Citation10 The most commonly reported symptom of plantar fasciitis is described as “first-step pain”, though plantar heel pain in general can be broadly associated with plantar fasciitis within the literature.Citation6,Citation9,Citation11
The plantar fascia, also known as the plantar aponeurosis is a broad, flat, fibrous, tendon-like structure, which consists of noncontractile irregularly ordered collagen fibers with minimal elastic properties.Citation12,Citation13 It originates from behind the medial tubercle of the calcaneus and then divides distally in the area of the metatarsal heads into both its superficial and deep segments. The superficial fibers insert into the skin, whilst the deep segments attach to the transverse metatarsophalangeal ligaments and to the plantar surface of the proximal digits.Citation13 The plantar fascia provides stability to the arch of the foot and aids in re-supination of the foot during propulsion.Citation14,Citation15
Conservative treatments remain popular for many patients with plantar fasciitis. A recent clinical practice guideline, recommends a number of conservative interventions in the management of plantar fasciitis.Citation16 Among these conservative treatment options prefabricated foot orthoses (PFO), customized functional foot orthoses (CFO) and corticosteroid injections feature regularly (CSI).Citation7–Citation11,Citation16–Citation22
Clinicians may be led to the use of PFO and CFO for the treatment of plantar fasciitis, in the belief that these provide a mechanical correction to the poor and/or altered biomechanics of the symptomatic foot, ultimately relieving the symptoms associated with plantar fasciitis.Citation6 This treatment may be seen as having clinical benefit, as the clinician is trying to address the etiology of the condition, rather than simply “masking” the symptoms. Conversely, clinicians may look to use CSI as their treatment of choice as they are often considered a “quick fix”, are relatively easy to administer, and time and resource efficient.
These conservative treatments are routinely used in clinical practice, and widely recommended, yet there is no evidence based consensus on the most effective treatment for plantar fasciitis. Emerging evidence suggests that both CSI and PFO should be considered as part of the “tier 1 treatment options”, whilst CFO should be considered as part of the “tier 2 treatment options”. However, the evidence base underpinning these recommendations could be considered to be low level and low quality.Citation23 Despite this limited evidence base, in clinical practice, CFO and CSI remain popular, possibly driven by patient expectations and fee for service model. Confounding these issues are the known side effects, discomfort, and injection pain respectively for the use of CFO and CSI.Citation4,Citation5,Citation23–Citation26
Preliminary scoping search of the literature identified no study directly comparing CFO to CSI for the treatment of plantar fasciitis. In the absence of direct comparison between the two, literature which contained either of these as treatment options (with alternate comparators) was considered. Therefore, the primary aim of this systematic review was to assess the effectiveness of CFO and CSI in the management of plantar fasciitis. The secondary aim of this review was to report on the safety and, in particular, the side effects, associated with the use of these two interventions.
Methods
Data sources
Electronic databases were searched (Ovid [Medline], EMBASE, AMED, PubMed, SportDiscus, CINAHL, Cochrane Library, and AUSPORT) up to December 2010. The following search term combinations were used:
orthotic* or orthoses or functional foot orthotic* or functional foot orthoses or insert* or insole* AND plantar fasciitis or anterior medial heel pain or plantar heel pain or heel spur syndrome or painful heel syndrome or plantar aponeurosis
cortisone inject* or corticosteroid* inject* or steroid shot* or steroid injection AND plantar fasciitis or anterior medial heel pain or plantar heel pain or heel spur syndrome or painful heel syndrome or plantar aponeurosis. (*Indicates truncation)
Study selection
Only properly designed randomized control trials (RCT), which are considered to be level II in the hierarchy of evidence (National Health and Medical Research Council’s [NHMRC] designation of levels of evidence), from the past decade, published as peer review journal articles were accepted for inclusion in this review. In the interests of accessing best evidence for this review, only the highest level of RCT (level II) were sought after for inclusion into this review. For the study to be considered a properly designed randomized control trial, the method of randomization needed to be both rigorous and adequately described. Alternate allocation and other means, such as date of birth and sequential, are not considered rigorous techniques of randomization. With rigorous randomization process, there is equal probability of participants being allocated to each and every treatment group.Citation27 Inadequate randomization can lead to incorrect higher estimation of treatment effects, resulting in introduction of bias in the methodology.Citation27 For this reason, inadequate randomization techniques, and studies without adequate descriptions of randomization methods, were not considered for inclusion into this review. The other limiters include English language publications and research in human subjects only.
Only subjects with a diagnosis of plantar fasciitis were included as the population group. Custom made functional foot orthoses needed to be a pair of in-shoe devices that were moulded or milled from impressions of the feet, whether by plaster cast or 3D laser scan. The fabrication then needed to be carried out according to practitioner-prescribed specifications.Citation28 The CSI treatment had to involve an injection of a corticosteroid solution into the area of the plantar fascia.
Types of comparators included were, but not limited to: Achilles’ tendon and plantar fascia stretching programs, extracorporeal shock wave therapy, manipulations of the foot and ankle, prefabricated foot orthoses, night splints (calf and/or plantar fascia), true “sham” foot orthotic devices and autologous blood injections.
Pain and function were chosen as the outcome measures of interest as these measures are routinely collected and reported in clinical practice.
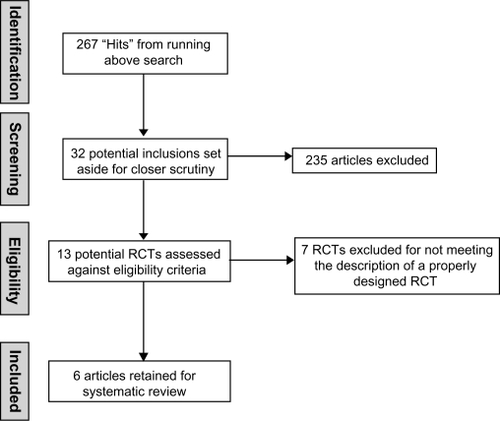
Authors HU and EB reviewed all potential search “hits” following the results of the above literature search. The full text, the abstract, or the design methodology was used to ascertain the relevance of the article to this review. Any potential articles were set aside for further scrutiny and then from these, the final articles were selected.
Methodological quality assessment
The authors collaboratively assigned the chosen articles to the appropriate level of hierarchy with the NHMRC designation of level of evidence categories.Citation29 PEDro quality assessment tool was applied to the included articles by both HU and EB independently. Any discrepancies in the assigned marks were addressed during discussions between HU and EB until agreement was found. The PEDro assessment tool contains 11 domains (10 included in the final score) which appraise the methodological rigor of randomized control trials and clinical control trials.Citation30
Data extraction
The data were extracted independently by HU and EB using the same data extraction table. The data tables were then compared and any difference in the data collection was further scrutinized until resolution was found. Demographic data were collected pertaining to the subjects within the selected studies, as were the outcome measures utilized and the results of the within-group changes for each treatment arm of interest. Data relevant to the information utilized by the PEDro instrument were also collected.Citation30
Results
Search results
Six properly designed RCTs (level II evidence) were retained for this systematic review.Citation6,Citation9,Citation20,Citation23,Citation31,Citation32 Seven pseudo-randomized trials were identified from the literature but due to an inadequate randomization process or the absence of randomization description, were excluded from this review.Citation8,Citation11,Citation17,Citation19,Citation33–Citation35 A summation of both the included and excluded studies can be found in . provides an overview of the literature selection process.
Table 1 Included and excluded randomized controlled trials
Four studies investigated the effectiveness of CFO.Citation6,Citation9,Citation20,Citation32 The study by Roos and colleaguesCitation6 randomized a total of 43 subjects into a CFO group (n = 10 at final), a night splint group (n = 15 at final) or a combined night splint and CFO group (n = 13 at final). Assessment measurements of pain and function were measured at baseline; 6, 12, 26, and 52 weeks. Landorf and colleaguesCitation9 recruited a total of 136 participants initially and randomized them into 1 of 3 groups; a sham orthotic group (n = 43 at final), a prefabricated orthotic group (n = 43 at final), or a CFO group (n = 45 at final). The outcomes of pain and function were measured at 3 and 12 months post intervention. The study by Dimou and colleaguesCitation20 randomly allocated 20 subjects into either group: 1 which received chiropractic adjustments of the foot and ankle twice a week for 4 weeks (n = 10) or group 2 which received a pair of CFO to wear for 8 weeks (n = 10). The outcome of pain was measured subjectively and objectively, using an Algometer, at baseline, day 15, day 29, and then at 1 month. Baldassin and colleaguesCitation32 initially randomized 142 participants to either a prefabricated orthoses group (n = 72) or a CFO group (n = 70). The outcome of pain was measured at baseline, 4 weeks, and 8 weeks. The primary pain outcome was a modified subscale of the Foot Function Index (FFI), whilst the secondary pain outcome was pain elicited by palpation of the medial calcaneal tuberosity. Data were complete at final analysis for 54 participants in the prefabricated group and 51 participants in the CFO group. No “intention to treat” approach was applied to statistical analysis.
The remaining 2 studies evaluated the effectiveness of CSI.Citation23,Citation31 Porter and ShadboltCitation23 recruited a total of 125 patients and randomized them into group A (n = 64 heels), which received 1 injection of a corticosteroid and group B (n = 61 heels) which received electro hydraulic shock wave therapy (ESWT). Both groups performed a standard stretching program for gastrocnemius, soleus, and plantar fascia. A third group C consisted of 19 “heels” that were eligible for the study but refused either a CSI or ESWT treatment and therefore only performed the stretching exercises. All patients were assessed for pain measures at baseline, 3 months, and 12 months. Lee and AhmadCitation31 randomized 64 participants into an autologous blood intralesional injection (n = 30) or CSI treatment group (n = 31). The outcome measure of pain was taken at baseline, 6 weeks, 3 months, and 6 months post treatment.
An overview of the psychometric properties for the outcome measures reported in the included studies is summarized in . A range of different outcome measures, including subjective and objective measures were reported. Subjective measures often related to pain severity and intensity (such as the Visual Analog Scale, Numeric Pain Rating Scale, and First Step Pain Scale) and also included measures of the impact of pain on function (Foot Health Status Questionnaire). Objective measures were primarily related to palpation findings (such as Tenderness Threshold). While psychometric properties of most of these outcome measures were recognized and reported, one study by Dimou and colleaguesCitation20 did not justify the psychometric properties of the First Step Pain Scale and the “Effect of Heel Pain on 3 Different Activities” form.
Table 2 Outcome measures – psychometric properties
Roos et alCitation6 reported no significant difference in pain scores (at any measurement points) between the 3 groups. When comparing the CFOs and the splint-only group, a clinically important difference in sport and recreation was observed at 26 weeks (assumed to be an increase in participation, but not stated). In addition, at 52 weeks the groups that were treated with CFOs reported a significantly higher pain reduction when compared with the splint alone group.
Landorf et alCitation9 also reported a reduction in pain between study groups, but not a statistically significant reduction. Prefabricated foot orthoses and CFO were shown to cause a statistically significant improvement in function when compared with sham orthoses in the short term (3 months) but not in the long term (12 months). Dimou et alCitation20 reported a significant difference for pain between the chiropractic treatment group and the CFO treatment group, with the chiropractic group being superior.
Baldassin and colleaguesCitation32 when comparing the effectiveness of low-cost prefabricated and customized foot orthoses, reported that both groups had similar outcomes. The findings from this study indicate that while there was a significant improvement in outcomes (both in pain and function) when compared with baseline, there were no differences between the groups at 4 and 8 weeks post intervention. These findings indicate that low-cost prefabricated orthoses are at least as effective in reducing pain and improving function as customized orthotic devices.
The 2 studies which investigated the use of CSI demonstrated statistically significant reductions in pain with between group comparisons.Citation23,Citation31 However, Porter and Shadbolt reported that at 12 months the CSI and ESWT group had similar levels of average pain while the control group had significantly higher levels of pain.Citation23 Similarly, Lee and Ahmad’s study reported the corticosteroid group to show a significant reduction in pain on the visual analog scale at both 6 weeks and 3 months in comparison to the autologous blood group.Citation31 However, this change was not significant at 6 months.
provides a summary of within-group change from baseline to follow-up. There was a consistent finding of decreased pain across all studies, irrespective of the intervention. A clear trend was noticed across 4 of the studies with a reduction in pain.Citation6,Citation9,Citation23,Citation31 This result was statistically significant within 3 of these 4 studies, Dimou et al being the notable exception with nonsignificant results.Citation20 Function was reported in only 2 of the reviewed studies, which both contained a customized functional foot orthoses treatment arm.Citation6,Citation9 Both studies reported a statistical improvement of function at each of the points of assessment. It was of note that none of the studies which investigated corticosteroid injections used function as an outcome measure.Citation23,Citation31
Table 3 Within-group change from baseline to follow-up
Little information was provided about the safety of CFO’s and corticosteroid injections in the included studies. Of the 4 studiesCitation6,Citation9,Citation20,Citation32 which investigated CFO, only one commented on the side effects of their use.Citation6 Roos et alCitation6 reported pressurerelated foot pain and tiredness of the foot in 3 of their subjects. Noncompliance with customized functional foot orthoses, a common clinical observation, was not reported in any of the studies. Both studiesCitation23,Citation31 which investigated corticosteroid injections reported side effects as a result of their use. Porter and ShadboltCitation23 reported that all of the patients found the corticosteroid injection painful. Of the 64 heels injected, 8 cases required analgesia and/or ice application for post-injection pain. Similarly, in the study by Lee and Ahmad all of the patients found the corticosteroid injection painful.Citation31 Of their cohort, 12.9% also experienced post-injection pain which required analgesia and/or ice application.Citation31 The post-injection pain was said to have continued for a mean duration of 5 and 7 days respectively.Citation23,Citation31
The methodological rigor of the included articles was assessed using the PEDro instrument.Citation29 A breakdown of the individual domain scores is provided in Appendix 1 (the higher the score out of 10, the less methodological bias within the study). Blinding of the subjects, the therapist, and/or the assessor were the domains on which most of the studies were flawed. In terms of blinding, only Baldassin et alCitation32 and Landorf et alCitation9 adequately fulfilled these criteria. Small sample sizes were also a characteristic of many of the included studies, with only three studiesCitation6,Citation9,Citation32 reporting power analyses to determine sample sizes.
Discussion
A systematic review, by its very nature, aims to evaluate best available research evidence, within a particular field of practice, with particular emphasis on rigor, precision, and generalizability. Within fields of practice where evidence is sparse, mixed and/or inconclusive, a systematic review of the current best available evidence provides useful information on current implications for practice and future research. The decision on whether to use CFO or CSI for the treatment of plantar fasciitis is one such area where the current best available evidence needs to be established.
The findings from this systematic review highlight several opportunities for reflection. Surprisingly, despite extensive literature interrogation, we were unable to find any high level evidence which compared effectiveness of CFOs with CSIs, despite these 2 treatments being widely promoted, recommended, and practiced in clinical practice.
The limited evidence base we did identify did pose unique challenges. The between-group results for the articles which contained a CFO treatment arm were mixed.Citation6,Citation9,Citation20 The only statistically significant finding was that from the study by Landorf et al, where the CFO group and the prefabricated foot orthoses group were both superior to the sham group in respect to functional outcome in the short term (3 months).Citation9 Similarly, the 2 articles which contained a CSI treatment armCitation23,Citation31 demonstrated statistically significant improvements in pain in comparison with the other treatment arms but only in the short term.
The articlesCitation6,Citation9,Citation20,Citation32 that investigated the effectiveness of customized functional foot orthoses were able to show a within-group reduction in pain at each and every assessment point. The study by Roos et alCitation6 and Landorf et alCitation9 contained the longest follow-up at 52 weeks post-intervention. This is in contrast to the Dimou et alCitation20 study which evaluated only once at 8 weeks post-intervention. Baldassin et alCitation32 also reported similar findings with positive outcomes at 4 and 8 weeks post intervention.
All 4 studies scored well (8 points) in the PEDro appraisal, indicating only minor issues with methodological quality. The main drawback was a lack of blinding of subjects and therapists in Baldassin et al,Citation32 Roos et al,Citation6 and Dimou et al,Citation20 which is to be expected given the nature of the intervention. The research by Dimou et alCitation20 also utilized outcome measures with poor psychometric properties.
A within-group reduction in pain at each and every assessment point was also found in the 2 articles that assessed the efficacy of corticosteroid injections.Citation23,Citation31 A statistically significant reduction in pain was reported at each of these measurement points. Both studies evaluated outcomes at 52 weeks post-intervention, at which time a reduction in pain was still reported for the use of this treatment. However, both of these studies were constrained by similar methodological flaws (both with a PEDro score of 6). The threats to internal validity in these studies included failure to blind the subjects, therapist and assessor, and failure to instigate an intention-to-treat analysis.
Function was assessed in the studies by Landorf et al,Citation9 Baldassin et al,Citation32 and Roos et al.Citation6 All these studies investigated the effectiveness of CFO and demonstrated a statistically significant increase in function at each of the measurement points. Adding to the strength of these results, all studies utilized outcome measures that had reported validity and/or reliability outcomes for their use within the literature.Citation6,Citation9,Citation32 Considering that foot pathologies can have a profound effect on functional ability, it is interesting to note that not all studies attempted to measure function.
The risk factors for the use of CSI include plantar fascial rupture, hypoglycemia in diabetic patients, skin and fat-pad atrophy, and sepsis.Citation4,Citation24,Citation25 However, this was not supported by evidence from the included studies. Neither of the studies involving a corticosteroid injection reported any such occurrences.Citation23,Citation31 Pain was however the primary risk factor reported consistently within these 2 studies. Universally, subjects in both the Porter and Shadbolt studyCitation23 and the study by Lee and AhmadCitation31 found the CSI painful. Not only was there injection pain but the associated post-injection pain was said to have continued for a mean duration of 5 and 7 days respectively.Citation23,Citation31 With regards to customized functional foot orthoses, only 1 study reported pain with the use of CFO.Citation6
Limitations of this review
This systematic review, like any other research, has its limitations. The very nature of a systematic review ensures a very specific, targeted body of literature is identified, accessed, evaluated, and synthesized. As the review only included published, English language literature, the potential for publication and language bias should be acknowledged. While the authors made all attempts to identify and access all relevant studies, it is possible, due to differing terminologies, access to databases and journals, some may have been missed. There is also a paucity of evidence on cost-effectiveness and long term effectiveness of CFO and CSI for plantar fasciitis. Finally, this review is based on a modest body of evidence (6 RCTs) which were underpinned by several methodological flaws (such as small sample sizes). While the quantity and quality of primary research is beyond the reviewers’ control, these limitations must be acknowledged when considering the findings from this review.
Conclusion
Currently there is limited research evidence which compares the effectiveness of CFO with CSI in the treatment of plantar fasciitis. This is an important evidence gap that needs to be addressed as plantar fasciitis is a commonly seen condition in clinical practice and clinicians are regularly confronted with needing to make informed decisions about CFO or CSI. Current best available evidence, with its inherent limitations, highlights that both CFO and CSI can lead to a decrease in pain associated with plantar fasciitis. Additionally, CFO may also provide an added benefit in terms of increased functional ability in patients with plantar fasciitis. In terms of harm and side effects, CSI may result in pain (from the injection). Clinicians using CFO and CSI should be aware of the limited evidence base and therefore routine use of CFO and CSI for plantar fasciitis should be carefully monitored and inform patient outcomes. This systematic review highlights current evidence gaps for two popular and increasingly accessible treatments for plantar fasciitis and emphasizes the importance of conducting ongoing high quality research in this area.
Implications for clinicians
As CFO and CSI seem to provide similar benefits for patients with plantar fasciitis, both these treatments could be considered as treatment options for plantar fasciitis. However, it is worthwhile to note that one of the side effects of CSI was pain as a result of the treatment procedure. While this may suggest an approach which favors CFO, which had minimal side effects reported in the literature, the cost of CFO may need to be considered. This scenario underscores the importance of collaborative decision making between the clinician and the patient, informed by best available evidence.
Implications for future research
Further research, such as RCTs, with sound methodological rigour, are required to investigate the effectiveness of CFO and CSI by directly comparing these 2 interventions. Future RCTs could also investigate the influence of the natural health course of plantar fasciitis by employing sham or a placebo group. As RCTs are time and resource intensive, it is likely that, in the short term at least, there will be an ongoing paucity of high quality literature. To address these gaps in the short term, well designed case studies can contribute to the evidence base for CFO and CSI. Future research should also focus on the cost effectiveness and long term effectiveness (including safety and side effects) of these two common treatment strategies.
Authors’ contributions
HU and EB contributed to the conceptualization of the topic and the synthesis of all data. HU contributed to the development of the manuscript. SK contributed to the development, editing, and reviewing of the manuscript.
Disclosure
The authors declare that they have no competing interests.
References
- SackettDLRosenbergWMCMuir GrayJAEvidence based medicine: what it is and what it isn’tBMJ199631271728555924
- KeenanAMRedmondACIntegrating research into the clinic – What evidence based practice means to the practicing PodiatristJ Am Podiatr Med Assoc20029211512211847266
- HawkeFBurnsJLandorfKBEvidence-based podiatric medicine – Importance of systematic reviews in clinical practiceJ Am Podiatr Med Assoc20099926026619448181
- LemontHAmmirartiKMUsenNPlantar fasciitis – A degenerative process (Fasciosis) without inflammationJ Am Podiatr Med Assoc20039323423712756315
- VohraPKKincaidBRJapourCJUltrasonographic evaluation of plantar fascia bands – A retrospective study of 211 symptomatic feetJ Am Podiatr Med Assoc20029244444912237265
- RoosEMEngstromMSoderbergBFoot orthoses for the treatment of plantar fasciitisFoot Ankle Int20062760661116919213
- LandorfKBKeenanAMHerbertRDEffectiveness of different types of foot orthoses for the treatment of plantar fasciitisJ Am Podiatr Med Assoc20049454254915547121
- LynchDMGoforthWPMartinJEConservative treatment of plantar fasciitis – A prospective studyJ Am Podiatr Med Assoc1998883753809735623
- LandorfKBKeenanAMHerbertRDEffectiveness of foot orthoses to treat plantar fasciitis: a randomized trialArch Intern Med20061661305131016801514
- SeligmanDADawsonDRCustomized heel pads and soft orthotics to treat heel pain and plantar fasciitisArch Phys Med Rehabil2003841564156714586928
- MartinJEHoschJCGoforthWPMechanical treatment of plantar fasciitis: a prospective studyJ Am Podiatr Med Assoc200191556211266478
- TortoraGJGrabowskiSRPrinciples of Anatomy and Physiology7th edNew YorkBiological Sciences Textbooks, Harper Collins College Publisher1992
- MariebENHuman Anatomy and Physiology5th edSan FranciscoBenjamin Cummings2001
- MichaudTCFoot Orthoses and Other Forms of Conservative Foot CareMassachusettsLippincott, Williams & Wilkins1997
- LisowskiFPA Guide to Dissection of The Human Body2nd edSingaporeWorld Scientific Publishing Company2004
- ThomasJLChristensenJCKravitzSRThe diagnosis and treatment of heel pain: a clinical practice guideline – revision 2010J Foot Ankle Surg201049119
- PfefferGBacchettiPDelandJComparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitisFoot Ankle Int19992021422110229276
- RomeKGrayJStewartFEvaluating the clinical effectiveness and cost-effectiveness of foot orthoses in the treatment of plantar heel pain: a feasibility studyJ Am Podiatr Med Assoc20049422923815153583
- TurlikMADonatelliTJVeremisMGA comparison of shoe inserts in relieving mechanical heel painThe Foot199998487
- DimouESBrantinghamJWWoodTRandomized, controlled trial (with blinded observer) of chiropractic manipulation and achilles stretching vs orthotics for the treatment of plantar fasciitisJournal of the American Chiropractic Association2004413242
- GrossMTByersJMKrafftJLThe impact of custom semirigid foot orthotics on pain and disability for individuals with plantar fasciitisJ Orthop Sports Phys Ther20023214915711949663
- CrawfordFThomsonCEInterventions for treating plantar heel pain (Review)Cochrane Database Syst Rev20033CD00041612917892
- PorterMDShadboltBIntralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathyClin J Sport Med20051511912415867552
- SpeedCACorticosteroid injections in tendon lesionsBMJ200132338238611509432
- TsaiWCScuCCChenCPPlantar fasciitis treated with local steroid injection: comparison between sonographic and palpation guidanceJ Clin Ultrasound200634121616353228
- ValmassyRLClinical Biomechanics of the Lower ExtremitiesSt. LouisMosby Year Book1996
- SoucacosPNJohnsonEOBabisGRandomised controlled trials in orthopaedic surgery and traumatology: Overview of parameters and pitfallsInt J Care Injured200839639642
- HawkeFBurnsJRadfordJAdu ToitVCustom-made foot orthoses for the treatment of foot painCochrane Database Syst Rev20083CD00680118646168
- National Health and Medical Research Council [homepage on the Internet]AustraliaA Guide to the Development, Implementation and Evaluation of Clinical Practice Guidelines [updated 2010 July 20] http://www.nhmrc.gov.au. Accessed March 18, 2011.
- PEDro [home on the Internet]AustraliaPhysiotherapy Evidence Database [updated 2011 March 7] http://www.pedro.org.au/. Accessed March 18, 2011.
- LeeTGAhmadTSIntralesional autologous blood injection compared to corticosteroid injection for treatment of chronic plantar fasciitis: a prospective, randomized, controlled trialFoot Ankle Int20072898499017880872
- BaldassinVGomesCRBeraldoPSEffectiveness of prefabricated and customized foot orthoses made from low – cost foam for no complication plantar fasciitis: A randomized controlled trialArch Phys Med Rehabil20099070170619345789
- KalaciACakiciHHapaOYanatANDogramiciYSevincTTTreatment of plantar fasciitis using four different local injection modalities: A randomized prospective clinical trialJ Am Podiatr Med Assoc20099010811319299346
- MulherinDPriceMEfficacy of tibial nerve block, local steroid injection or both in the treatment of plantar heel pain syndromeFoot (Edinb)2009199810020307457
- YucelIOzturanKEDemiraranYDegirmenciEKaynakGComparison of high-dose extracorporeal shockwave therapy and intralesional corticosteroid injection in the treatment of plantar fasciitisJ Am Podiatr Med Assoc201010010511020237361