Abstract
Objective
In recent years, the use of information and communication technologies (ICTs) has increased in various sectors, among which the healthcare service is no exception. However, studies have mostly focused on the use of ICTs among patients with chronic diseases, with few reports on the advantages and barriers of these technologies among physicians, particularly in Latin America. We designed this study to fill in the gap, as an objective assessment of the frequency of use, perceptions, and barriers of ICTs among physicians remains crucial for a successful implementation of these technologies into the mainstream medical practice.
Methods
We conducted an anonymous cross-sectional survey-based study in 640 Ecuadorian physicians. The survey used consisted of 13 items and evaluated the frequency of use, perceptions, and barriers of ICTs among physicians. Chi-square tests for goodness of fit and independence were performed, whilst Phi coefficient was interpreted to assess the strength of associations. Fisher exact test was performed when required.
Results
Over 90% of physicians reported the use of ICTs to message other colleagues and patients (p=0.000). While 89.5% of physicians used social media to interact with other colleagues, only 58.1% used them to interact with patients (p=0.000). Most participants reported the use of ICTs to search for academic information (p=0.000). Moreover, more than 80.0% agree that ICTs may be used to promote health and medical services, search new job opportunities, get involved in research projects and promote teamwork with colleagues. However, 83.6% of physicians expressed concerns about privacy and patient confidentiality, while 53.8% stated that they lacked the time to use ICTs.
Conclusion
High usage of ICTs was found among Ecuadorian physicians. Younger physicians, with less postgraduate years, and non-specialists were more likely to have a positive perception toward ICTs. Privacy and patient confidentiality, followed by time management, were the most reported barriers in our study.
Introduction
In recent years, information and communication technologies (ICTs) have presented a significant increase in their use in various sectors, among which the healthcare service is no exception.Citation1 Such growth has been even more pronounced with the use of mobile devices, through which ICTs offer accessible opportunities to improve efficiency and reduce costs in exchange for greater patient coverage and health system management.Citation1 This led to the World Health Organization (WHO) in 2010 to incorporate electronic health (e-health) as a concept that encompasses the cost-effective and secure use of ICTs in support of health and health-related fields, including healthcare services, health surveillance, health literature, health education, knowledge and research.Citation2
Several publications have recognized ICTs as useful tools for health education in developing countries, as well as opportunities for improving quality of life interventions, care provided to patients, and for better healthcare system organization.Citation3–Citation5 Moreover, ICTs have been shown to be useful in health promotion and primary prevention, even among older adults, as well as other applications. In any case, it is important to acknowledge the fact that although ICTs provide new benefits, it also brings with it new challenges, many of which represent a burden to the physician. For instance, training and management of these technologies, prolonged working time, conflicting priorities, lack of knowledge, absence of legal guidelines on privacy and confidentiality are some of the issues a care provider should be ready to handle.Citation1,Citation6,Citation7
Current studies have mostly focused on the use of ICTs among patients with chronic diseases; however, there are fewer reports on the advantages and barriers of ICTs among physicians, particularly in Latin America. Moreover, variability in perceived usability and practice behavior change by ICTs for the dissemination of clinical practice guidelines has been reported, suggesting that patterns and preferences for ICTs might exist.Citation8,Citation9 Whilst the incorporation of ICTs in medical practice cannot be fully understood and stated without exploring the ways physicians are applying ICTs within their daily practice, organizational contexts and the opportunities and challenges afforded by institutional, professional and patient demands; it is certain that despite the fact that potential benefits of emerging technologies exist, there are still noticeable gaps regarding the adaptation of mainstream medical practices to the ubiquitous use of the internet by patients.Citation10,Citation11 Not only that but also the fact that skepticism among doctors who do not necessarily look ICTs as innovative or desirable has been reported which is further dimed by a high rank of hampering factors such as data security and privacy, as well as the acceptance by patients advocates.Citation12 We designed this study to fill in the gap, as an objective assessment of the frequency of use, perceptions, and barriers of ICTs among physicians remains crucial for a successful implementation of these technologies into the mainstream medical practice.
Methods
Study Design and Population
We conducted an anonymous cross-sectional survey study, in which 640 Ecuadorian physicians, both, general practitioners and specialists, rated their frequency of use, perceptions, and barriers regarding ICTs. Inclusion criteria required the participants to have an active medical practice in Ecuador, regardless of the field of expertise.
Procedures
The questionnaire was designed using the data provided by other publications, as well as the recommendations of an expert panel of physicians, who evaluated potential items to be included.Citation13–Citation15 The final questionnaire assessed the frequency of use of ICT’s by physicians for professional purposes and towards communication with their patients, as well as the perceptions and limitations that ICTs represent to physicians in their practice.
To assess the reliability and validity of the prototype questionnaire, a pilot study was conducted with 30 physicians. Cronbach’s alpha equation was applied, and the reliability coefficient was calculated for the questions of interest, which were grouped into three constructs: frequencies (Q9.1- Q10.19), perceptions (Q11.1–11.7) and barriers (Q12.1–12.4). All the reliability coefficients were found to be above 0.70. The final survey and reliability analyses are included in Table S1.
The survey collected demographic information of each participant. Physicians were asked to quantify their use of each technology to communicate (SMS, e-mail, Line, WhatsApp, Hangouts, Vibe, Facebook messenger and Telegram) and interact through social media (Blogger, Facebook, Google plus, Instagram, Pinterest, Scrib, Slideshare, Snapchat, Tumblr, Twitter, Youtube) with either professionals or patients, as well as for academic research (Academia.edu, Google Scholar, LikendIn, Medscape, Pubmed, Researchgate, Scopus, UptoDate, and Yammer) under a specific scale (daily, at least once a week, at least once a month, less than once a month, or never). Furthermore, perceptions and barriers upon the use of ICTs were measured on a Likert Scale addressing interest (strongly disagree, disagree, neutral, agree, strongly agree).
Before taking the questionnaire, physicians were instructed about the purpose of the study and their role in it. During the survey, physicians completed the questionnaires either by themselves or with the help of a previously trained person (physician, nurse or intern).
Ethical Considerations
This study was approved by the local ethics committee “Comité de ética e Investigación en Seres Humanos” (CEISH). We obtained informed consent before participation in the survey. With the information recollected in the survey, personal identification was not possible; as such anonymity/personal data protection was conserved.
Statistical Analysis
For demographical data, descriptive statistics were performed, where categorical variables were reported as frequencies and percentages, while continuous variables were reported as means and standard deviations.
For each ICT, frequency of use was dichotomized as “Low” (at least once a month and at least once a week) and “High” (two or three times a week or daily). Questions regarding perceptions and barriers upon the use of ICTs were dichotomized into “disagree” (strongly disagree and disagree) or “agree” (neutral, agree and strongly agree). A chi-square test was performed to assess the association between the independent variables of age, gender, postgraduate years and medical degree, and the dependent variables frequency of use of ICTs resources, perceptions and barriers.
All data were analyzed using SPSS version 24.0 software (SPSS Inc., Chicago, IL, USA). A value of less than 0.05 was considered statistically significant for all tests.
Results
A total of 640 physicians were surveyed in our study, with a gender distribution of 53.0% males and 45.6% females (). The mean age was 36.9 years, with a mean of 14.9 years in practice in the medical field. Most participants were non-specialist (59.8%) and worked in public service (46.7%). Regarding access to smartphones, 95.2% of physicians reported they owned one.
Table 1 Demographic Characteristics of the Surveyed Population (n=640)
Frequencies of use of ICTs for professional purposes and patient communication
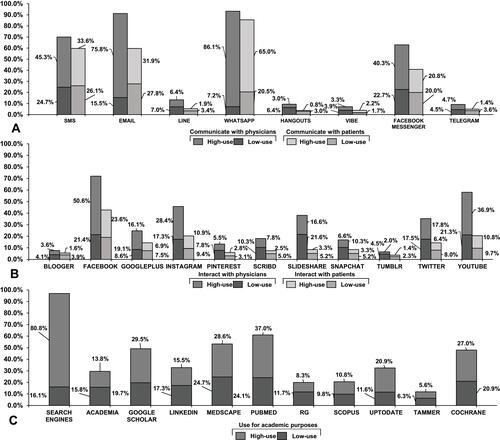
From the 640 participants, 99.7% (n=638) use ICTs to message other physicians, while 93.1% (n=596) use them to message patients (p=0.000). WhatsApp, followed by e-mail and SMS, represents the highest frequency of use for messaging with both physicians and patients (). Moreover, 89.5% (n=573) individuals use social media to interact with other physicians, while 58.1% (n=372) use such channels to interact with patients (p=0.000), being Facebook and YouTube reported in both scenarios with the highest rates (). Finally, 99.7% (n=638) physicians used ICTs to search academic information (p=0.000), where search engines PubMed and Medscape were reported the most (). Frequency of use of ICT according to demographic variables is further depicted on Tables S2 and S3.
Figure 1 Usage rate of information and communication technologies (ICTs) for communication, interaction, and academic purposes. (A) Frequency of individuals using each ICT to communicate with other physicians and patients. (B) Frequency of individuals interacting with other physicians and patients through each ICT. (C) Frequency of individuals using each ICT for academic purposes.
Abbreviations: SMS, short message service; RG, ResearchGate.
Perceptions and Barriers of ICTs Among Physicians
More than 80.0% of the physicians agreed that ICTs resources can be useful for promoting health and medical service, to search for new job opportunities, to get involved in research projects and to promote teamwork with colleagues (p=0.000) (). More than half disagreed about being reluctant to interact with colleagues through such resources, as well as preferring traditional channels of communication rather than using ICTs (p<0.005) ().
Figure 2 Overall frequencies of perceptions and barriers of ICTs among Ecuadorian physicians. (A) Frequencies of each perception are shown as percentages (I, “Promote private medical services”; II, “Search for new job opportunities and/or professional development”; III, “Participate in research projects”; IV, “Promote health”; V, “Work in group with colleagues”; VI, “Dislike to interact with colleagues through such channels”; VII, “Prefer traditional channels of communications”). (B) Frequencies of each barrier are shown as percentages (A, “Concerned about privacy or security about personal and/or patient information”; B, “Do not have access to mobile internet”; C, “Do not have access to internet at work”; D, “Do not have enough time to neither learn how to use them or use them”).
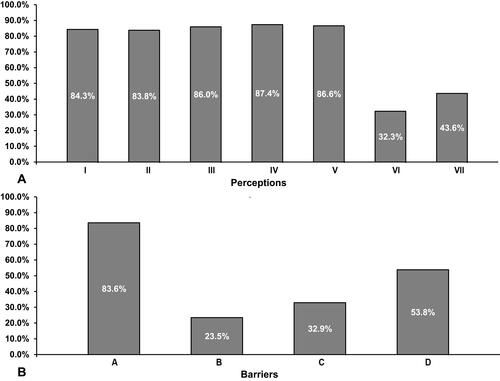
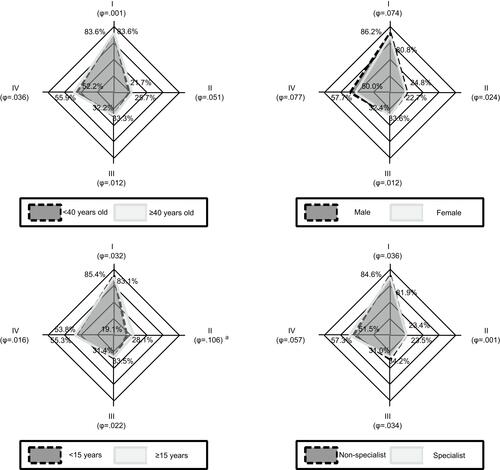
However, 83.6% of the physicians have concerns about privacy and patient confidentiality, while 53.8% lack the time to use ICTs resources (). Less than one-third agreed that limited internet access, either mobile or at work, could represent a barrier to use ICTs (). and depict perceptions and barriers by the selected demographic variables. Frequencies of agreement to specific perceptions and barriers according to demographic variables are also further described in Tables S4–S7.
Figure 3 Perceptions of ICTs by physicians according to selected demographic variables. Seven perceptions are represented on each heptagon. All proportions depicted are individuals that agree with the statement. Physicians on light gray and dark gray represent a dichotomy highlighted below each heptagon and are compared to assess the strength of correlation. I, “Promote private medical services” II, “Search for new job opportunities and/or professional development” III, “Participate in research projects” IV, “Promote health” V, “Work in group with colleagues” VI, “Dislike to interact with colleagues through such channels” VII, “Prefer traditional channels of communications” astatistically significant (p<0.05). Φ, Phi coefficient.
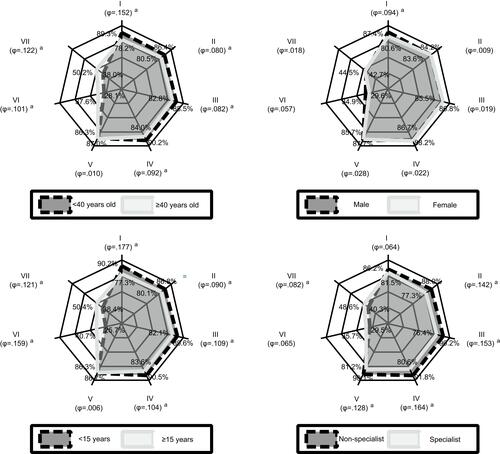
Figure 4 Barriers of ICTs by physicians according to selected demographic variables. Four barriers are represented on each diamond. All proportions depicted are individuals that agree with the statement. Physicians on light gray and dark gray represent a dichotomy highlighted below each diamond and are compared to assess the strength of correlation. I, “Concerned about privacy or security about personal and/or patient information” II, “Do not have access to mobile internet” III, “Do not have access to internet at work” IV, “Do not have enough time to neither learn how to use them or use them” aStatistically significant (p<0.05). Φ, Phi coefficient.
Discussion
The delivery of healthcare services through mobile platforms is a promising technological leap.Citation16 Instantaneous access and direct communication are some of the key benefits that allow for a faster transfer of health information, shaping new medical and public health practices in the process.Citation17 The use of technology, particularly through mobile platforms, can help to improve the quality of care and can be adapted quickly on a large scale at low cost, but there are still knowledge gaps about its effectiveness in different areas.Citation17
Timely communication within the healthcare team and patients remains a fundamental strategy to reduce medical errors.Citation18 Smartphones can serve this purpose, enabling a more efficient communication, and facilitating patient diagnosis and monitoring, with several studies highlighting the trend for the increasing use of smartphones among healthcare professionals.Citation19–Citation21 Interestingly, among developing countries availability of smartphones is considerably high, with studies estimating that 90% of physicians currently own one.Citation22,Citation23 Similarly, we found a high availability of this technology in Ecuadorian physicians (97.3%). The widespread use of smartphones among physicians in Ecuador is a key finding that could facilitate future ICTs enabled studies.
Overall, we found a high usage of ICTs among physicians. For instance, more than 90% of surveyed individuals communicated with other professionals and patients through ICTs designed primarily for communication purposes. Interestingly, while a similar percentage of physicians used social media platforms for interacting with other professionals, there is less usage of these applications for interacting with patients (89.5% vs 58.1%, respectively). In this regard, while social media can serve as a platform by which health professionals can help patients, enhance professional networks, and contribute to public health research and service, its acceptability among physicians might be influenced by the uncertainty of using a platform with unclear boundaries.Citation24,Citation25
Discussing specific ICTs, we found that WhatsApp and Facebook were the most used platforms for communication purposes, and social media interactions, respectively. WhatsApp is a cross-platform application that allows smartphone users to exchange not only text, but images, videos, and audio messages for free, and currently, the reported usage of this application in Latin America is considerably high.Citation26 On the other hand, Facebook is the largest social media platform in the world, allowing for complex social interactions with relatives and other people with similar interests.Citation27 Our results agree with recent estimates, suggesting that both WhatsApp and Facebook are amongst the most popular ICTs used by healthcare professionals for communicating and interacting with peers and patients.Citation23,Citation28,Citation29 The widespread adoption of these ICTs makes them an attractive cost-effective platform for fast communication, and efficient delivery of healthcare information.
The digital transformation of medicine has also enabled new ways of gaining medical knowledge, particularly through the use of search engines and medical databases, tools that are not only in many cases free and easy to access but also updated on a regular basis.Citation30 ICTs devices (eg, smartphones, tablets, and mobile computers) allow a faster and more convenient access to scientific information, and can significantly contribute to research purposes.Citation31 In our study, search engines (eg, google, yahoo, etc.) were selected as the main sources for searching scientific information (96.9%). This finding contrasts with a 2006 study by De Leo and colleagues where the vast majority of physicians avoided search engines as the main source for gathering information, citing inaccuracy as the main reason for avoiding using them.Citation32
However, search engines have significantly evolved, and most of the content of medical sites such as PubMed and Medscape (rated as the second and third main sources for obtaining scientific information in our study) can be accessed directly through them, explaining the higher usage of search engines in our study.Citation33 Moreover, we found that a clear majority of physicians had a positive perception of ICTs applications for helping in research projects (87.4%). These findings would suggest that physicians are already using these technologies in their professional field.
In the setting of health promotion, ICTs platforms can contribute in supporting healthy behaviors at a population level.Citation34 For instance, some studies have found that real-time feedback of users’ health status and motivational messages via social media platforms and mobile devices can have a positive impact on controlling behaviors such as alcohol consumption, exercise, diet, and sexual behavior.Citation35,Citation36 In our study, most physicians agree that ICTs can be useful in the promotion of health and medical services (87.4% and 84.3%, respectively). As eHealth applications continue to grow, they will allow for more personalized patient care, guiding patients when choosing a health professional, while providing relevant health information in the process.Citation37 However, this doctor–patient relationship through eHealth applications can subject physicians to a negative exposure by allowing their performances to be evaluated by means of “comments”.Citation30,Citation37 Healthcare professionals must learn and adapt to the use of these new technologies properly to obtain better results.
Performing remote diagnostics, finding solutions to clinical problems, helping surgeons in complicated operations, and even monitoring patients with chronic diseases are included among the various advantages of using ICTs.Citation38 Furthermore, these applications have allowed the creation of virtual communities among physicians as a way to be in constant communication and to promptly receive updates regarding new medical information.Citation38 We found that 86.6% of our physicians agreed that the use of these technologies can improve the workflow among colleagues. Despite the potential benefits and applications of ICTs, several challenges have arisen along the way, particularly in low and middle-income regions such as Latin America. As evidenced by the World Health Organization (WHO) eHealth global survey, the most common challenges for ICTs implementation among healthcare systems are conflicting priorities, lack of knowledge, absence of legal guidelines on privacy and confidentiality, and cost-effectiveness.Citation39
In our study, we found that privacy and patient confidentiality was the main barrier perceived by 83.6% of physicians. Similarly, Shuaib Qureshi and colleagues stated that privacy for both patients and physicians is considered a major concern with respect to human and social hurdles in healthcare communication technologies.Citation40 These concerns exist because as today, mobile technologies not only manage personal data but also highly personal information such as social interactions, location, emotions, health conditions and others.Citation41 As a matter of fact, in one publication it was reported that only half of patients consider appropriate for doctors to communicate with their online community about their own clinical cases to obtain better care.Citation37 Evidently, vulnerability of the patient’s privacy and confidentiality are obstacles that need to be addressed by both ICTs companies and the healthcare providers, so that sensitive information is only shared among authorized individuals.Citation31,Citation40 The research community is currently investigating different options available to preserve and provide users with better privacy and confidentiality.Citation41
Currently, physicians are managing a growing number of tasks and responsibilities in very limited time frames, ranging from the assessment of complex health issues in patients, to a larger volume of administrative paperwork, thus contributing to higher rates of professional burnout and major challenges regarding time management.Citation42 The increased issue regarding time management, as reported in our study by more than half of physicians, may impair the usage of electronic means for professional purposes and, consequently, their work performance. Furthermore, time is an important consideration regarding proper training in ICTs, as Farahat and colleagues found out; adequate training of physicians in new technologies can lead to a significant optimization in the use of digital resources and work performance in comparison with untrained individuals.Citation43
Additionally, limited access to internet in mobile devices and work facilities is also considered a major barrier. For instance, a study by Farahat et al found that 74.5% of physicians did not have access to internet at workplaces; likewise, G. Ajuwon stated that only few physicians (36%) had private internet connection, and the majority of them lacked internet access at work.Citation43,Citation44 Interestingly, in our study, more than two-thirds of physicians did not perceive lack of internet access in mobile devices or work facilities as a significant technological barrier (76.5% and 67.1%, respectively). This noteworthy finding may be justified by the rapid expansion of mobile phone subscriptions and usage shown in developing countries, which may go hand in hand with the increased internet access that the population is obtaining, providing a potential platform for future mHealth interventions.Citation17
Currently, the healthcare workforce is exhibiting a wide diversity since different generational groups are working alongside each other.Citation45 For instance, there are reports that demographic characteristics appear to influence the use of internet-based communication technologies, and attitudes of professionals toward telemedicine.Citation46,Citation47 As found in a recent study, younger physicians (<40 years) scored higher the utility of telemedicine and consider it might be able to improve patients’ health and therapeutic compliance.Citation47 Similarly, we found that younger physicians (<40 years) with less postgraduate years (<15 years) and non-specialists were more likely to have a positive perception for ICTs than their counterparts.
The differences in perceptions we found among demographic factors, particularly age, might be the result of what is known as the “digital divide”. Under this concept, individuals who were born and grew up speaking the language of computers and the internet might adapt faster to new technologies, and as such, use them more consistently than those not born in the digital world.Citation48 In practice, age has been found to be inversely associated with smartphone ownership, social media use, podcast downloading, and even blogging.Citation49,Citation50 Regarding postgraduate years and non-specialists, our results contrast with a previous study, in which these factors did not consistently influence ICTs usage.Citation46 As a final point, considering the differences regarding demographic factors, and how they influence the perceptions of ICTs usefulness, is key to facilitate an effective implementation of technology to routine medical practice.
Limitations
There are some important limitations to our research. First, this study was conducted on Ecuadorian physicians only; thus, the data provided might differ with other Latin American countries. In addition, even though the survey was validated and built under expert recommendations, more facts concerning attitudes, perceptions and barriers could have been included to provide a deeper picture of ICTs in Ecuador. Also, even though data collection was performed under the supervision of trained personnel, most analyses have heterogeneous sample size due to missing data in some surveys. Furthermore, even though the purpose of the study is to provide a general glimpse of how physicians perceive ICT in medical practice, this study did not establish causality on the selected independent variables towards the subject of study, whilst other possible factors not included in the analyses may have had a confounding effect not assessed in the adjustment. However, some strengths of the study are the significant sample size and relatively balanced demographic categories.
Conclusion
The use of information and communication technologies has the potential to change the way healthcare is delivered around the world. Low-cost, instantaneous access, and direct communication allow for a faster transfer of health information. In our study, we found a high usage of ICTs among physicians for communicating and interacting with patients and colleagues and obtaining scientific information. Most individuals had a positive perception toward ICTs, particularly among younger physicians, with less postgraduate years, and non-specialists. Finally, the major barriers reported were privacy and patient confidentiality, and time management. Further studies are needed to confirm our findings, and to develop strategies based on known patterns of usage, perceptions, and barriers of technology; thus allowing for a successful implementation of ICTs to the mainstream clinical practice.
Abbreviations
ICTs, Information and Communication Technologies; e-health, Electronic Health; mHealth, Mobile Health; WHO, World Health Organization; SMS, Short Message Service.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics and Consent Statement
This study was approved by the ethics committee Comité de ética e Investigación en Seres Humanos (CEISH), Guayaquil-Ecuador, in accordance to the principles established by the declaration of Helsinki.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Acknowledgments
The authors acknowledge the guidance and knowledge imparted by the MECOR Program for this study, especially from Sonia Buist MD, Ana Menezes MD, and Juliana Ferreira M.D. We express our gratitude to all members of Respiralab Research Group. We also want to acknowledge Universidad Espiritu Santo for their continuous support.
Disclosure
Dr Ivan Cherrez-Ojeda reports grants from Universidad Espiritu Santo, during the conduct of the study. The authors declare no other conflicts of interest related to this work.
Additional information
Funding
References
- Catan G, Espanha R, Veloso Mendes R, Toren O, Chinitz D. The impact of eHealth and mHealth on doctor behavior and patient involvement: an Israeli and Portuguese comparative approach. Stud Health Technol Inform. 2015;210:813–817.
- NIHP. The health system in the digital age. 11° Dead Sea Conference, 27–26 May 2010. Israel: The Israel National Institute for Health Policy Research; 2010.
- Houshyari AB, Bahadorani M, Tootoonchi M, Gardiner JJ, Peña RA, Adibi P. Medical education and information and communication technology. J Educ Health Promot. 2012;1:3. doi:10.4103/2277-9531.94411
- Maharana B, Biswal S, Sahu NK. Use of information and communication technology by medical students: a survey of VSS Medical College, Burla, India. Lib Philos Pract. 2009;281.
- D’Onofrio G, Sancarlo D, Ricciardi F, et al. Information and communication technologies for the activities of daily living in older patients with dementia: a systematic review. J Alzheimers Dis. 2017;57(3):927–935. doi:10.3233/JAD-161145
- Poissant L, Pereira J, Tamblyn R, Kawasumi Y. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review. J Am Med Inform Assoc. 2005;12(5):505–516. doi:10.1197/jamia.M1700
- Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood). 2005;24(5):1103–1117. doi:10.1377/hlthaff.24.5.1103
- Gund A, Lindecrantz K, Schaufelberger M, Patel H, Sjoqvist BA. Attitudes among healthcare professionals towards ICT and home follow-up in chronic heart failure care. BMC Med Inform Decis Mak. 2012;12(1):138. doi:10.1186/1472-6947-12-138
- De Angelis G, Davies B, King J. Information and communication technologies for the dissemination of clinical practice guidelines to health professionals: a systematic review. JMIR Med Educ. 2016;2(2):e16. doi:10.2196/mededu.6288
- Roper L, Jorm C. Please leave your phone outside: policymakers and medical app providers are encouraging patient participation, but doctors in the consult room are not. BMJ Innovations. 2017;3(2):65–70. doi:10.1136/bmjinnov-2016-000134
- Lupianez-Villanueva F, Hardey M, Torrent J, Ficapal P. The integration of information and communication technology into medical practice. Int J Med Inform. 2010;79(7):478–491. doi:10.1016/j.ijmedinf.2010.04.004
- Haluza D, Jungwirth D. ICT and the future of health care: aspects of doctor-patient communication. Int J Technol Assess Health Care. 2014;30(3):298–305. doi:10.1017/S0266462314000294
- Patil RN, Almale BD, Patil M, et al. Attitudes and perceptions of medical undergraduates towards mobile learning (M-learning). J Clin Diagn Res. 2016;10(10):Jc06–jc10. doi:10.7860/JCDR/2016/20214.8682
- Wallace S, Clark M, White J. ‘It’s on my iPhone’: attitudes to the use of mobile computing devices in medical education, a mixed-methods study. BMJ Open. 2012;2(4):4. doi:10.1136/bmjopen-2012-001099
- Gary Woodill CU. Mobile learning in medicine and healthcare: professional education applications. Float Mobile Learn. 2011.
- Sezgin E, Özkan-Yildirim S, Yildirim S. Understanding the perception towards using mHealth applications in practice: physicians’ perspective. Inf Dev. 2018;34(2):182–200. doi:10.1177/0266666916684180
- Marcolino MS, Oliveira JAQ, D’Agostino M, Ribeiro AL, Alkmim MBM, Novillo-Ortiz D. The impact of mHealth interventions: systematic review of systematic reviews. JMIR Mhealth Uhealth. 2018;6(1):e23. doi:10.2196/mhealth.8873
- Wong BM, Quan S, Cheung CM, et al. Frequency and clinical importance of pages sent to the wrong physician. Arch Intern Med. 2009;169(11):1072–1073. doi:10.1001/archinternmed.2009.117
- Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res. 2012;14(5):e128. doi:10.2196/jmir.1994
- Kiser K. 25 ways to use your smartphone. Physicians share their favorite uses and apps. Minn Med. 2011;94(4):22–29.
- Franko OI, Tirrell TF. Smartphone app use among medical providers in ACGME training programs. J Med Syst. 2012;36(5):3135–3139. doi:10.1007/s10916-011-9798-7
- Gavali MY, Khismatrao DS, Gavali YV, Patil KB. Smartphone, the new learning aid amongst medical students. J Clin Diagn Res. 2017;11(5):Jc05–jc08. doi:10.7860/JCDR/2017/20948.9826
- Vásquez-Silva L, Ticse R, Alfaro-Carballido L, Guerra-Castañon F. Acceso, uso y preferencias de las tecnologías de información y comunicación por médicos de un hospital general del Perú [Access, use and preferences of information and communication technologies by physicians in a general hospital in Peru. Rev Peruana de Medicina Experimental y Salud Pública. 2015;32(2):289–293. Spanish. doi:10.17843/rpmesp.2015.322.1622
- George DR, Rovniak LS, Kraschnewski JL. Dangers and opportunities for social media in medicine. Clin Obstet Gynecol. 2013;56(3):3. doi:10.1097/GRF.0b013e318297dc38
- Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, Hoving C. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res. 2013;15(4):4. doi:10.2196/jmir.1933
- Cherrez Ojeda I, Calderon JC, Jove OL, et al. What kind of information and communication technologies do patients with COPD prefer to use? A cross-sectional study in Latin America. Chron Respir Dis. 2018;15(3):286–295. doi:10.1177/1479972317741895
- Eghdam A, Hamidi U, Bartfai A, Koch S. Facebook as communication support for persons with potential mild acquired cognitive impairment: a content and social network analysis study. PLoS One. 2018;13(1):e0191878. doi:10.1371/journal.pone.0191878
- Bosslet GT, Torke AM, Hickman SE, Terry CL, Helft PR. The patient-doctor relationship and online social networks: results of a national survey. J Gen Intern Med. 2011;26(10):1168–1174. doi:10.1007/s11606-011-1761-2
- Sezgin E, Özkan-Yildirim S, Yildirim S. Investigation of physicians’ awareness and use of mHealth apps: a mixed method study. Health Policy Techn. 2017;6(3):251–267. doi:10.1016/j.hlpt.2017.07.007
- Altés J. Papel de las tecnologías de la información y la comunicación en la medicina actual [Role of information and communication technologies in today's medicine]. Seminarios de la Fundación Española de Reumatología. 2013;14(2):31–35. Spanish. doi:10.1016/j.semreu.2013.01.005
- Qidwai W. Advances in information and communication technology (ICT): issues, challenges and opportunities for health care professionals. J Coll Physicians Surg Pak. 2011;21(11):651–653. doi: 11.2011/jcpsp.651653
- De Leo G, LeRouge C, Ceriani C, Niederman F. Websites most frequently used by physician for gathering medical information. AMIA Annu Symp Proc. 2006;2006:902.
- Wang L, Wang J, Wang M, Li Y, Liang Y, Xu D. Using internet search engines to obtain medical information: a comparative study. J Med Internet Res. 2012;14(3):e74. doi:10.2196/jmir.1943
- Lupton D. M-health and health promotion: the digital cyborg and surveillance society. Social Theory Health. 2012;10(3):229–244. doi:10.1057/sth.2012.6
- Laakso E-L, Armstrong K, Usher W. Cyber-management of people with chronic disease: a potential solution to eHealth challenges. Health Educ J. 2012;71(4):483–490. doi:10.1177/0017896911408813
- Mays D, Cremeens J, Usdan S, Martin RJ, Arriola KJ, Bernhardt JM. The feasibility of assessing alcohol use among college students using wireless mobile devices: implications for health education and behavioural research. Health Educ J. 2010;69(3):311–320. doi:10.1177/0017896910364831
- Leis Dosil VM. Papel de las nuevas tecnologías en la relación médico-paciente. Piel. 2017;32(4):187–189. doi:10.1016/j.piel.2016.10.016
- Karsenti T, Charlin B. Information and Communication Technologies (ICT) in medical education and practice: the major challenges. Revue Internationale Des Technologies En Pédagogie Universitaire. 2008;5(2):68–81. doi:10.7202/037475ar
- Lewis T, Synowiec C, Lagomarsino G, Schweitzer J. E-health in low- and middle-income countries: findings from the center for health market innovations. Bull World Health Organ. 2012;90(5):332–340. doi:10.2471/BLT.00.000000
- Qureshi MS, Qureshi MB, Thayananthan V. Healthcare communication technologies: a short note on opportunities and challenges. Int Res J Eng Technol. 2016;04(06).
- Kumar S, Nilsen WJ, Abernethy A, et al. Mobile health technology evaluation: the mHealth evidence workshop. Am J Prev Med. 2013;45(2):228–236. doi:10.1016/j.amepre.2013.03.017
- Gordon CE, Borkan SC. Recapturing time: a practical approach to time management for physicians. Postgrad Med J. 2014;90(1063):267–272. doi:10.1136/postgradmedj-2013-132012
- Farahat TM, Hegazy NN, Mowafy M. Information and communication technologies in primary healthcare facilities in Egypt. Prim Health Care Res Dev. 2018;19(1):88–95. doi:10.1017/S1463423617000470
- Ajuwon GA. Use of the Internet for health information by physicians for patient care in a teaching hospital in Ibadan, Nigeria. Biomed Digit Libr. 2006;3(1):12. doi:10.1186/1742-5581-3-12
- Warshawski S, Barnoy S, Kagan I. Professional, generational, and gender differences in perception of organisational values among Israeli physicians and nurses: implications for retention. J Interprof Care. 2017;31(6):696–704. doi:10.1080/13561820.2017.1355780
- Cooper CP, Gelb CA, Rim SH, Hawkins NA, Rodriguez JL, Polonec L. Physicians who use social media and other internet-based communication technologies. J Am Med Inform Assoc. 2012;19(6):960–964. doi:10.1136/amiajnl-2011-000628
- Ruiz Morilla MD, Sans M, Casasa A, Giménez N. Implementing technology in healthcare: insights from physicians. BMC Med Inform Decis Mak. 2017;17(1):92. doi:10.1186/s12911-017-0489-2
- Repique RJ. Digital natives, digital immigrants: dichotomy or diversity in psychiatric nursing? J Am Psychiatr Nurses Assoc. 2013;19(2):100–101. doi:10.1177/1078390313481999
- Smith A. Smartphone Adoption and Usage; 2011. Available from: http://www.pewinternet.org/2011/07/11/smartphone-adoption-and-usage/. Accessed September 08, 2018.
- Zickuhr K. Generations 2010; 2010. Available from: http://www.pewinternet.org/2010/12/16/generations-2010/. Accessed September 08, 2018.
