Abstract
Purpose
The complexity of modern medicine requires high-performance teamwork to ensure quality care. Teams rely on communication patterns that are replicable and efficient. The purpose of this observational study was to characterize communication dynamics among interprofessional team members during a team huddle. The study aimed to (a) characterize communication within structured huddles on an inpatient medicine unit by evaluating who talked and to whom and what types of communication took place during each interaction and (b) explore participants’ perceptions of the huddles.
Materials and Methods
We used a sociogram to diagram direct observations of the structure and patterns of group interaction. Through the sociogram, we documented the flow and frequency of team members information exchange, questions, and requests. We conducted two follow-up focus groups—one with residents and one with nurses.
Results
The most frequent type of interaction observed was information exchange: nurse to resident (28.3%) and resident to nurse (47%). Both residents and nurses asked questions: nurse to resident (7.4%) and resident to nurse (14.2%). Nurses made more requests of residents (2.8%) than vice versa (0.3%). Four themes emerged from focus group analysis, including the huddle promotes (1) a better-informed team, (2) relationship building, (3) communication process efficiencies, and (4) logistical challenges.
Conclusion
Sociograms can serve as a novel tool to characterize what actually happens during information exchange at the point of care and identify the nature of communication among team members. Daily huddles among team members involved in the frontline of patient care provides an opportunity to share information, requests, and questions and update shared mental models to meet team objectives.
Introduction
The association between poor team communication and medical errors points to the need to link structured communication practices to interprofessional work processes. Poor communication is a common cause of medical errors.Citation1 Up to 91% of self-reported errors by resident physicians result from poor communication, and communication failures between residents and nurses result in delayed treatment, medication errors, and inaccurate reporting of patient health status.Citation2 Studies of communication between physicians and nurses demonstrate limited discussion (50% to 62% of the time) of a patient between physician and nurseCitation3 and little agreement on the patient priorities (17%) or planned procedures (11%) with somewhat improved agreement on planned medication changes (42%).Citation4
One strategy to improve communication among health-care team members is to schedule structured interprofessional communication as part of the day-to-day work routine. Effective team communication involves the distribution of information to other team members to promote the continuous updating of the team’s mental model.Citation5 Effective team communication also includes the processes through which team members interact to achieve an outcome.Citation5 Scheduling structured interprofessional communication provides an opportunity for updating the team’s mental model and provides a process through which team members routinely interact.
An example of scheduled, structured interprofessional communication includes “pre-briefs” or “team huddles” that incorporate communication as part of the team process. One study showed that interprofessional huddles increase communication, allow for formalized patient-care planning, and improve relationships among providers.Citation6 Team huddles are goal-oriented, intentionally brief, and built into the normal workday routine. Huddles increase the quantity and quality of information exchange and increase accountability. More specifically, huddles allow for clarifying questions and development of shared understanding.Citation6,Citation7 Huddle participants have reported additional benefits, including that (a) participants felt encouraged to report concerns about patients rather than remain silent, (b) nursing staff felt empowered to speak up and publicly express disagreement, flattening the power structure, and (c) all providers reported an increased sense of community and understanding of what challenges their team members faced.Citation7
Although the benefits of interprofessional team huddles are well documented, the literature is limited regarding the dynamics among team members during a huddle in the general medical inpatient setting. The aim of this study was to (a) characterize communication within structured huddles on an inpatient medicine unit by evaluating who talked and to whom and what types of communication took place during each interaction throughout the huddle and (b) explore participants’ perceptions of the huddles.
Materials and Methods
Setting and Background
An interprofessional team “huddle” was implemented at a 361-bed acute care teaching hospital and the region’s only Level 1 trauma center. Huddles took place on a 28-bed inpatient medicine unit and had explicit goals to: (a) verify team/patient assignments, (b) share overnight information, and (c) establish daily goals of care. The ward medical staff consisted of three physician teaching teams that included an attending physician, two residents (one off duty and one on duty), and two interns per team. At the time of this study, nurses were assigned to patients based on patient acuity and location of patient rooms.
The structure of the huddle was established based on guidelines from the Crew Resource Management (CRM) training program,Citation8 and health-care professionals at the hospital were required to participate in CRM training. Adopted by the health-care industry, CRM training is focused on the cognitive and interpersonal skills needed to effectively manage team-based, high-risk activity. CRM trains for predictable and repeatable team briefings.Citation9
Our huddle was both predictable and repeatable; it occurred daily at the nurse’s station during nurse shift-change and was time-limited (~20 minutes). The huddles were added in addition to the attending physician-led patient rounds and provided a unique opportunity for nurses to share with resident physicians what happened during the night and for the resident physicians to share with nurses the tentative plans for the day. A resident, multiple nurses, one unit clerk, and a pharmacist participated in the huddle. All members of the three patient-care teams gathered at 8:00 a.m., and team huddles were conducted consecutively. It was common for a nurse to be part of more than one patient-care team based on nursing assignments. The pharmacist and unit clerk were unit-based and thus served in these roles for all three patient-care teams. Residents were assigned by patient-care team—the teams took turns to initiate their huddle to ensure complete attendance. The resident initiated interactions by calling out a patient room number; the nurse assigned to the patient responded, and the communication exchange began through a series of questions, requests, and information—each communication exchange took approximately 1 minute per patient.
To ensure that each patient was represented during the huddle, the team used the unit white board. The white board listed each patient's room number, the patient’s initials, the physician team assignment, and the nurse’s last name and pager number. The unit clerk placed a checkmark next to each patient as the team exchanged information. If the team assignment changed, the unit clerk updated the white board accordingly.
This project was initiated for quality improvement. Ethical approval to observe and interview huddle participants was obtained through the University of Missouri Institutional Review Board (IRB). Informed consent was obtained following IRB guidelines and indicated that all analysis would be de-identified and publication of responses to questions would be anonymized. We conducted direct observation of the huddle and completed two focus groups after observations—one with residents and one with nurses. Participants were selected for observation based on their assignment to the inpatient service.
Direct Observations with a Sociogram
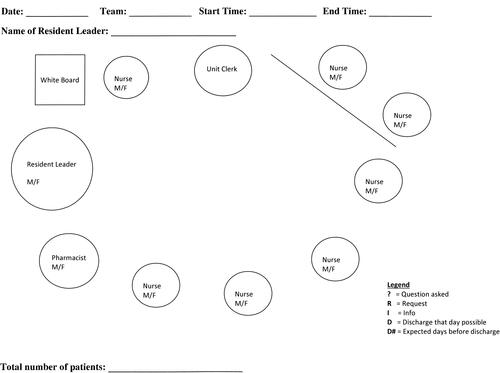
We utilized a sociogram to diagram observations of the structure and patterns of group interaction.Citation10 Through the sociogram () we documented the flow and frequency of team-members information exchange, questions, and requests. We customized the sociogram to depict the inpatient nursing station where the huddle took place. We used circles on the sociogram to represent participant positions within the huddle. The diagonal line represented the window at the nursing station. Observations occurred each weekday at 8:00 a.m. on the same inpatient ward. We observed three team huddles each day for 16 days yielding 48 completed sociograms. All sociograms were completed by the same researcher (LR) who also completed reflective field notes at the end of each encounter with the purpose of identifying patterns and points of clarification at the end of each observation.Citation11 Reflective field notes informed the development of strategies to capture data in the sociogram. A second observer (KH) observed three sociograms.
Figure 1 The sociogram used to document the flow and frequency of team-members information exchange, questions, and requests. The sociogram depicts the inpatient nursing station where the huddle took place. Circles represent participant positions within the huddle. The diagonal line represents the window at the nursing station.
The structure of the huddle required the resident to begin each patient report (termed “patient volley”) by stating a patient room number, and the nurse assigned to that patient responded. Next, the resident initiated a question, a request, or information to the nurse. Using a multi-colored pen, we captured this first interaction by drawing a line from the “resident” circle to the “nurse” circle. We captured the direction of communication with an arrow and annotated the type of communication as a question (?), a request (R), or information (I). If the nurse responded to the resident, a new line was drawn using the same pen color from the nurse circle back to the resident circle. We used the same process to capture direction of communication and type of communication. We documented each interaction between participants and truncated the lines by using a slash instead of the full line arrow. If a resident or nurse provided multiple forms of communication during the same interaction, symbols were written together without a slash. To start the next patient volley, the resident called out a new patient room number. The following are examples of two directly observed patient volleys:
Patient Volley 1
Patient Room 12
That’s me.
This patient will likely be discharged today, but I need to speak with the social worker first. (red line drawn from resident circle to nurse circle with arrowhead pointed to nurse circle; line labeled “I” for information)
Please talk to the caregiver—she’s worried about his anxiety. (red line drawn from nurse circle to resident circle with arrowhead pointed to resident circle; line labeled “R” for request)
Patient Volley 2
Patient Room 15
That’s me. (a different nurse than volley 1)
This patient will not be discharged any time soon. (green line drawn from resident circle to nurse circle with arrowhead pointed to nurse circle; line labeled “I” for information)
Please prescribe more pain medication. (green line drawn from nurse circle to resident circle with arrowhead pointed to resident circle; line labeled “R” for request)
How’s her mental state? (a slash is written after the “I” on the line drawn from resident circle to nurse circle, and a “Q” for question is written after the slash)
She is really out of it and delirious. (a slash is drawn after the “R” on the line drawn from nurse circle to resident circle, and an “I” for information is written after the slash)
Data from completed sociograms were input into a Microsoft Excel 2010 file we termed a “sociomatrix” and verified.
Participant Focus Groups
We conducted two focus groups with huddle participants—one with residents and one with nurses. The rationale for conducting focus groups separately was to provide a comfortable environment for participants to share their unique experiences and answer questions pertaining to the roles and expectations of other health professionals participating in the huddle. The facilitator used follow-up questioning and a focus group guide (see Appendix) to guide and spark conversation.
A total of ten residents were observed, and all were invited to the focus group. A total of four nursing staff who participated in the observed huddles and were still working at the hospital were invited to the focus group. Multiple invitation reminders were sent to encourage individuals to participate. Four residents and two nurses participated in focus groups. Both focus groups were facilitated by the same researcher (KH), and both discussions were typed in real-time by the same scribe (LR). Typed transcripts were reviewed by the facilitator to endorse accuracy.
Content analysis of focus group transcripts was completed using the constant comparative approach.Citation12,Citation13 Responses to each focus group question were used to develop a coding scheme that was progressively refined. A research assistant reviewed all completed coding and concurred with the findings.
Actions taken to enhance trustworthiness include: (a) a second observer (KH) observed three sociograms, (b) reflective field notes helped identify patterns, methodological problems, and points of clarification at the end of each observation, (c) a research assistant reviewed all completed focus group coding and concurred with the findings, and (d) we aligned data from direct observations with themes from the focus groups to verify concurring results.
Results
Direct Observations
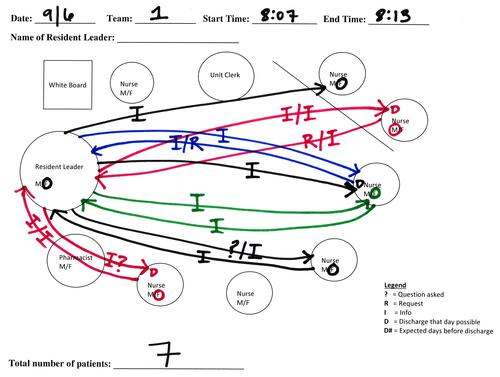
illustrates one completed sociogram. illustrates a completed sociomatrix from three sociograms. We included up to six interactions per patient volley in the sociomatrix.
Table 1 Sample Sociomatrix with Data from Three Sociograms. We Included Up to Six Interactions per Patient Volley in Each Sociomatrix
Figure 2 Sample of one completed sociogram. Using a multi-colored pen, we captured the first interaction by drawing a line from the “resident” circle to the “nurse” circle. We captured the direction of communication with an arrow and annotated the type of communication as a question (?), a request (R), or information (I). If the nurse responded to the resident, a new line was drawn using the same pen color from the nurse circle back to the resident circle. We used the same process to capture direction of communication and type of communication. We documented each interaction between participants and truncated the lines by using a slash instead of the full line arrow. If a resident or nurse provided multiple forms of communication during the same interaction, symbols were written together without a slash.
There was an average of 2.89 interactions per volley. Analysis of data from all observed interactions showed the most frequent type of interaction was information exchange: nurse to resident (28.3%) and resident to nurse (47%). Residents asked nurses more questions (14.2%) than vice versa (7.4%), and nurses made more requests of residents (2.8%) than residents made of nurses (0.3%).
Analysis of each type of interaction per team huddle indicated an average of 17 information interactions, 5 question interactions, and 1 request interaction between residents and nurses. Nineteen interactions took place between the resident and pharmacist during six of the observed huddles; most were information sharing between resident and pharmacist (13), some were questions between resident and pharmacist (5), and there was one request made from pharmacist to resident. There were zero interactions observed between pharmacist and nurse.
Focus Groups
Content analysis of the resident and nurse focus groups resulted in four overarching themes, including the huddle promotes: (1) a better-informed team, (2) relationship building, (3) communication process efficiencies, and (4) logistical challenges. includes themes aligned with representative quotes.
Table 2 Themes from Analysis of Resident and Nurse Focus Groups Aligned with Representative Quotes
A Better-Informed Team
When asked what motivated the huddle, nurses indicated that they needed to transfer the night report from nursing staff, including information not put in orders and they also needed to know the plan for the day. One stated “The ability for the nurse to know the plan for the day was a big part of where it came about.” Another described:
Things would happen overnight … pain prescriptions, one-time dose of something … some of these things and precautions were not put in actual orders, so the huddle gave us the opportunity to communicate these things to the residents. The huddle allowed for more big-picture planning … residents would use information and provide us with the plan for the day.
Another said:
Residents would take notes during the huddle and this made them more prepared for rounds … they weren’t put on the spot in front of the attending during rounds.
When asked to describe what happened during the huddle, residents reported they often received new patient information from nurses. One resident stated:
We received feedback from the nurses about patient issues. Many times this was information we did not know. We want to get the direct story from nursing staff who are the direct caregivers of the patient.
Another commented that:
There is no other point in the day you would have that interaction with the nursing staff about what happened overnight … nurses had just received direct checkout from night staff, so timing allowed less possibility for the nurses to forget what happened.
Another stated that the “huddle saved a lot of potential accidents because nurses brought things to our attention we didn’t know about.”
Residents also described presenting patient information about discharge and/or future plans of care to the team:
We would inform the nursing staff about discharging the patient either that day or a later day and provide future plans of care for each patient … It was the best opportunity for me to communicate patient plan.
The huddle provided time for “… nurses to air any questions or concerns and check things we may have missed.” Another resident stated, “Nursing staff realized they are a big source of our teaching … they recognize you don’t know everything and serve as a safety net.” One resident described the huddle as providing an opportunity for nurses to add to the patient report: [I could] “prepare ahead of time and then ask if they have anything to add.”
Relationship Building
The huddle promoted relationship building by making the nurses feel like they were part of the communication process:
It provided a way for the nurse to be a part of the communication process, face-to-face with the residents … it was an opportunity to advocate for your patient … [and tell them] this is what I’m concerned about.
The nurses stated that the face-to-face time with the residents made them more approachable: “We got to know the residents and built rapport … and made them easier to approach.”
Residents indicated the huddle promoted relationship building with nurses and increased trust. One resident stated:
Having everyone in a tight space helped identify which nurse had which patient and allowed us to know who the nurse was and which patient they were responsible for on that day.
Another indicated the huddle gave them an opportunity to learn nurse’s names:
It was no longer Nurse X; you knew their name. It became my friend Rebecca instead of Nurse X. You see the nurse’s face and their thought processes instead of a random voice on the phone … this increased my trust of them.
Some residents felt the huddle made the senior residents more approachable: “It makes you very approachable as a senior resident … providing a moment where nurses can talk to senior residents.” One resident felt the huddle built rapport with the nurses and explained they “made the nurses feel comfortable to call us and this resulted in more give and take throughout the day either in the hall or on the phone.”
When asked if the huddle created a flattened hierarchy, residents acknowledged there was a hierarchy because they led the huddle but stated “it didn’t seem like anyone was uncomfortable speaking up … we were the leaders but everyone was open to ideas.” One resident indicated that the huddle allowed nurses to see that they are a big part of resident teaching:
They were very nice about teaching us … they didn’t make it obvious like ‘you didn’t know this’ as long as the resident was receptive and didn’t act pompous … they recognize you don’t know everything and serve as a safety net.
Communication Process Efficiencies
Nurses indicated that the huddle was part of the regular schedule and they organized their work differently because of the huddle. Their morning process was night report from nurse, patient assessment, then the huddle:
To prepare for the huddle, we reorganized our work … we received the nurse night report at shift change and then assessed each of our patients by looking at labs, meds, and the patient … then we had the huddle.
They believed the huddle reduced the number of calls to the resident during the day: “Communication first thing in the morning reduced the number of calls to the resident throughout the day.”
Several residents indicated the huddle clarified which physician to call for each patient-care team and this streamlined communication by reducing the number of erroneous calls:
The unit clerk and nurse may know who the attending physician is but they may not know which resident was responsible for which patient on a certain day. The huddle provided an opportunity to clarify which resident physician to call for which team … identifying the right patient care provider reduced calls throughout the day.
Logistical Challenges
The nurses described logistical challenges with the huddle, stating “there were times the nurse could not be at the huddle because of patient-care issues.” They also acknowledged that the timing could be difficult for residents “because they had rounds right after the huddle … and they had to wait while other residents gave reports.” One nurse indicated the environment was distracting “with the phone going off and phlebotomist tube making noise.”
The residents felt the timing of the huddle was a downside and that it was hard to be there at the right time.
It was difficult to align everything at one single time. All three senior residents showed up for the huddle at 8:00 a.m. … without having scheduled times for each team, we would wait until the other residents gave report … so time was wasted.
Discussion
This work builds on what is known regarding inpatient medicine interprofessional team huddles by quantifying the direction and frequency of interactions and the nature of communication among team members. To advance research on interdisciplinary teams, better measurement is needed with “unobtrusive and real-time measures of team performance that can be practically implemented, especially in the field”.Citation14 Novel use of a sociogram added specificity to the team interactions and allowed us to identify the different types and quantity of information shared within the huddle. The sociogram provided a practical tool that we used in the context of patient care to characterize and document elements of team communication. Our sociogram findings that most of the interactions were the sharing of information and asking of questions are consistent with findings from other studiesCitation6,Citation7 and align with our focus group findings suggesting the sociogram worked.
The safety and quality of patient care are dependent on teamwork, communication, and a collaborative, professional practice environment.Citation15 Practice-based interprofessional communication interventions can improve collaboration between nurses and physicians and have positive impacts on teamwork, health-care processes, and outcomes.Citation16–Citation18 According to Salas et al,Citation5 three coordinating mechanisms are critical to a team’s success, including (1) shared mental models, (2) closed-loop communication, and (3) mutual trust. These mechanisms are required for teams to engage in components of effective teamwork. The use of a huddle creates a structured framework in which closed-loop communication can occur and ensures that all team members are operating on the most up-to-date mental model. Huddles promote proactive care by allowing professionals from multiple disciplines to contribute to the daily plan. Finally, and perhaps most importantly, they promote face-to-face interactions which, based on our focus groups, promote team building and trust among team members.
Though instant messaging, electronic medical records, and digital handoff tools have promoted the use of asynchronous communication in medicine, our focus groups suggest that direct, synchronous communication continues to have an important role in high-quality patient care. An important observation from our residents and nurses was that face-to-face interactions decreased the barriers to communication. Further, this provided an opportunity for larger planning beyond the problem-oriented discussions that tend to occur during nurse-physician phone calls. While phone calls represent “hot action” communication in which a decision and action is needed, the huddle represents “cold action” in which there is more open space for communication.Citation19,Citation20 It is likely that both the combination of face-to-face and cold communication space fostered resident-nurse relationship building. It also allowed the dissemination of information about overnight nursing events that are otherwise not well captured in the electronic medical record.
At our institution, the interprofessional huddle has “evolved” into interprofessional rounding at the patient bedside. There is abundant interest in interprofessional teamsCitation14,Citation17,Citation21–Citation23 including studies of the effects of adding patients and family members into interprofessional rounding.Citation24–Citation26 However, at our own institution, we have noted some logistical concerns. As stated prior, nurses often care for patients that reside on multiple internal medicine teams. If rounds occur simultaneously, as frequently occurs, nurses often have to choose which set of bedside rounds to attend. Further, we found the later in the morning these bedside rounds occur, the more likely nurses will be engaged in other patient care activities. It was notable that, despite the reported logistical concerns, the 8:00 am huddles were well attended and seemed to fit well into ongoing work flows.
Our study is the first we are aware of that characterizes communication patterns in interprofessional huddles using a sociogram. We believe this tool has broader applications and could serve to better understand communication patterns in other types of team settings. Future research could use the sociogram to evaluate interprofessional rounding and identify how the information exchange is changed in the presence of additional team members and the patient and/or family. Specifically, how do communication patterns change in the presence of patients/family and how do they fit into the communication flow?
There are several limitations to our study. First, research was conducted at one institution on one medicine unit. Second, a time-lapse between the huddle observations and focus group sessions likely contributed to the low focus group participant number and recall bias. It took time to complete sociogram analysis and focus groups were conducted after that analysis. In addition, the dissolution of the huddle occurred after direct observations and before the focus groups, limiting the number of directly observed nurse participants who still worked at the hospital. Our low focus group participant numbers did not allow us to reach data saturation. Third, with such limited interactions of the pharmacist within the huddle, we did not pursue conducting focus groups and do not have sufficient information to understand why there was no interaction between pharmacist and nurse. Lastly, our observations took place directly in the huddle and our presence may have influenced participant’s behaviors.
Conclusion
Sociograms can serve as a useful tool for characterizing the nature of communication among team members during structured communication practices and identify who on the team is talking or not talking. Daily huddles among team members involved in the frontline of patient care may foster mutual trust and shared decision-making and provide an opportunity for team members to update their shared mental models by communicating information, requests, and questions to meet team objectives.
Acknowledgments
This paper reports research that was funded by the Donald W. Reynolds Foundation and in keeping with the University of Missouri’s grant-funded program: Learning to Provide Better Care in Teams: The Next Steps in Strengthening Geriatrics Medical Education at University of Missouri School of Medicine. The authors wish to thank Jessica Fleagle and Karen Cox for their help providing access and their contributions to this research.
Disclosure
The authors report no conflicts of interest in this work.
References
- The Joint Commission. Most Commonly Reviewed Sentinel Event Types. The Joint Commission; 2016. Available from: https://www.jointcommission.org/se_data_event_type_by_year_/. Accessed February 4, 2019.
- Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186. doi:10.1097/00001888-200402000-00019
- O’Leary KJ, Thompson JA, Landler MP, et al. Patterns of nurse-physician communication and agreement on the plan of care. Qual Saf Health Care. 2010;19(3):195–199. doi:10.1136/qshc.2008.030221
- Evanoff B, Potter P, Wolf L, Grayson D, Dunagan C, Boxerman S. Can we talk? Priorities for patient care differed among health care providers. In: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in Patient Safety: From Research to Implementation (Volume 1: Research Findings). Advances in Patient Safety. Agency for Healthcare Research and Quality (US); 2005. Available from: http://www.ncbi.nlm.nih.gov/books/NBK20468/. Accessed February 4, 2019.
- Salas E, Sims DE, Burke CS. Is there a “big five” in teamwork? Small Group Res. 2005;36(5):555–599. doi:10.1177/1046496405277134
- Provost SM, Lanham HJ, Leykum LK, McDaniel RR, Pugh J. Health care huddles: managing complexity to achieve high reliability. Health Care Manage Rev. 2015;40(1):2–12. doi:10.1097/HMR.0000000000000009
- Goldenhar LM, Brady PW, Sutcliffe KM, Muething SE. Huddling for high reliability and situation awareness. BMJ Qual Saf. 2013;22(11):899–906. doi:10.1136/bmjqs-2012-001467
- Salas E, Fowlkes JE, Stout RJ, Milanovich DM, Prince C. Does CRM training improve teamwork skills in the cockpit?: two evaluation studies. Hum Factors. 1999;41(2):326–343. doi:10.1518/001872099779591169
- Haller G, Garnerin P, Morales M-A, et al. Effect of crew resource management training in a multidisciplinary obstetrical setting. Int J Qual Health Care. 2008;20(4):254–263. doi:10.1093/intqhc/mzn018
- Hollander CE. An Introduction to Sociogram Construction. Snow Lion Press, Inc.; 1978. Available from: http://asgpp.org/pdf/carl%20hollander%20sociogram.pdf. Accessed February 4, 2019.
- Bogdan R, Biklen SK. Qualitative Research for Education: An Introduction to Theories and Methods, Fifth Edition. 5th ed. Pearson; 2006.
- Bertrand JT, Brown JE, Ward VM. Techniques for analyzing focus group data. Eval Rev. 1992;16(2):198–209. doi:10.1177/0193841X9201600206
- Onwuegbuzie AJ, Dickinson WB, Leech NL, Zoran AG. A qualitative framework for collecting and analyzing data in focus group research. Int J Qual Methods. 2009;8(3):1–21. doi:10.1177/160940690900800301
- Salas E, Cooke NJ, Rosen MA. On teams, teamwork, and team performance: discoveries and developments. Hum Factors. 2008;50(3):540–547. doi:10.1518/001872008X288457
- The Joint Commission. Behaviors that undermine a culture of safety. Sentinel Event Alert. 2008;40. Available from: www.jointcommission.org/assets/1/18/SEA_40.PDF. Accessed September 14, 2020.
- Zwarenstein M, Goldman J, Reeves S. Interprofessional collaboration: effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009;(3):CD000072.
- O’Leary KJ, Buck R, Fligiel HM, et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678–684. doi:10.1001/archinternmed.2011.128
- Pronovost P, Berenholtz S, Dorman T, Lipsett PA, Simmonds T, Haraden C. Improving communication in the ICU using daily goals. J Crit Care. 2003;18(2):71–75. doi:10.1053/jcrc.2003.50008
- Eraut M. Informal learning in the workplace. Stud Continuing Educ. 2004;26(2):247–273. doi:10.1080/158037042000225245
- Eraut M. Developing Professional Knowledge and Competence. Routledge; 2002.
- Baker DP, Gustafson S, Beaubien JM, Salas E, Barach P. Medical team training programs in health care. In: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in Patient Safety: From Research to Implementation (Volume 4: Programs, Tools, and Products). Advances in Patient Safety. Agency for Healthcare Research and Quality (US); 2005. Available from: http://www.ncbi.nlm.nih.gov/books/NBK20580/. Accessed February 4, 2019.
- Leasure EL, Jones RR, Meade LB, et al. There is no “I” in teamwork in the patient-centered medical home: defining teamwork competencies for academic practice. Acad Med. 2013;88(5):585–592. doi:10.1097/ACM.0b013e31828b0289
- O’Leary KJ, Boudreau YN, Creden AJ, Slade ME, Williams MV. Assessment of teamwork during structured interdisciplinary rounds on medical units. J Hosp Med. 2012;7(9):679–683.
- Beck J, Meyer R, Kind T, Bhansali P. The importance of situational awareness: a qualitative study of family members’ and nurses’ perspectives on teaching during family-centered rounds. Acad Med. 2015;90(10):1401–1407. doi:10.1097/ACM.0000000000000810
- Gonzalo JD, Wolpaw DR, Lehman E, Chuang CH. Patient-centered interprofessional collaborative care: factors associated with bedside interprofessional rounds. J Gen Intern Med. 2014;29(7):1040–1047. doi:10.1007/s11606-014-2817-x
- Lehmann LS, Brancati FL, Chen M-C, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997;336(16):1150–1156. doi:10.1056/NEJM199704173361606
