Abstract
Background
COPD guidelines non-concordance is a challenge frequently highlighted by respiratory experts. Despite the provision of comprehensive evidence-based national and international guidelines, the COPD burden to frontline healthcare services has increased in the last decade. Suboptimal guidelines concordance can be disruptive to health-related quality of life (HRQoL), hastening pulmonary function decline and surging overall morbidity and mortality. A lack of concordance with guidelines has created an escalating economic burden on health-care systems. Identifying interdisciplinary interventions to facilitate improved adherence to guidelines may significantly reduce re-admissions, enhance HRQoL amongst patients and their families, and facilitate economic efficiency.
Materials and Methods
This review adhered to the Joanna Briggs Institute (JBI) methodology for mixed methods systematic reviews and the PRISMA ScR reporting guidelines. Two independent reviewers screened abstracts and full text articles in consonance with inclusion criteria. The convergent integrative JBI method collated quantitative, qualitative and mixed methods studies from nine databases. JBI critical appraisal tools were utilised to assess the quality of research papers. The theoretical domains framework (TDF) along with a specifically developed COPD data extraction tool were adopted as a priori to collect and collate data. Identified barriers and corresponding clinical behavioural change solutions were categorised using TDF domains and behavior change wheel (BCW) to provide future research and implementation recommendations.
Results
Searches returned 1068 studies from which 37 studies were included (see ). COPD recommendations identified to be discordant with clinical practice included initiating non-invasive ventilation, over- or under-prescription of corticosteroids and antibiotics, and a lack of discharging patients with a smoking cessation plan or pulmonary rehabilitation. TDF domains with highest frequency scores were knowledge, environmental resources, and clinical behaviour regulation. Electronic order sets/digital proforma with guideline resources at point of care and easily accessible digital community referrals to target both pharmacological and non-pharmacological management appear to be a solution to improve concordance.
Conclusion
Implementation of consistent quality improvement intervention within hospitals for patients with COPD may exclude any implementation gap and prevent readmissions. Electronic proformas with digital referrals will assist with future evaluation audits to prioritise and target interventions to improve guidelines concordance.
Ethics and Dissemination
Ethical approval is not required, and results dissemination will occur through peer-reviewed publication.
PROSPERO Registration Number
CRD42020156267.
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive life-threatening lung disease identified as a major global healthcare burden.Citation1 According to the World Health Organization, COPD caused 3.23 million deaths in 2019 equating to 6% of overall deaths, with over 80% of those occurring in low- and middle-income countries.Citation2 The Australian National Morbidity Database reveals that in 2017–2018, there were 77,660 hospitalisations of people over 45, with the rate of hospitalisation at 732 per 100,000 population.Citation3 In Australia, 7.5% of people ≥40 years old have stage II or above COPD as classified by the Global Initiative for Obstructive Lung Disease (GOLD) criteria and 30% in the >75-years age group.Citation3,Citation4 COPD is the fifth leading cause of death in Australia and second avoidable cause of hospitalisation.Citation3,Citation4 Worldwide, COPD related mortality ranks high amongst developed countries with the United States at 8th, United Kingdom at 12th and Australia at 34th.Citation5 Patients with COPD and their families experience a considerable financial burden due to functional decline in the workplace and at home. COPD prevalence, morbidity, and mortality is highly reported from high-income countries albeit 90% mortality occurs in low and middle-income countries.Citation6 In an Australian context in 2015–2016, the treatment of patients with COPD was estimated to reach $976.9 million, which was 24% of total expenditure for all respiratory conditions.Citation6 Globally, COPD is predicted to increase its economic burden by US$2.3 trillion by 2030.Citation1 Varied COPD treatment and effective long-term preventative management strategies are however known to decrease the number of acute exacerbations, improve health-related quality of life outcomes, and sustain pulmonary function.Citation7
National guidelines in Australia (COPD-X plan) and international guidelines (Global Initiative for Chronic Obstructive Lung Disease [GOLD]) continue to highlight the significance of non-pharmacological interventions to improve HrQoL, prevent readmissions and acute exacerbations.Citation8,Citation9 COPD guidelines non-adherence in both pharmacological and non-pharmacological management is well-recognised and is a reported phenomenon in national and international literature.Citation10–Citation12 A COCHRANE systematic review on integrated disease management programs for COPD reported improved disease-related quality of life, increased exercise capacity, reduced hospital admissions and hospital days per person.Citation13 Sub-optimal dissemination and implementation impede adoption into clinical practice by interdisciplinary health professionals.Citation14,Citation15 Guidelines assist with the incorporation of evidence into clinical practice to improve patient outcomes.Citation16,Citation17 However, worldwide research reports lack of COPD guideline adherence.Citation11,Citation18–Citation22 Implications of guidelines non concordanceare repetitive readmissions with COPD exacerbations, increased economic burden, and poor optimisation of lung function and overall health.Citation12,Citation23,Citation24
This systematic review set out to identify known contributing factors towards COPD guidelines non-adherence from the time of admission to hospital to time of discharge. Given the scarcity of research on interdisciplinary guidelines concordance with the population of patients with COPD, the review included a mixed methods approach that enabled all available evidence to be incorporated into the review. The Theoretical Domains Framework (TDF) assists in helping to identify factors that influence a behavior. The TDF framework is used by researchers to identify factors; interventions were filtered and targeted towards interdisciplinary implementation with specific recommendations for local, national, and international health systems.Citation25–Citation27 The Theoretical Domains Framework collation of data allowed robust filtration of evidence from multiple sources to provide improved implementation strategies and clinical behaviour change solutions utilising behavior change wheel taxonomy to augment COPD guidelines concordance.Citation25,Citation27 Identified barriers, facilitators and corresponding clinical behavioral change solutions utilising a behavior change wheel are categorised towards 14 TDF domains.Citation25,Citation26 These include knowledge, skills, social/professional role identity, beliefs about capabilities, beliefs about consequences, memory attention and decision processes, environmental context and resources, intentions, goals, social influences, optimism, emotion, behavior regulation. includes TDF domains and frequency scores with barriers and potential solutions from included studies (see ). We hypothesised notable discordance in adherence to COPD guidelines and asserted that compiling modifiable factors and implementation strategies may improve awareness, increase adherence, and assist stakeholders to adopt implementation strategies to improve patient outcomes.
Table 1 TDFa Domains and Frequency Scores with Barriers and Potential Solutions from Included Studies
Methods
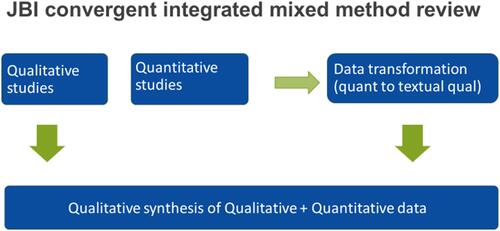
This review adheres to the Joanna Briggs Institute Methodology for Mixed Methods Systematic Reviews and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews Reporting Guidelines. The protocol for this study was published and registered in PROSPERO which elaborates on objective, search strategy, eligibility criteria, study selection, data collection, transformation and synthesis.Citation14 The mixed methods review provides a comprehensive synthesis compared with a single-method review as it combines quantitative and qualitative evidence to assist clinical decision-makers and policymakers to adopt an appropriate implementation strategy.Citation28 A convergent integrative method where quantitative evidence was qualitised to provide a narrative review is included to enable the integration of all studies and the ability to attain a deepened understanding of any discrepancies noted in the evidence (see ).Citation28 The 14 TDF domains and BCW taxonomy have guided the process for developing interventions specifically targeting identified barriers in three behavior change conditions: capability, opportunity, and motivation (referred to as the COM-B system).Citation25 Identified TDF domains causing non-adherence to guidelines were mapped to the capability (C), opportunity (O), and motivation (M) components, which form the behavior change wheel with nine intervention functions (education, persuasion, incentivisation, coercion, training, restriction, environmental restructuring, modeling and enablement) and seven policy change categories (guidelines, environmental/social planning, communication/marketing, legislation, service provision, regulation, fiscal measures).Citation25 Sub-components of COM-B were merged with the domains, barriers, and recommendations from the studies to produce interventions that if adopted by clinical stakeholders may assist in enhancing COPD guideline adherence.
Review Questions
What core elements of the COPD guidelines are adhered to by interdisciplinary health professionals?
What are the contributing factors to the lack of COPD guidelines concordance amongst interdisciplinary health professionals in hospitals?
Search Strategy and Study Selection
Qualitative, quantitative, and mixed methods studies were included to explore determinants of COPD guidelines concordance. A comprehensive three-tier search strategy was utilised to search nine databases (COCHRANE, EBSCO HOST, MEDLINE, SCIENCE DIRECT, JBI, SCOPUS, WEB OF SCIENCE, WILEY and DARE).Citation14 Studies published in English from 2010 to May 2021 from the nine identified databases were included. Although the protocol mentions including studies from 1997, during the review reported factors of non-adherence data was non-congruent with study reports in recent years. Hence, studies published before 2010 were excluded. Two independent reviewers screened abstracts (HI, CM) and full-text articles (HI, CM), (HI, MT), (HI, JL) in consonance with inclusion criteria. Disagreements that arose between the reviewers at each stage of the study selection process were resolved through discussion, or with a third reviewer (CM/MT). A PRISMA report of the search process and outcomes was produced. Inclusion criteria consisted of studies and reports published on interdisciplinary COPD guidelines concordance, compliance, or adherence in the hospital setting. Reviews of GOLD guidelines and COPD X plan guidelines were included. Exclusion criteria included studies not reported in English and studies which had not measured COPD guideline concordance. Primary health-care and community-based COPD guidelines concordance studies were excluded. The study population involved doctors, nurses, and allied health-worker reports on COPD guidelines concordance in the context of data from emergency departments, inpatient hospital units and hospital-based rehabilitation units.
Quality Appraisal
Quality appraisal was performed by two independent reviewers (HI, CM) utilising specific standardised critical appraisal instruments from the JBI system. Studies that were selected regardless of the methodological quality underwent extraction and synthesis. Critical appraisal results were tabled and appended to the review retrieval. See Supplementary Material.1).
Data Extraction and Transformation
A mixed methods data extraction tool designed for a convergent integrated approach (integration of qualitative data and “qualitised” data following data transformation) was published in the protocol and utilised to extract data.Citation14 This extraction tool included study type, the methodology, the number and characteristics of participants, the phenomenon of lack of concordance, guideline type, context (cultural and geographic), setting (hospitals, EDs and inpatient units), concordance with main recommendations of COPD guidelines, implementation method, evaluation and sustainability of implementation, and remissions within 30 days of hospital discharge. Two independent reviewers confirmed extracted data from articles and any disagreements were settled using the third reviewer utilising COVIDENCE systematic review management software. Quantitative data were converted to “qualitised data” following extraction according to the JBI convergent integrated approach. Quantitative numerical data were transfigured to textual or narrative interpretations to answer the overarching review question.
Data Synthesis and Integration
Extracted data in the form of themed textual description from quantitative studies plus themes and subthemes from qualitative studies were collated and categorised in congruence to 14 domains of TDF (see ). Applying the TDF assisted in identification of determinants or factors leading to a lack of COPD guidelines concordance. Identified barriers and enablers in guideline uptake were aligned with standard taxonomy of behavioral change technique to report existing and future recommendations for implementation strategies.Citation25,Citation26 Factors contributing to the lack of concordance with the guidelines were integrated based on similarity in meaning. This review adhered to the PRISMA-ScR reporting guidelines which also provided a comprehensive approach to suggest implementation strategies regarding any identified publication bias of this guidelines non-concordance phenomenon.
Results
This review included 37 studies (see ), that reported on COPD-X or GOLD guidelines concordance with 14 studies reported from Australia, 12 from Europe, 2 from Canada and the remaining 9 from developing countries. contains included studies demographics, barriers, potential solutions or recommendations (see ). COPD recommendations identified as highly discordant from clinical practice were initiating non-invasive ventilation, over- or under-prescription of corticosteroids, antibiotic use, and lack of discharging patients with smoking cessation and pulmonary rehabilitation plans. TDF domains with highest frequency scores above 15 and over 37 were knowledge, environmental resources, and clinical behavior regulation. Domains that scored below 15 were skills, memory attention and decision processes, social/ professional role identity. Results are disseminated in the following paragraphs as problems, related TDF domains bracketed within results, supporting evidence or statistics, solutions, and recommended implementation strategies from the literature.
Table 2 Included Studies Demographics, Barriers, Potential Solutions/Recommendations
Figure 1 Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.
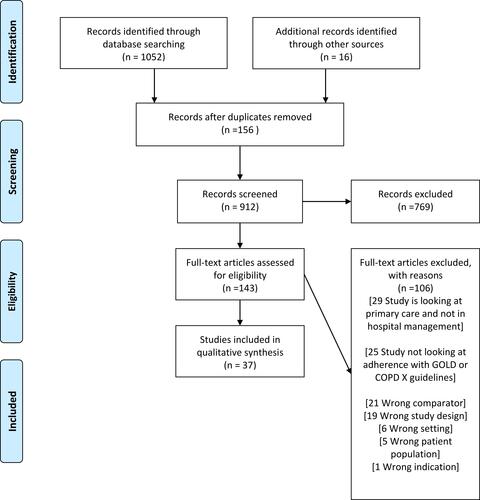
Figure 2 Represents data extraction graphic representation.
Diagnostic Utilisation of Spirometry, ABG and Oxygen Management
GOLD and COPD-X guidelines state diagnosis should occur utilising gold standard spirometry to detect persistent airflow limitation, however only 41% of Nigerian physicians knew spirometry diagnostic criteria and only 26.9% were aware of how to assess severity (knowledge).Citation29 Low rate of guideline adherence with 61.5% for 2011 and 49.6% for 2017 GOLD guidelines were reported from a Korean study.Citation30 Low utilisation of Arterial Blood Gas (ABG) data to utilise non-invasive ventilation (NIV) and diagnostic inaccuracy with respiratory failure is frequently reported in multiple studies.Citation11,Citation22–Citation25 Despite suitable ABG and NIV equipment being available patients were not started on this treatment.Citation22–Citation24,Citation30,Citation31 Lack of knowledge and awareness of spirometry guidelines was identified as a key contributor to mistreatment, misdiagnosis, and inaccurate management.Citation11,Citation12,Citation19,Citation20,Citation23,Citation29,Citation31,Citation32 Unavailability of spirometry test results despite previous diagnosis and admissions (behavioral regulation) was consistently addressed as a barrier from fragmented discharge planning and primary care diagnostic intervention.Citation22 Spirometry awareness campaigns and care bundles have successfully increased knowledge in some countries.Citation18–Citation20,Citation24,Citation33,Citation34 An accurate assessment of smoking history as a surrogate measure of the severity of COPD was reported as a potential substitute to spirometry particularly in the ED during acute exacerbation episodes when pulmonary function tests cannot be performed due to severity of presentation.Citation8,Citation18,Citation23
An Australian retrospective clinical audit reported unnecessary use of NIV in patients with adequate oxygenation (knowledge, behavior regulation)Citation10,Citation35 whereas another Australian study reported NIV was not utilised adequately despite meeting the guideline criteria (behavior regulation).Citation36 Low adherence was reported from Europe, Australia and Ireland in pre-hospital oxygen management which continues in the emergency department (until specialist review) with poor clinical outcome such as hypercapnic respiratory failure (social/professional role and identity).Citation10,Citation22,Citation24,Citation36,Citation37 Several patients not having an ABG test documented also received high-flow oxygen.Citation23 High-flow oxygen was used for the initial treatment of COPD exacerbations when only 53% of patients were recognised to have COPD.Citation32 In addition to patients not having an ABG test documented also receiving high-flow oxygen (behavior regulation),Citation11,Citation22,Citation38 reduced awareness of guidelines especially among junior doctors was identified (knowledge).Citation39 A reported disjunct exists between holistic respiratory ward-based COPD clinical pathways and atomistic acute ED clinical pathways generally due to the difference in care focus, time constraints, national targets, and lack of human and fiscal resources such as beds, clinicians, staff, and high patient turnover (environmental context and resources).Citation11,Citation15,Citation23,Citation40 Targeted speciality care order sets specifically designed for departmental needs and care focus such as in the ED is highly recommended for implementation.Citation11,Citation15,Citation41
Pharmacological Management
Guidelines suggest accurate pharmacological therapy will optimise function, prevent deterioration, prevent exacerbations and sustain pulmonary function.Citation8 Misalignment of prescribing with GOLD recommendations between respiratory physicians and general physicians was identified as being due to a lack of interspeciality communication and guidance amongst clinicians. This was one of the major barriers reported with COPD pharmacological management (social/professional role and identity).Citation36
Corticosteroids Guidelines Non-adherence and Potential Solutions
Multiple studies have reported on variability in duration, dosing and inconsistency from guidelines with corticosteroids management (behavioural regulation).Citation10,Citation11,Citation18,Citation30,Citation37,Citation38,Citation42,Citation43 Systemic corticosteroid regimens used in clinical practice are administered for much longer periods and at higher doses than recommended in guidelines (knowledge).Citation10,Citation11,Citation17,Citation25,Citation31–Citation34 Steroid doses relevant to an asthma diagnosis and treatment are utilised to treat for COPD (knowledge).Citation37 Despite the evidence, oral steroids are not inferior to intravenous steroids, with dose duration tripled from the recommended 5 days in practice (knowledge).Citation44 Use of steroids without indication or overtreatment with ICS inhalers have been reported from multiple studies leading to longer hospital length of stay and mortality.Citation10,Citation30,Citation37,Citation42 Approximately half of the COPD readmissions in an inpatient urban teaching hospital study in the United States did not receive steroids during their first admission.Citation18 Lack of awareness and knowledge of guidelines were reported to be a firm barrier to steroid prescription non-adherence (knowledge).Citation9,Citation10,Citation38,Citation42,Citation44 Interactive educational tools and clinical champions have appeared to provide an increase in pharmacological adherence by increasing awareness of the guidelines.Citation38,Citation45
Bronchodilators and Antibiotics Guidelines Non-adherence and Potential Solutions
Two studies, one Australian and one from Hong Kong, reported differences in prescription of long-acting bronchodilators (LABA) between general physicians and respiratory physicians despite guideline instructions (Social/professional role and identity).Citation36,Citation46 Inappropriate prophylactic antibiotic prescription despite normal white cell count is a concern with antimicrobial resistance an issue worldwide (Knowledge, behavioural regulation).Citation10,Citation22,Citation33,Citation38,Citation43,Citation47 Dual antibiotic therapy choice discordant from current guidelines was observed in 90% of patients in another Australian study.Citation48 Discordant duration of antibiotic therapy and failure to switch to oral antibiotics have been linked with an increased length of hospital stay (Knowledge).Citation48 The availability of a wide range of inhaler devices, coupled with a lack of patient education and checking of inhaler technique was noted as a major barrier potentially contributing to COPD exacerbations (Knowledge and skills).Citation15,Citation49 Lack of knowledge of updated guidelines and memory, attention or decision processes merged with environmental barriers such as low staffing, and time constraints contributed hugely to inaccurate pharmacological management. Dedicated AECOPD pathways may improve antibiotic or other drug selection and help to uplift pharmacological concordance with guidelines.Citation47 Easier to use devices and educational strategies on proper inhaler use from health caregivers can reduce readmissions.Citation42
Barriers and Potential Solutions for Increasing Pharmacological Guidelines Adherence
Respiratory specialists and nurses adhered to pharmacological guidelines more accurately over internists (Social/professional role and identity).Citation36,Citation50 Cross fertilization of knowledge across departments and interdisciplinary clinicians assists with consistently delivering pharmacological management to provide evidence-based care in the most efficient manner.Citation36 The development and validation of appropriate educational tools for inhaler techniques is necessary to assist clinicians and other health-care professionals who are involved in selecting inhalation devices.Citation14,Citation38 Given the wide range of inhaler devices available, inhaler prescription, technique and adherence are not checked or educated on well by interdisciplinary staff (Behavioural regulation).Citation32,Citation34,Citation36,Citation38,Citation42 Dedicated and holistic bundles of care for AECOPD have been implemented in the United Kingdom and have been demonstrated to improve patient management.Citation24 Training, modeling and enablement utilising education and other interventions to enhance self-learning among physicians was recommended and included strategies such as informational posters, and hospital guidelines with updated evidence. Educating clinicians regarding the indications and contraindication for corticosteroids and antibiotics including encouragement to prescribe according to the guidelines or standardizing prescriptions utilising electronic formats is a potential solution recommended by multiple studies.Citation10,Citation12,Citation41 Ambiguity, disagreement or when individual clinicians see the guideline as an interference in her/his freedom of clinical judgement is reported as a barrier (Social/professional role and identity).Citation38 Motivation with education, incentivisation post guideline adherence audits and environmental enablement utilising point of care resources may mitigate this phenomenon.Citation25 Change champions and senior leadership to discuss and influence total staff behaviour is reported to have assisted with this barrier in some implementation studies.Citation51
Non-Pharmacological Management
Non-pharmacological management includes pulmonary rehabilitation, smoking cessation, immunisations, self-management plans, COPD action plans, palliative care, and mental health assessment. GOLD and COPD-X guidelines recommend all patients with COPD after an acute exacerbation should have a referral for pulmonary rehabilitation within 2–3 weeks.Citation8 Major barriers were identified that included suboptimal understanding of COPD non-pharmacological recommendations, lack of perceived treatment benefit, along with ambiguity on self-efficacy and time constraints (knowledge, environmental and context resources).Citation19,Citation27,Citation33,Citation36
Pulmonary Rehabilitation Barriers and Potential Solutions
In studies surrounding guidelines adherence evidence shows very low pulmonary rehabilitation referrals after a COPD exacerbation (Behavioural regulation).Citation10,Citation11,Citation20,Citation31,Citation33,Citation42 Referral rates to pulmonary rehabilitation have reportedly increased from 13.6% to 68% with implementation of a COPD care bundle reported from a pre- and post-intervention study conducted in one Ireland inpatient unit.Citation20 Lack of knowledge of benefits, updated knowledge (in reference to publishing years), knowledge of existing community resources, and lack of patient education regarding attendance of these programs were identified as major barriers (Knowledge). These knowledge deficits are identified as particular barriers for non-respiratory physicians (Knowledge).Citation20,Citation38,Citation52 Some other barriers include lower support for rehabilitation at multiple levels such as time constraints, difficult referral process, lack of staffing resources, infrastructure, and lack of clarity on who provides the referral (Environmental and Context resources, Social/professional role identity).Citation25,Citation36 Well-structured screening protocols or program-based multimodality COPD care services are highly recommended for development to address identified barriers.Citation12 Political commitment, sustained funding, and establishment of a pulmonary rehabilitation unit were found to be of the utmost importance for Nigerian and possibly other developing COPD populations.Citation2,Citation29 Recommendations of referral to rehabilitation professionals included making lengthier commitments to rehabilitation, facilitating more activity by motivating and encouraging patients with COPD, and reducing their fears and reinforcing the benefits of lifelong activity.Citation20,Citation52
Smoking Cessation, Inhaler Technique, Immunisation and Vaccination Guidelines Non-adherence and Potential Solutions
Smoking cessation and immunisation are highly recommended and significant in preventing COPD exacerbation and preserving lung function. A general staff perception acting as a barrier concluded these to be the responsibility of the primary care physician, hence a lack of addressing this problem during an acute admission is reported in two studies (Social/professional role and identity).Citation20,Citation52 Lack of prevention of future exacerbations with particular attention to smoking cessation, immunisation, knowledge of current therapy including inhaler technique and self-management is reportedly low (Knowledge).Citation29,Citation33,Citation34,Citation52 Minimal support is provided to implement smoking cessation in public hospitals with human resources, staffing, smoking cessation teams/champions, telephone support, and a lack of role clarity in terms of initiating the cessation education (Environmental and Context resources, Social/ professional role identity).Citation10,Citation29,Citation34,Citation52 In Ireland implementation of a care bundle and care pathway improved referral for smoking cessation assistance from 18.2% to 100% and significantly lowered the 30-day readmission rates.Citation20,Citation34,Citation53 Care bundle implementation strategies may be adopted by national and international health systems to improve smoking cessation. Multifaceted implementation programs including patient pamphlets, brochures, electronic learning modules, and electronic reminders at point of clinical practice have proven successful.Citation12 Vaccination provision records are lower in summer months compared with winter admissions and unvaccinated patients were not vaccinated in the acute setting.Citation18 Time- and resource-poor clinicians often overlook vaccination as a primary care physician responsibility and trust this will be completed in the community setting (Social/professional role and identity, Environmental and Context resources).Citation10,Citation20,Citation33,Citation54,Citation55 Affordability of vaccines in developing countries was identified as a barrier (Environmental and Context resources).Citation29
Enablers identified were that physicians should collaborate with hospital authorities to establish smoking cessation teams, vaccination change champions and pulmonary rehabilitation units.Citation56 Difficulty remembering the most up to date guidelines or recalling all delivery devices and management modality from COPD guidelines (Memory attention and decision-making process) was problematic and presented as a barrier.Citation12,Citation41,Citation57 Environmental restructuring, enablement, and education initiated with Point of Care checklists in respiratory wards have improved guideline adherence.Citation12,Citation24,Citation41 Health professional education, decision-making algorithms (including electronic systems), reminders at the time of consultation, and continuous quality assurance programs with admission/ discharge bundles using electronic prescribing systems are recommended strategies to add consistency and reduce error or non-conformance.Citation12,Citation18,Citation24,Citation58
Anxiety/ Depression Screening and Palliative Care Guidelines Non-adherence and Potential Solutions
Barriers in screening and pharmacological treatment for clinically confirmed depression were documented as not being part of routine care, albeit this was not measured by many studies that reported on non-adherence of COPD clinical guidelines (Behavioral regulation).Citation41 The prevalence of clinical depression in patients with COPD varies from 18% to 80%, yet this aspect is not screened regularly with AECOPD.Citation59 Palliative care and care planning in advanced COPD remain discordant largely due to difficulty in prognosis of the disease due to variable disease trajectories (Behavioral regulation, Social/professional role and identity).Citation60 Care is reported to be fragmented, episodic and reactive and the role of carers were poorly recognised in end stage COPD (Knowledge and Behavioral regulation).Citation61,Citation62 Respiratory doctors initiating palliative care conversations, and with subsequent referral to palliative care clinicians and integrating multidisciplinary services could address fragmented care, however more work is required in this space (Social/professional role and identity).Citation62 Clinicians lacking time, fearful of taking away patient hope, lack of palliative specialist availability, insufficient communication and collaboration, poor access and lack of service availability are major barriers to COPD adherence (Environmental and context resources).Citation60,Citation62–Citation65 COPD action plans reduce hospitalisations and are recommended as part of COPD self-management plans.Citation8 Patients often receive minimal to no education on acute discharge from inpatient units. More work is required in this space (Knowledge and Behavioural regulation).Citation66 Recommendations that require patient education and team collaboration are the ones particularly discordant with current guidelines (Knowledge).Citation33,Citation34,Citation49 Lack of mental health assessments and palliative care significant and clinically appropriate awareness strategies aligned with poorly controlled COPD patient outcomes presented as major barriers (Social/professional role and identity, Behavioral regulation).
Potential Solutions to Improve Guidelines Adherence with Non-Pharmacological Management
Targeted health professional education, electronic checklists, user friendly and easy access resources, improvised communication between primary care physicians, educational campaigns, hospital staff audit and educational sessions presented in many studies were specifically related to improving concordance in health-care settings.Citation11,Citation12,Citation23,Citation32–Citation34,Citation38,Citation47–Citation49,Citation52,Citation54,Citation58,Citation66 Care bundles have resulted in reduced readmissions for COPD and increased adherence to guidelines by improving referrals for inhaler technique (59.1% to 91.2%) and smoking cessation (13.6% to 68%).Citation20 Referral rates to pulmonary rehabilitation rose higher and similar improvements were seen in the administration of self-management plans.Citation20 Communication between Guideline Committees and Clinicians should be improved and variability in resources and organisation of hospitals, patient characteristics, process of care, and outcomes needs to be addressed.Citation54
Discussion
Multidimensional barriers have evidently contributed to global COPD guideline non-concordance. Research repetitively reports a lack of awareness, knowledge and skills being the significant challenges demonstrating guidelines are not well disseminated or implemented in clinical practice. Major barriers are reported as a lack of awareness, lack of considering the complexity of the guideline, high turnover of patients and the involvement of inter disciplines. Mitigating strategies include providing guideline resources at point of care electronically. Diagnostic and pharmacological management are mostly well adhered to compared to non-pharmacological management (self-management education, COPD action plans, smoking cessation, pulmonary rehabilitation, palliative care, inhaler adherence and technique, home oxygen, immunisation). Non-pharmacological management seeks to provide better implementation strategies to enhance guideline concordance. Strategic implementation for interdisciplinary communication and cross fertilisation of knowledge is recommended by researchers for decades and yet globally literature is still reporting non-adherence. This review provides the inclusion of multifaceted implementation strategies for targeted implementation of COPD guidelines for national and international clinical settings compiled from research evidence and utilising the TDF implementation framework. Motivation using environmental restructuring, increasing education, and disseminating guidelines in the working area or utilising suitable implementation strategies is highly associated with improving guideline adherence rates.
This study collated all barriers and probable solutions, and recommends multiple strategies that may be adopted by stakeholders with suitability to local or national needs (see ). A significant recommendation from this study arising from frequency scores and the implementation framework is to install the proforma ideally in an electronic format in acute care settings from hospital (triage to discharge) to primary care. Concurrent studies and reviews have similar findings and recommend electronic or pre-formatted order sets to improve guideline adherence in Australia.Citation10–Citation12,Citation18,Citation20,Citation33,Citation47,Citation54 This implementation strategy appears to be capable of addressing almost all barriers (see ). The electronic proforma will provide easy access, increase knowledge and awareness, provide role clarity, time efficiency, and provide all resources in one place with self-learning resources. Other advantages include consistent pharmacological and non-pharmacological standardisation of management, provision of patient information or self-management resources, electronic referrals, data for future research, practicability, interdisciplinary acceptability, easier access to community services, automation of processes, discharge planning with primary care, and clinical behavior regulation. Future potential of such digital proforma with access to primary care records with read and write access will alleviate communication issues between primary care and speciality clinicians. Potential digital proforma can target fragmented care elements to initiate a new implementation strategy, with the capacity to liaise with a community pharmacist, nurses and other interdisciplinary staff from the hospital to reduce or avoid long hospital stays. Educating and self-learning opportunity is available with this strategy of implementation in the case of an interdisciplinary clinician requiring education resources to be provided to patients or staff. Pro-forma aided COPD management in concordance to guidelines significantly improved the standards of care in COPD patients especially among junior doctors.Citation57 ED short stay unit pathways and access to community follow-up care with primary care or specialist clinics, and disease-specific outreach services is recommended.Citation17 Guidelines specifically targeted to the process of emergency care may be more meaningful to ED clinicians, however further research is warranted to understand best implementation strategies for the Emergency department.Citation11,Citation67
Table 3 Summary Table on Electronic Proforma’s Ability to Address the Identified Barriers
Strengths and Limitations
This mixed method systematic review explored both qualitative and quantitative studies to deeply comprehend barriers to interdisciplinary staff guideline adherence. The Theoretical Domains Framework (TDF) utilisation facilitates understanding of existing barriers and probable clinical behaviour change solutions to improve concordance. Interdisciplinary perspectives to improve collaboration and concordance may lead to multifaceted implementation strategies. Due to the wide gap and the different focus of studies only three domains were identified from the TDF. Paucity of existing good quality data and reporting may confine our ability to report true barriers of concordance.
Conclusion
Barriers and potential solutions were identified for most clinical recommendations from the guidelines. The utilisation of the TDF implementation framework suggests electronic order sets/ proforma with guideline resources at point of care and easily accessible digital community referrals. This enables targeted recommendations to both pharmacological and non-pharmacological management that reverberates solutions to improve concordance. Various other implementation strategies are also recommended in this study for developing countries where digitalising is not an immediate option. Care bundles and clinical champions have proven to be effective in Europe and Australia. Stakeholders will have the opportunity to compare, analyse and conduct feasibility studies of different approaches recommended in this study that may be suitable for their settings.
Abbreviations
COPD, chronic obstructive pulmonary disease; TDF, theoretical domains framework; E-ICP, electronic integrated COPD proforma; HRQoL, health-related quality of life; JBI, Joanna Briggs Institute; GOLD, Global Initiative for Obstructive Lung Disease; COPD-X plan, chronic obstructive pulmonary disease-X plan; ABG, arterial blood gas; NIV, non-invasive ventilation; ED, emergency department; LABA, long-acting bronchodilators; AECOPD, acute exacerbation of chronic obstructive pulmonary disease.
Patient and Public Involvement
No patients from the included studies were involved in this review.
Ethics and Dissemination
Ethics approval is not required for this study as all data were obtained from publicly available studies. Knowledge and interpretations from this review will provide recommendations towards prominent implementation strategies to increase COPD guideline concordance. The results of this study will be presented before industry stakeholders, interdisciplinary clinicians, and appropriate future conferences to develop and assist with implementation initiatives.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Acknowledgments
We acknowledge Professor Sonya Osborne for her valuable input and expertise during University of Southern Queensland writing retreats. We acknowledge expertise of the University of Southern Queensland, Health Sciences Librarian, Rowena McGregor for assistance during the preliminary search phase.
Disclosure
The authors report no Competing interests related to this work.
References
- Quaderi S, Hurst J. The unmet global burden of COPD. Glob Health Epidemiol Genom. 2018;3. doi:10.1017/gheg.2018.1
- World Health Organisation. WHO global health estimates: the top 10 causes of death; 2020.
- The Australian Lung Foundation. COPD: the statistics, The Australian Lung Foundation; 2016.
- Australian Institute of Health and Welfare. Chronic obstructive pulmonary disease; 2017. Available from: https://www.aihw.gov.au/reports/chronic-respiratory-conditions/copd/contents/treatment-management. Accessed December 16, 2021.
- British Lung Foundation. Deaths from COPD; 2012. Available from: https://statistics.blf.org.uk/copd. Accessed December 16, 2021.
- May SM, Li JTC. Burden of chronic obstructive pulmonary disease: healthcare costs and beyond. In: Allergy and Asthma Proceedings. OceanSide Publications; 2015.
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. World Health Organisation. PLoS Med. 2006;3:209–224.
- Yang IA, George J, Jenkins S. The COPD-X Plan: Australian and New Zealand Guidelines for the management of chronic obstructive pulmonary disease 2018; 2018.
- Ruth Hadfield MH. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2019 report. Ruth Hadfield MH, ed; 2019.
- Sha J, Worsnop CJ, Leaver BA, et al. Hospitalised exacerbations of chronic obstructive pulmonary disease: adherence to guideline recommendations in an Australian teaching hospital. Intern Med J. 2019;50:453–459.
- Kelly AM, Van Meer O, Keijzers G, et al. Get with the guidelines - management of COPD in EDs in Europe and Australasia is sub-optimal. Intern Med J. 2019. doi:10.1111/imj.14323
- Overington JD, Huang YC, Abramson MJ, et al. Implementing clinical guidelines for chronic obstructive pulmonary disease: barriers and solutions. J Thorac Dis. 2014;6(11):1586–1596. doi:10.3978/j.issn.2072-1439.2014.11.25
- Kruis AL, Smidt N, Assendelft WJ, et al. Integrated disease management interventions for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013. doi:10.1002/14651858.CD009437.pub2
- Issac H, Moloney C, Taylor M, et al. Protocol: mapping of modifiable barriers and facilitators with interdisciplinary chronic obstructive pulmonary disease (COPD) guidelines concordance within hospitals to the theoretical domains framework: a mixed methods systematic review protocol. BMJ Open. 2020;10(7):e036060. doi:10.1136/bmjopen-2019-036060
- Hancy Issac MT, Moloney C, Lea J. Exploring factors contributing to Chronic Obstructive Pulmonary Disease (COPD) guideline non-adherence and potential solutions in the emergency department: interdisciplinary staff perspective. J Multidiscip Healthc. 2021;14:767. doi:10.2147/JMDH.S276702
- Légaré F, Ratté S, Gravel K, et al. Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns. 2008;73(3):526–535. doi:10.1016/j.pec.2008.07.018
- Francke AL, Smit MC, de Veer AJ, et al. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Med Inform Decis Mak. 2008;8(1):1–11. doi:10.1186/1472-6947-8-38
- Lipari M, Smith AL, Kale-Pradhan PB, et al. Adherence to GOLD guidelines in the inpatient COPD population. J Pharm Pract. 2018;31(1):29–33. doi:10.1177/0897190017696949
- Menzella F, Facciolongo N, Lusuardi M, et al. Clinical audit on diagnostic accuracy and management of respiratory failure in COPD. Respir Care. 2012;57(12):2067–2073. doi:10.4187/respcare.01502
- Migone C, O’Connor M, Kelly E, et al. Patients hospitalised with an acute exacerbation of COPD: is there a need for a discharge bundle of care? Ir Med J. 2015;108(9):273–275.
- Cousins JL, Wood-Baker R, Wark PAB, et al. Management of acute COPD exacerbations in Australia: do we follow the guidelines? ERJ Open Res. 2020;6(2):00270–2019. doi:10.1183/23120541.00270-2019
- Roberts CM, Lopez-Campos JL, Pozo-Rodriguez F, et al. European hospital adherence to GOLD recommendations for chronic obstructive pulmonary disease (COPD) exacerbation admissions. Thorax. 2013;68(12):1169–1171. doi:10.1136/thoraxjnl-2013-203465
- Khialani B, Sivakumaran P, Keijzers G, et al. Emergency department management of acute exacerbations of chronic obstructive pulmonary disease and factors associated with hospitalization. J Res Med Sci. 2014;19(4):297–303.
- McCarthy C, Brennan J, Brown L, et al. Use of a care bundle in the emergency department for acute exacerbations of chronic obstructive pulmonary disease: a feasibility study. Int J Chron Obstruct Pulmon Dis. 2013;8:605. doi:10.2147/COPD.S52883
- Michie S, Atkins L, West R. The Behaviour Change Wheel. A Guide to Designing Interventions. 1st ed. Great Britain: Silverback Publishing; 2014:1003–1010.
- Atkins L, Francis J, Islam R, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1):1–18. doi:10.1186/s13012-017-0605-9
- Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. doi:10.1007/s12160-013-9486-6
- Stern C, Lizarondo L, Carrier J, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Synth. 2020;18(10):2108–2118. doi:10.11124/JBISRIR-D-19-00169
- Desalu OO, Onyedum CC, Adeoti AO, et al. Guideline-based COPD management in a resource-limited setting—physicians’ understanding, adherence and barriers: a cross-sectional survey of internal and family medicine hospital-based physicians in Nigeria. Prim Care Res J. 2013;22(1):79–85. doi:10.4104/pcrj.2013.00014
- Kim T-O, Shin H-J, Kim Y-I, et al. Adherence to the GOLD guideline in COPD management of South Korea: findings from KOCOSS study 2011–2018. Chonnam Med J. 2019;55(1):47–53. doi:10.4068/cmj.2019.55.1.47
- Johnson C, Connolly MJ, Clover S, et al. Audit of acute exacerbations of chronic obstructive pulmonary disease at Waitemata District Health Board, New Zealand. New Zealand Med J. 2013;126(1378):15–25.
- Susanto C, Thomas PS. Assessing the use of initial oxygen therapy in chronic obstructive pulmonary disease patients: a retrospective audit of pre-hospital and hospital emergency management. Intern Med J. 2015;45(5):510–516. doi:10.1111/imj.12727
- Markun S, Franzen DP, Dalla Lana K, et al. Acute exacerbated COPD: room for improvement in key elements of care. Int J Chron Obstruct Pulmon Dis. 2017;12:2969. doi:10.2147/COPD.S145496
- Vanhaecht K, Lodewijckx C, Sermeus W, et al. Impact of a care pathway for COPD on adherence to guidelines and hospital readmission: a cluster randomized trial. Int J Chron Obstruct Pulmon Dis. 2016;11:2897. doi:10.2147/COPD.S119849
- Cousins JL, Wark PA, McDonald VM. Acute oxygen therapy: a review of prescribing and delivery practices. Int J Chron Obstruct Pulmon Dis. 2016;11:1067. doi:10.2147/COPD.S103607
- Wijayaratne K, Sivakumaran P, Wijayaratne K, et al. Differences in care between general medicine and respiratory specialists in the management of patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. Ann Thorac Med. 2013;8(4):197–203. doi:10.4103/1817-1737.118499
- Harrison A, Borg B, Thompson B, et al. Inappropriate inhaled corticosteroid prescribing in chronic obstructive pulmonary disease patients. Intern Med J. 2017;47(11):1310–1313. doi:10.1111/imj.13611
- Tang CY, Taylor NF, McDonald CF, et al. Level of adherence to the GOLD strategy document for management of patients admitted to hospital with an acute exacerbation of COPD. Respirology. 2014;19(8):1191–1197. doi:10.1111/resp.12361
- Alsubaiei M, Frith PA, Cafarella PA, et al. COPD care in Saudi Arabia: physicians‘ awareness and knowledge of guidelines and barriers to implementation. Int J Tuberc Respir Dis. 2017;21(5):592–595. doi:10.5588/ijtld.16.0656
- Sneath E, Bunting D, Hazell W, et al. Pre-hospital and emergency department pathways of care for exacerbations of chronic obstructive pulmonary disease (COPD). J Thorac Dis. 2019;11(Suppl 17):S2221. doi:10.21037/jtd.2019.10.37
- Gerber A, Moynihan C, Klim S, et al. Compliance with a COPD bundle of care in an Australian emergency department: a cohort study. Clin Respir J. 2018;12(2):706–711. doi:10.1111/crj.12583
- Hsieh M-J, Huang S-Y, Yang T-M, et al. The impact of 2011 and 2017 Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD) guidelines on allocation and pharmacological management of patients with COPD in Taiwan: Taiwan Obstructive Lung Disease (TOLD) study. Int J Chron Obstruct Pulmon Dis. 2018;13:2949. doi:10.2147/COPD.S176065
- Ta M, George J. Management of chronic obstructive pulmonary disease in Australia after the publication of national guidelines. Intern Med J. 2011;41(3):263–270. doi:10.1111/j.1445-5994.2009.02133.x
- Marcos PJ, Nieto-Codesido I, de Jorge Dominguez-Pazos S, et al. Treatment with systemic steroids in severe chronic obstructive pulmonary disease exacerbations: use of short regimens in routine clinical practice and their impact on hospital stay. Archivos de Bronconeumología. 2017;53(11):611–615. doi:10.1016/j.arbr.2017.09.007
- Sonstein L, Clark C, Seidensticker S, et al. Improving adherence for management of acute exacerbation of chronic obstructive pulmonary disease. Am J Med. 2014;127(11):1097–1104. doi:10.1016/j.amjmed.2014.05.033
- Au LH, Chan HS. Severity of airflow limitation, co-morbidities and management of chronic obstructive pulmonary disease patients acutely admitted to hospital. Hong Kong Med J. 2013;19(6):498–503. doi:10.12809/hkmj133909
- Brownridge D, Zaidi S. Retrospective audit of antimicrobial prescribing practices for acute exacerbations of chronic obstructive pulmonary diseases in a large regional hospital. J Clin Pharm Ther. 2017;42(3):301–305. doi:10.1111/jcpt.12514
- Fanning M, McKean M, Seymour K, et al. Adherence to guideline‐based antibiotic treatment for acute exacerbations of chronic obstructive pulmonary disease in an Australian tertiary hospital. Intern Med J. 2014;44(9):903–910. doi:10.1111/imj.12516
- Melani AS, Paleari D. Maintaining control of chronic obstructive airway disease: adherence to inhaled therapy and risks and benefits of switching devices. COPD. 2016;13(2):241–250. doi:10.3109/15412555.2015.1045972
- Sandhu SK, Chu J, Yurkovich M, et al. Variations in the management of acute exacerbations of chronic obstructive pulmonary disease. Can Respir J. 2013;20(3):175–179. doi:10.1155/2013/501038
- Goedken CC, Livorsi DJ, Sauder M, et al. “The role as a champion is to not only monitor but to speak out and to educate”: the contradictory roles of hand hygiene champions. Implement Sci. 2019;14(1):1–11. doi:10.1186/s13012-019-0943-x
- Pretto JJ, McDonald VM, Wark PAB, et al. Multicentre audit of inpatient management of acute exacerbations of chronic obstructive pulmonary disease: comparison with clinical guidelines. Intern Med J. 2012;42(4):380–387. doi:10.1111/j.1445-5994.2011.02475.x
- Seys D, Bruyneel L, Sermeus W, et al. Teamwork and adherence to recommendations explain the effect of a care pathway on reduced 30-day readmission for patients with a COPD exacerbation. COPD. 2018;15(2):157–164. doi:10.1080/15412555.2018.1434137
- Pozo-Rodríguez F, López-Campos JL, Álvarez-martínez CJ, et al. Clinical audit of COPD patients requiring hospital admissions in Spain: AUDIPOC study. PLoS One. 2012;7(7):e42156. doi:10.1371/journal.pone.0042156
- Jouleh B, Erdal M, Eagan TM, et al. Guideline adherence in hospital recruited and population based COPD patients. BMC Pulm Med. 2018;18(1):1–9. doi:10.1186/s12890-018-0756-8
- Desalu OO, Onyedum CC, Adeoti AO, et al. Unmet needs in asthma treatment in a resource-limited setting: findings from the survey of adult asthma patients and their physicians in Nigeria. Pan Afr Med J. 2013;16:1–13. doi:10.11604/pamj.2013.16.20.2798
- Sen B, Woollard M, Desira NL. Does the introduction of a COPD pro-forma improve the standards of care delivered by junior doctors in the emergency department. COPD. 2010;7(3):199–203. doi:10.3109/15412555.2010.481699
- Masoompour SM, Mohammadi A, Mahdaviazad H. Adherence to the Global Initiative for Chronic Obstructive Lung Disease guidelines for management of COPD: a hospital-base study. Clin Respir J. 2016;10(3):298–302. doi:10.1111/crj.12215
- Pumar IM, Gray CR, Walsh RJ, Yang. IA, Rolls TA, Ward DL. Anxiety and depression—Important psychological comorbidities of COPD. J Thorac Dis. 2014;11(6):1615–1631.
- Smallwood N, Currow D, Booth S, et al. Attitudes to specialist palliative care and advance care planning in people with COPD: a multi-national survey of palliative and respiratory medicine specialists. BMC Palliat Care. 2018;17(1):1–8. doi:10.1186/s12904-018-0371-8
- Crawford G, Brooksbank MA, Brown M, et al. Unmet needs of people with end‐stage chronic obstructive pulmonary disease: recommendations for change in A ustralia. Intern Med J. 2013;43(2):183–190. doi:10.1111/j.1445-5994.2012.02791.x
- Smallwood N, Thompson M, Warrender-Sparkes M, et al. Integrated respiratory and palliative care may improve outcomes in advanced lung disease. ERJ Open Res. 2018;4(1):00102–2017. doi:10.1183/23120541.00102-2017
- Vermylen JH, Szmuilowicz E, Kalhan R. Palliative care in COPD: an unmet area for quality improvement. Int J Chron Obstruct Pulmon Dis. 2015;10:1543. doi:10.2147/COPD.S74641
- Bloom CI, Slaich B, Morales DR, et al. Low uptake of palliative care for COPD patients within primary care in the UK. Eur Respir J. 2018;51(2):1701879. doi:10.1183/13993003.01879-2017
- Philip J, Crawford G, Brand C, et al. A conceptual model: redesigning how we provide palliative care for patients with chronic obstructive pulmonary disease. Palliat Support Care. 2018;16(4):452–460. doi:10.1017/S147895151700044X
- Seys D, Bruyneel L, Decramer M, et al. An international study of adherence to guidelines for patients hospitalised with a COPD exacerbation. COPD. 2017;14(2):156–163. doi:10.1080/15412555.2016.1257599
- Considine J, Botti M, Thomas S. Emergency department management of exacerbation of chronic obstructive pulmonary disease: audit of compliance with evidence‐based guidelines. Intern Med J. 2011;41(1a):48–54. doi:10.1111/j.1445-5994.2009.02065.x
- Moher D, Liberati A, Altman D, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10). doi:10.1016/j.jclinepi.2009.06.005
