Abstract
The COVID-19 outbreak is a world health problem that affects millions of people. The pandemic is also causing burdens and challenges to health-care providers. Therefore, this study aimed to examine and help understand health-care providers’ problems when caring for COVID-19 patients. An integrative review following Whittemore and Kanfl’s approach was used along with a systematic search for emerging online databases and grey literature conducted from January to August 2021. The quality of papers was analyzed and a report was presented following PRISMA guidelines. A total of 18 articles that were predominantly descriptive with five themes, including mental health problems in the early stage of COVID-19 outbreak, working stress, physical and psychological impacts of disease, and the lack of support were analyzed. The results showed the pandemic’s significant psychological impact on health-care providers directly caring for COVID-19 patients. Emotional, facilities and family support are needed to maintain the health-care providers’ well-being.
Introduction
COVID-19, a respiratory tract infection caused by SARSCoV-2 has caused a tremendous impact around the world. The coronavirus was first reported in Wuhan, China, in December 2019 and spread exponentially to other countries worldwide.Citation1,Citation2 Clinical syndromes of COVID-19 are mild upper respiratory illness, severe pneumonia, and acute respiratory distress.Citation3–5 The global impact of coronavirus made the World Health Organization (WHO) declare as a pandemic on Mar 12, 2020, and an international public health emergency.Citation3,Citation5,Citation6 Hence, it is crucial to examine the psychological implications of the pandemic for the general public, patients, and health-care providers (HCPs) globally.Citation4,Citation7–9 As the frontline workers, health-care providers must care for the patients every day and face a high risk of being infected. Furthermore, they encounter greater risks of mental health problems, such as anxiety, depression, insomnia, and stress.Citation5,Citation10 These psychological problems are caused by working long hours in high-pressure environments, inadequate personal protective equipment, and inadequate organizational support.Citation11–14
Some studies have been conducted in many countries to identify the psychological outcomes and distress among the HCPs during the five months of the COVID-19 pandemic. The results showed that caring for COVID-19 patients was emotionally difficult for health-care workers due to stress, uncertainty, and stigmatization.Citation15–17 The distress may negatively impact HCP’s psychology, mental status, and working performance. Moreover, a systematic review found that disasters significantly affect the mental well-being of the HCPs.Citation18 However, there is no systematic appraisal and critique of the existing studies. An integrative review assesses diverse data sources and methodologies such as qualitative interviews, surveys, and observational studies.Citation19 The reviews could present a comprehensive understanding of phenomena relevant to health care. Therefore, this study aimed to examine and help understand public literature regarding the problems faced by health-care providers when caring for COVID-19 patients globally.
Materials and Methods
Design
An integrative review, based on Whittemore and Knafl,Citation19 was conducted. It is a method that allows for diverse methodologies involving qualitative and quantitative data as well non-experimental survey data to develop a holistic understanding.Citation19 The first stage of the review was problem identification to ensure that the study question and aim were clearly defined. Other stages involved completing a well-defined literature search, evaluating the data quality, synthesizing the data, and presenting results. The objectives of the literature review and study questions were formulated first to identify problems. The key questions were related to the problems facing the HCPs when caring for COVID-19 patients globally.
Eligibility Criteria
This integrative review included quantitative and qualitative data published between January 2020 and August 2021. The qualitative articles were studies using phenomenological and exploratory approaches. In contrast, the quantitative papers contained studies with cross-sectional design and primary data collected applying questionnaires.
Inclusion Criteria
The following inclusion criteria were utilized to obtain the most relevant articles:
Articles published in English between 2019–2021.
Articles focused on the problems faced by health-care providers.
All study methodologies were included.
Data Collection
The study questions were first developed before searching for journal articles published through electronic databases. A systematic literature search was performed using PubMed, PMC, Science Direct, Google Scholar, ProQuest, Scopus, EBSCO, and Web of Science. Furthermore, the psychological problems of the HCPs worldwide were examined through keyword searches PubMed Central (PMC), Science Direct, Google Scholars, and Web of Science. This study used the terms “psychological problems [All Fields]” or “psychological distress” and “the healthcare workers’ needs” or “psychological outcomes” and “COVID-19ʹs impact” and “coronavirus disease” or “COVID-19” and “healthcare professionals”. These keywords incorporated Boolean operators and truncation marks to obtain the needed articles.
Study Selection and Data Collection Process
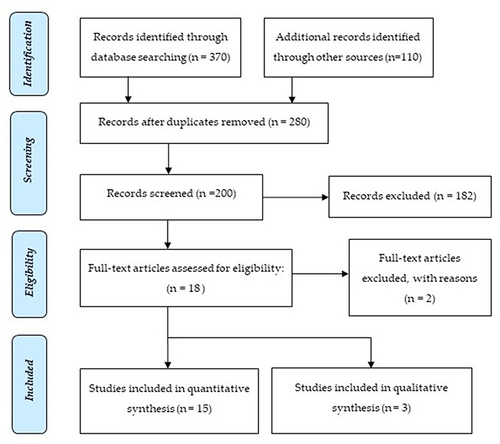
The titles of the articles were screened by three authors, HSM, FA, and SH to approve those that met the criteria used in the selection. The authors reviewed and approved information to be added in the final review. The selection process is illustrated by the Preferred Reporting Items or Systematic Reviews and Meta-Analysis (PRISMA) flow chart.Citation20
The search for electronic databases resulted in 480 titles and abstracts but were reduced to 200 papers after duplicates and some abstracts were removed. Furthermore, the 183 papers that did not meet the criteria were excluded. The authors also ensure that the selected articles were published in reputable journals by checking the name of the journal on the website. The remaining 17 papers which explored problems and demands of the HCPs when caring for COVID-19 patients were included in the final review, as shown in .
Figure 1 Flowchart describing article search and selection.
Quality Critical Appraisal
The quality of papers was independently appraised by two authors, HSM and YT. Full-text articles were evaluated using The Critical Appraisal Skills Program (CASP) research checklists,Citation21 to appraise the rigour, key methods, credibility, and relevance of the literature considered for inclusion. Both reviewers assessed the risk of bias, and the quality of studies was graded as moderately good on the scale and diverse in sources and discussion.
Data Synthesis and Presentation
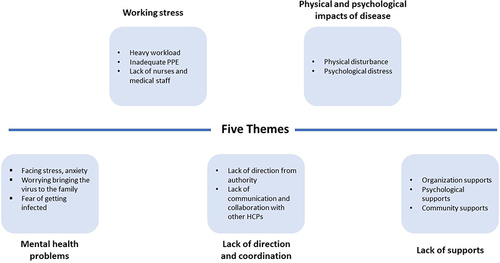
There are 18 quantitative and qualitative articles analyzed using a mixed-methods synthesis based on the study purpose, methods, and findings.Citation19,Citation22 The results in show the problems of the health-care providers (HCPs).
Table 1 Summary of Reviewed Articles
Results
Characteristics of the Studies
This review analyzed 15 quantitative and 3 qualitative studies published in 2020–2021. Most quantitative studies used the cross-sectional approach in data collection. In contrast, the qualitative studies used phenomenology with in-depth interviews. outlines the studies contained in the review and presents their design, sample size, instruments, and main findings. Specifically, 13 papers came from China, and one each from Singapore, Italy, Germany, India, and Bangladesh. Most of the selected articles came from China because, at the time of conducting systematic searching, the publication of research related to COVID-19 mostly came from China.
The results were integrated into themes with regard to their central issues and common meanings. This review identified four themes in the literature as shown in that addressed problems facing health-care workers when caring for COVID-19 patients.
The main themes include following points:
Mental health problems during COVID-19 outbreak.
Working stress.
Lack of direction and coordination.
Physical and psychological impacts of disease.
Lack of support.
Theme 1: Mental Health Problems During COVID-19
People are under increased psychological pressure, including health-care providers, facing the pandemic. This review found 16 studies stating that the frontline health-care providers suffered stress when caring for patients. The HCPs had psychological distress symptoms such as moderate to a high of anxiety, stress, worry, and depression, especially in the early pandemic stages.Citation23,Citation25–28,Citation30–40 Moderate and severe anxiety was associated with directly treating and caring for patients and lacking adequate personal protective equipment. Furthermore, the HCPs expressed feelings of anxiety, vulnerability, pain, and peril to their life and family. After reading and understanding the articles under review, a thematic analysis was conducted to assess the mental problems of the HCPs during the outbreak. This study found that HCPs faced suffered stress when caring for patients.
Theme 2: Working Stress
As the frontline in caring for COVID-19 patients, the HCPs have vital roles in delivering optimal health-care services. Their physical and mental health and safety are vital for providing continuous and safe patient care. However, this study identified that the HCPs were under working stress. Furthermore, several studiesCitation23,Citation24,Citation38–40 showed that the HCPs experienced job stress due to heavy workloads, long working hours, under-staffing, and high risk of infection due to lack of personal protective equipment (PPE). This study has shown that a high mental workload is the main source of stress in HCPs when caring for COVID-19 patients.
Theme 3: Lack of Direction and Coordination
This study showed that many HCPs lacked coordination and collaboration from nurses and medical doctors, especially from other wards, specialties, and different provinces,Citation23,Citation24,Citation40 potentially influencing working conditions. Working together, collaboration, coordination, and communication with a new multidisciplinary team were challenging. However, this is necessary when caring for COVID-19 patients, meaning that the HCPs should work together effectively and efficiently.
Theme 4: Physical and Psychological Impact of the Disease
Ten studies of this review showed that the HCPs on the front line directly implicated in diagnosis, treatment, and caring for patients reported experiencing physical and psychological reactions.Citation23,Citation25,Citation27,Citation29,Citation33,Citation34,Citation35,Citation37,Citation38,Citation40 The HCPs experienced anxiety, depression, insomnia, and psychological distress.
Theme 5: Lack of Support
Several studies found that health-care workers faced difficulties when caring for COVID-19 patients. The HCPs experienced a lack of support from the health-care team, organization, family, and community.Citation23,Citation24,Citation40 The shortage of PPE, lack of guidance, and psychological support from hospital authorities contribute to inadequate healthcare for the patients. Additionally, support from the health team was identified by Sun et alCitation23 as a protective factor.
Discussion
This integrative review thematically analyzed and synthesized 18 scholarly articles on problems the HCPs while caring for COVID-19 patients. The problems were classified as mental health complications, working stress, lack of direction, coordination, support, and physical and psychological impact of the disease.
The mental health problems might be related to the many workplace safety difficulties. These include the initially insufficient understanding of the virus, the lack of prevention and control measures, and the high risk of exposure to patients with COVID-19. Other difficulties were the shortage of PPE, the risk of infecting families, concerns regarding family care and responsibilities, and the exposure to critical life events, including the death of the infected. This shows that frontline health-care providers experienced psychological and mental health problems when caring for COVID-19 patients.
Preliminary studies promoted the adverse impact of the epidemic on people’s mental health, such as the HCPs.Citation41 Health-care providers are three times more prone to suffering post-traumatic stress disorder (PTSD) symptoms when located in high-risk areas, quarantined, or with infected families and friends.Citation42 These conditions may impact the psychological wellness of health-care providers and require mitigation strategies to ensure their psychological wellness.
The COVID-19 pandemic has increased hospital admissions, impacting the HCPs’ workload. Consequently, health-care providers have many tasks to fulfill when caring for COVID-19 patients. This may cause a high mental workload and psychological burden of the HCPs. High mental workload, long working hours, under-staffing of HCPs, and lack of PPE may cause working stress in nurses, negatively impacting their performance, behaviors, and quality of life. In line with this, previous studies found that many new infectious diseases of global health concern such as Ebola with no effective medications triggered working stress in health-care providers. Furthermore, nurses have high workloads in conducting a comprehensive assessment, monitoring, nursing interventions, responding to clinical deterioration, and providing care and psychological support. They experience challenges communicating and collaborating with other health-care professionals and preventing potential complications.Citation43,Citation44 Resilience and self-efficacy may mitigate the negative impact of working stress and improve the psychological and mental health of the HCPs.Citation44–46 Additionally, adequate physical and psychological working conditions are needed to ensure the HCPs have optimal health.
During the COVID-19 outbreak, health-care providers worldwide have been confronted with an influx of new challenges. They must make quick and better decisions, such as diagnosing and isolating patients suspected to be infected and shutting downwards. This is because of limited resources, especially in developing countries. The pressure of carrying out activities in a timely and successful manner, by isolating and treating patients is overwhelming.
This study showed that the HCPs were more stressed when caring for uncooperative COVID-19 patients not adherent to safety instructions. The HCPs feel powerless when unable to provide good care due to limited hospital beds and resources.Citation12 Moreover, using PPE for long made the HCPs face breathing difficulties and limited their access to toilets and water, resulting in physical and mental distress and fatigue. The demand for health-care services for COVID-19 patients may increase workforce shortages, psychological distress, and working stress on health-care providers. Consequently, these factors correlate with physical, mental, and social problems impacting HCPs’ work productivity and quality.
Stress and its associated feelings among the frontlines of the HCPs are normal, but it should not impact their ability to provide good care. The HCPs should manage their mental, psychosocial, and physical health during this pandemic. Therefore, they should use positive coping strategies such as ensuring adequate rest, eating healthy food during work, and keeping in contact with family and colleagues. The pandemic implies the necessity to measure and protect the psychological well-being of health-care providers by accepting that stress, fear, or anxiety are normal. However, it is important to ensure quick and easy access to additional support services for those in need.
The hospital organization should ensure the psychosocial well-being of health-care providers during the pandemic. Organizations should provide HCPs with up-to-date information on the protection measures against the pandemic’s infection and transmission. Moreover, there is a need for efficient interventions regarding the immediate psychological impact on the HCPs and their work responsibility. This includes convenient and inexpensive e-Health strategies such as telemedicine and telenursing.Citation47–49 Additionally, the organization should provide sick leave to support self-isolation for infected health-care providers. This study showed the importance of family and friends’ support for the HCPs during the COVID-19 pandemic, especially when stigmatized by the community.
Conclusion
This study indicates that frontline health-care providers experience psychological problems when caring for COVID-19 patients. Many HCPs faced psychological distress and working stress that impacted their physical and mental health and social life. These include fatigue, occupational burnout, anxiety, depression, and other mental health problems impacting work productivity and efficiency. Therefore, it is important to assess and minimize the psychological burden on the frontline health-care providers against the COVID-19. This is needed to protect the psychosocial well-being of health-care providers, including accepting that anxiety and stress are normal during this pandemic. The psychological problems and mental health challenges warrant more attention and support from policymakers, families, and the community. Therefore, future organizational and national strategies and interventions should improve frontline HCPs’ mental health and well-being during the pandemic. This would be achieved by building self-efficacy and resilience, providing adequate social support and PPE facilities, and ensuring that HCPs work voluntarily.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation. All authors gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agreed to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
Additional information
Funding
References
- Dalglish SL. COVID-19 gives the lie to global health experts. Lancet. 2020;395:1189. doi:10.1016/S0140-6736(20)30739-X
- Wu PX, Hao EHY, Lau JY, et al. Real-time tentative assessment of the epidemiological characteristics of novel coronavirus infections in Wuhan, China, as of Jan 22 2020. Euro Surveill. 2020;25:2000044.
- Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi:10.1016/S2215-0366(20)30078-X
- Ibrahim NK. Epidemiologic surveillance for controlling Covid-19 pandemic: types, challenges and implications. J Infect Public Health. 2020;13:1630–1638. doi:10.1016/j.jiph.2020.07.019
- Bibin J, Chith EN, Mascarenhas P. The outbreak of novel coronavirus in India: psychological impact. SSRN Electron J. 2020;1–18. doi:10.2139/ssrn.3562062
- World Health Organization. State of the World’s Nursing 2020: Investing in Education, Jobs and Leadership. Geneva: World Health Organization; 2020b.
- Dong L, Bouey J. Public mental health crisis during COVID-19 pandemic, China. Emergency Infection Disease; 2020:26: Available from: https://www.ncbi.nlm.nih.gov/pubmed/32202993. Accessed July 5, 2022.
- Tsamakis K, Rizos E, Manolis AJ, et al. COVID-19 pandemic and its impact on mental health of healthcare professionals. Exp Ther Med. 2020;1–3. doi:10.3892/etm.2020.8646
- World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak [WWW document]; 2020. Available from: https://www.who.int/docs/defaultsource/coronaviruse/mental-health. Accessed April 17, 2020.
- British Columbia Ministry of Health. Supporting the psychosocial well-being of health care providers during the novel coronavirus (COVID-19) pandemic introduction [WWW document]; 2020. Available from: bccdc.ca/Health-Professionals-Site/Documents/COVID19Psychosocial-Supports-HCW.pdf. Accessed April 15, 2020.
- Cai J, Sun W, Huang J, Gamber M, Wu J, He G. Indirect virus transmission in cluster of COVID-19 cases, Wenzhou, China, 2020. Emerg Infect Dis. 2020;26:1343–1345. doi:10.3201/eid2606.200412
- Lee VJ, Chiew CJ, Khong WX. Interrupting transmission of COVID19: lessons from containment efforts in Singapore. J Travel Med. 2020;27(3):39. doi:10.1093/jtm/taaa039
- Shen C, Wang Z, Zhao F, et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma published online ahead of print. JAMA. 2020;323(16):1582–1589. doi:10.1001/jama.2020.4783
- Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: a rapid review of the evidence. Lancet. 2020;395:912–920. doi:10.1016/S01406736(20)30460-8
- World Health Organization. Critical preparedness, readiness and response action for COVID-19 [WWW document]; 2020a. Available from: https://www.who.int/publicationsdetail/critical-preparedness-readiness-and-response-actions-for-covid-19. Accessed April 17, 2020.
- Amnesty International. Global: health workers silenced, exposed, and attacked. Available from: https://www.amnesty.org/en/latest/news/2020/07/health-workersrights-covid-report/. Accessed July 5, 2022.
- Ramaci T, Barattucci M, Ledda C, Raposarda V. Social stigma during COVID-19 and its impact on HCWs outcomes. Sustainability. 2020;12:3834. doi:10.3390/su12093834
- Naushad VA, Bierens JJ, Nishan KP, et al. A systematic review of the impact of disaster on the mental health of medical responders. Prehosp Disaster Med. 2019;34:632–i643. doi:10.1017/S1049023X19004874
- Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–553. doi:10.1111/j.1365-2648.2005.03621.x
- Morgan S, Pullon S, McKinlay E. Observation of inter-professional collaborative practice in primary care teams: an integrative literature review. Int J Nurs Stud. 2015;52:1217–1230. doi:10.1016/j.ijnurstu.2015.03.008
- Pearce-Smith N. Critical appraisal skills checklist; 2012. Available from: https://casp-uk.net/. Accessed July 5, 2022.
- Pearson A, White H, Bath-Hextall F, Salmond S, Apostolo J, Kirkpatrick P. The Joanna Briggs Institute Reviewers’ Manual 2014: Methodology for JBI Mixed Methods Systematic Reviews. Adelaide: The Joanna Briggs Institute; 2014:5–34.
- Sun N, Shi S, Jiao D, et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control. 2020;48:592–598. doi:10.1016/j.ajic.2020.03.018
- Yin X, Zeng L. A study on the psychological needs of nurses caring for patients with coronavirus disease 2019 from the perspective of the existence, relatedness, and growth theory. Int J Nurs Sci. 2020;7:157–160. doi:10.1016/j.ijnss.2020.04.002
- Guo J, Liao L, Wang B, et al. Psychological effects of COVID-19 on hospital staff: a national cross-sectional survey of China Mainland. Lancet Psychiatry. 2020;7:e15–e16.
- Liu CY, Yang ZXM, Xu X, et al. The prevalence and influencing factors for anxiety in medical workers fighting COVID-19 in China: a cross sectional survey. Lancet Psychiatry. 2020. doi:10.2139/ssrn.3548781
- Lu W, Wangi H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:1–5. doi:10.1016/j.psychres.2020.112936
- Tan BYQ, Chew NWS, Lee GKH, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173(4):317–320. doi:10.7326/M20-1083
- Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;1–7. doi:10.1016/j.bbi.2020.03.028
- Simione L, Gnagnarella C. Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. PsyArXiv. 2020. doi:10.1017/CBO9781107415324.004
- Zhu Z, Xu S, Wang H, et al. COVID-19 in Wuhan: immediate psychological impact on health workers. medRxiv. 2020. doi:10.1101/2020.02.20.20025338
- Dai Y, Hu G, Xiong H, Qiu H, Yuan X. Psychological impact of the coronavirus disease 2019 (COVID-19) outbreak on healthcare workers in China. medRxiv. 2020. doi:10.1101/2020.03.03.20030874
- Huang L, Lin G, Tang L, Yu L, Zhou Z. Special attention to nurses’ protection during the COVID-19 epidemic. Critical Care. 2020;24:1–3. doi:10.1186/s13054-020-2841-7
- Zerbini G, Ebigbo A, Reicherts P, Kunz M, Messman H. Psychosocial burden of healthcare professionals in times of COVID-19 in a survey conducted at the University Hospital Augsburg. German Med Sci. 2020;18. doi:10.3205/000281
- Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw open. 2020;3:e203976. doi:10.1001/jamanetworkopen.2020.3976
- Xiaoa J, Fang M, Chena Q, Hea B. SARS, MERS and COVID-19 among healthcare workers: a narrative review. J Infect Public Health. 2020;13:843–848. doi:10.1016/j.jiph.2020.05.019
- Liang Y, Chen M, Zheng X, Liu J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J Psychosom Res. 2020;133:110102. doi:10.1016/j.jpsychores.2020.110102
- Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51:102083. doi:10.1016/j.ajp.2020.102083
- Li Z, Ge J, Yang M, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020;88:916–919. doi:10.1016/j.bbi.2020.03.007
- Razu SR, Yasmin T, Arief TB, et al. Challenges faced by healthcare professionals during the COVID-19 pandemic: a qualitative inquiry from Bangladesh. Front Public Health. 2021. doi:10.3389/fpubh.2021.647315
- United Nations. Policy brief: COVID-19 and the need for action on mental health. 2020.
- Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020. doi:10.1016/j.bbi.2020.04.028
- Moghbelli H, Ellithy K, Eslami Z. SCCM COVID-19 rapid-cycle survey 2 report. 2020.
- Nicola M, Alsafi Z, Sohrabi C, et al. The socio-economic implications of the coronavirus and COVID-19 pandemic: a review. Int J Surg. 2020;78:185–193. doi:10.1016/j.ijsu.2020.04.018
- Delgado C, Upton D, Ranse K, et al. Nurses’ resilience and the emotional labor of nursing work: an integrative review of the empirical literature. Int J Nurs Stud. 2017;70:71–88. doi:10.1016/j.ijnurstu.2017.02.008
- Badu E, Paul O’Brien A, Mitchell R, et al. Workplace stress and resilience in the Australian nursing workforce: a comprehensive integrative review. Int J Ment Health Nurs. 2020;29:5–34. doi:10.1111/inm.12662
- Goulia P, Mantas C, Dimitroula D, Mantis D, Hyphantis T. General hospital staff worries, perceived sufficiency of information, and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect Dis. 2010;10:322. doi:10.1186/1471-2334-10-322
- Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382:1679–1681. doi:10.1056/NEJMp2003539
- Huang L, Xu F, Liu H. Emotional responses and coping strategies of nurses and nursing college students during COVID-19 outbreak. medRxiv. 2020. doi:10.1101/2020.03.05.20031898
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and MetaAnalyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi:10.1371/journal.pmed1000097