Abstract
Objective
To objectively analyze the research for empirical evidence of the efficacy of the use of the Calgary Family Intervention Model (CFIM) in assisting bedside education by nurses and to identify facilitators and barriers to the use of the Model.
Methods
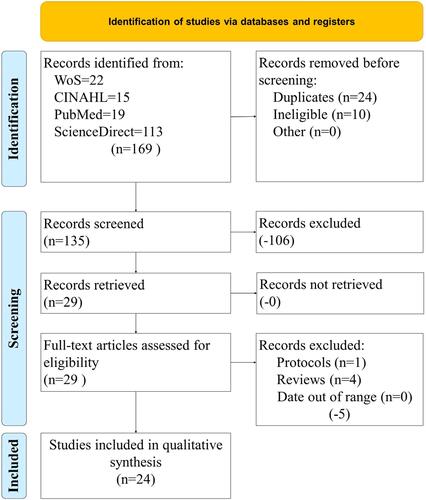
Four research databases (PubMed [MEDLINE], CINAHL, Web of Science, and Science Direct) were queried for studies commensurate with the objective statement from 1990 to 2021. In total, 169 articles were initially identified in the search, 135 were screened after duplicates and ineligible articles were removed, ultimately leaving the sample of 24 articles for the review.
Results
There is significant evidence to conclude that the CFIM is a very useful model to be used by nurses for bedside education and to improve overall patient and family outcomes. It enables communication, collaboration, and therapeutic conversations. The use of CFIM by nurses serves as a resource for both them and families and patients involved. There are some concerns to the use of CFIM as there are family dynamic issues, which result in problems providing care to patients. A lack of family sharing can result in inadequate care to the patient as well as unrealistic expectations from family members involved.
Conclusion
The CFIM is an excellent tool to enable nurses to provide education at the bedside and to enable improved patient and family outcomes. The use of the tool is suggested in situations where it would improve the level of care provided to patients and families.
Introduction
This systematic review examines the impact of utilizing the Calgary Family Intervention Model (CFIM) in bedside nurse intervention education and its impact upon patient and family compliance. Leahey and Wright’s CFIM is derived from their Calgary Family Assessment Model published in 1994, which addresses daily behaviors individuals display in relation to one another and their role within the family.Citation1 The intervention focus of CFIM creates a framework that provides a theoretical basis for collaboration in care that is highly applicable to family member empowerment and improved respectful communication of care options.Citation1 CFIM can help develop bedside nurse understanding and support of family-centered protocols, by increasing nurse buy-in to implementing and supporting the family dynamic at the bedside.Citation2,Citation3
The CFIM Framework is based on the family functioning domains of cognitive, behavioral, and affective ().Citation3 The family opens space in their domains to accept changes proposed by the healthcare worker, which occurs more readily when bedside education is presented as an opportunity to support improved patient outcomes allowing family members to reflect and include the intervention into their functional system.Citation1,Citation4 Research has shown the greatest change in family achievement occurs when the cognitive domain of thinking and feeling is addressed by an intervention.Citation1 The family must be engaged, educated, and invited to participate in order to alter their cognitive domain, which in turn creates behavioral domain change.Citation3 Choosing to accept an intervention allows the family to implement the change in their behavioral domain in a way that fits with the positive aspects of their family function.Citation5,Citation6 Thus, educating the bedside nurse through a family focus reinforces the centrality of family and promotes change in family functioning through the affective domain.Citation2
Table 1 CFIM Framework
Rationale
While CFIM has been widely accepted and used by nursing for decades, the use of CFIM as a framework for providing bedside nurse education to implement changes that include the family perspective has not been published. The family visitation restrictions due to COVID-19 demonstrated the importance of family connection, acknowledgement, and participation in care decisions.Citation7 Using the CFIM domains as the focus of implementing family centric protocols supports nurse influence on personalizing care to the family and demonstrates the effectiveness of nurse effort to include families in patient care.Citation6 CFIM has been used in previous implementation studies with a good effect on maintaining family roles and connections central to interventions.Citation4,Citation8,Citation9 Providing education to nurses in a way that incorporates family function as central to interventions, supports medicine’s shift toward family inclusion and the view that patients and families are not visitors in the room, but rather medical providers are stepping into their room.Citation2,Citation7
Objective
The purpose of this research was to evaluate the CFIM as an effective tool for use by nurses in the aid of bedside education of patients and families.
Materials and Methods
Eligibility Criteria
To be eligible for this study, articles had to be published between January 1990 and December 2021 in only peer-reviewed, academic journals published in English. All study designs were accepted including both quantitative and qualitative. Other systematic reviews and meta-analyses were excluded from the study, as well as dissertations.
Information Sources
Authors of this systematic review followed the Kruse Protocol for conducting a systematic review and reported results in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA).Citation10 This research was not registered.
Search Strategy
Four databases were queried with a standard search string for this study: PubMed (MEDLINE), Web of Science, and Science Direct. CINAHL was also queried, but no results were found which were not duplicated in the other three databases. PubMed yielded 19 articles, Science Direct yielded 11 articles, Web of Science yielded 3 articles, thus yielding the sample of 24 utilized in the final sample. We created a three-string Boolean search specifically designed to present more articles for review than utilizing only Medical Subject Headings (MeSH) of the US Library of Medicine. The search strategy was used across all databases. We used similar filtering strategies in each database, because not all databases offer the same filtering tools. The string utilized was (“Calgary Family Intervention Model” OR “CFIM”) AND (family OR families OR community OR communities) AND (educate OR education OR nurse OR develop OR train).
Selection Process
In accordance with the Kruse Protocol,Citation10 we searched key terms in all databases, filtered results, and screened abstracts for applicability. Reviewers rejected articles if they were not research or did not produce results, such as study protocols, opinions, or commentaries. Studies were also eliminated, which did not speak specifically to the use of the Calgary Family Intervention Model in some form or fashion. Overall, the literature search, data extraction, and risk of bias assessments were completed by at least two reviewers, blinded to each other’s choices.
Data Collection Process
We utilized an Excel spreadsheet as a data extraction tool collecting additional data at each step of the process. This spreadsheet was standardized in the Kruse Protocol.Citation10 A series of three consensus meetings were held. The first consensus meeting was held after abstract screening. Second and third meetings were held to identify observations and themes.
Data Items
In accordance with the Kruse Protocol, we collected the following fields of data at each step in the process: participants, intervention, results compared to the control group, health outcomes, study design (PICOS), bias, effect size, country of origin, statistics used, strength of evidence, and quality of evidence. We further collected facilitators and barriers from each article. These data items and observations became the subject of the second and third consensus meetings.
Study Risk of Bias Assessment
We observed bias and assessed the quality of each study using the Johns Hopkins Nursing tool for Evidence Based Practice (JHNEBP).Citation11 We considered the instances of bias in how to interpret the results as bias can limit external validity.
Effect Measures
As we accepted mixed methods and qualitative studies, we were unable to standardize summary measures, as would be performed in a meta-analysis. Effect size was not reported in any study of the group for analysis.
Synthesis Methods
During the screening process, reviewers compared elements of article abstracts against the objective statement for this review. Article abstracts which matched with the objective statement were marked for inclusion in the systematic review. The rest of this subheading is for meta-analyses—not for systematic reviews. Although the Kruse Protocol for conducting a systematic review uses elements of a meta-analysis, it falls short of this standard.
Additional Analyses
We performed a narrative analysis of the observations to convert them into themes (common threads between articles).Citation12 We calculated frequency of occurrence and reported these via affinity matrices. This technique does not imply a level of importance of these observations, but it simply illustrates the probability of occurrence of these observations across the group for analysis.
Results
Study Selection
illustrates our study selection process from the four databases. A kappa statistic was calculated on levels of agreement between reviewers (k = 1, high agreement).Citation13,Citation14
Study Characteristics
In accordance with PRISMA 2020, a PICOS table was created from the group of articles analyzed (see ). Of the 24 articles analyzed for the manuscript, all studies spoke specifically to the CFIM in some aspect. Results across studies varied widely.
Table 2 PICOS (Participants, Intervention, Results, Outcome, and Study Design) Characteristics of the Included Studies
Risk of Bias in Studies
The JHNEBP quality assessment tool identified the strength and quality of evidence in the literature. These are illustrated in . Approximately 75% of the articles were of strength III and 88% were quality B. This means a vast majority of articles were qualitative, mixed methods, non-experimental or quasi-experimental in nature, but their quality was still strong. Panel A illustrates strength of evidence. Level II studies were quasi experimental in nature (no randomization). Level III studies were non-experimental studies or qualitative studies. As the information was very germane, we did accept one level V study, which was based in a quality improvement study. Panel B illustrates quality of evidence. Quality category B, research shows reasonably consistent results, sufficient sample sizes, some control, and fairly definitive conclusions. Quality category C shows lower quality studies based on relatively inconsistent results; however, they were included due to the small sample size and perceived importance to the study.
Table 3 Summary of Strength and Quality of Evidence Identified with the JHNEBP
Reviewers independently recorded observations for each article commensurate with the objective statement. A thematic analysis was conducted to make sense of the data. When an observation was identified more than once, it became a theme. Themes were created to summarize the observations, but they did not always match the observations exactly. These themes can be observed in , the summary of the analysis. Articles are sorted most recent to oldest.
Table 4 Summary of Analysis, in Order of Use in Paper
Reviewers conducted a thematic or narrative analysis. Part of the analysis is making sense of the data. When an observation reoccurs, it becomes a theme. Observations without reoccurrence are just observations.
Discussion
Study results were broken into two thematic categories—facilitators and barriers—for the ease of discussion. There were nine facilitator themes encompassing 113 individual observations in the literature. The affinity matrix for facilitator themes is shown in .
Table 5 Study Results Affinity Matrix for Facilitators
Improved patient/family outcomes was recognized in 21/113 (18.58%) of facilitators. Patient outcomes were improved with support during critical illness phases of patient care.Citation15–Citation17 Support interventions which were provided by nurses were found to be helpful and useful by family members. This included support during end of life, emotional concerns, and psychiatric concerns of the patient.Citation16,Citation18,Citation19 Improved patient outcomes were shown when nurses shared their collective experiences with patients and families. Nurses were able to offer pertinent information, thoughts, and opinions, which assisted with outcomes.Citation15,Citation20,Citation21 Nursing interventions were found to be empowering to families to provide care for the patient.Citation20,Citation21 Positive outcomes were noted by nurses when the family was involved with decision-making. This allowed for a marked increase in the ability to make decisions for the family and in more positive experiences surrounding the provision of care for families.Citation17,Citation22 Improved outcomes were seen in patients who normally underutilize healthcare resources.Citation23 When families were empowered, improved relationships were seen between them and their healthcare providers, along with increased levels of trust and ability to make decisions.Citation20 With the increased knowledge regarding patient conditions came an increased ability of both family and patient to better manage symptoms.Citation20 When families had conversations with nursing staff, this resulted in an increased capacity for healing of the patient and of family concerns.Citation24,Citation25 Families were able to find relief and were enabled to have positive affective, behavioral, and cognitive changes as a result of nursing interventions.Citation22
Education increasing awareness of nurses was recognized in 14/113 (12.39%) of facilitators. Education was seen as an effective tool in increasing the confidence of nursing in working with families and patients in the areas of knowledge, skill, comfort, family systems, assessment, and interactions.Citation9,Citation15,Citation26–Citation28 Education was also found to be a tool to utilize to assist to clarify expectations in relationships between nurses and patients/families. Circular questioning was identified as an effective tool in this area. Nurses were also better enabled in assisting or managing a chronic exacerbation in patients if they were adequately educated on the concern and the techniques.Citation17,Citation26 Education of nurses was seen as a measure to increase awareness of the importance of families and their contributions. It also increased awareness of the benefits of collaborative efforts between nurses and families.Citation29 Nurses who received instruction on the development of family nursing skills became more aware of their own communications and thus more aware of their interactions with families.Citation29 Education of the value of CFIM increased awareness of agency nurses and encouraged them to work with their agencies to allocate time for family meetings and discussions as part of their daily work.Citation28 Education caused improvements to be seen in job satisfaction and improved morale of nurses.Citation28 Increase autonomy was also exhibited with more education for nurses in controlling their work assignments.Citation23
Families as a unit of care or collaboration was recognized in 14/113 (12.39%) of facilitators. Education assisted nurses in understanding that caring for patients is a collaborative effort.Citation29–Citation31 Increased knowledge of disease process for nurses helped to improve attitudes of collaboration with families and provided improved perspective of the patient/family situation.Citation21,Citation29,Citation32 Stronger nurse–family relationships afforded better coordination of care plans and increased understanding of the patient.Citation9,Citation33 Education led to furthered viewpoint of nurses regarding the family as a unit of care.Citation29 Patient care can be enhanced by nurse–family relationships, especially with families who are involved. This led to improved outcomes and improved patient care plans.Citation9 Outcomes after discharge were improved by nurse–family relationships in the hospital, which led to an increase in understanding for the families to assist in care post discharge.Citation9 The use of different models (such as the Illness Beliefs Model) helped to improve relationships and increase the feelings of support and collaboration between nurses and families.Citation32 Nurses found that the more families were involved in care, the better the understanding of the patient situation they had, which allowed for more comprehensive assessments and treatment plans.Citation28 Nurses who explored beliefs and family strengths had better overall patient outcomes.Citation28
Education for nurses/families was recognized in 13/113 (11.5%) of facilitators. When provided specific education, it was shown to lead to improved overall outcomes for nurses, families, and patients.Citation26,Citation29,Citation34 Increased levels of education adds important practical knowledge to the understanding of nursing roles and boundaries.Citation26,Citation29 Education leads to increased nursing confidence and competence in assessment skills and increased understanding of family needs and priorities.Citation24,Citation27 Increased education can lead to increased understanding of nurses regarding family illness experiences.Citation15 When simultaneously educating nurses and families on patient condition and prevention of symptoms, an increased partnership can be built to provide the patient care.Citation32 Education to nurses surrounding bedside manner allowed for an increase in family trust of the care being provided.Citation24 Education overall led nurses to feel more comfortable in taking leadership positions to help promulgate information to other nurses on how to improve care.Citation29
Therapeutic conversations with families was recognized in 13/113 (11.5%) of facilitators. Therapeutic conversations were found to be assistive in furthering discussions in learning problem solving communication, managing patient conditions, increased trust of providers with families, and in facilitating decision-making for families.Citation16,Citation21,Citation25,Citation30 Supportive conversations created opportunities for families to recognize their own strengths, needs, and experiences.Citation25,Citation30,Citation35 Therapeutic conversations were quite effective in allowing nurses to help families in validating their own emotions and concerns regarding the patient and their condition.Citation21,Citation24 The use of writing communications allowing patients to journal their experiences allowed for increased understanding of conditions and compliance with care.Citation18 Appropriate conversations between nurses and families allowed for greater compliance with treatment plans and greater compliance overall with “non-compliant” patients.Citation23 Quality family communications were important factors in ongoing family mental health.Citation22
Clear two-way communications necessary was recognized in 12/113 (10.62%) of facilitators. Reciprocal, clear, and honest communication between nurses and family is vital for caregiving and prevention. This is also noted to increase trust of nursing providers.Citation16,Citation21,Citation31,Citation32,Citation35 Clearer nursing communications led to easier understanding by patient and family regarding interventions being performed.Citation18,Citation19 Nursing interventions are shown to further provide family and patient with emotional support and engagement.Citation21,Citation31 Frequent interaction and reciprocity were noted in nurse/family relationships. This had positive connotations for nurses in perceptions towards families.Citation9 Nurses are enabled to promote family/patient relationships by assisting family to get to know patients and conditions better.Citation9 Patients expressed positive perceptions of nurses after more appropriate interactions were experienced between them.Citation23
Use of reflection and other tools was recognized in 9/113 (7.96%) of facilitators. Reflection tools are easy to use, time saving, and are beneficial in the nurse/patient relationship. They also can be used to build relationships, increase communications, and improve patient outcomes.Citation17,Citation22,Citation24 Nurses can use reflection and therapeutic questioning as a technique to better connect with families. This can increase nurse understanding of relationships, intercommunications, and personality.Citation24,Citation26,Citation33 The use of specific tools such as genograms and ecomaps can assist nurses with interactions around patient care.Citation24,Citation26 Measurement tools can provide insights to family perceptions surrounding nursing interactions to include cognitive and emotional functions.Citation16
Education changing perceptions of nurses towards CFIM was recognized in 9/113 (7.96%) of facilitators. Education regarding CFIM allowed nurses to have positive perceptions on importance of nursing/family interactions.Citation26,Citation36,Citation37 Increased education and training increased positive perceptions of support by nurses from administration and coworkers.Citation19,Citation25 Better understanding of why to use tools allowed for discovery by nurses to the beneficial nature of their usage.Citation27,Citation29 Use of tools and education surrounding them allowed for personal growth of nurses as this increased skills, abilities, and attitudes towards working with families and reflecting upon experiences.Citation24 Education led to increased support from families and can lead to treatment changes.Citation25
Resources to families was recognized in 8/113 (7.08%) of facilitators. Commendation of family strengths is a powerful tool and resource to provide for change in context for problem solving to allow family to take an active part in care.Citation21,Citation24 Resources such as websites provide to families allowed for more positive interactions and increased understanding of nursing interventions.Citation30,Citation36 Providing positive commendation to families allowed for positive emotions in nurses, which allowed for more rewarding experiences for nurses.Citation30 The sharing of information by nurses to family and patient led to increased perceptions of nurses regarding improving care and support of patients. An effective method for this was performed at discharge by sharing information on illness and lifestyle adjustments, which need to be implemented.Citation17 Circular questioning as a tool allowed for increased family understanding of beliefs, relationships, and interventions.Citation21
Barriers
The remainder of study results were barriers. There were eleven barrier themes encompassing 74 individual observations in the literature. The affinity matrix for barrier themes is shown in
Table 6 Study Results Affinity Matrix for Barriers
Nursing staff burden increased/stress concerns was recognized in 18/74 (24.32%) of barriers. Persistent perceptions exist that adding further work to the nursing staff is untenable and creates further issues with time constraint. Concerns were noted in time constraints regarding ability to perform the job, lack of ability to speak with families/patients, and nurses already having too much documentation to complete already.Citation21,Citation24,Citation25,Citation28,Citation29 Perceptions regarding a severely increased staff burden of already overburdened workers exist. More documentation can be overwhelming to the staff that already perceives that they have too much documentation to complete and provide adequate care.Citation25,Citation29,Citation32,Citation36 Poor perceptions surrounding the intervention by nursing as it will increase the workload. Nursing staff have doubts on the effectiveness and utility of the model and that implementing it could be intrusive to care provision.Citation9,Citation21,Citation25,Citation29 Organizational barriers exist such as increased pressure on nursing staff to perform, as well as budgetary constraints.Citation9,Citation26 Nursing views the model to be troubling and intrusive to family members.Citation28 The ability of use for the model could be dependent upon the type of environment, such as general patient wards, where they are already less supportive of family nursing due to high turnover and acuity levels.Citation29
Family dynamics concerns was recognized in 14/74 (18.92%) of barriers. Lack of family cooperation and lack of ability to make patient care decisions by the family are concerning.Citation21,Citation27 Among groups of family members, the dynamics and perceptions of what the patient required for adequate care were differing, causing confusion and delay in the process of providing care.Citation21,Citation22 Family members often were biased against nurses until they perceived sufficient levels of care coming from the individual nursing staff.Citation28,Citation31 Many nurses had a lack of experience or training in dealing with challenging family dynamics.Citation18,Citation32 Certain groups exhibited diminished functioning within their family units, which created significant issues with the nurse–family relationship.Citation9,Citation27 Families often exhibited passive natures towards care or nurses, which created issues with the provision of care.Citation9 Financial disparities of families often led to issues surrounding the provision of care.Citation23 Many families did not want to engage nurses as they believed that they would be seen as demanding or that their actions would have negative effects on the care being given.Citation31
Inadequate education was recognized in 13/74 (17.57%) of barriers. Nurses often lacked in the areas of education, skills, or abilities in the ability to adequately utilize tools provided to them to provide care.Citation26,Citation33,Citation34,Citation36,Citation37 Nurses also report a lack of confidence in communications, skills, knowledge, or attitudes in their interactions with families.Citation15,Citation34,Citation37 Many nurses reported not being confident in how to involve families in care planning or chosen interventions for care provision.Citation22,Citation28 Reports from nurses (after they have been provided education) that tools or processes are still unknown to them, leading to the conclusion that more education overall is necessary for successful implementation of CFIM.Citation27,Citation37 Nurses report that they do not understand how to cope with family suffering or other concerns.Citation24
Problems surrounding family sharing of patient information was recognized in 7/74 (9.46%) of barriers. It was problematic for family to share information about the patient due to traditional familial or gender roles, religious beliefs, or fear of judgement from others.Citation24,Citation25,Citation30 A perceived lack of collaboration and failure to share information caused issues between the nurse and family members.Citation21 Differing beliefs between family members caused difficulty in application of CFIM interventions.Citation27 Family members were often reluctant to disclose problems regarding the patient or themselves.Citation28
Increased time required to develop nursing skills was recognized in 6/74 (8.11%) of barriers. Nurses believe the knowledge of these interventions is important but thought that more time was necessary to develop the required skills to adequately work with the tools. The lack of experience in this area is concerning.Citation26,Citation29,Citation33,Citation36 The culture of the organization became disempowering towards attitudes and beliefs requiring time to resolve.Citation21 Nurses have personal perceptions to overcome over time due to their own family experiences or unwillingness to confront their own family concerns.Citation34
Lack of nursing or family commitment was recognized in 4/74 (5.41%) of barriers. Family felt not included as partners in patient care.Citation16,Citation24 Family also became frustrated with the perceived lack of communication about patient condition and treatment plans.Citation24 Families were often unable to commit to daily visits to patient causing a lack of family participation with the CFIM.Citation32
Communications concerns were recognized in 4/74 (5.41%) of barriers. Nurses were noted to not be communicating tools effectively to patients and families.Citation17 Families became overwhelmed at the amount of information they had to learn and comprehend.Citation21 Nurses became afraid of negative responses from family or making the patient angry.Citation28 Nurses expressed doubts regarding the effectiveness and utility of family intervention tool.Citation37
Unrealistic expectations from family was recognized in 3/74 (4.05%) of barriers. Nurses were noted to have trouble working with families who reported their relationships as troubling, thus leading to magnified perceptions by nurses regarding their own suffering or concerns.Citation15 Lack of knowledge, unrealistic expectations, and cultural/language barriers made it more difficult for families to understand the plan of care as explained by nurses.Citation9 High psychological and emotional demand of many families caused concerns for many nurses in meeting expectations of families.Citation16
Patients with preexisting health concerns lack motivation was recognized in 2/74 (2.70%) of barriers. When families were re-notified of patient conditions, it affected family functioning and created barriers to care.Citation17 Patients with existing health concerns lack motivation to follow treatment plans set forth in many cases, as well as they have a denial of care and assistance attitude.Citation23 Lack of administrative support was recognized in 2/74 (2.70%) of barriers. Nurses noted a lack of recognition and support for family nursing in healthcare by administration.Citation34 Certain programs became fragmented by the institution and the understanding of the programs became uncertain.Citation37 Self-assessment of nursing skills can be inadequately reported was recognized in 1/74 (1.35%) of barriers. Nurses who self-assessed their skills and competency using CFIM tools were noted to potentially have inaccurate self-reporting.Citation26
Further Considerations
The use of CFIM and nursing led educational interventions with the family can provide for excellent benefits to both the patient and the family. There were specific benefits regarding outcomes for the patient and family that might not have been realized without the use of these methods. This was particularly important during critical phases of the patients’ hospitalization. Overall, benefits were seen at end of life, during emotional times for patient or family, and during psychiatric interventions. Noted in the research was the benefits that the nurses interventions had in the ability for decision-making for the patient and in the overall patient experience. Families were often found to be empowered further and a part of the care team when nurses provided these interventions during a hospital stay. In fact, clearly the use of CFIM enables not only a more positive stay for the patient but also a more positive experience for the family, despite the status of the patient at discharge. These methods were able to bring together the patient, the family, and the nursing staff to allow for a much more beneficial experience for all involved.
The use of CFIM and nursing led educational interventions does not come without its fair share of concerns. Nursing staff can feel overburdened by the use of these methods and this can be perceived as additional work for them. Thus, this intervention could lead to increased workplace stress. Certain things which nurses cannot plan for or control cause issues continually, such as problems with family dynamics, family sharing, and family involvement and commitment (or lack thereof). Unrealistic family expectations are always a concern and were still a concern in many cases, even with these improved methodologies to assist the patient and family. Some nurses also still felt unequipped to use these methods, even after significant education was provided to them. Lastly, the perception of a lack of administrative support is concerning.
Limitations
Limitations to this manuscript stem from the small number of studies upon which to base conclusions. The CFIM and how it relates to patient and family compliance is not a well-studied area in the literature. The quality and strength of the articles may have had some implications in the quality of the findings of this article.
Conclusion
From an overarching perspective, it seems that the use of CFIM and nursing led educational interventions is beneficial for the nurses involved and it provides for a much better ability to achieve a healthy work environment.
Abbreviation
CFIM, Calgary Family Intervention Model.
Ethics Disclosure
This work was exempted from normal IRB processes, as it is a systematic review. The research was conducted in accordance with the Declaration of Helsinki.
Disclosure
The authors report no conflicts of interest in this work.
References
- Leahey M, Wright LM. Application of the Calgary family assessment and intervention models: reflections on the reciprocity between the personal and the professional. J Fam Nurs. 2016;22(4):450–459. doi:10.1177/1074840716667972
- McClay R. Implementation of the family HELP protocol: a feasibility project for a West Texas ICU. Health Care. 2021;9(2):146. doi:10.3390/healthcare9020146
- Wright LM, Leahey M. Calgary family intervention model: one way to think about change. J Marital Fam Ther. 1994;20(4):381–395. doi:10.1111/j.1752-0606.1994.tb00128.x
- Lee HW, Park Y, Jang EJ, Lee YJ. Intensive care unit length of stay is reduced by protocolized family support intervention: a systematic review and meta-analysis. Intensive Care Med. 2019;45(8):1072–1081. doi:10.1007/s00134-019-05681-3
- Hshieh TT, Yang T, Gartaganis SL, Yue J, Inouye SK. Hospital elder life program: systematic review and meta-analysis of effectiveness. Am J Geriatric Psychiatry. 2018;26(10):1015–1033. doi:10.1016/j.jagp.2018.06.007
- Rosenbloom-Brunton DA, Henneman EA, Inouye SK. Feasibility of family participation in a delirium prevention program for hospitalized older adults. J Gerontol Nurs. 2010;36(9):22–33. doi:10.3928/00989134-20100330-02
- Setliff EL, Schulman A. Innovative strategies for family engagement. Crit Connect. 2021;20(4):32–33.
- Heim N, van Stel HF, Ettema RG, Schurmans M, van der Mast RC, Inoye SK. HELP! Problems in executing a pragmatic, randomized, stepped wedge trial on the hospital elder life program to prevent delirium in older patients. Trials. 2017;18(1):1–12. doi:10.1186/s13063-017-1933-4
- Misto K. Family perceptions of family nursing in a magnet institution during acute hospitalizations of older adult patients. Clin Nurs Res. 2019;28(5):548–566. doi:10.1177/1054773817748400
- Kruse CS. Writing a systematic review for publication in a health-related degree program. JMIR Res Protoc. 2019;8:e15490. doi:10.2196/15490
- Newhouse R, Dearholt S, Poe S, Pugh L, White K. The Johns Hopkins Nursing Evidence-Based Practice Rating Scale. Baltimore, MD: The Johns Hopkins Hospital; 2005.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi:10.1191/1478088706qp063oa
- Light RJ. Measures of response agreement for qualitative data: some generalizations and alternatives. Psychol Bull. 1971;76:365. doi:10.1037/h0031643
- McHugh ML. Interrater reliability: the kappa statistic. Biochemia Medica. 2012;22:276–282. doi:10.11613/BM.2012.031
- Eggenberger SK, Sanders M. A family nursing educational intervention supports nurses and families in an adult intensive care unit. Australian Crit Care. 2016;29(4):217–223. doi:10.1016/j.aucc.2016.09.002
- Sveinbjarnardottir EK, Svavarsdottir EK, Wright LM. What are the benefits of a short therapeutic conversation intervention with acute psychiatric patients and their families? A controlled before and after study. Int J Nurs Stud. 2013;50(5):593–602. doi:10.1016/j.ijnurstu.2012.10.009
- Misto K. Nurse perceptions of family nursing during acute hospitalizations of older adult patients. Appl Nurs Res. 2018;41:80–85. doi:10.1016/j.apnr.2018.04.009
- Gísladóttir M, Svavarsdóttir EK. Educational and support intervention to help families assist in the recovery of relatives with eating disorders. J Psychiatr Ment Health Nurs. 2010;se18(2):122–130. doi:10.1111/j.1365-2850.2010.01637.x
- Ménard D, Saucier A. John’s story: an application of the Calgary family intervention model. Can Oncol Nurs J. 2000;10(2):64–68. doi:10.5737/1181912x1026468
- Arief YS, Rachmawati PD. Parent empowerment program in caring for children with leukemia. Enferm Clin. 2019;29(Supplement 2):897–899. doi:10.1016/j.enfcli.2019.04.136
- Rempel GR. Technological advances in pediatrics: challenges for parents and nurses. J Pediatr Nurs. 2004;19(1):13–24. doi:10.1016/j.pedn.2003.09.003
- Clausson E, Berg A. Family intervention sessions: one useful way to improve schoolchildren's mental health. J Fam Nurs. 2008;14(3):289–313. doi:10.1177/1074840708322758
- Brumfield R. A family systems approach to case management in a rural community setting. Home Care Provid. 1997;2(4):180–183. doi:10.1016/S1084-628X(97)90068-X
- Holtslander L, Solar J, Smith NR. The 15-minute family interview as a learning strategy for senior undergraduate nursing students. J Fam Nurs. 2013;19(2):230–248. doi:10.1177/1074840712472554
- Sigurdardottir AO, Svavarsdottir EK, Rayens MK, Adkins S. Therapeutic conversations intervention in pediatrics: are they of benefit for families of children with asthma? Nurs Clin North Am. 2013;48(2):287–304. doi:10.1016/j.cnur.2013.01.007
- Broekema S, Luttik MLA, Steggerda GE, Paans W, Roodbol PF. Measuring change in nurses’ perceptions about family nursing competency following a 6-day educational intervention. J Fam Nurs. 2018;24(4):508–537. doi:10.1177/1074840718812145
- Martinez A-M, D’Artois D, Rennick JE. Does the 15-minute (or less) family interview influence family nursing practice? J Fam Nurs. 2007;13(2):157–178. doi:10.1177/1074840707300750
- Simpson P, Yeung K, Yat K, Wah WK. Family systems nursing: a guide to mental health care in Hong Kong. J Fam Nurs. 2006;12(3):276–291. doi:10.1177/1074840706291436
- John WS, Flowers K. Working with families: from theory to clinical nursing practice. Collegian. 2009;16(3):131–138. doi:10.1016/j.colegn.2009.04.001
- Choi H, Van Riper M. mHealth family adaptation intervention for families of young children with down syndrome: a feasibility study. J Pediatr Nurs. 2020;50:e69–e76. doi:10.1016/j.pedn.2019.03.010
- Dorell Å, Sundin K. Becoming visible - experiences from families participating in family health conversations at residential homes for older people. Geriatric Nurs. 2016;37(4):260–265. doi:10.1016/j.gerinurse.2016.02.015
- Rosenbloom DA, Fick DM. Nurse/family caregiver intervention for delirium increases delirium knowledge and improves attitudes toward partnership. Geriatric Nurs. 2014;35(3):175–181. doi:10.1016/j.gerinurse.2013.12.004
- Binding LL, Morck AC, Moules NJ. Learning to see the other: a vehicle of reflection. Nurse Educ Today. 2010;30(6):591–594. doi:10.1016/j.nedt.2009.12.014
- Lee ACK, Leung SSK, Mak YW. The application of family-nursing assessment skills: from classroom to hospital ward among final-year nursing undergraduates in Hong Kong. Nurse Educ Today. 2012;32(1):78–84. doi:10.1016/j.nedt.2011.01.013
- Sveinbjarnardottir EK, Svavarsdottir EK, Hrafnkelsson B. Psychometric development of the Iceland-Family Perceived Support Questionnaire (ICE-FPSQ). J Fam Nurs. 2012;18(3):328–352. doi:10.1177/1074840712449203
- Silva M, Moules N, Silva L, Bousso R. The 15-minute family interview: a family health strategy tool. Revista da Escola de Enfermagem da USP. 2013;47(3):634–639. doi:10.1590/S0080-623420130000300016
- de Jesus Silva Figueiredo MH, da Silva Martins MMFP. From practice contexts towards the (co)construction of family nursing care models. Revista da Escola de Enfermagem. 2009;43(3):612–618. doi:10.1590/S0080-62342009000300017