Abstract
Background
The rate of cesarean section is increasing from 15% to 40% in recent years. The type of delivery influences the hormonal, emotional and mental health of the mother, which correlates positively or negatively with the health benefits of the newborn. There have been many published studies on kangaroo mother care for mothers undergoing elective cesarean section, but there is still a lack of understanding about emergency cesarean section.
Objective
This study aimed to evaluate the benefits of KMC practice for mothers undergoing emergency cesarean section in terms of hormone levels such as oxytocin, cortisol, prolactin, interleukin-6 and interleukin-10.
Methods
This retrospective analysis used remnant serum (KMC group = 16; control group = 9), and clinical data such as KMC practice (15–30 minutes three or four times daily until discharge), breastfeeding initiation time, feeding time, crying time and hospital stay were extracted from the electronic database. All hormone and cytokine expressions were quantitatively determined by ELISA. Comparisons within and between groups were performed using appropriate statistical tests.
Results
In the KMC group, increased levels of the hormone oxytocin significantly reduced cortisol and IL-6 and negatively influenced prolactin and IL-10 levels. The elevated prolactin facilitates overall lactation behaviour, of which 64% reported breastfeeding directly at the breast. The cytokine analysis revealed a reduction in pro-inflammatory cytokines and thereby an improved wound healing was seen in the KMC group.
Conclusion
These quantitative results strongly encourage the use of KMC for mothers undergoing emergency cesarean section. These simple yet effective breastfeeding strategies promote maternal and infant health, which can reduce medication use.
Introduction
Cesarean Rate Worldwide and in Saudi Arabia
The process of caesarean delivery, also referred to as a C-section or caesarean section, involves the surgical procedure of an open incision made in the mother’s abdomen or uterus. The World Health Organization (WHO) reported that the global acceptable rate of caesarean section stands at 10–15% of all births.Citation1 However, the C-section has surpassed the 15% benchmark in many developed and developing countries, climbing up to 40%.Citation2–4 This trend is particularly evident in countries such as Saudi Arabia, where the rate of cesarean deliveries peaked at 26.3% in Jeddah in 2016.Citation5 Recent evidence from King Abdulaziz Medical City in Riyadh reveals that elective cesarean deliveries account for at least 13.7% of caesarean deliveries.Citation6 Qassim City reported an alarming 55.4% caesarean section rate out of a total of 936 births in 2018.Citation7
Stress after Cesarean
The rise in cortisol levels due to post-traumatic stress is a common occurrence in C-sections.Citation8 The stress related signalling pathways are controlled by the hypothalamic–pituitary–adrenal (HPA) axis that starts from the paraventricular nucleus (PVN). Corticotrophin releasing hormone (CRH) triggers the anterior pituitary to upregulate the adrenocorticotrophin (ACTH).Citation9 The resulting cortisol release causes a reduction in prolactin output.Citation10 Furthermore, stress can indirectly reduce prolactin levels by stimulating the sympathetic nervous system. This deficiency in prolactin may lead to lactational difficulties in mothers who have undergone C-sections. Besides, hormonal fluctuations following a cesarean section typically occur between the third and fifth day and may even last for six to eight weeks postpartum.Citation11 Anticipate experiencing undulations in oestrogen and progesterone, which may manifest as melancholy, overwhelm, apprehension, and despondency.
KMC: An Introduction
The WHO defined kangaroo mother care (KMC) or skin-to-skin contact (SSC) as “care for a premature baby born skin-to-skin with the mother”. It is a potent, simple yet effective technique to improve the overall health of full-term and preterm infants. KMC between mother and neonate pair should be initiated at early hours after postpartum; however, the duration and method differs with clinical settings. Continuous KMC is the term used for KMC that is administered throughout a 24-hour period in the original approach in low-income settings. The low birth weight infants and/or preterm infants in NICU settings are advised for the intermittent KMC approach; however, in wealthy settings, this strategy is used with brief exposures of one to three hours.
KMC Benefits
KMC has been reported to decrease the incidence of neonatal mortality from 53% to 36% by the following ways.Citation12 The practice of SSC has greatly improved the health and mental status of mother and infant. Research suggests that SSC can improve blood oxygenation, maintain the blood glucose level, encourage longer duration of breastfeeding, reduce apnoea during sleep, reduce stress of birth, decrease the risk of jaundice, strengthen the immune system and aid in pain management for infants.Citation12,Citation13 KMC also benefits mothers who have undergone C-section as it helps to strengthen the mother–baby bond and helps them to cope with anxiety and postpartum depression. The growing evidence augmented that the surge of oxytocin, a neuropeptide hormone during or after KMC, plays a paramount role in the aforementioned health benefits.
SSC provides immediate and long-term benefits that include improved recognition and attachment between mother and newborn infant,Citation14 faster expulsion of the placenta, lowered primary postpartum haemorrhage condition,Citation15 improved maternal self-efficacy toward breastfeeding,Citation16 facilitation of breastfeeding initiation,Citation16 increased exclusive breastfeeding duration,Citation16,Citation17 frequency of breastfeeding per day increases,Citation18 and reduced maternal post-traumatic stress and depression.Citation19,Citation20, From the infant point of view, SSC stabilizes thermoregulationCitation18 and cardiopulmonary dynamics, helps to maintain the blood glucose levelCitation14 and reduces pain during intramuscular injections. KMC have found to reduce infant’s stress and crying duration and frequency during the early period post birth.
KMC and Hormone Study
During KMC, skin-to-skin contact causes the release of oxytocin, which can alleviate the mother’s discomfort. When oxytocin released in the brain enters the amygdala during KMC, it functions to deactivate the stress mechanisms via decreased secretion of cortisol, and other metabolites that are harmful to the mother and the baby. Moreover, apart from encouraging maternal conduct like bonding, oxytocin also possesses tranquilizing, anxiolytic and analgesic properties. Furthermore, oxytocin also encompasses qualities that are similar to those of antidepressants. A positive consequence of the hormone oxytocin is that it can aid in reducing the mother’s circulation of catecholamines, which subsequently diminishes maternal stress.Citation21
The aforementioned hormonal axis facilitates parent–infant interactions by means of a bio-socio-behavioural feedback loop that involves the hormone oxytocin. Subsequently, the release of oxytocin promotes increased maternal–infant proximity. Previous studies have correlated the peripheral oxytocin levels during KMC practice with maternal behaviours. Besides, engaging in KMC enhances the production of maternal prolactin. Such oxytocin release may help enhance maternal responses to the baby and bonding, while simultaneously reducing maternal stress levels.
KMC could be considered as an alternative for post-operative analgesia since both interventions have resulted in similar outcome. The recovery rate of surgical wound made during C-section is another contributing factor for mother’s stress response. The pro-inflammatory cytokines such as IL-6 is a well-known biomarker for surgical tissue damage and nowadays can be used in the prognosis of severity of operative wound. Therefore, inhibition of these kinds of cytokines is beneficial to post-operative recovery.Citation22,Citation23
IL-10, an anti-inflammatory cytokine, activates and promotes infiltration of immune cells and non-immune cells at the wound site.Citation24 Studies have highlighted that the overexpression of IL-10 markedly reduces the plasma IL-6 level during skin damage. Both these actions promote faster post-surgical wound healing, including cesarean delivery.Citation25,Citation26 Despite copious studies focused on the effects of KMC on maternal and neonatal health, few studies determine the involvement of hormones and its effects on stress management in the early postpartum period after cesarean section.
Aim/Objective
Even though the WHO recommends KMC for at least 80% of all births,Citation1 the prevalence of KMC varies greatly across different parts of the world.Citation2 The role of KMC in vaginal as well as elective C-section delivery was well studied. In C-section cases, immediate SSC is achievable using spinal or epidural anaesthetics (WHO & UNICEF 2009)Citation27. Growing trends on emergency C-section cases were documented in recent years, and to date there is limited research on the benefits of KMC reported in these cases, particularly in the province of Saudi Arabia. Thus, our objective was to scrutinize how hormonal fluctuations during KMC practice to mothers who underwent emergency cesarean delivery alters maternal and neonatal behaviour relevant to stress, wound healing and feeding aspects.
Materials and Methods
Study Design
This present retrospective study was carried out on leftover stored samples (secondary use). The de-coded patient material was used in accordance with the Institutional Ethics Committee. Data pertaining to mothers who delivered a baby via emergency C-section delivery between January 2022 and December 2022 and those who met the inclusion criteria were identified through the available electronic database.
Study Sample
Inclusion
The eligibility criteria were women who delivered via emergency C-section and were exposed to KMC at different time points during hospitalization. All pregnancies were primiparous and delivery took place between 34 and 40 weeks of gestation. Samples collected before and after KMC were included.
Exclusion
Samples were excluded who had a pregnancy with HIV/HBV/HCV, history of confirmed COVID-19, pregnancy with chronic diseases, received steroid therapy in the last 72 hours, twin pregnancy, fetal death and congenital abnormalities of the fetus.
KMC Procedure
Briefly, intermittent KMC was routinely practised for approximately 15–30 minutes in a day for three to four times at intervals until discharge, mainly before breastfeeding.
Sample Collection
Step-down thawing of stored remnant serum was followed, mixed well and aliquoted before use. Convenience sampling was adopted.
Variables and Measurements
Maternal hormones including oxytocin, cortisol, prolactin, IL-6 and IL-10 were analysed. Data on other parameters such as baby-crying time, feeding frequency and feeding duration were retrieved.
Quantification of Serum Hormones
Oxytocin (OXT): the serum concentration of OXT was analysed using Enzyme Linked IuumoSorbent Assay kit (EIAab). This quantitative sandwich immunoassay detects OXT in the range between 15.6 and 1000 pg/mL with a limit of detection at <11.7 pg/mL. The concentration was determined as per the manufacturer’s protocol and by measuring the end-point colour intensity using a spectrophotometer at 450 nm.Citation26
Cortisol and prolactin (PRL): the maternal cortisol and prolactin in serum were determined by competitive ELISA kits, DiaMetra ELISACitation28 and EIA kit respectively.Citation29
Serum Inflammatory Markers
IL-6 and IL-10: IL-6 and IL-10 in maternal serum samples collected at different time points were measured by ELISA (eBioscience, San Diego, CA). The sensitivity of each assay kit was 2 pg/mL; the samples were assayed in triplicate for determining the intra- or inter-assay coefficient variations (CV). Each run was considered valid only when the results of CV were 14.0% and 3%, respectively.
Other Neonatal Parameters
Variables for breastfeeding outcomes and infant-related parameters were adapted from Abdulghani et al's studyCitation30 with modifications: (1) breastfeeding initiation time in hours (h) and (2) feeding duration was measured in average min/day. Infant’s crying time (h/day) and duration of hospital stay (days) were also assessed from clinical data.
Statistical Analysis
Data were extracted from the database, converted into an Excel sheet and analysed using the Statistical Package for the Social Sciences (SPSS), version 21. All statistical tests were performed with a two-sided significance level of 5%. Results were presented as mean ± standard deviation (SD) and the range were determined for each data set by descriptive statistics. The distribution of data for each variable at different intervals under two groups was presented in box and whisker plot. Within and between-group variance were measured by one-way ANOVA, followed by a Tukey Post-hoc test. The Pearson correlation matrix among the KMC group was constructed to identify the relationship within and between the study variables.Citation31
Ethics
This study protocol was in accordance with the Research Ethics Committee of King Khalid University, Kingdom of Saudi Arabia (ECM#2023-1702). All data were de-identified, provided a unique study code and conserved using a password-protected archive.
Results
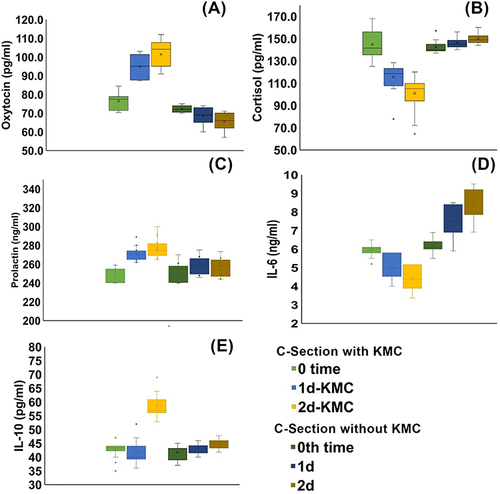
There were no adverse events or wound or infections reported during the study period. There were no reports of delayed surgical healing or wound infection. A total of 25 mothers’ serum who underwent cesarean was included in the study. Of which, 16 serum were from mothers who practised KMC (KMC group) while nine did not practise KMC (control group). This study focused on the variations in serum hormonal and cytokine levels observed after KMC practice in emergency C-section mothers. depicts the change in serum hormonal and cytokine profile between and within groups at different time intervals.
Figure 1 Changes in hormonal levels (A) oxytocin, (B) cortisol and (C) prolactin and cytokine levels (D) interleukin-6 and (E) interleukin-10 among the KMC group. Data represented in a box and whisker plot in which distribution of data are depicted as percentiles. The minimum value on the Y axis (pg/mL) of each graph is adjusted to the nearest low level of each parameter studied. KMC, kangaroo mother care; d, day(s).
Serum OXT Quantification
Basal quantity of OXT did not differ significantly between with and without KMC practice among emergency C-section mothers (70.4 vs 70.0 pg/mL). KMC positively influenced the oxytocin level with an increase from basal line over three days postpartum from 70.4 to 112.0 pg/mL. Mothers who delivered via emergency cesarean but did not undergo KMC showed decreased OXT concentration (~16 pg/mL) in the following 2nd day postpartum. The net difference between the last day OXT quantities between two groups was 36 pg/mL (112.0 vs 65.5 pg/mL). In the KMC group, the minimum was 70.4 pg/mL and a maximum level was 112.0 pg/mL. The data range differs from 14.1, 15.7 and 21.0 in the KMC group whereas control samples showed 5.0, 14.0 and 14.0 pg/mL, respectively. The increase in OXT level was significantly evidenced in the KMC group as compared to control serum ().
Serum Cortisol Quantification
Higher cortisol levels were observed in the control serum of the women who underwent C-section labour: 146.1 ± 4.8 ng/mL and 150.0 ± 5.4 ng/mL for 1st and 2nd day after delivery, respectively. The minimum and maximum values in that group of serum samples were 156 ng/mL and 140 ng/mL. The peak cortisol peptide of 144.7 ± 14.0 ng/mL was controlled in the KMC serum group to 100.9 ± 15.0 ng/mL. In addition, a significant falling trend () in the cortisol concentration due to repeated sessions of KMC practice was evidenced in these two days (144.7 vs 115.6 ng/mL).
Prolactin Level
The mean PRL level of 2nd day in the KMC mothers (276.6 ± 10.0 mg/dL) was significantly higher than that in the control group (256.6 ± 13.4 mg/dL) (p=0.001). The maximum and minimum values observed in this study were 240.0 mg/dL (baseline in both groups) and 300.0 mg/dL (2nd day KMC group).
Serum Inflammatory Markers
and clearly shows the positive effect of KMC practice among cesarean mothers. On day 1 and 2, the mean baseline IL-6 serum levels in non-KMC mothers were 7.4 ± 0.9 and 8.3 ± 0.8 pg/mL, while after KMC they were significantly reduced to 5.1 ± 0.7 and 4.5 ±0.8 pg/mL (P=0 0.01).
The mean serum level of IL-10 on day 2 in the control group was 45.1 ± 2.9 pg/mL, whereas in the KMC group it was significantly higher up to 58.7 ± 4.1 pg/mL (P=0.05).Citation32 These levels differ with the mean baseline levels (41.7 ± 2.7 and 43.0 ± 3.2 pg/mL) in the control and 0th day KMC groups, respectively.
Other Neonatal Parameters
Breastfeeding and other neonatal outcomes are presented in . Mothers in the KMC group have started their lactation in 39.3 ± 2.59 h, while it was 49.3 ± 2.65 h in the control group. None started their first breastfeeding within 24 h. The average feeding time per lactation was higher in the KMC group (10.00 ± 3.0 average min/day) as compared to the non-KMC group (15.31 ± 1.2 average min/day). During the first two to three days after birth, about two-thirds of mothers in the KMC group exclusively breastfed directly at the breast (n = 16, 64%). In control infants, the mean crying time was 2.26 ± 1.38 h/day but got reduced to 1.50 ± 0.25 h/day in KMC infants (P=0.001). Due to the hormonal changes induced as a result of KMC practice, the hospital stay for mothers in emergency C-section was reduced to 3.69 from 4.81 days.
Table 1 Evaluation of KMC on Other Maternal and Neonatal Parameters
Correlation Matrix
A detailed relationship matrix within (at different time points) and between quantitative variables in KMC group is tabulated as . As the frequency of KMC practice increased, a strong positive correlation was observed across two days in all parameters studied. IL-6 showed a high r value (r=0.946, IL-6 (2) vs IL-6 (3)), followed by IL-10 (r=0.886, IL-10 (2) vs IL-10 (3)) and OXT (r=0.877, OXT2 vs OXT3). As OXT gradually increased from day 0 to day 2, prolactin (r=0.477, OXT1 vs PRL1) and IL-10 (r=0.63, OXT3 vs IL-10 (3)) also increased. A negative correlation was evidenced in all the other molecules such as cortisol and IL-6. Highest was between OXT and IL-6 on day 2 (r=−0.800).
Table 2 Pearson’s Correlation Matrix Within and Between the KMC Group
Discussion
Many studies have documented data on attitude, knowledge and implementation of KMC among nurses in Saudi Arabia.Citation33–35 In the study region, it was found that KMC was less often in practice due to newborn infants often being separated from their mothers and hence delayed breastfeeding initiation for hours or days was observed.Citation17 The present study’s aim was to determine the hormonal levels after intermittent KMC practice in mothers who had emergency C-section and compare them with the non-KMC C-section group. To our knowledge, this is the first report on intermittent KMC that improves oxytocin level in emergency cesarean delivery. The outcome was justified quantitatively using immunoassays and behavioural neonatal parameters. Due to practical difficulties, remnant serum samples were obtained at relatively long intervals.
KMC is devoted to mothers who had preterm deliveries or with infants less than 2000 g birth weight. Few studies have compared the benefits of KMC practice on elective C-section and vaginal deliveries. Among cesarean deliveries, there are different modes such as elective (personal decision) and emergency (medical need) becoming routine in these days. Hence, it is important to reveal the health benefits of KMC on emergency C-section mothers. Results showed overall pros of SSC practice with respect to the hormonal levels.
Oxytocin
The OXT concentration found in the study sample is comparable (32.3 to 2297.6 pg/mL) with the previous data. The author reported a two-fold difference among individuals in OXT levels (57 to 108 pg/mL).Citation36 However, peripheral OXT levels in women documented by other studies was much lower than this.Citation37 Thus determined OXT values in this study using stored serum samples differ with the previous findings in terms of sample processing and assay methods. Previously, the maternal OXT levels among mothers who had spontaneous delivery were mentioned as higher but not significantly than those at elective C-section. The maternal–fetal attachment scale resulted in higher OXT in women during the third trimester.Citation38 Another study concluded that mothers with lower level of OXT had experienced postpartum depression in mid-pregnancy.Citation39
Cortisol
An earlier study has noted that the range of serum cortisol was from 831 ± 257 nmol/L to 906 ± 243 nmol/Lin pre- and post-operative cesarean delivery, respectively. S-cortisol was significantly higher among spontaneous delivery women as compared to the preoperative cesarean section mothers.Citation40 Many have worked in elective C-section, but there is still lacunae on S-cortisol levels at emergency C-section in this study region. The present data on KMC practice have also shown a reduction in S-cortisol level in the KMC group as compared to the non-KMC group.
Prolactin
The present study observed that the mothers in the KMC group had less anxiety which contributed to more active breastfeeding resulting in generous milk production. The increased prolactin level in the KMC group further validated the copious milk secretion. This facilitates the milk production, initiation of breast feed, prolongation of feeding time and frequency of feed per day. High prolactin levels support exclusive breastfeeding which indirectly reduces mortality in low birth weight infant. The present result suggests that there is no need for drugs for prolactin secretion. KMC makes patients more relaxed that reduces trauma after C-section delivery.
Feeding Behaviour
Studies conducted in Saudi Arabia mostly compared elective C-section with vaginal delivery.Citation41 In this study, the intermittent KMC among cesarean delivery revealed a minor proportion of mothers breastfeed on the day of delivery. This is contrary to what has been previously reported (ranged from 76% to 98%). This because of mother–infant separation was unknowingly practised during the initial hour after birth in emergency C-section. A growing body of evidence supports the association between KMC during the first hour postpartum with successful breastfeeding. This study revealed breastfeeding directly at the breast observed during the postpartum stay was 62% and is associated well with increased breastfeeding even at six months postpartum.Citation41
Crying Time
As seen in infants of the KMC group, the decrease in crying time and restlessness, and an increase in the duration of deep sleep and relaxation were documented in colicky infants.Citation42
Colicky infants responded well to KMC practice as it significantly reduced the symptoms of irritability and crying in comparison with the control group.Citation43
Cytokines
The clinical consequences of modulating wound cytokine concentrations and anti-inflammatory strategies are incompletely understood among emergency C-section deliveries and hence require detailed studies. The postoperative pain can be mediated by the release of various kinds of inflammatory cytokines from the wound itself.
Generally, analgesia can inhibit or reduce the release and movement of pro-inflammatory cytokines to wound tissue, thereby accelerating the wound's recovery.Citation44
The IL-6 concentration decreased in this study rather than elevated as previously reported, most likely reflecting the effect by KMC practice that significantly reduced the levels of both. The IL-6 level in the control group began to increase postoperatively at day 1 and maintained at day 2. This pain-induced higher level of IL-6 level in this group was brought down effectively by analgesia in postoperative care.Citation45
The present study justified the changes in serum IL-10 levels were indirectly proportional in the study groups; its level began to rise postoperatively at day 1 and peaked at day 2. A study has found that the pre-operative levels of IL-6 was higher but IL-10 was relatively unchanged.Citation44 This explains the relationship between the two different effects of cytokines during post-operation and from the surgical wound site.
The overall comparison revealed that KMC might have control on the hypothalamic–pituitary–adrenal axis which was evidenced by the correlation matrix. Once OXT secretion is triggered by KMC on day 1, cortisol and IL-6 levels were in a down trend that resulted in the surge of prolactin hormone and upregulation of IL-10. This rise in OXT and PRL are known to facilitate lactation in cesarean mothers. The pro-inflammatory cytokine decreased with an increase in OXT may reduce postoperative trauma. Hence, the mothers in the intervention group showed a reduction in hospital stay with earlier discharge as compared to the control group. KMC, a simple, effective and easy to perform nursing strategy, has shown several health benefits for both cesarean mothers and their infants.
Limitations of the Study
Only samples with data for all study parameters were included. Due to practical difficulties, remnant serum samples were obtained at relatively long intervals. Further subgrouping that comprises preterm and term deliveries was not focused. A prospective-based cohort study with a large sample size will substantiate the findings of the present study.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Betran A, Torloni MR, Zhang JJ, et al. WHO statement on caesarean section rates. BJOG. 2016;123(5):667–670. doi:10.1111/1471-0528.13526
- Betrán AP, Ye J, Moller A-B, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and national estimates: 1990–2014. PLoS One. 2016;11(2):e0148343. doi:10.1371/journal.pone.0148343
- Olieman RM, Siemonsma F, Bartens MA, Garthus-Niegel S, Scheele F, Honig A. The effect of an elective cesarean section on maternal request on peripartum anxiety and depression in women with childbirth fear: a systematic review. BMC Pregnancy Childbirth. 2017;17:195. doi:10.1186/s12884-017-1371-z
- Xie R-H, Gaudet L, Krewski D, Graham ID, Walker MC, Wen SW. Higher cesarean delivery rates are associated with higher infant mortality rates in industrialized countries. Birth. 2015;42(1):62–69. doi:10.1111/birt.12153
- Yaqoub RM, Khouj MA, Alsaif AA, Eissa GA, Alhemdi JA, Albasri S. Awareness and knowledge of caesarean section complications among women in Jeddah, Saudi Arabia. Cureus. 2022;14(12):e32152. doi:10.7759/cureus.32152
- Ahmed AE, Mohammad RS. Motives for - and prevalence of - cesarean delivery on maternal request: a survey in Saudi Arabia. Qatar Med J. 2019;2019(1):2. doi:10.5339/qmj.2019.2
- AlSheeha MA. Epidemiology of Cesarean Delivery in Qassim, Saudi Arabia. Open Access Maced J Med Sci. 2018;6(5):891–895. doi:10.3889/oamjms.2018.213
- Nurdin NOS, Wantania JJE, Mewengkang RAA. Assosiation between serum cortisol levels and anxiety levels in elective and emergency cesarean section: hubungan antara kadar kortisol serum dan tingkat kecemasan pada operasi caesar elektif dan darurat. Indones J Obstet Gynecol. 2022;205–210. doi:10.32771/inajog.v10i4.1624
- Martinez LD, Glynn LM, Sandman CA, Wing DA, Davis EP. Cesarean Delivery and Infant Cortisol Regulation. Psychoneuroendocrinology. 2020;122:104862. doi:10.1016/j.psyneuen.2020.104862
- Uvnäs-Moberg K. Maternal plasma levels of oxytocin during breastfeeding—A systematic review. PLoS One. 2020;15(8):e0235806. doi:10.1371/journal.pone.0235806
- Trifu S, Vladuti A, Popescu A. The neuroendocrinological aspects of pregnancy and postpartum depression. Acta Endocrinol. 2019;15(3):410–415. doi:10.4183/aeb.2019.410
- Al-Shehri H, Binmanee A. Kangaroo mother care practice, knowledge, and perception among NICU nurses in Riyadh, Saudi Arabia. Int J Pediatrics Adolesce Med. 2021;8(1):29–34. doi:10.1016/j.ijpam.2019.11.003
- Stevens J, Schmied V, Burns E, Dahlen H. Immediate or early skin‐to‐skin contact after a Caesarean section: a review of the literature. Matern Child Nutr. 2014;10(4):456–473. doi:10.1111/mcn.12128
- Moore ER, Anderson GC, Bergman N, Dowswell T. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2012;5(5):CD003519. doi:10.1002/14651858.CD003519.pub3
- Saxton A, Fahy K, Hastie C. Effects of skin-to-skin contact and breastfeeding at birth on the incidence of PPH: a physiologically based theory. Women Birth. 2014;27(4):250–253. doi:10.1016/j.wombi.2014.06.004
- Aghdas K, Talat K, Sepideh B. Effect of immediate and continuous mother–infant skin-to-skin contact on breastfeeding self-efficacy of primiparous women: a randomised control trial. Women Birth. 2014;27(1):37–40. doi:10.1016/j.wombi.2013.09.004
- Bramson L. Effect of early skin-to-skin mother--infant contact during the first 3 hours following birth on exclusive breastfeeding during the maternity hospital stay. J Hum Lact. 2010;26(2):130–137. doi:10.1177/0890334409355779
- Marín Gabriel MA, Llana Martín I, López Escobar A, Fernández Villalba E, Romero Blanco I, Touza Pol P. Randomized controlled trial of early skin-to-skin contact: effects on the mother and the newborn. Acta Paediatr. 2010;99(11):1630–1634. doi:10.1111/j.1651-2227.2009.01597.x
- Cooijmans KHM, Beijers R, Brett BE, de Weerth C. Daily mother-infant skin-to-skin contact and maternal mental health and postpartum healing: a randomized controlled trial. Sci Rep. 2022;12:10225. doi:10.1038/s41598-022-14148-3
- Bigelow A, Power M, MacLellan-Peters J, Alex M, McDonald C. Effect of mother/infant skin-to-skin contact on postpartum depressive symptoms and maternal physiological stress. J Obstet Gynecol Neonatal Nurs. 2012;41(3):369–382. doi:10.1111/j.1552-6909.2012.01350.x
- Badr HA, Zauszniewski JA. Kangaroo care and postpartum depression: the role of oxytocin. Int J Nurs Sci. 2017;4(2):179–183. doi:10.1016/j.ijnss.2017.01.001
- Zhou Y-Q. Interleukin-6: an emerging regulator of pathological pain. J Neuroinflammation. 2016;13(1):141. doi:10.1186/s12974-016-0607-6
- Torrance HDT. Post-operative immune suppression is mediated via reversible, Interleukin-10 dependent pathways in circulating monocytes following major abdominal surgery. PLoS One. 2018;13(9):e0203795. doi:10.1371/journal.pone.0203795
- Mosser DM, Zhang X. Interleukin-10: new perspectives on an old cytokine. Immunol Rev. 2008;226:205–218. doi:10.1111/j.1600-065X.2008.00706.x
- Singampalli KL. The role of an IL-10/hyaluronan axis in dermal wound healing. Front Cell Dev Biol. 2020;8:636. doi:10.3389/fcell.2020.00636
- Achie LN, Ibrahim G, Olorunshola KV, Ayegbusi FO, Toryila JE. Serum levels of oxytocin in pregnancy, parturition and postpartum for Nigerian females in Zaria, Nigeria. Afr J Pharm Pharmacol. 2016;10(21):458–464. doi:10.5897/AJPP2015.4406
- World Health Organization & UNICEF (2009) () Baby‐Friendly Hospital Initiative. Revised Updated and Expanded for Integrated Care. Section 3: Breastfeeding Promotion and Support in a Baby‐Friendly Hospital: A 20‐Hour Course for Maternity Staff. : http://whqlibdoc.who.int/publications/2009/9789241594981_eng.pdf (Accessed 27 September Accessed 2023). Available from:
- Bulska M. Different modes of delivery and hormonal stress response. Ginekol Pol. 2021;92(7):481–486. doi:10.5603/GP.a2021.0068
- Respati SH, Bhaskoro R, Yuliantara EE, Budihastuti UR, Septiawan D. Effect of hypnotherapy on prolactin level in women after cesarean section. Univ Med. 2023;42(1):6–11. doi:10.18051/UnivMed.2023.v42.6-11
- Abdulghani N, Cooklin A, Edvardsson K, Amir LH. Mothers’ perceptions and experiences of skin-to-skin contact after vaginal birth in Saudi Arabia: a cross-sectional study. Women Birth. 2022;35(1):e60–e67. doi:10.1016/j.wombi.2021.02.001
- Hassanshahi G. Anesthesia technique and serum cytokine concentrations in the elective cesarean section. J Res Med Sci. 2021;26:91. doi:10.4103/jrms.JRMS_536_20
- Stein K. Leukocyte-derived interleukin-10 aggravates postoperative ileus. Front Immunol. 2018;9:2599. doi:10.3389/fimmu.2018.02599
- Al Mutair A. Assessment of nurses’ knowledge, attitude and implementation of skin‐to‐skin care within the perinatal setting in Saudi Arabia: survey study. Nursing Open. 2023;10(4):2165–2171. doi:10.1002/nop2.1464
- Cristóbal Cañadas D, Parrón Carreño T, Sánchez Borja C, Bonillo Perales A. Benefits of kangaroo mother care on the physiological stress parameters of preterm infants and mothers in neonatal intensive care. Int J Environ Res Public Health. 2022;19(12). doi:10.3390/ijerph19127183
- Taha Z, Wikkeling-Scott L. Review of Kangaroo Mother Care in the Middle East. Nutrients. 2022;14(11). doi:10.3390/nu14112266
- Prevost M. Oxytocin in Pregnancy and the Postpartum: relations to Labor and Its Management. Front Public Health. 2014;2:1. doi:10.3389/fpubh.2014.00001
- Grewen KM, Davenport RE, Light KC. An investigation of plasma and salivary oxytocin responses in breast- and formula-feeding mothers of infants. Psychophysiology. 2010;47(4):625–632. doi:10.1111/j.1469-8986.2009.00968.x
- Levine A, Zagoory-Sharon O, Feldman R, Weller A. Oxytocin during pregnancy and early postpartum: individual patterns and maternal-fetal attachment. Peptides. 2007;28(6):1162–1169. doi:10.1016/j.peptides.2007.04.016
- Skrundz M, Bolten M, Nast I, Hellhammer DH, Meinlschmidt G. Plasma oxytocin concentration during pregnancy is associated with development of postpartum depression. Neuropsychopharmacology. 2011;36(9):1886–1893. doi:10.1038/npp.2011.74
- Stjernholm YV, Nyberg A, Cardell M, Höybye C. Circulating maternal cortisol levels during vaginal delivery and elective cesarean section. Arch Gynecol Obstet. 2016;294(2):267–271. doi:10.1007/s00404-015-3981-x
- Al Juaid DAM, Binns CW, Giglia RC. Breastfeeding in Saudi Arabia: a review. Int Breastfeed J. 2014;9(1):1. doi:10.1186/1746-4358-9-1
- Ellett MLC, Bleah DA, Parris S. Feasibility of using kangaroo (skin-to-skin) care with colicky infants. Gastroenterol Nurs. 2004;27(1):9–15. doi:10.1097/00001610-200401000-00003
- Saeidi R. Kangaroo mother care for infantile colic: a randomized clinical trial; 2010.
- Xing Z-M, Zhang Z-Q, Zhang W-S, Liu Y-F. Effects of analgesia methods on serum IL-6 and IL-10 levels after cesarean delivery. Genet Mol Res. 2015;14(2):4778–4783. doi:10.4238/2015.May.11.10
- Arababadi MK. Cytokines in Preterm Delivery. Lab Med. 2012;43(4):27–30. doi:10.1309/LMY9ILPGSETU2CO0
