Abstract
This umbrella review was to synthesize the summarized evidence-based research regarding interventions addressing symptoms in older populations with multimorbidity. Three databases including PsycINFO, MEDLINE, and CINAHL were searched systematically. The JBI Methodology for Umbrella Reviews and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statements were used to report this review. Six reviews published between 2016 and 2010 were included for analysis. Interventions were mixed and included components on health-related behaviors, body systems or functions, activities and participation domains, and the environment. Outcomes concerning physiological/clinical functioning were most reported. The evidence regarding the symptoms-related interventions was mixed, but all showed promising outcomes compared with usual care or not. To sum up, this umbrella review reveals the lack of strong empirical evidence for the effectiveness of intervention addressing symptoms in older adults with multimorbidity. It highlights the need to evaluate the established approach of interventions further to support this population.
Introduction
As the global population continues to age, the prevalence of multimorbidity among older adults has become a significant public health concern.Citation1 Multimorbidity, also known as multiple chronic conditions, is defined as the co-existence of two or more chronic health conditions in one person and usually requires ongoing healthcare.Citation2 The epidemiological statistics of multimorbidity varied greatly based on the conditions considered in count,Citation3 this might be explained by the absence of consensus on the operational definitions of multimorbidity. For example, researchers utilized data from the Chinese Longitudinal Healthy Longevity Survey (CLHLS) to assess physical multimorbidity.Citation4 They considered a total of 19 chronic diseases, including conditions like hypertension, diabetes, heart disease, and stroke or CVD. Another study conducted in Australia investigated the occurrence of multimorbidity by examining 21 chronic health conditions such as arthritis, bowel disease, Crohn’s disease, liver disease, and others.Citation5 Although it is possible to ascertain diverse variants of the term of multimorbidity across studies. These conditions can profoundly impact the quality of life of older adults,Citation6 as they often experience a range of symptoms that can be challenging to manage.Citation7
Symptoms may refer to expressions of disturbed features in the body and mind by a patient.Citation8 Symptom science in the context of nursing principally focuses on ranges from understanding the etiology of diseases’ symptoms and possible clusters to developing creative measures and interventions to lessen their negative impacts.Citation9 The management of symptoms in older adults with multimorbidity is a complex and multifaceted task because of the inconsistent definitions of multimorbidity and the challenges in examining various outcomes.Citation10 It requires a comprehensive understanding of the unique physiological, psychological, and social factors that influence symptom presentation and progression in multimorbid populations. The presence of multimorbidity often necessitates a holistic and integrated approach to care, where healthcare professionals must consider the interactions between different conditions and their respective symptoms.Citation11 Also, healthcare professionals must focus on the individual needs and preferences of older adults, as well as the available resources and support systems in place.Citation12 Furthermore, older adults with multimorbidity may experience age-related physiological changes that can impact symptom presentation and response to treatment. For example, alterations in metabolism, organ function, and immune response can influence the pharmacokinetics and pharmacodynamics of medications used for symptom management.Citation13,Citation14 These age-related changes may necessitate dosage adjustments or alternative treatment modalities to optimize symptom management.
In recent years, there has been a growing recognition of symptom-oriented interventions for older adults with multimorbidity. Tripp-Reimer et alCitation15 established the Integrated Model of Multimorbidity and Symptom Science model of connecting multimorbidity with symptom science, which incorporates three predominate domains (1) risk factors, which are based on the WHO’s framework and contain individual and contextual factors; (2) interactions among symptoms, diseases, and treatments, highlighting the dynamic relationships between these elements; and (3) patient outcomes, which focus on patient-centered measures such as morbidity, mortality, functioning, well-being, burden related to multimorbidity, and optimizing self-care. The integrated model highlights the position of personalized care, recognizing that each person’s experience of multimorbidity and associated symptoms is different. It also underlines the necessity for interdisciplinary collaboration in research and clinical practice, as well as the importance of patient-centered care in managing multimorbidity. According to this model, healthcare professionals are encouraged to document symptoms, monitor their changes over time, and consider symptom management when making healthcare decisions for individuals with multimorbidity.
With the global population aging, the number of older adults with multimorbidity is growing. This presents a significant challenge for healthcare systems worldwide. In addition, the complex nature of multimorbidity indicates that a one-size-fits-all approach to treatment needs refinement and improvement. By gaining a deeper understanding of the complexities surrounding symptom management in older adults with multimorbidity, we can work towards developing more tailored and effective approaches to care. As a result, we aimed to explore the current evidence and best practices of interventions addressing symptom-related outcomes among older adults with multimorbidity. We will examine various strategies and interventions that have been shown to be effective in alleviating symptoms and improving the outcomes for this population.
Aims and Research Questions
This umbrella review aimed to summarize the existing systematic reviews focusing on interventions in addressing symptoms in older adults with multimorbidity. The specific research questions were:
What interventions are used to manage symptoms in older adults with multimorbidity?
In what healthcare aspects, contexts, and settings have studies of those interventions been conducted?
How have those interventions been examined regarding their health-related outcomes?
Materials and Methods
Design
An umbrella review is an overview of previous reviews.Citation16 We chose this Design in this study because (1) since the first publication of the Symptom Management Model,Citation17 researchers have applied this model across different settings and published a growing number of reviews; (2) an umbrella review helps to answer a broad question and can contribute to the development of further interventions and guidelines.Citation18
The protocol for this study was registered on the Open Science Framework (https://osf.io/6rx3k). The methodology was developed based on the JBI Methodology for Umbrella Reviews.Citation16 We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement to enhance the transparency of reporting in this study.Citation19
Literature Search
An electronic search guided by the PICO (population, intervention, comparator, and outcomes) framework was conducted on October 4, 2023, and updated on Nov 28, 2023. Three databases were systematically searched: MEDLINE, CINAHL, and PsycINFO. The publication data was limited to 10 years to obtain the most recent evidence. In addition, the reference lists of included reviews were also searched. reports the search concepts and terms of this review.
Table 1 Academic Search Approach
Literature Management
Search results were imported into EndNote TM 21 for screening. After the check of duplicates, a two-step screening was conducted: titles and abstracts and full-text check. We included systematic reviews that evaluated symptom management in addressing multimorbidity among the older population. Two authors independently examined all potential reviews against the inclusion and exclusion criteria. Any disagreements were discussed and a third experienced researcher was available for assistance. reports the inclusion and exclusion criteria of this review.
Table 2 Inclusion and Exclusion Criteria
Quality Assessment
We used JBI’s critical appraisal tools for systematic review as an instrument to assess systematic reviews.Citation20 Any disagreements were discussed and a third experienced researcher was available for consultation. No review was excluded due to low quality.
Data Collection
We extracted the following information with three designed tables: (1) general information including author and publication year, aim, setting and sample, multimorbidity of interest, designs of included studies, the timeframe of review, and key findings; (2) Intervention & outcomes information including the type of interventions, the outcome of interests, and quality of evidence; and (3) quality assessment information including quality appraisal method and results. Two authors extracted the above information independently and then compared their results. A third experienced researcher was available for consulting if necessary.
Data Analysis
Given the heterogeneous definition of multimorbidity and mixed interventions analyzed in previous reviews, we adopted a narrative approach to systematically and transparently summarize past systematic evidence and to provide a text-based synthesis instead of a statistical analysis.Citation21
Results
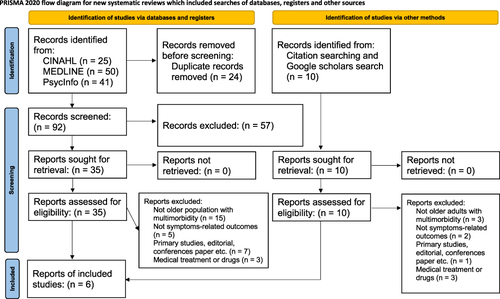
illustrates a flow diagram of publication selection. We screened 126 citations and identified six potentially relevant full-text articles. Excluded articles were presented with reasons.
reports the key characteristics of the included reviews. Six reviews were published between 2016 and 2010, with 72 studies involved (RCT: 52).Citation22–27 Most reviews did not limit their research settings, only two focused on home care.Citation22,Citation23 All reviews aimed to examine a certain type of intervention for older adults with multimorbidity. Most reviews demonstrated their broad definition of multimorbidity and one focused on dementia and multimorbidity.Citation25 The most common conditions were diabetes, hypertension, respiratory diseases, and heart diseases.
Table 3 Key Characteristics of Included Reviews
reports the summary of interventions and their outcomes. We used the International Classification of Health Interventions (ICHI) to categorize and report interventions in this review as the ICHI offers a standardized procedure for collecting, combining, and analyzing health-related interventions.Citation28 According to ICHI, interventions of the included reviews were mixed and involved components of health-related behaviors, body systems or functions, activities and participation domains, and the environment.
Table 4 Summary for the Interventions, Outcomes, and Quality of Evidence of Included Reviews
We adopted the taxonomy for outcome classification to classify and report symptom-related outcomes that participants achieve through interventions in this review.Citation29 Outcomes concerning physiological/clinical functioning were most reported. Only two reviews have mentioned biochemical indicators.Citation23,Citation27
reports the adopted quality appraisals of included reviews. Most used Grading of Recommendations, Assessment, Development and Evaluation (GRADE) or Cochrane Collaboration tools as an instrument. The included reviews reported mixed ratings of their reviewed studies. Several authors suggested their Results might be affected by the study quality.
Table 5 Summary of Quality Appraisal of Included Reviews
reports the methodological quality assessment of the included reviews. Overall, the quality of the included reviews was satisfactory as those reviews generally met most requirements of the checklist. The most important sources of possible risk of bias were the indication of review questions according to the JBI checklist.
Table 6 Methodological Quality Assessment by JBI Critical Appraisal Checklist
Discussion
This umbrella review has presented an overview of evidence for intervention addressing symptoms across settings in older adults with multimorbidity. The evidence regarding the symptoms-related interventions was mixed, but all showed promising outcomes compared with usual care or not. These interventions have positive effects on such as self-reported health status, clinical indicators, and health service use, and may also improve knowledge, attitude, and behaviors.
Older adults are considered at greater risk of vulnerability.Citation30 The longer one lives, the more likely one is to be diagnosed with multimorbidity. Compared with an earlier overview of the management of multimorbidity,Citation31 our study outlines the paucity of interventions designed to manage multimorbidity in aging populations, especially in the area of symptoms. Petrillo and RitchieCitation10 indicated that inconsistent definitions of multimorbidity and variety in outcome measurement were two major challenges of symptom management for multimorbidity. There were a range of terminologies and definitions were used to identify multimorbidity.Citation32 Due to the complex nature of multimorbidity, older adults with multimorbidity often have various healthcare needs, making it challenging to examine their symptoms across different clinical settings. In this review, our focus was on interventions that specifically address symptoms. However, the literature covers a wide range of outcomes, including but not limited to measures of function, QoL, and mood indicators such as anxiety and depression. Selecting appropriate and valid outcome measures for symptoms is crucial as it directly impacts the effectiveness of the corresponding intervention. Unfortunately, there is a lack of standardization in both the measurement and reporting of symptom-related outcomes in clinical trials related to multimorbidity. This lack of standardization hinders efforts to synthesize evidence and may contribute to observed heterogeneity and bias, caused by factors like challenges in data collection, variations in instruments used, and differences in the length of follow-up. The validity and feasibility of measuring symptoms can significantly impact the validity of the evidence base and potentially limit its applicability in real-world settings. Also, previous researchers have indicated the gap between disease-focused care and patients’ needs-oriented care in the multimorbid population.Citation33 Guidelines developed by NICE (National Institute for Health and Care Excellence) suggest that the implementation of effective care for people with multimorbidity requires tailored plans based on a personalized assessment.Citation34
Kastner et alCitation35 synthesized and classified three types of theory-based interventions to explain multimorbidity management: (1) care coordination interventions, (2) illness prioritization, and (3) self-management. We found that most previous reviews focused on behavior change and psychosocial support, primarily referring to disease management. Only two reviews mentioned care-coordinated intervention. This inconsistency might be explained by the diversity in research aims and authors’ expertise. For example, Goehner, Kricheldorff and BitzerCitation24 presented the interventions delivered by trained volunteers while other reviews mainly included interventions provided by healthcare professionals. To tackle the complex needs of people with multimorbidity, integrated care, also known as coordinated care, comprehensive care, which incorporates health assessment, treatment, management, rehabilitation, and so on, should be advocated.Citation36 Thus, we suggest that further research values the significance of integrated care from many different settings in clarifying the best clinical pathways given its potential of caring for multimorbid populations.
Despite the variety of included reviews in types of interventions, the implementer of intervention, and outcomes, all showed promising impacts. QoL, physical functioning, and moods in terms of anxiety and depression were considered as predominant outcomes that multimorbidity negatively affects.Citation37–40 In line with the results from a large cross-sectional study, which showed old adults with multimorbidity might report more symptoms of psychological distress. Our study suggested the significance of mental health among older adults with multimorbidity. In addition, those outcomes summarized in each review also reflect the components of the intervention offered. Given the variety of interventions identified and the overall quality of evidence, further studies are needed to strengthen these findings.
This umbrella review identified several knowledge gaps in multimorbid outcomes in the context of aging. First, there was a dearth of attention on the symptom burden, referring to the subjective, quantifiable burden on patients.Citation41 Evidence shows that people with multimorbidity face challenges concerning their symptoms, which is a substantial burden for them,Citation7 and the association between symptom burden and functional status in individuals with multimorbidity was significant.Citation42 Also, out of the important domains of outcomes, no specific interventions for morbidity and mortality were identified, suggesting a lack of long-term effectiveness of interventions within multimorbidity research. Furthermore, after a categorization of the interventions retrieved, we found that still there was a substantial gap in interventions addressing basic needs, including social care and support services, and interventions that enhance societal contribution.
This umbrella review had limitations. We used terms such as symptoms and signs to search past reviews that focus on symptom-based intervention. The search terms were intentionally broad, so some reviews outlining “health communication between healthcare professionals and patients” and “shared decision-making” might have been excluded. Next, interventions for symptom management are diverse, especially in the area of multimorbidity. The timeframe was limited to the last 10 years to offer a most recent summary of evidence, but reviews published before were not considered. The number of databases searched in this umbrella review was also limited as we had a healthcare emphasis. We narratively categorized certain types of interventions described across reviews based on their research questions. This might have prevented us from comparing those interventions and making Conclusions regarding the effects of those interventions.
Conclusion
This review aims to improve the current understanding and offer insights that can guide clinical practice and policy decisions, ultimately enhancing the well-being of older adults who have multimorbidity. The findings of this study suggest that interventions for symptom management show promise, but the empirical evidence supporting them is limited. It is recommended that future research should emphasize the need for larger and more rigorous trials and develop guidelines for assessing and reporting outcomes related to multimorbidity. By using standardized definitions, protocols for exposures and outcomes, and statistical analyses, the potential biases can be minimized, leading to more reliable and trustworthy literature in this area.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Chowdhury SR, Das DC, Sunna TC, Beyene J, Hossain A. Global and regional prevalence of multimorbidity in the adult population in community settings: a systematic review and meta-analysis. EClinicalMedicine. 2023;57: 57.
- Van Den Akker M, Buntinx F, Knottnerus JA. Comorbidity or multimorbidity: what’s in a name? A review of literature. Eur J Gen Pract. 1996;2(2):65–70. doi:10.3109/13814789609162146
- Gontijo Guerra S, Berbiche D, Vasiliadis H-M. Measuring multimorbidity in older adults: comparing different data sources. BMC Geriatr. 2019;19(1):166. doi:10.1186/s12877-019-1173-4
- Lin Y, Hu Y, Guo J, et al. Association between sleep and multimorbidity in Chinese elderly: results from the Chinese Longitudinal Healthy Longevity Survey (CLHLS). Sleep Med. 2022;98:1–8. doi:10.1016/j.sleep.2022.06.007
- Hunter ML, Knuiman MW, Musk B, et al. Prevalence and patterns of multimorbidity in Australian baby boomers: the Busselton healthy ageing study. BMC Public Health. 2021;21(1):1539. doi:10.1186/s12889-021-11578-y
- Walker V, Perret-Guillaume C, Kesse-Guyot E, et al. Effect of multimorbidity on health-related quality of life in adults aged 55 years or older: results from the SU. VI. MAX 2 cohort. PLoS One. 2016;11(12):e0169282. doi:10.1371/journal.pone.0169282
- Willadsen TG, Siersma V, Nicolaisdottir DR, et al. Symptom burden in multimorbidity: a population-based combined questionnaire and registry study from Denmark. BMJ open. 2021;11(4):e041877. doi:10.1136/bmjopen-2020-041877
- Malterud K, Guassora AD, Graungaard AH, Reventlow S. Understanding medical symptoms: a conceptual review and analysis. Theor Med Bioeth. 2015;36:411–424. doi:10.1007/s11017-015-9347-3
- Dorsey SG, Griffioen MA, Renn CL, et al. Working together to advance symptom science in the precision era. Nurs Res. 2019;68(2):86–90. doi:10.1097/nnr.0000000000000339
- Petrillo LA, Ritchie CS. The challenges of symptom management for patients with multimorbidity in research and practice: a thematic review. Prog Palliat Care. 2016;24(5):262–267. doi:10.1080/09699260.2016.1192320
- Vetrano DL, Calderón-Larrañaga A, Marengoni A, et al. An international perspective on chronic multimorbidity: approaching the elephant in the room. J Gerontol a Biol Sci Med Sci. 2018;73(10):1350–1356. doi:10.1093/gerona/glx178
- Chi WC, Wolff J, Greer R, Dy S. Multimorbidity and decision-making preferences among older adults. Anna Family Med. 2017;15(6):546–551. doi:10.1370/afm.2106
- Sera LC, McPherson ML. Pharmacokinetics and pharmacodynamic changes associated with aging and implications for drug therapy. Clin Med Geriatr. 2012;28(2):273–286. doi:10.1016/j.cger.2012.01.007
- Drenth-van Maanen AC, Wilting I, Jansen PAF. Prescribing medicines to older people-how to consider the impact of ageing on human organ and body functions. Br J Clin Pharmacol. 2020;86(10):1921–1930. doi:10.1111/bcp.14094
- Tripp-Reimer T, Williams JK, Gardner SE, et al. An integrated model of multimorbidity and symptom science. Nurs Outlook. 2020;68(4):430–439. doi:10.1016/j.outlook.2020.03.003
- Aromataris E, Fernandez RS, Godfrey C, Holly C, Khalil H, Tungpunkom P. Methodology for JBI umbrella reviews; 2014.
- Larson P, Carrieri-Kohlman V, Dodd M, et al. A model for symptom management. Image J Nurs Sch. 1994;26(4):272–276.
- Belbasis L, Bellou V, Ioannidis JPA. Conducting umbrella reviews. Br Med J. 2022;1(1):e000071. doi:10.1136/bmjmed-2021-000071
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.doi: 10.1136/bmj.n71
- Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13(3):132–140. doi:10.1097/xeb.0000000000000055
- Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Po. 2005;10(1_suppl):6–20. doi:10.1258/1355819054308576
- Crowe M, Jordan J, Burrell B, et al. Clinical effectiveness of transdiagnostic health management interventions for older people with multimorbidity: a quantitative systematic review. J Adv Nurs. 2016;72(10):2315–2329. doi:10.1111/jan.13011
- Kastner M, Cardoso R, Lai Y, et al. Effectiveness of interventions for managing multiple high-burden chronic diseases in older adults: a systematic review and meta-analysis. CMAJ. 2018;190(34):E1004–E1012. doi:10.1503/cmaj.171391
- Goehner A, Kricheldorff C, Bitzer EM. Trained volunteers to support chronically ill, multimorbid elderly between hospital and domesticity - a systematic review of one-on-one-intervention types, effects, and underlying training concepts. BMC Geriatr. 2019;19(1):126. doi:10.1186/s12877-019-1130-2
- Parker KJ, Hickman LD, Phillips JL, Ferguson C. Interventions to optimise transitional care coordination for older people living with dementia and concomitant multimorbidity and their caregivers: a systematic review. Contemp Nurse. 2020;56(5–6):505–533. doi:10.1080/10376178.2020.1812416
- Kennedy MA, Hatchell KE, DiMilia PR, et al. Community health worker interventions for older adults with complex health needs: a systematic review. J Am Geriatr Soc. 2021;69(6):1670–1682. doi:10.1111/jgs.17078
- Søgaard MB, Andresen K, Kristiansen M. Systematic review of patient-engagement interventions: potentials for enhancing person-centred care for older patients with multimorbidity. BMJ open. 2021;11(12):e048558. doi:10.1136/bmjopen-2020-048558
- Fortune N, Hardiker NR, Strudwick G. Embedding nursing interventions into the World Health Organization’s international classification of health interventions (ICHI). J Am Med Inf Assoc. 2017;24(4):722–728. doi:10.1093/jamia/ocw173
- Dodd S, Clarke M, Becker L, Mavergames C, Fish R, Williamson PR. A taxonomy has been developed for outcomes in medical research to help improve knowledge discovery. J Clin Epidemiol. 2018;96:84–92. doi:10.1016/j.jclinepi.2017.12.020
- Langmann E. Vulnerability, ageism, and health: is it helpful to label older adults as a vulnerable group in health care? Med Health Care Philos. 2023;26(1):133–142. doi:10.1007/s11019-022-10129-5
- Zhou Y, Dai X, Ni Y, et al. Interventions and management on multimorbidity: an overview of systematic reviews. Ageing Res Rev. 2023;87:101901. doi:10.1016/j.arr.2023.101901
- Johnston MC, Crilly M, Black C, Prescott GJ, Mercer SW. Defining and measuring multimorbidity: a systematic review of systematic reviews. European Journal of Public Health. 2019;29(1):182–189. doi:10.1093/eurpub/cky098
- Prince MJ, Wu F, Guo Y, et al. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385(9967):549–562. doi:10.1016/s0140-6736(14)61347-7
- Farmer C, Fenu E, O’Flynn N, Guthrie B. Clinical assessment and management of multimorbidity: summary of NICE guidance. BMJ. 2016;354. doi:10.1136/bmj.i4843
- Kastner M, Hayden L, Wong G, et al. Underlying mechanisms of complex interventions addressing the care of older adults with multimorbidity: a realist review. BMJ Open. 2019;9(4):e025009. doi:10.1136/bmjopen-2018-025009
- Lin J, Islam K, Leeder S, et al. Integrated care for multimorbidity population in Asian Countries: a scoping review. Int J Integr Care. 2022;22(1):22. doi:10.5334/ijic.6009
- Read JR, Sharpe L, Modini M, Dear BF. Multimorbidity and depression: a systematic review and meta-analysis. J Affective Disorders. 2017;221:36–46. doi:10.1016/j.jad.2017.06.009
- Wei MY, Mukamal KJ. Multimorbidity, mortality, and long-term physical functioning in 3 prospective cohorts of community-dwelling adults. American Journal of Epidemiology. 2018;187(1):103–112. doi:10.1093/aje/kwx198
- Makovski TT, Schmitz S, Zeegers MP, Stranges S, van den Akker M. Multimorbidity and quality of life: systematic literature review and meta-analysis. Ageing Res Rev. 2019;53:100903. doi:10.1016/j.arr.2019.04.005
- Fortin M, Bravo G, Hudon C, Lapointe L, Dubois M-F, Almirall J. Psychological distress and multimorbidity in primary care. Anna Family Med. 2006;4(5):417–422. doi:10.1370/afm.528
- Gapstur RL. Symptom burden: a concept analysis and implications for oncology nurses. Oncol Nurs Forum. 2007;34(3):673–680. doi:10.1188/07.Onf.673-680
- Portz JD, Kutner JS, Blatchford PJ, Ritchie CS. High symptom burden and low functional status in the setting of multimorbidity. J Am Geriatr Soc. 2017;65(10):2285–2289. doi:10.1111/jgs.15045