Abstract
Introduction
The complexity of healthcare is increasing, mainly due to the prevalence of multimorbidity in an ageing population. Complex care for patients with multimorbidity requires a multidisciplinary approach. Traditional physician-centered hospital structures do not facilitate the necessary multidisciplinary collaboration. European hospitals are implementing process-based hospital designs with patient- and process-oriented units to stimulate multidisciplinary collaboration. Patient-oriented units are formed based on shared patient groups and focus on care trajectories, while process-oriented units are formed based on having similar processes and focus on efficiency.
Purpose
This study has two aims. First, to study the effect of introduction of these units on multidisciplinary collaboration and perceived impact (efficiency, innovation, and effectiveness). Second, to study whether there are differences between patient- and process-oriented units.
Methods
A survey-based longitudinal evaluation study was conducted in 2020 and 2022 among physicians in a Dutch hospital to measure multidisciplinary collaboration (relational coordination) and perceived impact (efficiency, innovation, and effectiveness). In addition, open questions were used to enrich the data.
Results
Quantitative and qualitative data together suggest that physicians in patient-oriented units notice benefits from the redesign to multidisciplinary units, they perceive higher impact over time. Physicians in process-oriented units achieve a better relationship with the physicians in their unit over time, but they do not perceive impact as high as physicians in patient-oriented units.
Conclusion
A process-based design with patient- and process-oriented units is supportive of multidisciplinary collaboration and perceived impact, especially for physicians in patient-oriented units. Physicians in patient-oriented units are positive about the introduction of these units as they feel it contributes to better multidisciplinary patient care. As the results for physicians in process-oriented units may be less directly visible in terms of quality of care, they are less likely to see positive effects, even though their relationships are improving.
Introduction
Complexity of care has increased because of the high prevalence of multimorbidity in the aging population.Citation1–5 Organizational structures of hospitals have repeatedly been criticized for not being able to respond to the corresponding healthcare demands, due to their focus on medical specialties and their lack of integration.Citation6,Citation7 Steinmann et al even argue that current structures impede coordination between healthcare professionals, hamper efficiency, and are not suitable for the provision of patient-centered care.Citation8 Therefore, a redesign of organizational structures seems required to stimulate multidisciplinary collaboration which can be defined as: collaborative work with shared objectives and decision-making responsibilities in which physicians from different medical disciplines work together and address complexity by focusing multiple perspectives on a focused topic in a coordinated manner.Citation9,Citation10
However, other authors suggest that such a redesign may not be sufficient to guarantee an integrated and collaborative approach across medical disciplines.Citation11 Redesigns might support an integrated approach by creating opportunities for building relationships, communication, and coordination between medical disciplines, but it might also challenge clinical work and professional relationships by disrupting discipline-based interdisciplinary collaboration.Citation11
Traditionally hospitals have been physician-centered organizations, in which structures are built around medical specialties, so-called functional designs.Citation6,Citation12 Healthcare professionals with similar specialized skills, expertise, and knowledge are grouped together. These physician-centered organizations seem to facilitate contact and communication among physicians from the same medical discipline and thereby create efficiency.Citation6,Citation13 At the same time, functional designs do not seem to support collaboration and coordination between physicians from different medical disciplines, which is increasingly required.Citation8,Citation14 Therefore, in today’s hospitals we see reforms towards organizational structures around medical conditions, called process-based, thematic, or care focused designs.Citation7,Citation8,Citation15 Designs built around patients’ needs which group multiple specialties that play a role in a patients’ care trajectory.Citation7,Citation8,Citation12,Citation16 In general, process-based designs are expected to increase quality of care and improve patient-centredness.Citation2,Citation7,Citation13 However, as most hospitals are reluctant to radically redesign their structures, many hospitals currently combine functional and process-based designs by, for example, only introducing integrated practice units for specific care trajectories, such as oncology.Citation8,Citation15,Citation16
Internationally, there are few examples of hospitals opting for a fundamental redesign towards a process-based hospital. The Karolinska hospital is the most well-known example in Europe which completely redesigned their structure based on patient groups that had similar care pathways.Citation16 This resulted in the organization of care in seven themes (eg, cancer, heart and vascular, ageing, children’s and women’s health) with an addition of five functions (eg, emergency medicine, intensive care, radiology and imaging) that cut across the themes.Citation16 A similar example is seen in a Finnish hospital (Turku University Hospital) that restructured into eight care lines (eg, cardiac care, neurological care, children and adolescents) and organized the functions that cut across these care lines into shared service units (eg, pharmacy, emergency services, medical imaging).Citation17 Six of the introduced care lines in this Finnish hospital had a relatively restricted set of patients, while the other two were containers for treatment processes for which it was not medically or economically feasible to create single care lines.Citation17 In both examples, there are clearly two distinct units. On the one hand, there are structures based on patient groups, called themes and carelines. In these units, focus is placed on care trajectories (hereafter referred to as patient-oriented units). On the other hand, there are units that have similar processes, called functions and shared service units, in which focus is placed on increasing efficiency (hereafter referred to as process-oriented units). Organizational redesign intends to stimulate multidisciplinary collaboration, but empirical evidence is provided that by redesigning organizational structures also patient satisfaction and financial and operational outcomes can be improved.Citation18,Citation19 To date, empirical evidence is limited to organizational structures around strategically important patient groups. Differences that can be expected between patient-oriented and process-oriented units remain understudied.Citation8,Citation18 This study focuses on a Dutch hospital that (in line with the ideas of Karolinska and Turku University Hospital) has opted for a redesign, with patient- and process-oriented units.
New Contributions
Process-based designs are expected to facilitate multi-specialist cooperation by creating opportunities for dialogue, connection, and coordination between physicians.Citation6,Citation11,Citation12,Citation18 Furthermore, it is known that bringing together individuals from diverse backgrounds can help generate innovative ideas.Citation20,Citation21 However, different studies suggest that crossing boundaries between disciplines is not guaranteed even when the opportunities are explicitly provided, nor a fast and easy process.Citation11,Citation12,Citation18 Physicians encounter obstacles such as power imbalances, conflicting views on how clinical protocols should be followed, different perspectives on care (holistic versus specialized), and diverse role conceptions.Citation11 It is argued that these obstacles are encountered because of differing norms and values that are deeply rooted in professional identities and are difficult to change.Citation11 This study aims to longitudinally explore the effect of a process-based redesign on collaboration between physicians and their ability to improve patient care, with explicit interest in differences between patient-oriented and process-oriented units. There are two research questions proposed: (I) How will the formation of units around patients as well as processes affect (i) multi-specialist collaboration and (ii) the perceived impacts (efficiency, innovation, and effectiveness)? and (II) are there differences between patient- and process-oriented units?
Setting
This research was conducted in a Dutch, so-called, top-clinical hospital. In Dutch healthcare, there are three types of hospitals (general, top-clinical, university) that differ in the care they offer, their expertise, and whether they participate in academic research. A top-clinical hospital is characterized by its role as medical educator and by delivering more complex care and participation in more academic research than a general hospital, but less than a university medical hospital. Most physicians in top-clinical Dutch hospitals are independent, non-salaried workers. They are united in a medical specialist company (MSC), which has a partnership with the hospital. Together with the board of directors, they are responsible for reaching proper agreements about governance of the hospital and care to be provided.
According to previous research, Dutch hospitals are moving away from a structure based on medical specialties towards a more process-oriented design through the development of multi-specialty centers.Citation8,Citation15 In most hospitals, these changes especially concern specialisms in which the majority of patients suffer from comorbidities and multidisciplinary work is required (eg, oncology, mother and child). Most hospitals choose an incremental change process by stepwise introducing new centers instead of through radical redesign.Citation8,Citation15 The hospital in our study chose for radical redesign. In May 2019, the organizational structure was changed. The hospital embedded six accountable multidisciplinary units within its structure. Three of these units are based on patient groups, patient-oriented: mother and child; chronic care and frail elderly; oncology; the other three units are based on processes, process-oriented: acute care, planned care, and the diagnostic center. A physician working in the hospital is now part of their own medical specialty group and belongs to one of the six multidisciplinary units. Whereas in the past the focus was on medical specialty group silos, emphasis is now placed on the multidisciplinary units, which is reinforced by formal communication structures, economic accountability at unit level, and dual leadership (business manager and medical manager) at unit level. Physicians from the same medical specialty group may be embedded within different units. For example, a gastroenterologist may be subspecialized in chronic bowel diseases (eg, Crohn’s disease) and therefore be part of the chronic care and frail elderly unit, while another gastroenterologist is subspecialized in gastrointestinal cancer and therefore part of the oncology unit.
Methods
We conducted a longitudinal evaluation study of the effect of redesign on the collaboration between physicians and perceived impact, by measuring relational coordination and impact (efficiency, innovation, and effectiveness) and asking several open-ended questions. A survey was distributed among physicians at two time points. First, from October to December 2020 and second from October to December 2022. We invited all physicians, from medical specialist to first-year resident to participate (2020: n = 392, 2022: n = 391). Both times an invitation to participate in the survey and multiple reminders were sent via email, with a direct link to the survey. Because the 2020 survey had taught the researchers that response was below 22%, after several reminders and after also providing paper versions, the respondents in 2022 were rewarded with a voucher for a smoothie drink at the hospital canteen. Nevertheless, an extra incentive was needed at the end of 2022 to recruit respondents. Based on the successful experience in 2020, a raffle of bottles of champagne was used as additional incentive. In the data analysis, we included participants who had answered all items of the impact-scale and at least six out of seven items from the relational coordination Measurements.
We decided to conduct our first measurements after the redesign of the hospital structure took shape. Although the new hospital structure was introduced in May 2019, several delays in the process meant that the change did not take shape until the end of 2020. These delays in the process included the fact that the dual leadership positions had not yet been permanently filled. Some interim managers were put in place pending assessment, and it took up to six months to find the right person for the job. In addition, medical specialists installed as medical managers took up to three months to fit their management duties into their schedules. After the installation of these managers, surveys were planned, however then the first cases of COVID appeared in the Netherlands in March 2020. As COVID caused uncertainty, high workload, and pressure, the survey was postponed until the end of 2020. At that point, COVID was not yet gone, but the situation had been contained.
Measurements
In the survey, collaboration between physicians was assessed by the widely used relational coordination scale. Furthermore, items in the survey assessed perceived impact and demographics. The 2022 survey also included four open-ended questions to enhance the richness of the data. These questions focused on changes in collaboration after the hospitals’ redesign, the role of the medical specialist group, and potential recommendations to further improve multidisciplinary collaboration.
Relational Coordination
Relational coordination is a concept developed by Jody Hoffer Gittell, which provides an opportunity to map multidisciplinary collaboration.Citation22 According to the relational coordination concept, effective collaboration is determined by both positive relationships and coordinated interaction between physicians.Citation22 We used relational coordination as a measure of collaboration between physicians from the same medical specialty groups (eg, pediatrics, internal medicine) and between physicians from different medical specialties working together in a unit (in our study hospital, eg, oncology, acute care). The relational coordination survey is a recommended and frequently used tool in hospital settings for measuring quality of communication and relational ties between professionals.Citation23,Citation24 Relational coordination is defined as a “mutually reinforcing process of interaction between communication and relationships”. Relational coordination was measured using seven survey questions on a 5-point scale (1 = never, 2 = rarely, 3 = occasionally, 4 = mostly, 5 = all the time) at two different points in time (2020 and 2022). The survey has two subscales: a communication sub-scale consisting of four items about communication (frequency, timeliness, accuracy, problem-solving) and a relationship sub-scale consisting of three items about relationships (shared goals, shared knowledge, mutual respect).Citation23 The relational coordination scores were derived by calculating the mean score, either as a whole or at the level of the subscales. Higher scores indicate better relational coordination, indicating better communication and relational ties.Citation25,Citation26 Relational coordination has in previous studies shown a Cronbach’s alpha between 0.80 and 0.90.Citation25–27 In this study, we found Cronbach’s alpha for the relational coordination questionnaire of 0.92 in 2020 and 0.86 in 2022 for the full scale (7 items). The Cronbach’s alpha for the communication sub-scale was respectively 0.88 in 2020 and 0.77 in 2022 and for the relation sub-scale 0.86 and 0.77.
Perceived Impact
From an existing (sub-)scale of five items to assess the impact of multidisciplinary collaboration,Citation10 we used three items to assess the perceived impact of multidisciplinary collaboration. Although not officially labelled as, we refer to this as the impact-scale. The existing scale was developed for a research setting, which shifted from individually oriented towards team-based initiatives focusing on integration of disciplines. We believed this shift in the research setting is comparable to the shift taking place in healthcare. We used the items of the scale as a starting point for formulating a scale that assesses the impact of the team-based initiatives introduced in the studied hospital. We developed a three-item scale to assess the impact of multidisciplinary collaboration. Physicians are asked to evaluate the efficiency of multidisciplinary meetings, the ability of the unit to innovate across specialties, and the general effectiveness of the multidisciplinary unit on a 4-point scale (1 = poor, 2 = fair, 3 = good, 4 = excellent). The three items together provided a Cronbach’s alpha of 0.80 in 2020 and 0.71 in 2022.
Other Information
The physicians were also asked for some relevant additional information, namely, their gender, their medical specialty, the unit they belong to, their function (eg, medical specialist, resident), the number of years they work in the hospital (ranging from 1, <1 year, to 6, >21 years), and the number of years they work in their current position (ranging from 1, <1 year, to 6, >21 years). As responding to these questions might reveal respondents’ identity, an opt-out option was included to avoid dropouts. Furthermore, physicians were asked whether they agreed (ranging from 1, totally disagree to 5, totally agree) with two statements. The first statement was ‘I am satisfied with the collaboration between physicians from different specialties within the hospital’. In 2020, a second statement was presented implicitly referring to improvement after the introduction of the new unit structure: “Collaboration between physicians from different specialties within the hospital has improved in the past year”. In 2022, a second statement was presented explicitly referring to improvement after the introduction of the new unit structure: “Collaboration between physicians from different specialties within the hospital has improved since the introduction of units”.
Analysis
Data collected in a hospital setting might violate the assumption of independence of observations based on group structures (medical specialty group and/or unit), which might require multi-level analysis. As not all physicians from the same medical specialty were in our hospital nested within the same unit, a three-level multilevel analysis was not applicable. Therefore, we conducted the first analysis, the random intercept model, for two-level multilevel analyses with clustering at the level of the medical specialty group and the level of units. These analyses indicated that there were no between-group differences. Therefore, continuing with multilevel analysis was not appropriate and would make the analysis unnecessarily complicated.Citation28 Statistical analyses were performed with IBM SPSS Statistics version 27. Based on the small sample size and use of Likert-scales it was decided to use non-parametric techniques. Mann Whitney U-tests were performed to compare the process-oriented and patient-oriented units, in 2020 and in 2022, and to compare the results of 2020 and 2022. Furthermore, Wilcoxon Signed Rank tests were used to compare matched pairs over time (2020 and 2022). Finally, as no non-parametric alternative was available, we used mixed between-within subject ANOVAs to assess whether there were differences between patient-oriented and process-oriented units over time (2020 and 2022).
The qualitative data provided by the answers to the open-ended questions were inductively coded using a thematic analysis.Citation29 First, we familiarized ourselves with the available data by closely reading all the answers. Then, we divided the data into two groups, namely the answers from respondents in patient-oriented units and the answers from respondents in process-oriented units. Then for each group, open coding was used to analyze the answers to each question and identify themes. These themes and a comparison between the two groups were used to enhance the richness and interpretation of the quantitative data.
Ethics
The Ethics Review Board decided that our study was outside the scope of the Netherlands’ medical research involving human subjects act, especially as the study focused on professionals instead of patients (METC-LDD-2019-Z19.010). Respondents were informed of the purpose of the study and participation in the survey was entirely voluntary. Participants were informed and consented that their responses would be used in this study and could be published in an anonymized fashion, that all identifiable information would be removed to protect their privacy, and that responses would not be presented in a manner that could be traced back to any individual (informed consent).
Results
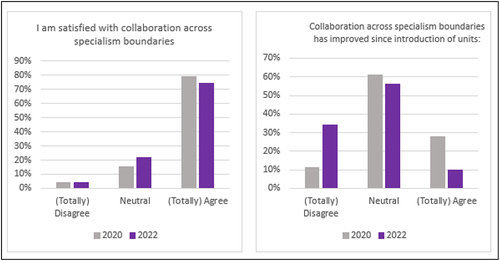
In 2020, 27% of the invited physicians responded to the survey (93/392), in 2022, 28% (109/391). Fifteen of the physicians that had responded to the survey in 2020 were no longer employed in the study hospital in 2022, leaving us with seventy-five physicians able to participate at both times. In total, thirty-four physicians participated in the survey both in 2020 and 2022. In 2022, more woman (n = 66, 61%) than men (n = 39, 36%) responded to the survey, while in 2020 an almost even number of woman (n = 45, 48%) and men (n = 43, 46%) responded. Most respondents in both years were medical specialists n = 73 (79%) and n = 85 (78%) in 2020 and 2022, respectively. For all descriptive information see Table S1. The histograms below (see ) shows the percentages of (all) respondents’ (2020: n = 93, 2022: n = 109) agreement with two statements, satisfaction with and improvement of collaboration across specialism boundaries. The left histogram shows that most respondents in both years are satisfied with collaboration across specialism boundaries (>70%). The right histogram shows that in 2020 a relatively small percentage of respondents (~10%) disagreed that the introduction of the units let to improvement, while almost 30% did agree on this matter. This changed in 2022, where only a small percentage of respondents (~10%) agreed that the introduction of the units let to improvement, while more than 30% disagreed on this matter.
Comparisons Between Patient-Oriented and Process-Oriented Units
Mann–Whitney U-tests were conducted to compare the patient-oriented and process-oriented units on relational coordination and the impact on the healthcare process (see ). In 2020, there were no differences between patient- and process-oriented units in relational coordination nor on the impact on the healthcare process. In 2022, nonsignificant differences between patient-oriented and process-oriented units were shown in relational coordination, but a Mann–Whitney U-test revealed a larger impact on the healthcare process of patient-oriented (Md = 2.67, n = 57) compared to process-oriented units (Md = 2.33, n = 47) units, U = 924, z = −2.77, p = 0.006, r = 0.27. This would be considered a small-to-medium effect size using Cohen’s (1988) criteria of 0.1 = small effect, 0.3 = medium effect, 0.5 = large effect.
Table 1 Comparisons Between Patient-Oriented and Process-Oriented Units
Comparisons Between 2020 and 2022
Responses from 2020 to 2022 were compared using Mann–Whitney U-tests (see ). Only one significant difference between 2020 and 2022 was shown. The relationships between physicians from the same medical specialty group scored better in 2022 (Md = 4.67, n = 104) than in 2020 (Md = 4.33, n = 93), U = 5931, z = 2.75, p = 0.006, r = 0.19.
Table 2 Comparisons Between 2020 and 2022
In addition, analyses were conducted to compare responses from 2020 to 2022 separately for patient-oriented and process-oriented units (see ). For patient-oriented units, no significant differences between 2020 and 2022 were shown. For process-oriented units, two significant differences were shown. First, the relationship scores between physicians from the same medical specialty group increased from 2020 (Md = 4.33, n = 39) to 2022 (Md = 4.67, n = 47), U = 1195, z = 2.49, p = 0.013, r = 0.27. Second, the relationship scores between physicians from different medical specialties increased from 2020 (Md = 3.83, n = 40) to 2022 (Md = 4.00, n = 45), U = 1159, z = 2.33, p = 0.020, r = 0.24.
Paired Comparisons
Only for a small sample (n = 34) data at two time points were available, for which Wilcoxon Signed Rank tests were performed (see ). These Wilcoxon Matched Pairs Signed Rank Tests revealed only one statistically significant change from 2020 to 2022. The Wilcoxon Signed Rank Test revealed a statistically significant improvement of the relationship between physicians from different medical specialties, z = 2.25, n = 30, p = 0.024, with a medium effect size (r = 0.41). While the median scores on the relationship sub-scale of relational coordination are equal to 2020 (Md = 4.00) and 2022 (Md = 4.00), suggesting that there is a significant difference in the distribution of paired observations but not in the central tendency (median).
Table 3 Wilcoxon Matched Pairs Signed Rank Tests
In addition, as no non-parametric test is available,Citation30 we performed mixed between-within subject ANOVAs to tell whether the change over time is different for patient-oriented compared to process-oriented units (interaction effect) on participants’ scores for relational coordination and perceived impact (see ). For participants’ scores on perceived impact, there was a significant interaction between unit-base and time, Wilks’ Lambda = 0.88, F (1, 32) = 4.26, p = 0.047, partial eta squared = 0.12. The plotted results (see Figure S1) show an increase from 2020 to 2022 for patient-oriented units, but a decrease from 2020 to 2022 for process-oriented units. The other analysis revealed a similar picture to the Wilcoxon Matched Pairs Signed Rank tests, with no significant interaction effects, and only a substantial main effect of time for the relationship between physicians from different specialties within the same unit, Wilks’ Lambda = 0.80, F (1, 28) = 6.88, p = 0.014, partial eta squared = 0.20.
Table 4 Scores for the Patient-Oriented and Process-Oriented Units at Two Points in Time
Qualitative Results
In 2022, respondents were also asked four open-ended questions. Sixty-five respondents (40 from patient-oriented units and 25 from process-oriented units) answered these questions. Several topics emerge from their answers. These provide insights into the changes following the implementation of the new organizational structure. Although at first sight there are many similarities in the answers given by respondents, a closer examination reveals differences between physicians from patient- and process-oriented units. Most importantly, the qualitative results provide more nuance and context for interpreting and discussing the survey results.
Changes in Cross-Specialty Collaboration
Positive and negative changes in the collaboration between physicians from different specialties after the introduction of the new units are mentioned by the respondents. Positive changes mentioned relate to shared responsibility, having a common goal, and more cross-specialism meetings. In contrast, other respondents claim that they are spending more time on cross-specialism meetings that do not bring many benefits. In their view, although consultation structures have changed, this did not affect their day-to-day patient care practice much, nor did it lead to improved integration.
Some respondents also suggest that collaboration is not necessarily linked to the organizational structure. Collaboration with physicians from some specialisms goes well, while collaboration with other specialisms is difficult, independent of the prevailing structure.
As an oncologist, you are constantly working with all the other medical specialists involved with patients with oncologic conditions, and this is reflected in all daily multidisciplinary consultations we have with all these involved colleagues. Respondent from a patient-oriented group
With some specialties cooperation goes very well, with others less so. Respondent from a process-oriented group
Physicians from patient-oriented units seem mostly positive about the changes made but they see room for improvement. They mention that some specialties are assigned to units where they do not fit that well, while others are assigned to a specific unit, while they mostly work across units. In contrast, respondents from process-oriented units that responded to the open questions seem mostly negative, and even frustrated. They state that they are not being heard enough by management and that decision-making power is misallocated. Some even experience the changes as an intervention designed by management without really listening to what is needed in practice.
Regarding the units, which is a variation on a theme and in my opinion that has nothing to do with whether you work together more efficiently or not, that is again typical managerial thinking. Respondent from a process-oriented group
Role of the Medical Specialty Group
In the former hospital design, the medical specialty groups played a vital role. In the new design that role might change as the structure is no longer built around medical specialties. Only a few respondents see a clearly different role for medical specialty groups in the future and suggest that the current role inhibits multidisciplinary collaboration. However, these respondents do not define what the new role would be, or how it should be reached. Especially, respondents from the process-oriented units emphasize the fact that the medical specialty group is nowadays still the most important entity in the provision of care.
The role of the medical specialty group must remain! It is the entity for solving organizational problems as well as problems related to medical content in daily work. By remaining organized as a medical specialty group, there is also a good possibility to maintain different expertise within a specialty group. Respondent from a process-oriented group
Similar but more nuanced, respondents from the patient-oriented units emphasize the practical necessity of the medical specialty group for quality reviews, education, planning, and connection.
It is good to organize care around the patient. As a result, as a caregiver, you may have more contact with colleagues from the care team than with your colleagues from the specialty group. We are not yet ready to abolish the medical specialty group. Things like schedules, vacations, and shifts are arranged through the medical specialty group. But things around patient care such as protocols, processes, care paths must be arranged by the care team. And that is sometimes quite difficult and takes time, needs to be made time for. Respondent from a patient-oriented group
Improving Cross Specialty Collaboration
While general respondents seem satisfied with the collaboration between different specialties, they do offer suggestions for improvement. They especially stress that culture (eg, implicit hierarchy) and underlying structures (eg, quality and education) must change to truly focus on multidisciplinarity. Physicians see opportunities for improving collaboration by strengthening the relationship between different specialties and creating greater mutual understanding, for example, by doing team-building activities or participating in a shift of another specialty. In general, to improve multidisciplinarity respondents feel that the voice of physicians is paramount and there should be more room for medical leadership. The professionals on the work floor need to be heard as they play a key role in change.
Improving mutual understanding, eg by looking at each other in practice. Respondent from a process-oriented group.
Reducing the current tensions between management and medical staff, sometimes a bit of give and take, dialogue rather than Discussion, will help to free up energy and time for inter-physician collaboration. Respondent from a patient-oriented group.
Discussion
Internationally, a shift is seen from hospitals organized around specialties towards more process-based hospitals, focusing on patient groups.Citation7,Citation8,Citation15 Two distinct types of units can be distinguished within these process-based hospitals, namely patient-oriented and process-oriented units. With the current study, we aimed to generate insights about the effect of the introduction of patient-oriented and process-oriented units on multi-specialist collaboration and impact (effectiveness, efficiency, and innovativeness). The results of our study as discussed below should be interpreted with caution. First, because the study included only one hospital and only 100 physicians per wave. Second, we only look at collaboration from the physicians’ point of view.
The qualitative data suggest that mostly physicians in patient-oriented units perceive benefits from an organization based on multidisciplinary units. The quantitative results provided some support, but we did not find that the relationships with physicians from other specialties improved over time. This might be related to the fact that these physicians already worked together intensively.Citation19 However, the qualitative results show that these physicians do acknowledge the relevance of the structural changes. Furthermore, they also experience a greater perceived impact (in 2022) than physicians in process-oriented units. In the patient-oriented units, physicians from different medical disciplines are grouped together around the patients they treat (eg, oncology).Citation11,Citation13 As this involves primarily patients that require a multidisciplinary approach, the direct relevance of the new structure for improving quality of care seems clear.Citation30 Therefore, these changes are very much in line with physicians’ professional logics and interests.Citation31,Citation32
In contrast, physicians in process-oriented units did experience better relationships with physicians from other specialties, as is shown by the quantitative results. In addition, there is an indication that the relationship with physicians from their own specialty group also improved. However, that did not result in more perceived impact. Also, physicians from process-oriented units noticed few changes since the introduction of the new structure and emphasize that they now spend more time on meetings that bring no immediate benefits (qualitative results). In the process-oriented units, different medical specialties are grouped together because they are part of similar processes and share resources (eg, acute care, planned care).Citation12,Citation13 These structures cater more directly to managerial logics and interests related to efficiency, then to professional logics related to quality of care.Citation33 In our view, this could possibly explain differences in perceived impact and experienced relevance. In patient-oriented units, there is a clear opportunity to improve multidisciplinary care (make impact), while in process-oriented units quality of care might not necessarily improve, despite more coordination (improved relationships with other specialties) on better use of resources.Citation30
The qualitative results of this study also show that despite the need for multi-specialty integration of care, respondents still see a significant role for the medical specialty group. The medical specialism is still a delineated group that is important for education and training, assessment of quality, specialization, research, and division of work. Through historical practices and patterns physicians’ professional identities have also largely been shaped around their medical disciplines.Citation33 Many authors agree that these professional identities need to change or expand to support multidisciplinary collaboration. Some authors suggest that dissolving the medical specialty group is required for this.Citation19,Citation33 Others suggest that medical specialty group can be maintained and serve as solid foundation while opening up to organizational logics of multidisciplinarity.Citation34–36
A final important nuance raised by the respondents is that multi-disciplinary cooperation is not only dependent on the prevailing structure but also on existing interprofessional relationships. In our earlier studies, we suggested that professional domains and autonomy are of influence.Citation37,Citation38 Especially when professional domains (partly) overlap, multidisciplinarity can result in a complex situation where professionals experience competition.Citation32 Rivalry might emerge from shortages in healthcare personnel and resources, domain conflicts, as well as from unclarity about who is accountable, unpredictability of the situation, or lack of common understanding.Citation32,Citation39 In summary, it seems that the intrinsic factor of improving quality of care for multimorbid patients drives physicians towards multidisciplinary collaboration, but external factors such as resources and incentives lead to competition.
Limitations
The study presented has its shortcomings, and findings must be interpreted with caution. First, we need to recognize that we compare data collected in 2020 and 2022. In the meantime, there has been a pandemic that has put excessive pressure on healthcare. Other researchers found the pandemic to have a positive effect on interdisciplinary collaboration across departmental boundaries.Citation40,Citation41 This might have biased our results. Second, despite trying to take into account the limited time of our respondents by limiting the number of questions in the questionnaire, reaching out to them multiple times, and rewarding participation we are dealing with response rates of 27% (in 2020) and 28% (in 2022), and a sample of n = 34 respondents that participated both in 2020 and 2022. Therefore, our results might not reflect all physicians and decrease generalizability. Despite the small sample, our sample represents a variety of medical specialties, units, experience on the job, and gender representing the diversity of the physician workforce within a hospital. In addition, the average response rate among physicians is known to be lower than in other target groups.Citation42 The trade-off between questionnaire length and the use of validated items resulted in the use of a relatively small number of items to measure perceived impact. Although impact has not been measured in this way before, it presents an acceptable Cronbach's alpha within this study. In addition, to enhance interpretation of the results, open-ended responses were used.Citation43,Citation44 These responses provide the opportunity to uncover more sensitivities and enrich the interpretation.Citation45 Despite the limitations and recommendations for future research, the strength of this study is that it contributes to current scientific and practical debates on integration in healthcare and reveals relevant insights on collaboration between physicians from different medical disciplines.
Despite the added value of this study, the debate on integration of care and restructuring is broader than collaboration between physicians and offers opportunities for future research on how restructuring within a hospital is embedded in the wider healthcare system. For example, will redesign of a hospital affect its connection with primary care institutions, will it lead to different reimbursement of physicians, how will it affect competition within and across hospitals, and what can medical schools do to prepare students to work in these new structures.
Conclusion
The introduction of patient-oriented units (based on shared patient groups, focus on care trajectories) and process-oriented units (based on similar processes, focus on efficiency) has impact and influences inter-physician collaboration. Patient-oriented units are perceived positively by physicians, especially in terms of improving multidisciplinary care for complex patients. In contrast, process-oriented units show improvements in relationships between physicians but may not necessarily have an impact multidisciplinary care. In addition, while emphasizing the need for multidisciplinary collaboration, this study highlights the importance of the medical specialty group, which should be seen as a necessary condition for education and training purposes. However, given the limitations of the study, including the relatively small sample size and research in one single center, the results should be interpreted with caution.
Disclosure
The authors report no conflicts of interest in this work.
References
- van Oostrom SH, Picavet HSJ, van Gelder BM, et al. Multimorbidity and comorbidity in the Dutch population – data from general practices. BMC Public Health. 2012;12(1):715. doi:10.1186/1471-2458-12-715
- Moffat K, Mercer SW. Challenges of managing people with multimorbidity in today’s healthcare systems. BMC Fam Pract. 2015;16(1):129. doi:10.1186/s12875-015-0344-4
- Van Merode T, Van De Ven K, Van Den Akker M. Patients with multimorbidity and their treatment burden in different daily life domains: a qualitative study in primary care in the Netherlands and Belgium. J Comorb. 2018;8(1):9–15. doi:10.15256/joc.2018.8.119
- Koné Pefoyo AJ, Bronskill SE, Gruneir A, et al. The increasing burden and complexity of multimorbidity. BMC Public Health. 2015;15(1):415. doi:10.1186/s12889-015-1733-2
- Zulman DM, Asch SM, Martins SB, Kerr EA, Hoffman BB, Goldstein MK. Quality of care for patients with multiple chronic conditions: the role of comorbidity interrelatedness. J Gen Intern Med. 2014;29(3):529–537. doi:10.1007/s11606-013-2616-9
- Lega F, DePietro C. Converging patterns in hospital organization: beyond the professional bureaucracy. Health Policy. 2005;74(3):261–281. doi:10.1016/j.healthpol.2005.01.010
- Vera A, Kuntz L. Process-based organization design and hospital efficiency. Health Care Manage Rev. 2007;32(1):55–65. doi:10.1097/00004010-200701000-00008
- Steinmann G, Daniels K, Mieris F, Delnoij D, Bovenkamp H VD, van der Nat P. Redesigning value-based hospital structures: a qualitative study on value-based health care in the Netherlands. BMC Health Serv Res. 2022;22(1):1193. doi:10.1186/s12913-022-08564-4
- Petri L. Concept Analysis of Interdisciplinary Collaboration. Nurs Forum. 2010;45(2):73–82. doi:10.1111/j.1744-6198.2010.00167.x
- Mâsse LC, Moser RP, Stokols D, et al. Measuring Collaboration and Transdisciplinary Integration in Team Science. Am J Prev Med. 2008;35(2):S151–S160. doi:10.1016/j.amepre.2008.05.020
- Liberati EG, Gorli M, Scaratti G. Invisible walls within multidisciplinary teams: disciplinary boundaries and their effects on integrated care. Soc Sci Med. 2016;150:31–39. doi:10.1016/j.socscimed.2015.12.002
- Villa S, Barbieri M, Lega F. Restructuring patient flow logistics around patient care needs: implications and practicalities from three critical cases. Health Care Manag Sci. 2009;12(2):155–165. doi:10.1007/s10729-008-9091-6
- Fiorio CV, Gorli M, Verzillo S. Evaluating organizational change in health care: the patient-centered hospital model. BMC Health Serv Res. 2018;18(1):95. doi:10.1186/s12913-018-2877-4
- Clark JR. Comorbidity and the limitations of volume and focus as organizing principles. Med Care Res Rev. 2012;69(1):83–102. doi:10.1177/1077558711418520
- van Wijngaarden JDH, Braam A, Buljac-Samardžić M, Hilders CGJM. Towards process-oriented hospital structures; drivers behind the development of hospital designs. Int J Environ Res Public Health. 2023;20(3):1993. doi:10.3390/ijerph20031993
- Wise J. Melvin Samsom: rebuilding hospitals for patients. BMJ. 2017;j2088. doi:10.1136/bmj.j2088
- Suomi R, Müller O, Vom Brocke J. Hospital-wide process-oriented organization of care: the case of turku university central hospital. J Inform Tech the Appl. 2018;19(4):32–54.
- Vos L, Chalmers SE, Dückers M LA, Groenewegen PP, Wagner C, van Merode GG. Towards an organisation-wide process-oriented organisation of care: a literature review. Implement Sci. 2011;6(1):8. doi:10.1186/1748-5908-6-8
- Elrod JK, Fortenberry JL. Centers of excellence in healthcare institutions: what they are and how to assemble them. BMC Health Serv Res. 2017;17(S1):425. doi:10.1186/s12913-017-2340-y
- Gomez LE, Bernet P. Diversity improves performance and outcomes. J Natl Med Assoc. 2019;111(4):383–392. doi:10.1016/j.jnma.2019.01.006
- Johnson A, Nguyen H, Groth M, White L. Reaping the Rewards of Functional Diversity in Healthcare Teams: why Team Processes Improve Performance. Group Organ Manag. 2018;43(3):440–474. doi:10.1177/1059601118769192
- Gittell JH. Relational perspectives in organizational studies: A research companion. In: Relational Coordination: Coordinating Work Through Relationships of Shared Goals, Shared Knowledge and Mutual Respect. Edward Elgar Publishing Ltd.; 2006:74–94.
- Hustoft M, Hetlevik Ø, Aßmus J, Størkson S, Gjesdal S, Biringer E. Communication and relational ties in inter-professional teams in Norwegian specialized health care: A multicentre study of relational Coordination. Int J Integr Care. 2018;18(2):9. doi:10.5334/ijic.3432
- Valentine MA, Nembhard IM, Edmondson AC. Measuring teamwork in health care settings: a review of survey instruments. Med Care. 2015;53(4):e16–30. doi:10.1097/MLR.0b013e31827feef6
- Gittell JH, Weinberg D, Pfefferle S, Bishop C. Impact of relational coordination on job satisfaction and quality outcomes: a study of nursing homes. Human Res Manag J. 2008;18(2):154–170. doi:10.1111/j.1748-8583.2007.00063.x
- Gittell JH. Relational coordination: guidelines for theory, measurement and analysis. Waltham MA. 2011;1:1.
- Gittell JH, Logan C, Cronenwett J, et al. Impact of relational coordination on staff and patient outcomes in outpatient surgical clinics. Health Care Manage Rev. 2020;45(1):12–20. doi:10.1097/HMR.0000000000000192
- Heck RH, Thomas SL, Tabata LN. Multilevel and Longitudinal Modeling with IBM SPSS. Routledge, Taylor & Francis Group; 2014.
- Khokhar S, Pathan H, Raheem A, Abbasi AM. Theory Development in Thematic Analysis: procedure and Practice. Revi Appl Manage Social Scie. 2020;3(3):423–433. doi:10.47067/ramss.v3i3.79
- Pallant J. SPSS Survival Manual. A Step by Step Guide to Data Analysis Using IBM SPSS. Routledge; 2020.
- Andersson T, Liff R. Co-optation as a response to competing institutional logics: professionals and managers in healthcare. J Profes Organ. 2018;5(2):71–87. doi:10.1093/jpo/joy001
- Albert-Cromarias A, Dos Santos C. Coopetition in healthcare: heresy or reality? An exploration of felt outcomes at an intra-organizational level. Soc Sci Med. 2020;252:112938. doi:10.1016/j.socscimed.2020.112938
- Kyratsis Y, Atun R, Phillips N, Tracey P, George G. Health systems in transition: professional identity work in the context of shifting institutional logics. Acad Manage J. 2017;60(2):610–641. doi:10.5465/amj.2013.0684
- Noordegraaf M. Reconfiguring Professional Work. Adm Soc. 2016;48(7):783–810. doi:10.1177/0095399713509242
- Noordegraaf M. Protective or connective professionalism? How connected professionals can (still) act as autonomous and authoritative experts. J Profes Organ. 2020;7(2):205–223. doi:10.1093/jpo/joaa011
- Braam A, van Wijngaarden JDH, Vollmann M, CGJM H, Buljac-Samardžić M, Cola PA. Clinical leaders crossing boundaries: a study on the role of clinical leadership in crossing boundaries between specialties. PLoS One. 2023;18(11):e0294264. doi:10.1371/journal.pone.0294264
- Nugus P, Greenfield D, Travaglia J, Westbrook J, Braithwaite J. How and where clinicians exercise power: interprofessional relations in health care. Soc Sci Med. 2010;71(5):898–909. doi:10.1016/j.socscimed.2010.05.029
- Powell AE, Davies HTO. The struggle to improve patient care in the face of professional boundaries. Soc Sci Med. 2012;75(5):807–814. doi:10.1016/j.socscimed.2012.03.049
- Prætorius T, Becker MC. How to achieve care coordination inside health care organizations: insights from organization theory on coordination in theory and in action. Int J Care Coord. 2015;18(4):85–92. doi:10.1177/2053434516634115
- Hiller M, Bracht H, Schroeder S. One year with the COVID-19 pandemic − Lessons learnt? Intersectoral collaboration measures established during the crisis could benefit capacity and patient flow management in daily clinical practice. J Health Organ Manag. 2022;36(2):141–148. doi:10.1108/JHOM-06-2021-0211
- Matusov Y, Matthews A, Rue M, Sheffield L, Pedraza IF. Perception of interdisciplinary collaboration between ICU nurses and resident physicians during the COVID-19 pandemic. J Interprof Educ Pract. 2022;27:100501. doi:10.1016/j.xjep.2022.100501
- Drees C, Krevers B, Ekerstad N, et al. Clinical Priority Setting and Decision-Making in Sweden: a Cross-sectional Survey Among Physicians. Int J Health Policy Manag. 2021. doi:10.34172/ijhpm.2021.16
- Semyonov-Tal K, Lewin-Epstein N. The importance of combining open-ended and closed-ended questions when conducting patient satisfaction surveys in hospitals. Health Policy Open. 2021;2:100033. doi:10.1016/j.hpopen.2021.100033
- Harland N, Holey E. Including open-ended questions in quantitative questionnaires—theory and practice. Int J Ther Rehabil. 2011;18(9):482–486. doi:10.12968/ijtr.2011.18.9.482
- Riiskjaer E, Ammentorp J, Kofoed PE. The value of open-ended questions in surveys on patient experience: number of comments and perceived usefulness from a hospital perspective. Int J Qual Health Care. 2012;24(5):509–516. doi:10.1093/intqhc/mzs039