Abstract
Lower extremity peripheral artery disease (PAD) is a common atherosclerotic cardiovascular disease (ASCVD) involving the aortoiliac, femoropopliteal, and infrapopliteal arterial segments. PAD remains a largely underdiagnosed and undertreated condition. The ankle-brachial index (ABI) is a simple and widely available test that is key detection tool in the diagnosis of PAD and is prognostic for mortality and morbidity. The cardiovascular (CV) team is a diverse array of health care clinicians (eg, nurses, nurse practitioners, physician assistants/associates, pharmacists, podiatrists) who have the qualifications and skills to be able to recognize when patients are at risk for PAD and perform an ABI. It is critical that the healthcare community recognize the critical role the CV team could play in improving outcomes and reducing disparities for patients with PAD.
Introduction
An estimated 8–10 million adults in the United States (US) over 40 years-old are diagnosed with PAD.Citation1–5 Lower extremity peripheral artery disease (PAD) is a common atherosclerotic cardiovascular disease (ASCVD) involving the aortoiliac, femoropopliteal, and infrapopliteal arterial segments. While several non-atherosclerotic etiologies of PAD exist (eg, vasculitis, entrapment syndrome, cystic adventitial disease), overwhelmingly atherosclerotic PAD is most common. Multi-disciplinary care is a hallmark of PAD management, including both medical and surgical specialties along with the cardiovascular (CV) team (Central Figure). Unfortunately, PAD remains an underdiagnosed and undertreated condition associated with significant morbidity and mortality that could be prevented with early detection and initiation of medical therapies. The aim of this work is to outline and leverage the role of the CV team in the diagnosis of PAD.
Peripheral Artery Disease Awareness
The ankle-brachial index (ABI) is a simple, noninvasive measure of systolic blood pressures at different levels of the arms and legs in the supine position using a Doppler device and is a key detection tool in the diagnosis of PAD.Citation6 In a meta-analysis of ~48,000 individuals in the US, an ABI ≤ 0.9 was associated with triple the risk of all-cause death compared with ABIs of 1.11–1.40.Citation7,Citation8
The relative morbidity, mortality, and quality of life impact associated with PAD present a significant burden of disease and associated strain on the healthcare system. Unfortunately, population- and clinician-level awareness of PAD, associated complications, and optimal medical therapy (eg, antiplatelet, statin) remain historically low.Citation1,Citation9–12 Surveys of primary care practices have demonstrated low identification of PAD despite low ABI results.Citation9,Citation12 This results in less use of optimal medical therapy and involvement of the CV team, despite guidelines demonstrating improved outcomes with early medical optimization.Citation6 As a result, patients often adjust their lifestyle to avoid or manage symptoms, in comparison to coronary artery disease.Citation11
PAD Amongst High-Risk Populations
Guidelines recommend ABI testing to establish the diagnosis of PAD in patients with history of physical exam findings suggestive of PAD. This includes patients with claudication, nonjoint-related exertional lower extremity symptoms, ischemic rest pain, history of lower extremity ulcers, or erectile dysfunction.
PAD prevalence is similar between sexes. However, an aging population whose life expectancy is longer in women as compared to men, the burden of disease disproportionately impacts women in the US aged ≥40. When women experience PAD, they are more likely to have atypical symptoms and less likely to have ideal cardiovascular health. As a result, they experience worse outcomes even after revascularization, likely because of delayed diagnosis and undertreatment of medical risk factors.Citation13
Health disparities or preventable differences are also noted by one’s race and ethnicity. Non-Hispanic Black adults have the greatest risk of PAD while Hispanic adults have the same, if not slightly lower, rate of PAD compared with their non-Hispanic White counterparts. This similar-to-lower rate of PAD among Hispanic adults is somewhat counterintuitive given the higher prevalence of risk factors that lead to PAD, particularly diabetes.Citation1 First and foremost, it is important to highlight that the concept of race and ethnicity is a social construct, not rooted in biology, and but governed by inequities in society as a factor of the social determinants of health (SDOH).Citation14 Therefore, excess PAD prevalence among Black people cannot be explained by traditional risk factors alone. As Black Americans, they are not only more likely to have PAD than other racial and ethnic groups, but tend to present with more severe disease, have more atypical symptoms, and are more likely to suffer worse outcomes. Specifically, they less often undergo limb salvage therapy and more often are referred for limb amputation and thus are more likely to die from major CV events.Citation14,Citation15
Detection and Diagnosis
PAD is often asymptomatic in mild cases, becoming more symptomatic with progression to moderate or severe. Through a careful history and physical (H&P) examination, signs and symptoms of PAD can be detected as well as risk factors outlined in the guidelines ().Citation6
Table 1 Pertinent Questions When Detecting for Peripheral Artery Disease
After the H&P exam, diagnostic studies can be ordered to provide quantifiable evidence of PAD. Arterial physiologic testing is a great tool to aid the diagnosis, providing a clear objective evaluation. Testing is also useful in the determination of the extent of arterial disease ().Citation16
Table 2 Peripheral Artery Disease Testing ModalitiesCitation6,Citation16–22
Cardiovascular Team in Disease State Management
A key strategy in addressing health inequity related to PAD detection is engagement of the CV team ().Citation23,Citation24 Within the realm of PAD, multiple members of the team are capable to assist in PAD diagnosis.Citation6,Citation19,Citation23–31 Specifically, the American Heart Association (AHA) states that ABI testing should be performed by qualified individuals through the following principles.1) Measurement and interpretation of the ABI should be within standard curriculum for medical and nursing students, and 2) all allied health professionals, beyond nursing and physicians, who perform the ABI should have didactic and experiential learning under a qualified healthcare professional to perform the ABI.Citation32 In the team-based model, having multiple members of the team who can perform or recommend an ABI, throughout the care continuum, expands accessibility for PAD detection with potential to increase diagnosis and management.
Table 3 The Various Roles of the Cardiovascular Team in the Detection & Diagnosis of Peripheral Artery Disease
The role of the CV team in PAD diagnosis, with a focus on recommending, ordering, and interpreting ABI testing, can occur in three settings: 1) inpatient 2) outpatient 3) community (). In terms of inpatient, all members of the CV team should assess patients for PAD risk to determine the need for diagnostic testing and/or follow-up as outlined in the ACC/AHA guideline on the management of lower extremity of PAD.Citation6,17 Patients admitted to the hospital are seen by various members of the CV team who have the capability of performing an assessment and coordinating follow-up including allied professionals with a specialized training to assist with assessment, diagnosis, and transition of care management. Advanced practice clinicians bring a high-level, advanced CV skills in accordance with the minimum competencies set by CV organizations.Citation29 Pharmacists within these CV specialties obtain post-graduate specialty residency accreditation, board certification, and provide direct care through comprehensive medication management.Citation31
Figure 1 The Collaboration of Cardiovascular Team Members for Peripheral Artery Disease Management at Each Phase of Care.
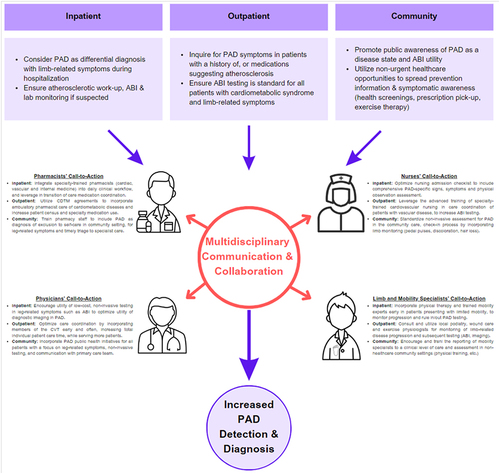
In the outpatient setting, there are a multitude of clinicians in various locations that should be engaged in PAD assessment and ABI testing. A policy for CV team involvement in PAD diagnosis should include outlining the assurance of competency, outlining roles and expectations, and process for ordering specific testing or collaborative management protocols (recommending supervised exercise therapy, initiating pharmacotherapy, tobacco cessation).Citation29,Citation31 Beyond the traditional clinic space, there are numerous other sites with CV team members that should be engaged in PAD detection and diagnosis. Often patients who are referred to wound care clinics may have foot-related ulcer and undiagnosed PAD.Citation19 Exercise physiologists are engaged with patients enrolled in workout programs.Citation19 In these programs and clinics, signs and symptoms of PAD are noticed and ABI testing ordered. Lastly, an even more underutilized resource are pharmacists who exist both in clinics and community-based pharmacies. Pharmacists, one of the most accessible healthcare clinicians, are in a unique position to increase detection and implement treatment for PAD.Citation33 The training of these accessible professionals to identify PAD symptoms and risk factors, and then mitigate ABI referrals has been proven to be effective and should be expanded upon.Citation33 CV team members offer an effective and cost-conscious approach to improving PAD diagnosis and treatment for this highly morbid and under-treated condition.
Lastly, all members of the CVT should be engaged in community outreach. When healthcare access is improved for patients within their own communities, diagnosis and management improves.Citation34,Citation35 Having trained, competent-based healthcare clinics working with trusted members of varying communities to provide detection should be best practice. CV team members should be instrumental in increasing access to ABI testing in a wide range of clinical settings.
While the importance of having a diverse array of clinicians who are competent in detection and/or diagnosis, the additional benefit of CV team engagement in the management of PAD should be acknowledged. Within the cardiovascular realm, there are exhaustive examples of how team-based care improves outcomes, patient satisfaction, and reduces clinician burnout.Citation25 The utility of the various CV team members’ knowledge base may allow for better navigation through resources for patients to obtain treatment, address barriers, and provide detailed education. As such, the detection, identification, and management of PAD patients should be incorporated early into the various healthcare curricular programs.
Conclusion
CV team members could improve the diagnosis and medical management of PAD patients. Given the heterogeneous nature of CV team roles, specific opportunities to improve PAD diagnosis and treatment will differ between clinician and within each system. Nonetheless, we should empower CV team members to 1) recognize patients with risk factors, signs, and symptoms of PAD; 2) facilitate early diagnostic testing for PAD; and 3) discuss appropriate medical management with their clinical colleagues. PAD awareness, detection and management should be an emphasis in the training of all CV team members. For vulnerable populations to underdiagnosis and undertreatment, leveraging each CV team member to assist with diagnosis and medical management of PAD is paramount.
Society Endorsements
The following organizations have reviewed and endorsed this document, recognizing the critical role of the cardiovascular team in peripheral artery disease detection and diagnosis. Furthermore, they believe that the involvement of multidisciplinary CV team members including nurses, pharmacists, and advanced practice providers will lead to improved outcomes and reduced disparities for patients with PAD:
American Association of Colleges of Pharmacy
American College of Cardiology Cardiovascular Team Section
American College of Clinical Pharmacy Cardiology Practice and Research Network
Anticoagulation Forum
Society for Vascular Medicine
Society for Vascular Nursing.
Disclosure
Dr Barnes provides consulting for Pfizer, Bristol-Meyers Squibb, Janssen, Bayer, Boston Scientific, AstraZeneca, Sanofi, Anthos, Abbot Vascular and serves on the Board of Directors of the Anticoagulation Forum. The remaining authors report no conflicts of interest in this work.
Acknowledgments
The Anticoagulation Forum supported the development of this manuscript.
Additional information
Funding
References
- Virani SS, Alonso A, Aparicio HJ. et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021;143(8):e254–e743. doi:10.1161/CIR.0000000000000950
- Allison MA, Ho E, Denenberg JO, et al. Ethnic-specific prevalence of peripheral arterial disease in the United States. Am J Prev Med. 2007;32(4):328–333. doi:10.1016/j.amepre.2006.12.010
- Creager MA, Matsushita K, Arya S, et al. Reducing nontraumatic lower-extremity amputations by 20% by 2030: time to get to our feet: a policy statement from the American Heart Association. Circulation. 2021;143(17):e875–e891. doi:10.1161/CIR.0000000000000967
- Matsushita K, Sang Y, Ning H, et al. Lifetime risk of lower-extremity peripheral artery disease defined by ankle-brachial index in the United States. J Am Heart Assoc. 2019;8(18):e012177. doi:10.1161/JAHA.119.012177
- Nehler MR, Duval S, Diao L, et al. Epidemiology of peripheral arterial disease and critical limb ischemia in an insured national population. J Vasc Surg. 2014;60(3):686–95 e2. doi:10.1016/j.jvs.2014.03.290
- Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC Guideline on the management of patients with lower extremity peripheral artery disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2017;69(11):e71–e126. doi:10.1016/j.jacc.2016.11.007
- Fowkes FG, Murray GD; Ankle Brachial Index C. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA. 2008;300(2):197–208. doi:10.1001/jama.300.2.197
- Control CoD. CDC WONDER online database. Available from: https://wonder.cdc.gov/ucd-icd10.html. Accessed June 7, 2024.
- Bridgwood BM, Nickinson AT, Houghton JS, Pepper CJ, Sayers RD. Knowledge of peripheral artery disease: what do the public, healthcare practitioners, and trainees know? Vasc Med. 2020;25(3):263–273. doi:10.1177/1358863X19893003
- Eraso LH, Fukaya E, Mohler ER, Xie D, Sha D, Berger JS. Peripheral arterial disease, prevalence and cumulative risk factor profile analysis. Eur J Prev Cardiol. 2014;21(6):704–711. doi:10.1177/2047487312452968
- Hira RS, Cowart JB, Akeroyd JM, et al. Risk factor optimization and guideline-directed medical therapy in US veterans with peripheral arterial and ischemic cerebrovascular disease compared to veterans with coronary heart disease. Am J Cardiol. 2016;118(8):1144–1149. doi:10.1016/j.amjcard.2016.07.027
- Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286(11):1317–1324. doi:10.1001/jama.286.11.1317
- Hirsch AT, Allison MA, Gomes AS, et al. A call to action: women and peripheral artery disease: a scientific statement from the American Heart Association. Circulation. 2012;125(11):1449–1472. doi:10.1161/CIR.0b013e31824c39ba
- Hackler EL, Hamburg NM, White Solaru KT. Racial and ethnic disparities in peripheral artery disease. Circ Res. 2021;128(12):1913–1926. doi:10.1161/CIRCRESAHA.121.318243
- Collins TC, Johnson M, Henderson W, Khuri SF, Daley J. Lower extremity nontraumatic amputation among veterans with peripheral arterial disease: is race an independent factor? Med Care. 2002;40(1 Suppl):I106–I116. doi:10.1097/00005650-200201001-00012
- McDermott MM, Greenland P, Liu K, et al. Leg symptoms in peripheral arterial disease: associated clinical characteristics and functional impairment. JAMA. 2001;286(13):1599–1606. doi:10.1001/jama.286.13.1599
- Gornik, H, Aronow, H. et al. 2024 ACC/AHA/AACVPR/APMA/ABC/SCAI/SVM/SVN/SVS/SIR/VESS guideline for the management of lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2024;83(24):2497–2604. doi:10.1016/j.jacc.2024.02.013
- Chen X, Stoner JA, Montgomery PS, et al. Prediction of 6-minute walk performance in patients with peripheral artery disease. J Vasc Surg. 2017;66(4):1202–1209. doi:10.1016/j.jvs.2017.03.438
- Criqui MH, Matsushita K, Aboyans V, et al. Lower extremity peripheral artery disease: contemporary epidemiology, management gaps, and future directions: a scientific statement from the American Heart Association. Circulation. 2021;144(9):e171–e191. doi:10.1161/CIR.0000000000001005
- Pollak AW, Norton PT, Kramer CM. Multimodality imaging of lower extremity peripheral arterial disease: current role and future directions. Circ Cardiovasc Imaging. 2012;5(6):797–807. doi:10.1161/CIRCIMAGING.111.970814
- Shrestha LS, Talaie R. Magnetic resonance angiography in the evaluation of peripheral arterial disease. J Radiol Nurs. 2018;37(4):228–232.
- Tummala S, Scherbel D. Clinical assessment of peripheral arterial disease in the office: what do the guidelines say? Semin Intervent Radiol. 2018;35(5):365–377. doi:10.1055/s-0038-1676453
- Kovacs RJ, Drozda JP Jr. The changing face of team care, and a challenge for the future. J Am Coll Cardiol. 2015;65(19):2137–2139. doi:10.1016/j.jacc.2015.03.556
- Miller AP, Handberg EM, Rodgers GP. It takes a team to deliver optimal cardiovascular care. J Am Coll Cardiol. 2018;72(8):948–951. doi:10.1016/j.jacc.2018.07.017
- Brush JE Jr, Handberg EM, Biga C, et al. 2015 ACC Health policy statement on cardiovascular team-based care and the role of advanced practice providers. J Am Coll Cardiol. 2015;65(19):2118–2136. doi:10.1016/j.jacc.2015.03.550
- Creager MA, Hamburg NM, Calligaro KD, et al. 2021 ACC/AHA/SVM/ACP advanced training statement on vascular medicine (Revision of the 2004 ACC/ACP/SCAI/SVMB/SVS clinical competence statement on vascular medicine and catheter-based peripheral vascular interventions). Circ Cardiovasc Interv. 2021;14(2):e000079. doi:10.1161/HCV.0000000000000079
- Dhand S. Multidisciplinary Approach to PAD: who’s on Your Team? Semin Intervent Radiol. 2018;35(5):378–383. doi:10.1055/s-0038-1676094
- Kolte D, Parikh SA, Piazza G, et al. Vascular teams in peripheral vascular disease. J Am Coll Cardiol. 2019;73(19):2477–2486. doi:10.1016/j.jacc.2019.03.463
- Rodgers GP, Linderbaum JA, Pearson DD, et al. 2020 ACC Clinical competencies for nurse practitioners and physician assistants in adult cardiovascular medicine: a report of the ACC competency management committee. J Am Coll Cardiol. 2020;75(19):2483–2517. doi:10.1016/j.jacc.2020.01.005
- Writing C, Birtcher KK, Allen LA, et al. 2022 ACC expert consensus decision pathway for integrating atherosclerotic cardiovascular disease and multimorbidity treatment: a framework for pragmatic, patient-centered care: a report of the American college of cardiology solution set oversight committee. J Am Coll Cardiol. 2023;81(3):292–317. doi:10.1016/j.jacc.2022.08.754
- Dunn SP, Birtcher KK, Beavers CJ, et al. The role of the clinical pharmacist in the care of patients with cardiovascular disease. J Am Coll Cardiol. 2015;66(19):2129–2139. doi:10.1016/j.jacc.2015.09.025
- Aboyans V, Criqui MH, Abraham P, et al. Measurement and interpretation of the ankle-brachial index: a scientific statement from the American Heart Association. Circulation. 2012;126(24):2890–2909. doi:10.1161/CIR.0b013e318276fbcb
- Winfrey C, Wortman S, Frede S, Kunze N, Conrad WF, Heaton PC. Pharmacist-initiated peripheral arterial disease screening program in a community pharmacy setting. J Am Pharm Assoc. 2011;51(3):373–377. doi:10.1331/JAPhA.2011.09160
- Sussman JB, Heisler M. Of Barbershops and churches: can community-based interventions improve cardiovascular risk in high-risk patients? Circulation. 2018;11(10):e005149. doi:10.1161/CIRCOUTCOMES.118.005149
- White Solaru KT, Coy T, DeLozier S, et al. Findings of a novel barbershop-based peripheral artery disease screening program for black men. J Am Heart Assoc. 2022;11(20):e026347. doi:10.1161/JAHA.122.026347
