Abstract
This review describes and summarizes the available evidence related to the treatment and management of Barth syndrome. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standards were used to identify articles published between December 2004 and January 2015. The Cochrane Population, Intervention, Control, Outcome, Study Design (PICOS) approach was used to guide the article selection and evaluation process. Of the 128 articles screened, 28 articles matched the systematic review inclusion criteria. The results of this review indicate the need for a flexible and multidisciplinary approach to manage the symptoms most commonly associated with Barth syndrome. It is recommended that a comprehensive care team should include individuals with Barth syndrome, their family members and caregivers, as well as medical, rehabilitative, nutritional, psychological, and educational professionals. The evidence for specific treatments, therapies, and techniques for individuals with Barth syndrome is currently lacking in both quality and quantity.
Introduction
Barth syndrome is a rare X-linked genetic disorder first described by Dr Peter G Barth in 1983.Citation1 It is caused by mutations in the TAZ gene, which is known to encode for the protein tafazzin. Tafazzin plays an important role in the remodeling of cardiolipin, a component of the mitochondrial membrane necessary for maintaining mitochondrial structure as well as for mitochondrial apoptosis and functioning of the electron transport chain.Citation2,Citation3 Heart failure is the most common clinical feature identified at birth and is the leading cause of death in infants with Barth syndrome. The most common cardiac features of Barth syndrome include dilated cardiomyopathy, left ventricular non-compaction, endocardial fibroelastosis, and serious disturbances of heart rhythm such as ventricular fibrillation or tachycardia.Citation4 Sepsis due to neutropenia may also be present at birth and is the second leading cause of infant mortality in Barth syndrome.Citation5 Though survival past infancy is now common in Barth syndrome, cardiovascular and hematological features (ie, neutropenia) in addition to 3-methylglutaconic aciduria often continue throughout the individual’s lifespan.Citation6
Clinical presentation of Barth syndrome also includes neuromuscular features such as skeletal myopathy, hypotonia, delayed motor milestones, exercise intolerance, and abnormal fatigability.Citation7 Growth delay is common in childhood; however, catch-up growth often occurs during late adolescence with achievement of normal adult height in most boys. Often in Barth syndrome, there is the presence of sensory or oral–motor feeding problems, nutritional deficiencies, and episodic or chronic diarrhea.Citation8,Citation9 Specific feeding-related behaviors include difficulty transitioning to solid foods, frequent gagging or difficulty swallowing, and a strong preference for salty or spicy foods while rejecting many other foods eaten by the family.Citation10 There is no definitive cognitive or neurological profile associated with Barth syndrome, though mild learning disabilities, attention deficits, visual spatial deficits, and auditory processing difficulties have been reported.Citation7,Citation9,Citation11
Considering that Barth syndrome is a multisystem disorder, it may be first identified by many different specialists or generalists.Citation7 While there is currently no cure for Barth syndrome, management of clinical features is possible in many cases. Subsequently, individuals with Barth syndrome are likely to interact with a wide range of health care professionals throughout the course of their lifespan in order to address the myriad of symptoms associated with the disorder. The purpose of this review was to identify interventions that are being used to manage symptoms of the disorder and to evaluate the evidence for these interventions related to health and function-related outcomes.
Methods
Prior to initiating a literature search, a protocol using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement was established. Five databases were strategically searched: PubMed, CINAHL, Physiotherapy Evidence Database, Dentistry and Oral Sciences Source, and ProQuest index of Dissertation and Theses. This initial search was followed by secondary selection of articles based on a review of references in relevant articles and articles published online by the Barth Syndrome Foundation. Following PRISMA guidelines, titles of all articles were reviewed for appropriateness, followed by a review of relevant abstracts and appraisal of full-text articles.Citation12 Selection was based on preestablished inclusion and exclusion criteria (the information is described in the paragraph below). The search strategy was initiated using the following question: What treatments, therapies, or techniques are recommended for the management of symptoms seen in males with Barth syndrome? Search terms included Barth AND Syndrome. Only articles published in the last 10 years (December 2004–January 2015) were considered; nonelectronic sources of literature were not considered and only those articles written in English were appraised.
The population was specifically defined as males with a diagnosis of Barth syndrome. Studies using in vitro methods or models (eg, rodent or yeast models) were not considered. To meet the inclusion criteria for intervention, each publication needed to report on the use of a treatment, therapy, or technique to improve the health, well-being, or level of functioning for an individual with Barth syndrome. Interventions focused on end-of-life care were not considered. No comparative intervention or population was required. The studies included were required to assess outcomes relevant to the management of symptoms commonly seen in Barth syndrome including, but not limited to, cardiac function, feeding/eating, nutrition, motor skill development, education, growth, and fatigue. The following standards were used for assessing the levels of evidence and to evaluate the study design and quality of the reviewed articles:
Level I: systematic reviews, meta-analyses, randomized controlled trials
Level II: two groups, nonrandomized studies (eg, case–control)
Level III: one group, nonrandomized (eg, before and after, pretest and posttest)
Level IV: descriptive studies that include analysis of outcomes (single-subject design, case series)
Level V: case reports and expert opinion that include narrative literature reviews and consensus statements.Citation13,Citation14
Results
Initial search strategies of the five databases yield 309 articles, with an additional 16 records identified through reference review and supplemental searches (). After duplicates were removed (n=19) and titles were screened for relevance, a total of 129 articles remained.Citation2–Citation11,Citation15–Citation133 Within the screened publications, descriptive studies, case reports, narrative reviews, consensus statements, and expert opinion articles were represented. Of the 129 abstracts screened, 86 were excluded with reasons, while 17 appeared to match the Cochrane Population, Intervention, Control, Outcome, Study Design (PICOS) inclusion criteria. An additional 27 articles did not have enough information in the abstract to justify exclusion, received the designation of “maybe”, and were included in the next phase of the review. A comprehensive list of the reviewed abstracts with rationale for exclusion is presented in . Based on established exclusion criteria, 24 studies did not meet population criteria (28.6%) and 71 studies did not fulfill the intervention criteria (84.5%). Among the abstracts reviewed, there were none that met both population and intervention criteria but were excluded due to irrelevant outcome measures.
Figure 1 PRISMA flow diagram.
Abbreviation: PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
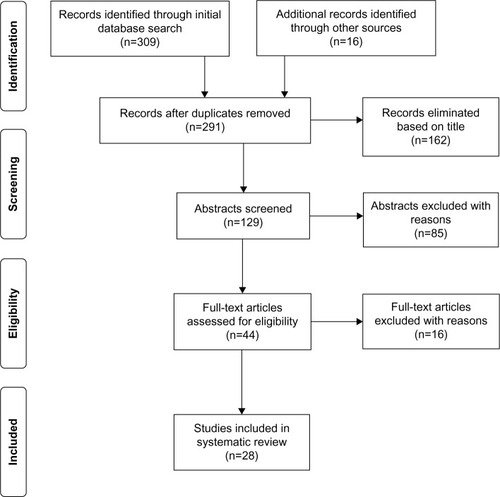
Table 1 Master citation table of reviewed abstracts
A total of 44 articles were assessed for eligibility through a full-text review. Each of the 44 articles was read and evaluated based upon the preestablished inclusion/exclusion criteria and level of evidence rating. Sixteen articles did not meet inclusion criteria and were therefore excluded (). Twenty-eight studies met all inclusion criteria; two articles were ranked at Level IV and 26 were ranked at Level V. identifies the characteristics of all the 28 articles meeting inclusion criteria, including all PICOS components.
Table 2 Articles excluded after full-text review
Table 3 Articles included in systematic review
Study design
Of the 28 articles selected for this systematic review, 15 were case reports,Citation17,Citation21,Citation39,Citation54,Citation60,Citation69,Citation70,Citation84,Citation85,Citation91,Citation101,Citation105,Citation113,Citation114,Citation131 six were literature reviews,Citation2,Citation3,Citation7,Citation19,Citation47,Citation82 and five were fact sheets.Citation8,Citation20,Citation23,Citation24,Citation26 The selected articles also included one descriptive cohort studyCitation6 and one descriptive comparison design.Citation112 Of the 28 articles included in this review, only two used statistical analysis procedures for the analysis of outcomes. Rigaud et al used descriptive and multivariate statistics in a natural history cohort study of 22 individuals with Barth syndrome.Citation6 In this paper, the Kaplan–Meier method was used to estimate survival rates and survival was compared between groups of individuals based on birth year using a log-rank test. Storch et al compared a sample of 34 boys with Barth syndrome with 22 healthy male controls.Citation112 Independent sample t-tests were used to compare the two groups on a variety of psychosocial outcomes. In this study, the alpha level for significance was set at P<0.05; no corrections were made for the possibility of type I error with multiple t-tests.
Population
Across all the 28 reviewed articles, 74 males with the diagnosis of Barth syndrome were enrolled. The sample varied in ethnic origin with representation from American, European, and Asian countries. Case reports described the clinical courses of individuals with Barth syndrome ranging in age from birth to 30 years.
Interventions
Medical interventions
Medical interventions were the most common interventions reported, with 23/28 articles reporting on the use of prescription medications and/or surgical techniques. Medical management of heart failure often used a polypharmacological approach. Cardiac hypertension and congestive heart failure (CHF) were frequently reported to be treated with cardiac glycosides such as digoxin, diuretics such as furosemide, and angiotensin-converting enzyme inhibitors such as captopril; beta-adrenoceptor blockers (β-blockers) such as carvedilol were also reported to be frequently used for the treatment of hypertension, CHF, and/or arrhythmia.Citation2,Citation3,Citation6,Citation7,Citation17,Citation21,Citation23,Citation54,Citation69,Citation70,Citation82,Citation85,Citation91,Citation101,Citation113
In addition to pharmacological therapy to address heart failure, surgical techniques were also identified. Case reports indicated cardiac transplants in six individuals with Barth syndrome,Citation60,Citation84,Citation105 while two additional case reports indicated mitral valve replacement or valvuloplasty.Citation69,Citation131 Three case reportsCitation39,Citation60,Citation105 and one cohort studyCitation6 identified the use of a ventricular assistance device (eg, the Berlin Heart EXCOR) as a successful bridge to cardiac transplant. An implantable cardioverter defibrillator was utilized in one case to prevent sudden death due to life-threatening ventricular arrhythmias.Citation70
Medical management of neutropenia was most frequently accomplished with the use of granulocyte colony-stimulating factor (G-CSF), as reported in four case reports.Citation21,Citation54,Citation60,Citation70 In their cohort study of 22 individuals with Barth syndrome, Rigaud et al indicated that G-CSF was used in six patients, with two individuals receiving long-term G-CSF therapy and the other four using G-CSF “on demand” when an infection occurred.Citation6 In the same study, four individuals also received antibiotic prophylaxis for the treatment of infections secondary to neutropenia.
Dietary interventions
Dietary interventions were identified in 11/28 of the reviewed articles. The use of oral carnitine supplementation (eg, L-carnitine) was identified in one case report,Citation17 one fact sheet,Citation23 and two literature reviews.Citation7,Citation47 Dietary supplementation with argentine was recommended in two literature reviewsCitation7,Citation3 and one cohort study.Citation6 Other nutritional supplements recommended as dietary interventions in the Barth population included cornstarch given before bedtime,Citation7,Citation20 parenteral amino acid nutrition or intravenous supplemental amino acids,Citation8,Citation24 magnesium supplementation,Citation114 potassium supplementation,Citation8,Citation23,Citation24 and daily multivitamins.Citation23,Citation24 Storch et al noted that boys with Barth syndrome may also need a special diet at school, suggesting the need for dietary interventions across multiple settings.Citation112
Feeding aids and strategies
Feeding aids were identified in 5/28 of the reviewed articles. Nasogastric and gastronomy tubes were recommended in cases where boys with Barth syndrome could not take adequate amounts of food or drink by mouth and therefore needed nutrients to be placed directly into the stomach.Citation6,Citation7,Citation24,Citation70,Citation91 Other feeding aids recommended by the Barth Syndrome FoundationCitation24 included preemie nipples, Habermann Feeders®, and Supplemental Nutrition Systems™. Feeding strategies for boys with Barth syndrome were also described in cases where the child had strong food and eating preferences (eg, picky eaters or sensory sensitivities). These strategies included giving the child control over food choices or having the option to spit something out, consuming small portions of food throughout the day instead of eating three large meals, and slowly introducing new foods into the child’s diet.Citation24
Rehabilitative
Limited rehabilitative interventions were identified in this review. One case studyCitation105 and one literature reviewCitation47 identified physical therapy (ie, physiotherapy) as a possible intervention to improve muscle weakness and tone in boys with Barth syndrome. Another literature review acknowledged that mobility aids such as wheelchairs may be used to conserve energy.Citation7
Educational
Storch et al reported a significant need for academic accommodations for boys with Barth syndrome as compared to healthy male controls.Citation112 Specific accommodations identified in this study were classroom seating changes, rest periods, schedule adjustments, note takers, extra books for home use, alternative assignments, extra tutorials, use of tape recorders, and peer mentors. In addition, some boys with Barth syndrome may need medication administration at school. As noted by Clarke et al, approximately 33% of boys with Barth syndrome require some form of special education.Citation7
Psychological
In addition to academic and educational supports, Storch et al found that out of the 34 boys – with Barth syndrome – surveyed, 26% were monitored by a school psychologist, while 22% had close contact with a guidance counselor.Citation112 No other psychological interventions were identified in the 28 articles included in this review.
Outcomes
The most frequent outcomes reported in the 28 reviewed articles were related to the core features of Barth syndrome, which are cardiac complications (eg, CHF, hypertension, and arrhythmia) and neutropenia. Specific outcomes related to heart function included improvement of ejection fraction on echocardiogram,Citation17 progressive improvement of left ventricular function,Citation85 improvement in cardiomegaly with reduced pulmonary edema,Citation91 and decreased incidence of heart failureCitation6 with the use of cardiac medications. However, since most articles reported on the use of multiple medications simultaneously, the individual contributions of each medication or medication type are indistinguishable from the overall effects of the medication regime. In contrast, neutropenia was primarily treated using G-CSF, and therefore outcomes such as increased neutrophil count and reduced infection can be more specifically linked with this medical treatment.Citation6,Citation21 Interestingly, the simultaneous use of multiple drugs (polypharmacy) was questioned in one review, indicating that coadministration of contraindicated medications may prove to be life threatening in some children with Barth syndrome.Citation82
Objective outcomes related to dietary interventions or use of feeding aids were limited in this systematic review. While one literature review suggested that carnitine deficiency in Barth syndrome may be ameliorated by means of substitution,Citation47 other articles suggested no significant benefit with the use of carnitine supplements.Citation7,Citation17,Citation23 Similarly, one published reviewCitation7 and one case reportCitation84 suggested that there is no evidence for the use of pantothenic acid supplements in this population. Magnesium supplementation was utilized in one case report of an 18-year-old male with Barth syndrome.Citation114 In this report, magnesium supplementation led to a slight improvement in muscle strength and normalization of serum magnesium levels. Specific outcomes data related to caloric intake, weight gain, and/or growth were not reported in the other reviewed articles which utilized dietary interventions, feeding aids, or feeding strategies.
Rehabilitative outcomes were also limited in this review. Singh et al reported on a 7-month-old African-American male with Barth syndrome whose muscle tone improved with physical therapy; however, the frequency and duration of physical therapy were not reported, nor were any specific measures of muscle strength or tone.Citation105 In line with this outcome, Finsterer and Frank indicated in their 2013 review that physiotherapy may help to improve muscle weakness in boys with Barth syndrome.Citation47 Interestingly, Takeda et al argued in their review of the literature that no treatment is needed for hypotonia because it usually resolves spontaneously.Citation2
No outcomes related to educational or psychological interventions were reported.
Discussion
Medical management of Barth syndrome
The interventions and outcomes identified in this review reinforce that treatment of medical complications associated with Barth syndrome is of primary importance in this population. However, the types of articles available for this systematic review represent reports that are not based on scientific analysis of clinical outcomes. Of the 28 reviewed articles, 15 were case reports. While case reports have a role in medical literature, particularly for detecting novelties and describing unique cases, findings from case reports often lack generalizability and are reliant upon the author’s memory of events or availability of information in medical records.Citation134
Though lacking direct evidence, the accumulation of descriptive data from case reports and expert clinical opinion suggest that cardiac medications (eg, β-blockers, angiotensin-converting enzyme inhibitors) can be used to alleviate symptoms of heart failure and prolong life in boys with Barth syndrome. In addition, several sources reported increased levels of circulating neutrophils following G-CSF treatment, suggesting that G-CSF, possibly combined with appropriate prophylactic antibiotics, is the best available treatment for neutropenia in this population.Citation19,Citation21,Citation70 While neutropenia appears to respond well to G-CSF, Rigaud et al noted that 2 of the 22 Barth patients in their cohort study had episodes of severe infection while on G-CSF therapy.Citation6 It is also important to note that some medications, either in isolation or coadministered with other medications, may cause symptoms to worsen, and therefore starting or stopping of any new medications or increasing the dosage of the existing ones should be closely monitored in boys with Barth syndrome.Citation23
While several successful surgeries, including cardiac transplants, were reported in the 28 reviewed articles,Citation60,Citation84,Citation105 none of the articles provided data on how many boys with Barth syndrome failed to survive the surgery or what was the long-term survival rates post discharge. Since journals often prefer publication of cases with positive outcomes, there is a risk in overstating or generalizing the surgical outcomes gleaned in this review.Citation134
Despite the lack of specific outcomes in this review, it is clear that medical management of Barth syndrome is essential for growth and survival. Medical team members involved in the care of boys with Barth syndrome may include specialists in cardiology, hematology, metabolism, endocrinology, neurology, and genetics, as well as developmental pediatricians and primary care physicians.
Feeding and dietary interventions for Barth syndrome
The literature supporting nonmedical interventions for Barth syndrome is much scarcer. While it has been identified that feeding issues are stressful for families of boys with Barth syndrome, very little research has been directed toward interventions that support feeding behaviors or nutritional concerns.Citation9,Citation10 Further, there does not appear to be consensus about which nutritional supplements are effective in this population or what process should go into the selection of a supplemental regime.
Given the complexity of feeding and nutritional issues in boys with Barth syndrome, multiple disciplines may be involved in the management of these clinical features. Dietitians and nutritional specialists will likely work closely with medical doctors, including metabolic specialists, to determine what and how much food/liquid the child should be consuming. Decisions about the placement of nasogastric tubes or other long-term enteral nutritional support will likely be made by a team of individuals familiar with the specific child and familiar with the complexities of Barth syndrome. Throughout the lifespan of a boy with Barth syndrome, the needs of the child and the family will likely require consultation or intervention by a variety of other health care professionals. During infancy, lactation consultants, pediatric nurses, and occupational therapists may work with families in order to facilitate good positioning for breastfeeding and recommend appropriate feeding aids and strategies to assist the child with oral sucking and self-regulation during the feeding process. When the child begins transitioning to solid foods, rehabilitative professionals (ie, physical therapists, occupational therapists, and speech and language pathologists) may be consulted for issues related to proper positioning, coordination of chewing and swallowing, or sensory sensitivities leading to picky eating patterns. As the child grows, nutritional concerns related to growth will likely become important and ongoing case management with the medical team may be necessary. During the school years, special dietary or feeding needs may need to be documented on the child’s individualized education plan and consultation between the school team and medical team may be required. Since eating is a big part of normal socialization patterns, practitioners should be mindful of the need for children, adolescents, and adults with Barth syndrome to participate in these types of activities as part of their overall psychosocial health.
Interventions to support participation and well-being
This systematic review identified a relative gap in the literature in regard to the interventions that support the participation and well-being of boys with Barth syndrome and their families. Physical therapy was identified as one rehabilitative service that could potentially help enhance muscle strength and tone; however, it was unclear from the review whether these improvements in strength and tone led to increased play with peers, greater participation due to lack of fatigue, or an improvement in self-concept or self-esteem. Research using mouse models of Barth syndrome are beginning to provide insights into the physiological benefits of exercise and endurance training;Citation135 however, translation of these findings into practice are nonexistent. As basic science research begins to work its way from bench to bedside, it will be important for researchers and clinicians alike to focus on the functional and participation benefits of exercise in addition to changes in muscle physiology.
Finally, this review did not identify any currently researched interventions to address the psychosocial needs of boys with Barth syndrome and their families. As noted by Storch et al, youth with Barth syndrome tend to have more internalizing and externalizing symptoms, social problems, and loneliness compared to healthy children; in addition, they rate their overall quality of life much lower than that of healthy controls and other children with cardiac problems.Citation112 Parents of boys with Barth syndrome also report higher stress levels compared to parents of health controls. Psychologists, licensed clinical social workers, occupational therapists, and other mental health professionals may be able to help children and families with these issues through a variety of therapeutic interventions. There is a current need to examine the usefulness and applicability of these types of services in the Barth population.
Conclusion
This systematic review highlights the paucity of objective, high-level evidence supporting interventions for males with Barth syndrome. While case reports and literature reviews on this rare disorder are important contributions to the literature, future studies should aim to include systematic and objective analyses of outcomes using research designs with methodological rigor. This level of research is needed across multiple disciplines in order to develop best practices for the management of the symptoms most commonly associated with the Barth syndrome. Clinically, it is recommended that a comprehensive care team be established, which includes individuals with Barth syndrome, their family members and caregivers, as well as medical, rehabilitative, nutritional, psychological, and educational professionals. While medical management of symptoms that preserves life is of primary importance, services that enhance the child’s and family’s quality of life and participation should also be included as part of the individual’s care plan.
Acknowledgments
Stacey Reynolds would like to thank Hope Caracci, OTD, OTR/L, Division of Pediatric Rehabilitation, Children’s Hospital of The Kings Daughter, for her assistance in preparing this paper.
Disclosure
The author reports no conflicts of interest in this work.
References
- BarthPGScholteHRBerdenJAAn X-linked mitochondrial disease affecting cardiac muscle, skeletal muscle and neutrophil leucocytesJ Neurol Sci1983621–33273556142097
- TakedaASudoAYamadaMEponym: Barth syndromeEur J Pediatr2011170111365136721947198
- JefferiesJLBarth syndromeAm J Med Genet C Semin Med Genet2013163C319820523843353
- GarrattVRiddifordDStewardCTsai-GoodmanBNewbury-EcobRWhat is Barth syndrome?Midwives2011144323324893484
- FerriLDonatiMAFunghiniSNew clinical and molecular insights on Barth syndromeJ Rare Disord2013827
- RigaudCLebreASTouraineRNatural history of Barth syndrome: a national cohort study of 22 patientsJ Rare Disord2013870
- ClarkeSLBowronAGonzalezILBarth syndromeJ Rare Disord2013823117
- KelleyRIManagement of Diarrheal Illness in Patients With Barth Syndrome2008 Available from: https://www.barthsyndrome.org/CMFiles/Resources/DiarrheaBarthFINAL2008.pdfAccessed January 18, 2015
- ReynoldsSKreiderCMBendixenRA mixed-methods investigation of sensory response patterns in Barth syndrome: a clinical phenotype?Am J Med Genet A2012158A71647165322711649
- ReynoldsSKreiderCMMeeleyLEBendixenRFeeding history and chemical taste sensitivity in boys with Barth syndromeJ Rare Disord201531
- MazzoccoMMHenryAEKelleyRIBarth syndrome is associated with a cognitive phenotypeJ Dev Behav Pediatr2007281223017353728
- MoherDLiberatiATetzlaffJAltmanDGPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementJ Clin Epidemiol2009621006101219631508
- American Occupational Therapy Association (AOTA)Guidelines to Critically Appraised Paper Worksheet2014 Available from: http://www.aota.org/-/media/Corporate/Files/Practice/EvidenceExchange/CAP%20Guidelines%20for%20Evidence%20Exchange.pdfAccessed August 4, 2014
- SackettDLRosenbergWMGrayJAHaynesRBRichardsonWSEvidence based medicine: what it is and what it isn’tClin Orthop Relat Res20074553517340682
- AcehanDXuYStokesDLSchlameMComparison of lymphoblast mitochondria from normal subjects and patients with Barth syndrome using electron microscopic tomographyLab Investig2007871404817043667
- AcehanDVazFHoutkooperRHCardiac and skeletal muscle defects in a mouse model of human Barth syndromeJ Biol Chem2011286289990821068380
- AljishiEAliFBarth syndrome: an X-linked cardiomyopathy with a novel mutationIndian J Pediatr20107721432143320981509
- AncesBMSullivanJWeigeleJBStroke associated with Barth syndromeJ Child Neurol200621980580716970891
- ApikyanAAKhuchuaZAdvances in the understanding of Barth syndromeBr J Haematol2013161333033823432031
- AveryRCornstarch Fact Sheet2006 Available from: https://www.barthsyndrome.org/CMFiles/Resources/Cornstarch.pdfAccessed January 18, 2015
- BachouTGiannakopoulosATrapaliCVazeauAKattamisAA novel mutation in the G4.5 (TAZ) gene in a Greek patient with Barth syndromeBlood Cells Mol Disord2009423262264
- Barth Syndrome FoundationMetabolism of Barth syndrome2005 Available from: https://www.barthsyndrome.org/CMFiles/Resources/MetabolismBarthSyndromeFINAL.pdfAccessed January 18, 2015
- Barth Syndrome FoundationMedications Used in Barth syndrome2005 Available from: https://www.barthsyndrome.org/CMFiles/Resources/MedicationsFactSheetfinaledit82105.pdfAccessed January 18, 2015
- Barth Syndrome FoundationNutrition Facts in Barth syndrome2006 Available from: https://www.barthsyndrome.org/CMFiles/Resources/NutritionFactSheetFINALRevisedMay06.pdfAccessed January 18, 2015
- Barth Syndrome FoundationNeurological Manifestations in Barth Syndrome2006 Available from: https://www.barthsyndrome.org/CMFiles/Resources/NeurologicalManifestationsBarthedited.pdfAccessed January 18, 2015
- BowenSKelleyRIMannSOral Hygiene For Children With Barth Syndrome2007 Available from: https://www.barthsyndrome.org/CMFiles/Resources/OralHygieneBarthSyndromeFINAL.pdfAccessed January 18, 2015
- BowronAFrostRPowersVEThomasPHHealesSJStewardCGDiagnosis of Barth syndrome using a novel LC-MS/MS method for leukocyte cardiolipin analysisJ Inherit Metab Dis201336574174623109063
- BowronAHoneychurchJWilliamsMBarth syndrome without tetralinoleoyl cardiolipin deficiency: a possible ameliorated phenotypeJ Inherit Metab Dis201438227928625112388
- BradyANShehataBMFernhoffPMX-linked fetal cardiomyopathy caused by a novel mutation in the TAZ genePrenat Diagn200625546246516548007
- BrandnerKMickDUFrazierAETaylorRDMeisingerCRehlingPTaz1, an outer mitochondrial membrane protein, affects stability and assembly of inner membrane protein complexes: implications for Barth syndromeMol Biol Cell200516115202521416135531
- CadeWTSpencerCTReedsDNSubstrate metabolism during basal and hyperinsulinemic conditions in adolescents and young-adults with Barth syndromeJ Inherit Metab Dis20133619110122580961
- ChangBMomoiNShanLGonadal mosaicism of a TAZ (G4.5) mutation in a Japanese family with Barth syndrome and left ventricular noncompactionMol Genet Metab2010200219820320303308
- ChiccoAJSparagnaGCRole of cardiolipin alterations in mitochondrial dysfunction and diseaseAm J Physiol Cell Physiol20072921C33C4416899548
- ClaypoolSMBoontheungPMcCafferyJMLooJAKoehlerCMThe cardiolipin transacylase, tafazzin, associates with two distinct respiratory components providing insight into Barth syndromeMol Biol Cell200819125143515518799610
- ClaypoolSMMcCafferyJMKoehlerCMMitochondrial mislocalization and altered assembly of a cluster of Barth syndrome mutant tafazzinsJ Cell Biol2006174337939016880272
- ClaypoolSMWhitedKSrijumnongSHanXKoehlerCMBarth syndrome mutations that cause tafazzin complex labilityJ Cell Biol2011192344746221300850
- DayJASpencerCTByrneBGrip strength in a population of boys with Barth syndromePediatr Phys Ther20061818889
- DebnathSAddyaSMis-sense mutations in tafazzin (TAZ) that escort to mild clinical symptoms of Barth Syndrome is owed to the minimal inhibitory effect of the mutations on the enzyme function: in-silico evidenceInterdiscip Sci201471212525118650
- DedieuNGiardiniAStewardCGSuccessful mechanical circulatory support for 251 days in a child with intermittent severe neutropenia due to Barth syndromePediatr Transplant2013172E46E4923190323
- DiMauroSMitochondrial myopathiesCurr Opin Rheumatol200618663664117053512
- DiMauroSGurgel-GiannettiJThe expanding phenotype of mitochondrial myopathyCurr Opin Neurol200518553854216155436
- DonatiMAMalvagiaSPasquiniEBarth syndrome presenting with acute metabolic decompensation in the neonatal periodJ Inherit Metab Disord2006295684
- FanYStellerJGonzalezILA novel exonic splicing mutation in the TAZ (G4.5) gene in a case with atypical Barth syndromeJ Inherit Metab Disord20131199106
- Feillet-CoudrayCFouretGCasasFCoudrayCImpact of high dietary lipid intake and related metabolic disorders on the abundance and acyl composition of the unique mitochondrial phospholipid, cardiolipinJ Bioenerg Biomembr201446544745724951897
- FinstererJHematological manifestations of primary mitochondrial disordersActa Haematol20071182889817637511
- FinstererJCardiogenetics, neurogenetics, and pathogenetics of left ventricular hypertrabeculation/noncompactionPediatr Cardiol200930565968119184181
- FinstererJFrankMHaematological features in Barth syndromeCurr Opin Hematol2013201364023041719
- FinstererJStöllbergerCAtrial fibrillation/flutter in myopathiesInt J Cardiol2008a128330431018343511
- FinstererJStöllbergerCPrimary myopathies and the heartScand Cardiovasc J200842192418273731
- FinstererJStöllbergerCUnclassified cardiomyopathies in neuromuscular disordersWien Med Wochenschr201316321–2250551324154801
- FinstererJStöllbergerCBlazekGNeuromuscular implications in left ventricular hypertrabeculation/noncompactionInt J Cardiol2006110328830016364474
- FinstererJStöllbergerCBlazekGPrevalence of Barth syndrome in adult left ventricular hypertrabeculation/noncompactionScand Cardiovasc J200842215716018365900
- FinstererJStöllbergerCFazioGNeuromuscular disorders in left ventricular hypertrabeculation/noncompactionCurr Pharm Des201016262895290420632953
- FolsiVMigliettiNLombardiACardiomyopathy in a male patient with neutropenia and growth delayItal J Pediatr2014404524887148
- GerbertNJoshiASKutikSMitochondrial cardiolipin involved in outer-membrane protein biogenesis: implications for Barth syndromeCurr Biol200919242133213919962311
- Gilbert-BarnessEBarnessLAPathogenesis of cardiac conduction disorders in children genetic and histopathologic aspectsAm J Med Genet A2006140191993200616969859
- GonzalezILBarth syndrome: TAZ gene mutations, mRNAs, and evolutionAm J Med Genet A2005134440941415793838
- GonzalvezFD’AurelioMBoutantMBarth syndrome: cellular compensation of mitochondrial dysfunction and apoptosis inhibition due to changes in cardiolipin remodeling linked to tafazzin (TAZ) gene mutationBiochim Biophys Acta2013183281194120623523468
- GonzalvezFSchugZTHoutkooperRHCardiolipin provides an essential activating platform for caspase-8 on mitochondriaJ Cell Biol2008183468169619001123
- HankeSPGardnerABLombardiJPLeft ventricular noncompaction cardiomyopathy in Barth syndrome: an example of an undulating cardiac phenotype necessitating mechanical circulatory support as a bridge to transplantationPediatr Cardiol20123381430143422427193
- HastingsRStewardCTsai-GoodmanBNewbury-EcobRDysmorphology of Barth syndromeClin Dysmorphol200918418518719648820
- HauffKDHypocholesterolemia in Barth syndrome (NR52998)ProQuest Dissertations and ThesesCanadaUniversity of Manitoba2009335 Available from: http://search.proquest.com/docview/305061005?accountid=14780.(305061005)Accessed February 15, 2015
- HauffKDHatchGMCardiolipin metabolism and Barth syndromeProg Lipid Res20064529110116442164
- HauffKDHatchGMReduction in cholesterol synthesis in response to serum starvation in lymphoblasts of a patient with Barth syndromeBiochem Cell Biol201088459560220651830
- HonzikTTesarovaMMagnerMNeonatal onset of mitochondrial disorders in 129 patients: clinical and laboratory characteristics and a new approach to diagnosisJ Inherit Metab Disord2012355749759
- HoutkooperRHRodenburgRJThielsCCardiolipin and monolysocardiolipin analysis in fibroblasts, lymphocytes, and tissues using high-performance liquid chromatography-mass spectrometry as a diagnostic test for Barth syndromeAnal Biochem2009387223023719454236
- HoutkooperRHTurkenburgMPoll-TheBTThe enigmatic role of tafazzin in cardiolipin metabolismBiochim Biophys Acta20091788102003201419619503
- HoutkooperRHVazFMCardiolipin, the heart of mitochondrial metabolismCell Mol Life Sci200865162493250618425414
- HuangSCWuETChiuSNHwuWLWuMHWangSSMitral annuloplasty in an infant with Barth syndrome and severe mitral insufficiency: first case report and determination of annular diameterJ Thorac Cardiovasc Surg200813641095109718954662
- HuhtaJCPomeranceHHBarnsssEGClinicopathologic conference: Barth syndromeFetal Pediatr Pathol2005244–523925416396830
- JoshiASIdentification of cellular functions of cardiolipin as physiological modifiers of Barth syndrome (354426)ProQuest Dissertations and ThesesDetroit, MIWayne State University2012154 Available from: http://search.proquest.com/docview/1225792947?accountid=14780.(122579247)
- Karkucinska-WieckowskaATrubickaJWernerBLeft ventricular noncompaction (LVNC) and low mitochondrial membrane potential are specific for Barth syndromeJ Inherit Metab Disord2013366929937
- KimGBKwonBSBaeEJNohCISeongMWParkSSA novel mutation of the TAZ gene in Barth syndrome: acute exacerbation after contrast-dye injectionJ Korean Med Sci201328578478723678274
- KirwinSMManolakosABarnettSSGonzalezILTafazzin splice variants and mutations in Barth syndromeMol Genet Metab20141111263224342716
- KirwinSMVinetteKMSchwartzSBFunanageVLGonzalezILMultiple transmissions of Barth syndrome through an oocyte donor with a de novo TAZ mutationFertil Steril2007874976e5e717241629
- KleefstraTWortmannSBRodenburgRJMitochondrial dysfunction and organic aciduria in five patients carrying mutations in the Ras-MAPK pathwayEur J Hum Genet201119213814421063443
- KulikWvan LentheHStetFSBloodspot assay using HPLC-tandem mass spectrometry for detection of Barth syndromeClin Chem200854237137818070816
- LamariFMochelFSedelFSaudubrayJMDisorders of phospholipids, sphingolipids and fatty acids biosynthesis: toward a new category of inherited metabolic diseasesJ Inherit Metab Disord2013363411425
- LiGThe role of mitochondrial anionic phospholipids in signaling pathways and essential functions (3259009)ProQuest Dissertations and ThesesDetroit, MIWayne State University2007157 Available from: http://search.proquest.com/docview/3048022665?accountid=14780. (304802665)
- MakaryanVKulikWVazFMThe cellular and molecular mechanisms for neutropenia in Barth syndromeEur J Haematol201288319520922023389
- MalhotraAEdelman-NovemskyIXuYRole of calcium-independent phospholipase A2 in the pathogenesis of Barth syndromeProc Natl Acad Sci U S A200910672337234119164547
- MalhotraAKahlonPDonohoTDoyleICPharmacogenomic considerations in the treatment of the pediatric cardiomyopathy called Barth syndromeRecent Pat Biotechnol20148213614325185984
- ManELaffertyKAFunkeBHNGS identifies TAZ mutation in a family with X-linked dilated cardiomyopathyBMJ Case Report2013
- MangatJLunnon-WoodTReesPElliottMBurchMSuccessful cardiac transplantation in Barth syndrome – single-centre experience of four patientsPediatr Transplant200711332733117430492
- MarzilianoNMannarinoSNespoliLBarth syndrome associated with compound hemizygosity and heterozygosity of the TAZ and LDB3 genesAm J Med Genet A2007143A990791517394203
- MayrJALipid metabolism in mitochondrial membranesJ Inherit Metab Disord2015381137144
- MazurováSTesařováMMagnerMNovel mutations in the TAZ gene in patients with Barth syndromePrague Med Rep20131143139153
- McCantaACChangACWeinerKCardiomyopathy in a child with neutropenia and motor delayCurr Opin Pediatr200820560560718781126
- McKenzieMLazarouMThorburnDRRyanMTMitochondrial respiratory chain supercomplexes are destabilized in Barth syndrome patientsJ Mol Biol2006361346246916857210
- MejiaEMColeLKHatchGMCardiolipin metabolism and the role it plays in heart failure and mitochondrial supercomplex formationCardiovasc Hematol Disord Drug Targets20141429810624801725
- MomoiNChangBTakedaIAoyagiYEndoKIchidaFDiffering clinical courses and outcomes in two siblings with Barth syndrome and left ventricular noncompactionEur J Pediatr2012171351552021987083
- MonteiroJPOliveiraPJJuradoASMitochondrial membrane lipid remodeling in pathophysiology: a new target for diet and therapeutic interventionsProg Lipid Res201352451352823827885
- Moric-JaniszewskaEMarkiewicz-ŁoskotGGenetic heterogeneity of left-ventricular noncompaction cardiomyopathyClin Cardiol200831520120417729299
- OsmanCHaagMWielandFTBrüggerBLangerTA mitochondrial phosphatase required for cardiolipin biosynthesis: the PGP phosphatase GEP4EMBO J201029121976198720485265
- PoloncováKGriačPPhospholipid transport and remodeling in health and diseaseGen Physiol Biophys201130Spec NoS25S3521869448
- RachesDMazzoccoMMEmergence and nature of mathematical difficulties in young children with Barth syndromeJ Dev Behav Pediatr201233432833522566029
- RajaVGreenbergMLThe functions of cardiolipin metabolism-potential modifiers of the Barth syndrome phenotypeChem Phys Lipids2014179495624445246
- RavalKKKampTJCardiomyopathy, mitochondria and Barth syndrome: iPSCs reveal a connectionNat Med201420658558624901565
- RobertsAENixonCStewardCGThe Barth Syndrome Registry: Distinguishing disease characteristics and growth data from a longitudinal studyAm J Med Genet A2012158A112726273223045169
- RonveliaDGreenwoodJPlattJHakimSZaragozaMVIntra-familial variability for novel TAZ gene mutation: Barth syndrome with dilated cardiomyopathy and heart failure in an infant and left ventricular noncompaction in his great uncleMol Genet Metab2012107342843223031367
- Sabater-MolinaMGuillén-NavarroEGarcia-MolinaEBallesta-MartinezMJEscuderoFRuiz-EspejoFBarth syndrome in adulthood: a clinical caseRev Esp Cardiol (Engl Ed)2013661687022999963
- Saini-ChohanHKMitchellRWVazFMZelinskiTHatchGMDelineating the role of alterations in lipid metabolism to the pathogenesis of inherited skeletal and cardiac muscle disorders: Thematic Review Series: Genetics of human lipid diseaseJ Lipid Res201253142722065858
- SchlameMRenMBarth syndrome, a human disorder of cardiolipin metabolismFEBS Lett2006580235450545516973164
- SchugZTFrezzaCGalbraithLCGottliebEThe music of lipids: how lipid composition orchestrates cellular behaviorActa Oncol201251330131022283492
- SinghHRYangZSiddiquiSA novel Alu-mediated Xq28 microdeletion ablates TAZ and partially deletes DNL1L in a patient with Barth syndromeAm J Med Genet A2009149A51082108519396829
- SoustekMSFalkDJMahCSCharacterization of a transgenic short hairpin RNA-induced murine model of Tafazzin deficiencyHum Gene Ther201122786587121091282
- SparagnaGCLesnefskyEJCardiolipin remodeling in the heartJ Cardiovasc Pharmacol200953429030119276988
- SpencerCTBryantRMDayJCardiac and clinical phenotype in Barth syndromePediatrics20061182e337e34616847078
- SpencerCTByrneBJBryantRMImpaired cardiac reserve and severely diminished skeletal muscle O2 utilization mediate exercise intolerance in Barth syndromeAm J Physiol Heart Circ Physiol20113015H2122H212921873497
- SpencerCTByrneBJGewitzMHVentricular arrhythmia in the X-linked cardiomyopathy Barth syndromePediatr Cardiol200526563263716235007
- StewardCGNewbury-EcobRAHastingsRBarth syndrome: an X-linked cause of fetal cardiomyopathy and stillbirthPrenat Diagn2010301097097620812380
- StorchEAKeeleyMMerloLJPsychosocial functioning in youth with Barth syndromeChild Health Care200938213715620808735
- SweeneyRTDavisGJNoonanJACardiomyopathy of unknown etiology: Barth syndrome unrecognizedCongenit Heart Dis200936433438
- TajimaTSatohKOkuharaKTsubakiJFujiedaKHypomagnesemia in a patient with Barth syndromeJ Pediatr Endocrinol Metab200518552315921184
- TakedaASudoAYamadaMBarth syndrome diagnosed in the subclinical stage of heart failure based on the presence of lipid storage myopathy and isolated noncompaction of the ventricular myocardiumEur J Pediatr2011170111481148421932011
- TikhomirovEAeryanovaNBasarginaEDegtyarevaTGene symbol: TAZ. disease: Barth syndromeHum Genet20081243315316
- TowbinJALeft ventricular noncompaction: a new form of heart failureHeart Fail Clin2010626459462
- ValianpourFMitsakosVSchlemmerDMonolysocardiolipins accumulate in Barth syndrome but do not lead to enhanced apoptosisJ Lipid Res20054661182119515805542
- van RaamBJKuijpersTWMitochondrial defects lie at the basis of neutropenia in Barth syndromeCurr Opin Hematol2009161141919057200
- van WerkhovenMAThorburnDRGedeonAKPittJJMonolysocardiolipin in cultured fibroblasts is a sensitive and specific marker for Barth syndromeJ Lipid Res200647102346235116873891
- VernonHJSandlersYMcClellanRKelleyRIClinical laboratory studies in Barth syndromeMol Genet Metab2014112214314724751896
- WanCYuHHLuMYClinical manifestations and outcomes of pediatric chronic neutropeniaJ Formos Med Assoc2012111422022722526211
- WangGMcCainMLYangLModeling the mitochondrial cardiomyopathy of Barth syndrome with induced pluripotent stem cell and heart-on-chip technologiesNat Med201420661662324813252
- WhitedKBaileMGCurrierPClaypoolSMSeven functional classes of Barth syndrome mutationHum Mole Genet2013223483492
- WilsonLDAl-MajidSRakovskiCSMdCDHigher IL-6 and IL6:IGF ratio in patients with Barth syndromeJ Inflamm (Lond)2012912522721508
- WortmannSBEspeelMAlmeidaLInborn errors of metabolism in the biosynthesis and remodeling of phospholipidsJ Inherit Metab Disord201538199110
- XingYIchidaFMatsuokaTGenetic analysis in patients with left ventricular noncompaction and evidence for genetic heterogeneityMol Genet Metab2006881717716427346
- XuYMalhotraARenMSchlameMJ Biol Chem200628151392173922417082194
- XuYSutachanJJPleskenHKelleyRISchlameMCharacterization of lymphoblast mitochondria from patients with Barth syndromeLab Invest200585682383015806137
- YeCShenZGreenbergMLCardiolipin remodeling: a regulatory hub for modulating cardiolipin metabolism and functionJ Bioenerg Biomembr Epub11292014
- YenTYHwuWLChienYHAcute metabolic decompensation and sudden death in Barth syndrome: report of a family and a literature reviewEur J Pediatr2008167894194417846786
- ZaragozaMVArbustiniENarulaJNoncompaction of the left ventricle: primary cardiomyopathy with an elusive genetic conditionCurr Opin Pediatr200719661962718025927
- ZweigerdtRGruhIMartinUYour heart on a chip: iPSC-based modeling of Barth-syndrome-associated cardiomyopathyCell Stem Cell201415191124996164
- NissenTWynnRThe clinical case report: a review of its merits and limitationsBMC Res Notes201472641724382056
- SoustekMSBaligandCFalkDJWalterGALewinASByrneBJEndurance training ameliorates complex 3 deficiency in a mouse model of Barth syndromeJ Inherit Metab Dis Epub4102015
