Abstract
Atrial fibrillation (AF) is a very common cardiac arrhythmia, and its prevalence is increasing along with aging in the developed world. This review discusses racial differences in the epidemiology and treatment of AF between African-American and Caucasian patients. Additionally, the effect of race on warfarin and novel oral anticoagulant use is discussed, as well as the role that physicians and patients play in achieving optimal treatment outcomes. Despite having a lower prevalence of AF compared with Caucasians, African-Americans suffer disproportionately from stroke and its sequelae. The possible reasons for this paradox include poorer access to health care, lower health literacy, and a higher prevalence of other stroke-risk factors among African-Americans. Consequently, it is important for providers to evaluate the effects of race, health literacy, access to health care, and cultural barriers on the use of anticoagulation in the management of AF. Warfarin-dose requirements vary across racial groups, with African-American patients requiring a higher dose than Caucasians to maintain a therapeutic international normalized ratio; the novel oral anticoagulants (dabigatran, rivaroxaban, and apixaban) seem to differ in this regard, although data are currently limited. Minority racial groups are not proportionally represented in either real-world studies or clinical trials, but as more information becomes available and other social issues are addressed, the treatment disparities between African-American and Caucasian patients should decrease.
Introduction
Atrial fibrillation (AF) is highly prevalent in the US, and with the incidence of AF continuing to grow, the costs of treatment are also increasing.Citation1 Stroke is a serious but preventable complication of AF, but therapeutic anticoagulation for the prevention of stroke can lead to an increased risk of bleeding;Citation2,Citation3 therefore, clinicians must be aware of the optimum benefit:risk ratio for the treatment of these patients. Despite African-Americans having a lower incidence of AF than Caucasians, the burden remains high, with one in nine African-Americans receiving a diagnosis before 80 years of age.Citation4
The objectives of this review are: 1) to provide clinicians with an overview of AF and the importance of stroke prevention; 2) to discuss stroke prevention in underrepresented patient populations, particularly African-American patients; 3) to highlight knowledge gaps related to stroke prevention in underrepresented patient populations; 4) to discuss racial differences in the prevalence of AF and response to anticoagulants; and 5) to discuss the role clinicians may play in the care of patients with AF.
Description, prevalence, and consequences of atrial fibrillation and stroke
AF, defined as an abnormal rate or rhythm of the heart, is the most common type of arrhythmia. In patients with AF, multiple disorganized electrical impulses lead to rapid and chaotic contractions that prevent the atria from contracting properly, and as a result blood does not travel normally through the heart and vasculature.Citation1 Although many patients with AF do not experience any symptoms, some patients can experience heart palpitations, lack of energy, dizziness, or shortness of breath. Additionally, AF can lead to an increase in the risk of stroke by allowing clots to form within the heart, which may travel to the brain. Nonvalvular AF (NVAF), defined as AF in the absence of rheumatic mitral valve disease, a prosthetic heart valve, or mitral valve repair, is the most common type of AF.Citation3,Citation5
The prevalence of AF is increasing along with aging in the developed world, and AF is associated with a fivefold-increased risk of stroke, with a fifth of all strokes associated with AF.Citation6,Citation7 Strokes are classified by the type of brain injury (eg, ischemic, hemorrhagic) and the type and location of the vascular lesion.Citation8 Ischemic strokes are by far the more common type, causing over 80% of all strokes, and 20% of all ischemic strokes result directly from AF.Citation9,Citation10 The absolute risk of stroke in patients with AF can vary 20-fold, and this risk is dependent on the number of additional risk factors that a patient may have, such as heart failure, hypertension, older age, diabetes, prior stroke, vascular disease, and female sex.Citation2,Citation11,Citation12 Strokes related to AF tend to be associated with greater morbidity and mortality compared with non-AF-related strokes;Citation13,Citation14 however, the risk of stroke can be reduced with anticoagulant treatment.Citation2,Citation3,Citation6,Citation15
The total health care cost of all strokes in the US was $53.9 billion in 2010, and of that figure, the cost of AF-related strokes was estimated to range from $3.2 billion to nearly $13 billion. By 2050, the economic burden of strokes related to AF in the US is estimated to approach $30 billion.Citation16
Are there racial/ethnic differences in the epidemiology of AF?
The incidence of AF is lower in African-Americans than in Caucasians; the reasons for this remain unclear.Citation17–Citation21 It has been suggested that the incidence of AF in African-Americans may be underreported, and that the number of African-Americans with AF might be higher if more sensitive methods for detection were used.Citation18,Citation20,Citation22 A study investigating racial differences in the incidence of and risk factors for AF in older adults found that for all associations examined, risk factors were similar in African-Americans and Caucasians, except for left ventricular posterior-wall thickness, which was more strongly associated with AF in African-Americans.Citation23
Conversely, the relative rate of stroke is higher in African-Americans than in Caucasians,Citation21 which appears to contradict the strong association between stroke and AF. One possible reason for the higher incidence and mortality rate of stroke in African-Americans may be the higher prevalence of other stroke-risk factors, including hypertension, obesity, and diabetes, in this population.Citation17,Citation19
In general, cryptogenic stroke (defined as ischemic stroke without a well-defined etiology) accounts for 34%–54% of ischemic strokes in most modern stroke registries and databases.Citation24–Citation29 Additionally, a population-based study showed that the rate of cryptogenic stroke in African-Americans was approximately double the rate observed in Caucasians (risk ratio 1.9, 95% confidence interval 1.5–2.3).Citation28 Use of sophisticated heart-monitoring techniques like implanted loop recorders might detect unrecognized paroxysmal AF as the cause of some cryptogenic strokes in African-Americans.Citation30 This suggestion is further supported by results from the REGARDS (REasons for Geographic And Racial Differences in Stroke) study, a national, population-based, longitudinal study of African-American and Caucasian adults aged at least 45 years in the US, which found that the odds of an association of stroke with race (African-American versus Caucasian) and AF progressively decreased with increasing test sensitivity.Citation22
Treatment of AF: reducing the risk of stroke with oral anticoagulants
There are many treatment options for patients with AF that aim to control irregular heart rate or prevent stroke.Citation31 Options include cardioversion, ablation, and pharmacological agents, which may be used for rate or rhythm control.Citation32 Additionally, antithrombotic therapy can be used to reduce the risk of stroke in patients with AF, and that is the focus of this article.
Antithrombotic therapy to prevent thromboembolism is recommended for all patients with AF, except those with lone AF or contraindications, and the selection of an antithrombotic agent should be based on absolute risks of stroke and bleeding and the relative risk and benefit for a given patient.Citation31
Guidelines for oral anticoagulant use in patients with AF in both the US and Europe are summarized in ;Citation2,Citation3,Citation6,Citation33,Citation34 however, it should be noted that some of these were published prior to the approval of apixaban and edoxaban.
Table 1 Guideline recommendations on the use of warfarin and novel oral anticoagulants for the prevention of stroke in patients with nonvalvular atrial fibrillation
Differences in treatment by race/ethnicity
A treatment disparity exists between African-American and Caucasian patients; however, none of the current guidelines for the prevention of stroke in patients with AF states whether any amendments to treatment should be made based on racial differences.Citation2,Citation3,Citation5,Citation6,Citation15,Citation35
African-Americans are undertreated, and thus are at an increased risk of stroke.Citation18,Citation36,Citation37 Differences in access to health care may account in part for lower rates of AF detection in African-Americans than in Caucasians. In the REGARDS study, race and income were both found to be independent predictors of patients being aware that they had AF, with African-Americans being less than a third as likely as Caucasians to be aware.Citation18 Additionally, this study found that race was an independent predictor of warfarin treatment, with the odds of African-American patients being treated with warfarin only a quarter as great as the odds for Caucasians.Citation18 A study using a multiethnic stroke-free cohort of hospitalized patients with nonrheumatic AF found that although the percentage of time on warfarin did not differ by race/ethnicity, the median percentage of time that patients spent within the therapeutic range (international normalized ratio [INR] 2.0–3.0) was lower in African-American than Caucasian patients (47.8% versus 55.2%).Citation38 Additionally, an analysis of the AFFIRM (Atrial Fibrillation Follow-up Investigation of Rhythm Management) study population found that ethnic minority status was an independent predictor of poor INR control, and race was subsequently included in a scoring system used to predict poor INR control in patients with AF treated with warfarin (SAMe-TT2R2: female sex, age <60 years, medical history [more than two comorbidities], treatment [with interacting drugs], tobacco use [doubled], and race [doubled]).Citation39
Results from the Cardiovascular Health Study, a prospective, US-based cohort study of risk factors for cardiovascular disease in community-dwelling adults aged over 65 years, found that African-Americans have poorer access to health care than Caucasians, and were more likely to have no supplemental insurance coverage.Citation40 A study investigating the differences in the type of hospital where minorities and low-income patients received care found that African-American patients and those living in low-income areas more frequently received care in teaching and safety-net hospitals and hospitals with higher bed counts, more intensive care unit beds, and emergency department volume, compared with Caucasians and those living in high-income areas.Citation41 Crude inpatient-mortality rates for patients hospitalized with acute ischemic stroke were significantly lower in African-American than Caucasian patients across all three socioeconomic status cohorts (low, medium, and high income); however, African-American patients were younger, and fewer had any form of AF.Citation41 When adjusted for risk, inpatient mortality was similar in African-American and Caucasian patients, but was significantly higher in low-income-area patients than in high-income-area patients.Citation41 Caucasian patients were more likely than African-American patients to arrive by emergency medical services, to be evaluated by a stroke team, and to have a documented National Institutes of Health Scale score.Citation42 Additionally, African-Americans were less likely to have visited a physician 1 year after their stroke than Caucasians.Citation43 Together, these results highlight the socioeconomic differences between African-American and Caucasian patients, and suggest that there is a need for better access to health care and improvements to education programs for African-American patients.
Warfarin
For over 50 years, warfarin has been the standard of care for the prevention of stroke in patients with AF, and remains the most commonly used anticoagulant in this population. A meta-analysis of six randomized controlled trials showed that warfarin reduced the risk of all strokes (ischemic and hemorrhagic) by 64% versus placebo.Citation44 Although highly efficacious for the prevention of stroke in patients with AF, warfarin has many limitations, including an increased risk of bleeding, multiple drug and food interactions, and the need for regular monitoring and dose adjustment to maintain treatment within the narrow therapeutic range (INR 2.0–3.0).Citation45 These limitations can result in the underuse of warfarin.Citation46 It has been shown that warfarin-dose requirements vary across racial/ethnic groups, with African-American patients requiring a higher dose than Caucasian patients to maintain an INR between 2.0 and 3.0.Citation47 A chart review comparing older African-American and Caucasian patients found that although the dose of warfarin required to maintain a therapeutic INR decreased with age, African-Americans required a higher maintenance dose than Caucasians.Citation48 Therefore, strategies for initiating warfarin therapy based on studies of patients of European ancestry could result in insufficient anticoagulation of older African-American patients, thereby potentially increasing their risk of thromboembolism.Citation48
Several studies have investigated the treatment disparity between African-American and Caucasian patients.Citation49–Citation51 A cohort study of Medicare beneficiaries with AF found that the use, monitoring, and effectiveness of warfarin therapy were suboptimal, especially in African-American patients.Citation49 One possible effect of this is that African-American patients with AF are at greater risk of warfarin-related intracranial hemorrhage.Citation52 Additionally, African-American patients were significantly less likely than Caucasians to fill a warfarin prescription for newly incident NVAF or to receive a warfarin prescription at hospital discharge.Citation50,Citation51
Several genetic factors have recently been identified as possible reasons why African-American patients require a higher dose of warfarin.Citation53,Citation54 Dose variability is affected by single-nucleotide polymorphisms (SNPs) in genes encoding cytochrome P450 (CYP)-2C9, which metabolizes the S-enantiomer of warfarin, and vitamin K epoxide reductase complex 1, which is the target enzyme for warfarin.Citation55,Citation56 These genotypes explain up to 30% of total variability in warfarin-dose requirements in people of European or Asian origin; however, they explain substantially less genetic variability in African-Americans (10%).Citation56 A genome-wide association study identified a novel association between an SNP in CYP2C9 (rs12777823) and warfarin-dose variability in African-American patients.Citation54 Patients carrying this SNP require a significantly lower stable dose of warfarin than those without the variant.Citation54
Novel oral anticoagulants
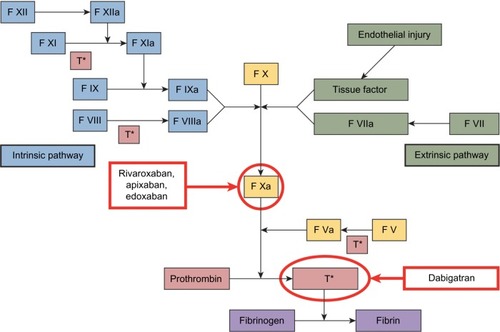
Four novel oral anticoagulants (NOACs) have recently been approved by the US Food and Drug Administration (FDA): a direct thrombin inhibitor (dabigatran), and three factor-Xa inhibitors (apixaban, edoxaban, and rivaroxaban) (). Unlike warfarin and other vitamin K antagonists, NOACs (dabigatran, rivaroxaban, apixaban, and edoxaban) do not require dose adjustments to maintain a therapeutic dose and have fewer risks of food and drug interactions.Citation57–Citation60 Lower doses of NOACs may be required based on renal function, weight, and/or age. Their predictable pharmacokinetic (PK) and pharmacodynamic profiles mean that routine monitoring is not necessary with these agents ();Citation45,Citation57–Citation61 however, no specific antidotes are currently available for the reversal of the anticoagulant effects of NOACs in the event of overdose or hemorrhagic complications.Citation57–Citation60 Several options for the reversal of the anticoagulant effects of these agents are under investigation.Citation62–Citation68
Table 2 Comparison of pharmacokinetic/pharmacodynamic interactions and dosing of warfarin and novel oral anticoagulants
In their respective Phase III trials, all of the NOACs were found to be noninferior to warfarin for reducing the risk of stroke or systemic embolism (SE) in patients with NVAF; however, only the dabigatran 150 mg twice daily (bis in die [BID]) (P<0.001) and apixaban 5 mg BID (P=0.01) dosages showed superiority ().Citation69–Citation73 Additionally, dabigatran (110 mg BID), apixaban, and edoxaban (both dosages) significantly reduced the risk of major bleeding compared with warfarin. A summary of other key end points is provided in .
Table 3 Phase III clinical trial results for the novel oral anticoagulants
There is limited information about the effect of race on NOAC treatment, and the number of patients by race was not provided in all of the NOAC Phase III trial publications.Citation69–Citation74 In an analysis of key subgroups in the ROCKET AF (Rivaroxaban Once daily oral direct factor Xa inhibition Compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation) trial, the effects of rivaroxaban versus warfarin were found to be similar across racial groups (Caucasian, African-American, Asian, other) for the outcomes of stroke or SE and major or clinically relevant nonmajor bleeding (P-values for interaction 0.486 and 0.591, respectively).Citation73 Similarly, an analysis of key subgroups in the ENGAGE AF-TIMI (Effective aNticoaGulation with factor XA next GEneration in Atrial Fibrillation – Thrombolysis In Myocardial Infarction) 48 study found that the treatment effects of both doses of edoxaban compared with warfarin were similar across racial groups (Caucasian versus non-Caucasian) for the outcomes of stroke or SE (P-values for interaction 0.28 and 0.49 for edoxaban 60 mg and 30 mg BID, respectively) and for major bleeding (P-values for interaction 0.16 and 0.34 for edoxaban 60 mg and 30 mg BID, respectively).Citation71 No subgroup analyses by race have been published for the RE-LY (Randomized Evaluation of Long-term anticoagulant therapY) or ARISTOTLE (Apixaban for Reduction In STroke and Other ThromboemboLic Events in atrial fibrillation) trials,Citation72,Citation74 and no real-world data are currently available comparing the treatment effects of NOACs by race.
The prescribing information for dabigatran and rivaroxa-ban does not state whether any dose adjustments are needed for race;Citation58,Citation60 however, based on the results of a PK study in healthy subjects that showed no difference in apixaban PK among Caucasians, Asians, and African-Americans, the apixaban prescribing information states that no dose adjustment is required based on race/ethnicity.Citation59
Role of physicians and patients in stroke prevention in patients with AF
There are disparities in stroke awareness between minority groups compared with Caucasians, including lack of awareness of stroke symptoms and signs and lack of knowledge about the need for urgent treatment and the causal role of risk factors.Citation75 The Centers for Disease Control and Prevention analyzed data from an optional module of the 2005 Behavioral Risk Factor Surveillance System that had used data from 13 US states and the District of Columbia to assess public awareness of stroke warning symptoms and the importance of seeking emergency care. The results showed that the proportion of respondents who were able to identify all five stroke warning signs and recognized the need to call emergency services was lower in African-Americans than in Caucasians (29.5% versus 41.3%).Citation76 This and other similar studies empha-size the need for educational efforts to improve knowledge about stroke symptoms among African-Americans.Citation76–Citation81
There are differences in attitudes, beliefs, and compliance among minority groups, including denial of disease, concern for potential or experienced side effects of medications, absence of symptoms, hierarchy of need, burden of filling prescriptions, attending doctor visits, and lower health literacy, all of which influence compliance with treatment.Citation78 It is also important for physicians to evaluate the effects of health literacy, access to health care, and cultural barriers to anticoagulant use.Citation82
Studies have shown that literacy decreases with age, and that this is more pronounced in African-American than Caucasian patients.Citation82 Older patients receiving oral anticoagulants must become active participants in their own care, in that they and their families must read and comprehend written information regarding their treatment.Citation82 It is also important to ensure that the reading materials supplied to patients with NVAF are sufficiently comprehensible to older adults.Citation82 This may in part be easier with NOAC than with warfarin use, due to fewer food and drug interactions associated with NOACs.
Conclusion
AF is less common in African-Americans than in Caucasians; however, African-Americans have a higher risk of stroke. This could be due to African-Americans having a higher prevalence of other stroke-risk factors compared with Caucasians, although this may be an oversimplified view, as there are a number of other reasons why this disparity may occur. These include a need for more sensitive methods of detecting AF and a need for better access to health care and patient education for African-Americans. Warfarin-dose requirements vary across racial/ethnic groups, with African-American patients requiring a higher dose than Caucasians to maintain a therapeutic INR: the NOACs seem to differ in this regard, although data are currently limited. Minority racial groups are not proportionally represented in either real-world studies or clinical trials, and as more information becomes available and other social issues are addressed, the treatment disparities between African-American and Caucasian patients should decrease.
Acknowledgments
Professional medical writing and editorial assistance was provided by Claire Hall, PhD, and Nicole Draghi, PhD, at Caudex Medical, and was funded by Bristol-Myers Squibb and Pfizer Inc.
Disclosure
The author reports grant support from Bristol-Myers Squibb and Pfizer. The author reports no other conflicts of interest in this work.
References
- American Heart AssociationWhat is atrial fibrillation?2013 Available from: http://www.heart.org/idc/groups/heart-public/@wcm/@hcm/documents/downloadable/ucm_300294.pdfAccessed October 30, 2013
- FurieKLGoldsteinLBAlbersGWOral antithrombotic agents for the prevention of stroke in nonvalvular atrial fibrillation: a science advisory for healthcare professionals from the American Heart Association/American Stroke AssociationStroke201243123442345322858728
- YouJJSingerDEHowardPAAntithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice GuidelinesChest20121412 Supple531Se575S22315271
- AlonsoAAgarwalSKSolimanEZIncidence of atrial fibrillation in whites and African-Americans: the Atherosclerosis Risk in Communities (ARIC) studyAm Heart J2009158111111719540400
- FusterVRydénLECannomDS2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelinesCirculation201112310e269e36721382897
- CammAJLipGYDe CaterinaR2012 Focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm AssociationEur Heart J201233212719274722922413
- GoASMozaffarianDRogerVLHeart disease and stroke statistics – 2013 update: a report from the American Heart AssociationCirculation20131271e6e24523239837
- FurieKLKasnerSEAdamsRJGuidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke AssociationStroke201142122727620966421
- MariniCDeSFSaccoSContribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based studyStroke20053661115111915879330
- SudlowCLWarlowCPComparable studies of the incidence of stroke and its pathological types: results from an international collaboration. International Stroke Incidence CollaborationStroke19972834914999056601
- GageBFWatermanADShannonWBoechlerMRichMWRadfordMJValidation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial FibrillationJAMA2001285222864287011401607
- LipGYNieuwlaatRPistersRLaneDACrijnsHJRefining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on Atrial FibrillationChest2010137226327219762550
- BenjaminEJWolfPAD’AgostinoRBSilbershatzHKannelWBLevyDImpact of atrial fibrillation on the risk of death: the Framingham Heart StudyCirculation199898109469529737513
- LinHJWolfPAKelly-HayesMStroke severity in atrial fibrillation. The Framingham StudyStroke19962710176017648841325
- FusterVRydénLECannomDSACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm SocietyCirculation20061147e257e35416908781
- DeitelzweigSAminAJingYMedical cost reductions associated with the usage of novel oral anticoagulants vs warfarin among atrial fibrillation patients, based on the RE-LY, ROCKET-AF and ARISTOTLE trialsJ Med Econ201215477678522449118
- GoldsteinLBBushnellCDAdamsRJGuidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke AssociationStroke201142251758421127304
- MeschiaJFMerrillPSolimanEZRacial disparities in awareness and treatment of atrial fibrillation: the REasons for Geographic and Racial Differences in Stroke (REGARDS) studyStroke201041458158720190000
- SmithSCJrClarkLTCooperRSDiscovering the full spectrum of cardiovascular disease: Minority Health Summit 2003: report of the Obesity, Metabolic Syndrome, and Hypertension Writing GroupCirculation200511110e134e13915769755
- SolimanEZPrineasRJCaseLDZhangZMGoffDCJrEthnic distribution of ECG predictors of atrial fibrillation and its impact on understanding the ethnic distribution of ischemic stroke in the Atherosclerosis Risk in Communities (ARIC) studyStroke20094041204121119213946
- WhiteHBoden-AlbalaBWangCIschemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan StudyCirculation2005111101327133115769776
- PrineasRJSolimanEZHowardGThe sensitivity of the method used to detect atrial fibrillation in population studies affects group-specific prevalence estimates: ethnic and regional distribution of atrial fibrillation in the REGARDS studyJ Epidemiol200919417718119561382
- JensenPNThackerELDublinSPsatyBMHeckbertSRRacial differences in the incidence of and risk factors for atrial fibrillation in older adults: the Cardiovascular Health StudyJ Am Geriatr Soc201361227628023320758
- Kolominsky-RabasPLWeberMGefellerONeundoerferBHeuschmannPUEpidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based studyStroke200132122735274011739965
- LeeBINamHSHeoJHKimDIYonsei Stroke Registry. Analysis of 1,000 patients with acute cerebral infarctionsCerebrovasc Dis200112314515111641577
- PettyGWBrownRDJrWhisnantJPSicksJDO’FallonWMWiebersDOIschemic stroke subtypes: a population-based study of incidence and risk factorsStroke199930122513251610582970
- SaccoRLEllenbergJHMohrJPInfarcts of undetermined cause: the NINCDS Stroke Data BankAnn Neurol19892543823902712533
- SchneiderATKisselaBWooDIschemic stroke subtypes: a population-based study of incidence rates among blacks and whitesStroke20043571552155615155974
- SchulzUGRothwellPMDifferences in vascular risk factors between etiological subtypes of ischemic stroke: importance of population-based studiesStroke20033482050205912829866
- ChristensenLMKriegerDWHøjbergSParoxysmal atrial fibrillation occurs often in cryptogenic ischaemic stroke. Final results from the SURPRISE studyEur J Neurol201421688488924628954
- AndersonJLHalperinJLAlbertNMManagement of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on Practice GuidelinesJ Am Coll Cardiol201361181935194423558044
- FergusonCInglisSCNewtonPJMiddletonSMacdonaldPSDavidsonPMAtrial fibrillation: stroke prevention in focusAust Crit Care2014272929824054541
- JanuaryCTWannLSAlpertJS2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm SocietyJ Am Coll Cardiol2014642122462280
- MeschiaJFBushnellCBoden-AlbalaBGuidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke AssociationStroke201445123754383225355838
- CammAJKirchhofPLipGYGuidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC)Eur Heart J201031192369242920802247
- IbrahimSAKwohCKHarperDLBakerDWRacial differences in the utilization of oral anticoagulant therapy in heart failure: a study of elderly hospitalized patientsJ Gen Intern Med200015213413710672118
- SchwammLHReevesMJPanWRace/ethnicity, quality of care, and outcomes in ischemic strokeCirculation2010121131492150120308617
- ShenAYYaoJFBrarSSJorgensenMBWangXChenWRacial/ethnic differences in ischemic stroke rates and the efficacy of warfarin among patients with atrial fibrillationStroke200839102736274318635860
- ApostolakisSSullivanRMOlshanskyBLipGYFactors affecting quality of anticoagulation control among patients with atrial fibrillation on warfarin: the SAMe-TT(2)R(2) scoreChest201314451555156323669885
- Henry J Kaiser Family FoundationExamining sources of supplemental insurance and prescription coverage among Medicare beneficiaries; findings from the Medicare Current Beneficiary Survey2007 Available from: http://kff.org/medicare/report/examining-sources-of-supplemental-insurance-and-prescriptionAccessed December 9, 2014
- HanchateADSchwammLHHuangWHylekEMComparison of is chemic stroke outcomes and patient and hospital characteristics by race/ethnicity and socioeconomic statusStroke201344246947623306327
- BhattacharyaPMadaFSalowich-PalmLAre racial disparities in stroke care still prevalent in certified stroke centers?J Stroke Cerebrovasc Dis201322438338822078781
- SaccoRLKargmanDEZamanilloMCRace-ethnic differences in stroke risk factors among hospitalized patients with cerebral infarction: the Northern Manhattan Stroke StudyNeurology19954546596637723951
- HartRGPearceLAAguilarMIMeta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillationAnn Intern Med20071461285786717577005
- Bristol-Myers SquibbCoumadin [prescribing information]2011 Available from: http://packageinserts.bms.com/pi/pi_coumadin.pdfAccessed October 11, 2013
- RosenmanMBSimonTATealEMcGuirePNisiDJacksonJDPerceived or actual barriers to warfarin use in atrial fibrillation based on electronic medical recordsAm J Ther201219533033722964558
- DangMTHambletonJKayserSRThe influence of ethnicity on warfarin dosage requirementAnn Pharmacother20053961008101215855242
- GarwoodCLClementeJLIbeGNKandulaVACurtisKDWhittakerPWarfarin maintenance dose in older patients: higher average dose and wider dose frequency distribution in patients of African ancestry than those of European ancestryBlood Cells Mol Dis2010451939720418129
- Birman-DeychERadfordMJNilasenaDSGageBFUse and effectiveness of warfarin in Medicare beneficiaries with atrial fibrillationStroke20063741070107416528001
- SchauerDPJohnstonJAMoomawCJWessMEckmanMHRacial disparities in the filling of warfarin prescriptions for nonvalvular atrial fibrillationAm J Med Sci20073332677317301583
- ThomasKLPicciniJPLiangLRacial differences in the prevalence and outcomes of atrial fibrillation among patients hospitalized with heart failureJ Am Heart Assoc201325e00020024072530
- ShenAYYaoJFBrarSSJorgensenMBChenWRacial/ethnic differences in the risk of intracranial hemorrhage among patients with atrial fibrillationJ Am Coll Cardiol200750430931517659197
- CavallariLHAstonJLMomaryKMShapiroNLPatelSRNutescuEAPredictors of unstable anticoagulation in African AmericansJ Thromb Thrombolysis200927443043718563532
- PereraMACavallariLHLimdiNAGenetic variants associated with warfarin dose in African-American individuals: a genome-wide association studyLancet2013382989479079623755828
- LimdiNABeasleyTMCrowleyMRVKORC1 polymorphisms, haplotypes and haplotype groups on warfarin dose among African-Americans and European-AmericansPharmacogenomics20089101445145818855533
- LimdiNAArnettDKGoldsteinJAInfluence of CYP2C9 and VKORC1 on warfarin dose, anticoagulation attainment and maintenance among European-Americans and African-AmericansPharmacogenomics20089551152618466099
- Daiichi Sankyo Co. LtdSavaysa™ (edoxaban) prescribing information2015 Available from http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/206316lbl.pdfAccessed January 22, 2015
- Boehringer IngelheimPradaxa dabigatran etexilate capsules [prescribing information] Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/022512s017lbl.pdfAccessed September 18, 2013
- Bristol-Myers SquibbEliquis® (apixaban tablets) [prescribing information]2014 Available from: http://packageinserts.bms.com/pi/pi_eliquis.pdfAccessed March 20, 2014
- Janssen PharmaceuticalsXarelto® (rivaroxaban tablets) [prescribing information]2014 Available from: http://www.xareltohcp.com/sitesdefault/files/pdf/xarelto_0.pdf#zoom=100Accessed March 8, 2014
- SongYWangXPerlsteinIBioavailability of apixaban solution formulation and crushed tablet via nasogastric tubeClin Pharmacol Ther201393Suppl 1S120S121
- Boehringer IngelheimStudy to evaluate the safety, pharmacokinetics and pharmacodynamics of BI 655075 administered alone or with dabigatran etexilate Available from: http://clinicaltrials.gov/show/NCT01688830. NLM identifier: NCT01688830Accessed June 6, 2013
- CrowtherMKittMLorenzTA phase 2 randomized, double-blind, placebo-controlled trial of PRT064445, a novel, universal antidote for direct and indirect factor Xa inhibitors [Abstract]J Thromb Haemost201311Suppl 230
- CrowtherMMathurVKittMA phase 2 randomized, double-blind, placebo-controlled trial demonstrating reversal of rivaroxaban-induced anticoagulation in healthy subjects by andexanet alfa (PRT064445), an antidote for FXa inhibitorsPoster presented at: 55th ASH Annual Meeting and ExpositionDecember 7–10, 2013New Orleans, LA
- HollenbachSJLuGTanSPRT064445 but not recombinant FVIIa reverses rivaroxaban induced anticoagulation as measured by reduction in blood loss in a rabbit liver laceration modelPoster presented at: 54th ASH Annual Meeting and ExpositionDecember 8–11, 2012Atlanta, GA
- LaulichtBBakhruSLeeCSmall molecule antidote for anticoagulantsCirculation2012126A11395
- PerospherePER977: an anticoagulant reversal agent2013 Available from: http://perosphere.com/content/research/per977.htmAccessed June 6, 2013
- van RynJLitzenburgerTWatermanADabigatran anticoagulant activity is neutralized by an antibody selective to dabigatran in in vitro and in vivo modelsJ Am Coll Cardiol20115714 Suppl 1E1130
- ConnollySJEzekowitzMDYusufSDabigatran versus war-farin in patients with atrial fibrillationN Engl J Med2009361121139115119717844
- ConnollySJEzekowitzMDYusufSReillyPAWallentinLNewly identified events in the RE-LY trialN Engl J Med2010363191875187621047252
- GiuglianoRPRuffCTBraunwaldEEdoxaban versus warfa-rin in patients with atrial fibrillationN Engl J Med2013369222093210424251359
- GrangerCBAlexanderJHMcMurrayJJApixaban versus war-farin in patients with atrial fibrillationN Engl J Med20113651198199221870978
- PatelMRMahaffeyKWGargJRivaroxaban versus warfa-rin in nonvalvular atrial fibrillationN Engl J Med20113651088389121830957
- ConnollySJEikelboomJJoynerCApixaban in patients with atrial fibrillationN Engl J Med2011364980681721309657
- Cruz-FloresSRabinsteinABillerJRacial-ethnic disparities in stroke care: the American experience: a statement for healthcare professionals from the American Heart Association/American Stroke AssociationStroke20114272091211621617147
- Centers for Disease Control and PreventionAwareness of stroke warning symptoms – 13 states and the District of Columbia, 2005MMWR Morb Mortal Wkly Rep2008571848148518463605
- GreenlundKJNeffLJZhengZJLow public recognition of major stroke symptomsAm J Prev Med200325431531914580633
- LutfiyyaMNLipskyMSBalesRWChaIMcGrathCDisparities in knowledge of heart attack and stroke symptoms among adult men: an analysis of behavioral risk factor surveillance survey dataJ Natl Med Assoc2008100101116112418942272
- LutfiyyaMNCumbaMTMcCulloughJEBarlowELLipskyMSDisparities in adult African American women’s knowledge of heart attack and stroke symptomatology: an analysis of 2003–2005 Behavioral Risk Factor Surveillance Survey dataJ Womens Health (Larchmt)200817580581318479229
- LutfiyyaMNNgLAsnerNLipskyMSDisparities in stroke sympto-mology knowledge among US midlife women: an analysis of population survey dataJ Stroke Cerebrovasc Dis200918215015719251192
- ZerwicJHwangSYTuccoLInterpretation of symptoms and delay in seeking treatment by patients who have had a stroke: exploratory studyHeart Lung2007361253417234474
- WilsonFLRacineETekieliVWilliamsBLiteracy, readability and cultural barriers: critical factors to consider when educating older African Americans about anticoagulation therapyJ Clin Nurs200312227528212603561