Abstract
Background
There is limited literature investigating preoperative physical therapy (pre-op PT) treatment on pain intensity and disability after musculoskeletal surgery. The purposes of the present cohort study were to describe patient characteristics for those who had and did not have pre-op PT treatment and determine whether pre-op PT influenced the length of postoperative physical therapy (post-op PT) treatment (number of sessions) and 3-month and 6-month postsurgical outcomes, such as pain intensity and disability.
Patients and methods
A total of 124 patients (mean age =43 years, 81 males) with shoulder pain were observed before and after shoulder arthroscopic surgery. Demographic data, medical history, and validated self-report questionnaires were collected preoperatively and at 3 months and 6 months after surgery. Analysis of variance models were performed to identify differences across measures for patients who had pre-op PT treatment and those who did not and to examine outcome differences at 3 months and 6 months. Alpha was set at the 0.05 level for statistical significance.
Results
Males had less participation in pre-op PT than females (P=0.01). In contrast, age, pain intensity, disability, and pain-associated psychological factors did not differ between pre-op PT treatment groups (P>0.05). Subacromial bursectomies were more commonly performed in patients having pre-op PT treatment (P<0.05). Pre-op PT treatment did not influence length of post-op PT treatment and did not affect 3-month and 6-month pain intensity and disability outcomes. Differences in distribution of pre-op PT for males and females and subacromial bursectomy did not influence 3-month or 6-month postsurgical outcomes.
Conclusion
Receiving pre-op PT treatment did not influence post-op PT treatment or pain and disability outcomes at 3 months and 6 months. This prospective cohort study provides no evidence of benefit for pre-op PT on post-op PT treatment or postsurgical outcomes. Females or patients receiving certain surgical procedures are more likely to undergo pre-op PT treatment. However, these differences did not influence postoperative outcomes in this cohort.
Introduction
Although there is a relatively large body of knowledge assessing postoperative physical therapy (post-op PT),Citation1–Citation6 there is limited literature investigating preoperative physical therapy (pre-op PT) on pain intensity and disability after musculoskeletal surgery.
The main goal of pre-op PT treatment is to reduce postoperative complications and improve postoperative outcomes.Citation7 However, previous literature shows that isolating the real impact of a preoperative rehabilitation is not easy, mainly because of the heterogeneity in the type of the physical therapy (PT) intervention.Citation8 In cases, such as cardiac, thoracic, and abdominal surgeries, the main goal of pre-op PT is to improve the physiological capacity of the individual. In this case, it seems that strengthening the inspiratory muscle prior to surgery may result in fewer postoperative complications and shorter postoperative length of stay, enhance functional capacity,Citation9,Citation10 improve the quality of life, and reduce postoperative pain and complications.Citation11
The reported effects of pre-op PT intervention on postoperative outcomes in patients having elective musculoskeletal surgeries are conflicting. A systematic review including functional measures as outcome measures concluded that preoperative exercise programs were not effective on postoperative outcomes on total knee or total hip arthroplasty.Citation12 On the other hand, preoperative level of function is predictive of postoperative outcome after lower limb arthroplasty, where patients with better function preoperatively had better function postoperatively.Citation13 Moreover, the authorsCitation8,Citation14 have recommended a multidisciplinary preoperative rehabilitation program before total hip and knee arthroplasty to reduce hospital length of stay and modify discharge conditions.
Reported evidence on the effects of pre-op PT intervention on general postoperative outcomes for musculoskeletal pain is inconclusive,Citation15 and few studies have investigated this issue for shoulder arthroscopy. Arthroscopy of the shoulder is a common musculoskeletal surgery and has become widely accepted as a diagnostic and therapeutic tool in the management of shoulder disordersCitation1,Citation16,Citation17; however, data describing postoperative outcomes following pre-op PT interventions are scarce.
This topic is important because whether pre-op PT intervention influences postoperative outcomes may assist in decision making for optimal timing of rehabilitation in the operative management of shoulder pain. Therefore, the purposes of this prospective study were to 1) identify differences in demographic, clinical, surgical type, and psychological characteristics between patients having and not having pre-op PT treatment and 2) determine whether having pre-op PT influences the length of post-op PT treatment (number of sessions) and 3-month and 6-month postsurgical outcomes (pain intensity and disability). We hypothesized that 1) there would be a difference between patients having and not having pre-op PT in demographic, clinical, surgical types and psychological characteristics and 2) having pre-op PT would favorably influence the length of post-op PT treatment and 3-month and 6-month postsurgical outcomes.
Patients and methods
Patients
The University of Florida’s Institutional Review Board for human participants approved this study. This prospective design includes data from consecutive patients seeking operative treatment of shoulder pain, where procedures were limited to arthroscopy of the glenohumeral joint or distal clavicle. Specific operative procedures included rotator cuff repair, adhesive capsulitis, acromioplasty, and labral repair (). Patients were recruited by participating physicians and provided written informed consent before participating in this study.
Table 1 Demographic and psychological characteristics and summary of medical history between patients having and not having pre-op PT treatment
Inclusion criteria
The inclusion criteria for being a participant were as follows: 1) aged between 18 years and 85 years; 2) complained of pain limited to anterior, lateral, or posterior shoulder; 3) documented or suspected rotator cuff tendinopathy (evidence from clinical examination or imaging studies), including small (<1 cm), medium (1–3 cm), and large (3–5 cm) tears; 4) documented or suspected adhesive capsulitis (evidence from clinical examination or imaging studies); 5) documented or suspected superior labrum from anterior to posterior lesion (evidence from clinical examination or imaging studies); 6) shoulder instability (anterior or posterior labral lesions); and 7) scheduled for arthroscopic surgery.
Exclusion criteria
The exclusion criteria were as follows: 1) current complaints of pain lasting longer than the past 3 months involving neck, elbow, hand, low back, hip, knee, or ankle; 2) massive rotator cuff tear (>5 cm); 3) documented shoulder osteoarthritis or rheumatoid arthritis; 4) prior shoulder surgery within the past year or currently complaining of pain from prior shoulder surgery; 5) current shoulder fracture, tumor, or infection; 6) previously diagnosed chronic pain disorder (including, but not limited to, irritable bowel syndrome, fibromyalgia, temporomandibular disorders, and chronic low back pain); 7) current psychiatric management; and 8) current gastrointestinal or renal illness.Citation18
Overall procedure
After signing the informed consent, study participants completed a standard intake information form. Patients underwent baseline assessments, which included psychological questionnaires, and self-reported pain intensity and disability 24–48 hours before shoulder surgery. Patients underwent an arthroscopic procedure affecting the glenohumeral joint and/or distal clavicle. Specific operative procedures included acromioplasty, subacromial bursectomy, labral repair, rotator cuff repair, and others (which included, but was not limited to, capsulorrhaphy, coracoacromial ligament release, stabilization, and Bankart). In addition, the size of the rotator cuff tear was recorded from the operative report, ranging from “no tear” to “massive tear”. Four different surgeons operated on all the patients in this cohort. After 3 months and 6 months from the surgical procedure, patients were reassessed on all measures.
Measures
Demographic and historical information
Study participants completed a standard intake information form. Demographic data collected at initial evaluation included sex, age, employment status, litigation status, marital status, educational level, and health history. Historical data included the type of onset of symptoms, the length of time of the symptoms, the number of previous episodes of musculoskeletal pain, and previous PT treatment for their shoulder.
Pre-op PT and post-op PT measurements
Study participants were asked if they had had previous PT treatments (under the supervision of a licensed physical therapist) for their shoulder condition in the last 6 months. Participants who attended presurgical treatment were classified as “having pre-op PT treatment”, and those who did not attend were classified as “not having pre-op PT treatment”. Since the main goal of this study was to pragmatically determine whether having or not having pre-op PT intervention would influence postsurgical outcome, the frequency, intensity, and type of the pre-op PT were not tracked. At 3 months and 6 months, patients were asked for the total number of sessions (and weeks) of post-op PT treatment that they had after shoulder surgery.
Shoulder pain intensity
Shoulder pain intensity was assessed with the Brief Pain Inventory (BPI),Citation19 which includes a numerical rating scale for pain intensity. Patients rated their pain intensities over the following three conditions: the present pain intensity, the worst pain intensity over the past 24 hours, and the least pain intensity over the past 24 hours. These three ratings were summed and divided by three for use in data analyses.Citation20 Studies have shown that this aggregate measure has sufficient psychometric strengths.Citation20,Citation21
Shoulder disability
Disability was assessed with the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire.Citation22 The DASH questionnaire includes 30 items to measure the extent to which patients’ pain or limited activity affects their ability to perform certain functions, to sleep, and to carry on routine daily activities and social activities. The DASH questionnaire has been validated for the assessment of shoulder disorders.Citation23–Citation25
Psychological factors
A previous study from our group has shown that pain catastrophizing and depressive symptoms were relevant psychological factors in predicting the postoperative clinical pain intensity in a population with similar characteristics.Citation18 Therefore, for our current study, we selected the same psychological factors to explore if pre-op PT has an influence on psychological factors.
Depressive symptoms
Self-reports of depressive symptoms were measured using the patient health questionnaire (PHQ-9).Citation26 The PHQ-9 is a 9-item self-report questionnaire designed to evaluate the presence of depressive symptoms during the prior 2 weeks. As a severity measure, scores can range from 0 (absence of depressive symptoms) to 27 (severe depressive symptoms). Each of the nine items, asking for each of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnostic criteria, can be scored from 0 (not at all) to 3 (nearly every day). As a diagnostic measure, major depression is diagnosed if five or more of the nine depressive symptom criteria have been present at least “more than half the days” (a score of 2) in the past 2 weeks, and one of the symptoms is depressed mood or anhedonia. A previous study supports the PHQ-9’s validity, feasibility, and capacity to detect changes in depressive symptoms over time.Citation27
Pain catastrophizing
Pain catastrophizing was measured by the pain catastrophizing scale (PCS).Citation28 The PCS has 13 descriptions of pain experience assessing catastrophic cognitions, for example, “I feel I can’t go on”, and “There’s nothing I can do to reduce the intensity of the pain”. Patients were asked to indicate whether they agreed with these statements by using a five-point rating scale (0, “not at all” to 4, “all the time”) to rate the frequency of these cognitions. A PCS sum score was calculated for all items (range, 0–52), with a high score indicating a high level of pain catastrophizing.
Data analysis
Data analysis was conducted with SPSS, Version 18.0. Significance levels were set a priori at P<0.05 for all comparisons. Descriptive statistics (mean and standard deviation) were calculated for all variables for baseline, 3 months, and 6 months between groups (patients who had pre-op PT treatment and those who did not). The proportion of patients and the sex distribution between each group were determined. The distributions of variables were tested for normality by visual examination and with Kolmogorov–Smirnov test before conducting analyses.
Analysis of variance (ANOVA) models and the Mann–Whitney U test were performed to identify differences across all measures for patients who had pre-op PT treatment and those who did not. Multivariate ANOVA models were performed to examine outcome differences at 3 months and 6 months (pain intensity and disability) and the length of post-op PT (number of PT sessions after shoulder surgery) on patient characteristics observed to be significantly different between groups.
Results
This study included 124 consecutive patients having arthroscopic surgery with a completed 6-month follow-up. Descriptive statistics for the demographic and psychological characteristics, clinical pain, and medical history between patients who had pre-op PT treatment and those who did not is summarized in . All continuously dependent variables were found to approximate a normal distribution by visual examination and were deemed appropriate for our planned analyses and ANOVAs.
Differences between preoperative groups
No significant baseline differences (P>0.05) in age, pain intensity, disability, and psychological factors between patients having and not having pre-op PT treatment were observed (). However, sex significantly differed (P=0.01) between patients having and not having pre-op PT treatment. Proportionally, more men were in the not having pre-op PT treatment group (59%), and more women were in the having pre-op PT treatment group (65%). Size of rotator cuff tear (P=0.56) had no significant difference between patients having and not having pre-op PT treatment. Differences in surgical type were further explored between patients having and not having pre-op PT treatment. Significantly, more subacromial bursectomies were performed (37.7%) in patients having pre-op PT treatment compared to patients not having pre-op PT treatment (20.6%) ().
Influence of pre-op PT on outcomes
There was no significant difference in the length of post-op PT treatment at 3 months (F[1,96]=0.37; P=0.54) and at 6 months (F[1,81]=0.26; P=0.61) between patients having and not having pre-op PT treatment.
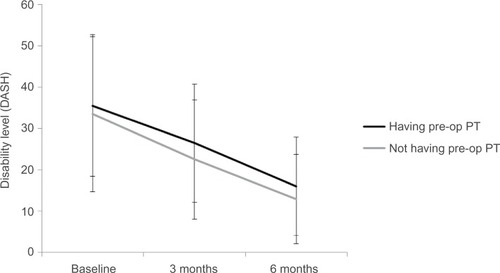
Repeated measures of ANOVA examined changes in clinical pain intensity and disability between patients having and not having pre-op PT treatment. Results showed no time × group interaction for clinical pain intensity (F[2,180]=0.33; P=0.72); as expected, there was a significant main effect of clinical pain over time (F[2,180]=64.41; P<0.001), where pain significantly decreased from baseline (mean =3.33; SD =2.33) to 3 months (mean =1.52; SD =1.61) and from 3 months to 6 months (mean =1.17; SD =1.45) ().
Figure 1 Clinical pain over time between patients having pre-op PT treatment and patients not having pre-op PT treatment.
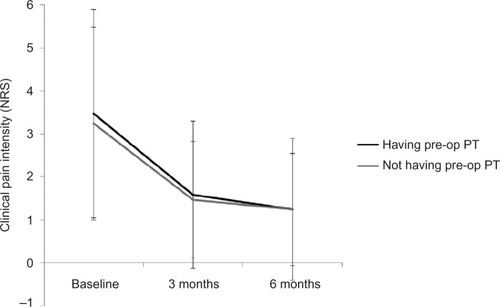
In addition, no time × group interaction for disability was found (F[2,192] =0.69; P=0.49); as expected, there was a significant main effect of disability over time (F[2, 192]=73.16; P<0.001), where disability significantly decreased from baseline (mean =34.18; SD =17.08) to 3 months (mean =24.67; SD =14.51) and from 3 months to 6 months (mean =13.75; SD =10.39) ().
Exploratory analysis
Since significant differences at baseline were found for the distribution of sex and subacromial bursectomy between patients having and not having pre-op PT treatment, an exploratory analysis of these results was performed. Differences in demographic, clinical pain, medical history, and psychological characteristics between sex and subacromial bursectomy are summarized in . Significant differences were found in baseline clinical pain intensity (BPI) (t[118]=2.57; P=0.01) and baseline disability (DASH) (t[122]=4.05; P<0.01) between males and females, where females had higher mean in both clinical outcome measures (BPI mean =4.09; DASH mean =42.97) compared to males (BPI mean =2.97; DASH mean =30.05) (). Patients who had bursectomy were significantly older (t[122)=–3.37; P<0.01) and predominantly females (41.8% for females vs 22% for males). Repeated measures of ANOVA were used to assess whether pre-op PT treatment differences in sex or subacromial bursectomy affected postsurgical outcomes. No significant interaction was found between pre-op PT treatment, sex, and pain intensity (baseline, 3 months, and 6 months) (F[2,176]=0.06; P=0.93) or between pre-op PT treatment, sex, and disability (F[2,188]=1.38; P=0.26), suggesting that the potential effect of pre-op PT treatment on the length of post-op PT and clinical outcomes did not differ between males and females. The same trend of results was found between pre-op PT treatment, bursectomy, and pain intensity or disability, suggesting that differences in surgical intervention do not influence 3-month or 6-month postsurgical outcomes.
Table 2 Exploratory analyses – differences in demographic and psychological characteristics between sex and subacromial bursectomy
Discussion
The main goal of pre-op PT treatment is to reduce postoperative complications and improve postoperative outcomes.Citation8 This study identified differences in demographic, clinical, and psychological characteristics between patients having and not having pre-op PT treatment and determined that pre-op PT treatment did not influence postoperative outcomes. The only pre-op PT treatment differences observed in this cohort were that males had less participation in pre-op PT treatment than females, and significantly more subacromial bursectomies were performed in patients having pre-op PT treatment. The results of this study also indicated that pre-op PT treatment did not influence the length of post-op PT treatment or postoperative pain and disability outcomes. Our study is a new addition to the small body of literature investigating this topic in elective arthroscopic shoulder surgery and extends the work from different surgical cohorts.Citation29–Citation31 In addition, the larger sample size and prospective design are other strengths of this study.
The results from several studies have showed the positive effects of pre-op PT treatment on postsurgical outcomes in patients undergoing cardiac surgery and in patients after lung volume reduction surgery.Citation32,Citation33 However, the results from studies looking at the effect of pre-op PT on postsurgical outcomes after musculoskeletal or joint replacement surgery have been contradictory.Citation8 For example, Beaupre et alCitation34 showed no differences in knee measurements (range of motion [ROM] and strength), pain, function, or quality of life between patients having a preoperative exercise/education program and patients having a total knee arthroplasty. Rooks et alCitation35 evaluated the effect of a short preoperative exercise intervention on the functional status, pain, and muscle strength of patients before and after total joint arthroplasty. They found that hip and knee arthroplasty patients responded differently in the preoperative and immediate postoperative periods. D’Lima et alCitation30 compared the effects of pre-op PT of general cardiovascular conditioning exercises with the routine procedure of no pre-op PT in patients undergoing primary total knee replacement. All three groups showed significant improvement postoperatively; however, neither type of preoperative exercise added to the degree of improvement after surgery. In contrast, Crowe and HendersonCitation36 showed the effectiveness in reducing the length of stay after an individually tailored rehabilitation program for patients undergoing hip or knee arthroplasty. Our results add to this literature by suggesting that in a cohort of patients undergoing shoulder arthroscopy, there appears to be no benefit of pre-op PT treatment on postsurgical pain and disability outcomes. Overall, this finding is in-line with previous studies,Citation29–Citation31 indicating that a beneficial effect of pre-op PT treatment is more likely to occur after major surgeries.Citation14
One potential explanation for the differences in the benefits of pre-op PT is that the recovery period after invasive and major surgeries involves bed rest and sometimes long periods of physical inactivity, which induces deconditioning and postoperative complications. Therefore, it is reasonable to assume that increasing a patient’s physical activity and physiological parameters prior to a surgical intervention will increase the patient’s functional capacity with an increase in quality of life. Previous studies have shown that poor fitness before the surgery results in a significantly longer stay in hospital after the surgeryCitation37,Citation38 and greater surgical complications.Citation8,Citation37 However, the “standard of care” pre-op PT intervention for shoulder conditions would not target the increment in physiological parameters or fitness improvement; therefore, the chance of overall fitness improvement is low. Even though an ambulatory surgery such as a shoulder arthroscopy may not involve bed rest or long periods of inactivity, there is often a period of immobility considered as a “relative rest” that could eliminate any potential benefits from pre-op PT. Looking at sex differences, Charousset et alCitation39 described that female sex was negatively associated with the improvement of clinical results. Other studiesCitation40,Citation41 have reported that sex is not associated with postoperative outcomes. Our results are consistent with earlier findings, because even though males had less participation in pre-op PT treatment than females, baseline sex differences did not influence the length of post-op PT treatment, pain intensity, and disability outcomes.
Psychological factors are believed to play a role in the patient’s response to treatment and final outcome.Citation42–Citation44 However, there is little evidence in the literature assessing the potential influence of psychological characteristics on seeking PT care. Our data show that depression and pain catastrophizing did not differ at baseline between patients having or not having pre-op PT treatment. This is an interesting finding because we would expect that patients with greater psychological distress would be more likely to utilize pre-op PT; however, this was not the case for this cohort. Therefore, this is preliminary evidence that pre-op PT is not associated with common measures of psychological distress that have been associated with an increased health care utilization for musculoskeletal pain.
A previous studyCitation45 has shown that after a conservative treatment for subacromial impingement syndrome has failed, there is a greater rate of successful outcome with a specific exercise protocol (strengthening eccentric exercises for the rotator cuff and concentric/eccentric exercises for the scapula stabilizers in combination with manual mobilization) compared to a control exercise group. In addition, a significantly lower proportion of patients in the specific exercise group subsequently chose to undergo surgery. Lee et alCitation5 show that pain, range of motion, muscle strength, and function significantly improved after arthroscopic rotator cuff repair, regardless of early postoperative rehabilitation protocols. The goal of this study was to evaluate the broad influence of having pre-op PT on postoperative outcomes and not to test the effectiveness of any specific exercise approaches used during PT. These results still advance the field by showing that pain intensity and disability significantly potentially decrease after shoulder arthroscopy, regardless of having or not having preoperative rehabilitation. Future research using more highly controlled designs is needed, however, to determine if specific exercise approaches have measurable impact on postoperative outcomes.
There are some limitations to this study that should be recognized. First, the operational definition of PT treatment was pragmatically determined, so it does not include treatment dosage or type, so we cannot account for the intensity, frequency, or nature of the PT delivered in this study. This is a relevant issue because the nature of the preoperative intervention may be an important consideration, so that future prospective studies can better measure the application of pre-op PT. Furthermore and consistent with the pragmatic nature of the analysis, there was no control over how the pre-op PT was selected or administered, and there could be other relevant factors in the patient decision making (eg, protocol selection, access to care, socioeconomic status, dosage, and content of treatment) that were not included in our analysis. Second, by recruiting patients who are having surgery, we may be missing patients who already succeeded with conservative treatment approaches; therefore, our sample may be less likely to have had a positive response to PT treatment in general. A more comprehensive future study including a wider range of patients to determine whether pre-op PT is preventative of future surgery is needed, as this study was not designed to answer that particular question.
Despite these limitations, this study represents a new contribution to the literature by investigating the influence of pre-op PT treatment on 3-month and 6-month postsurgical outcomes. In summary, having pre-op PT was not associated with the length of post-op PT treatment or postsurgical pain and disability.
Conclusion
This prospective cohort study provides no evidence of benefit for pre-op PT on post-op PT treatment or postsurgical outcomes. Receiving pre-op PT treatment did not influence the length of post-op PT treatment or pain and disability outcomes at 3 months and 6 months. Females or patients receiving certain surgical procedures are more likely to undergo pre-op PT treatment. However, these differences did not influence postsurgical outcomes in this cohort.
Acknowledgments
The authors thank Warren Greenfield III for his assistance with clinical participant screening and recruitment. Doctor Deenesh T Sahajpal provided patients from his clinic. The authors also wish to thank Lindsay Kindler for assistance with testing. This study was supported by Grant #AR055899 from NIAMS/NIH.
Disclosure
The authors report no conflicts of interest in this work.
References
- BhatiaSMatherRC3rdHsuARArthroscopic management of recalcitrant stiffness following rotator cuff repair: a retrospective analysisIndian J Orthop201347214314923682175
- CuffDJPupelloDRProspective randomized study of arthroscopic rotator cuff repair using an early versus delayed postoperative physical therapy protocolJ Shoulder Elbow Surg201221111450145522554876
- HolmgrenTObergBSjobergIJohanssonKSupervised strengthening exercises versus home-based movement exercises after arthroscopic acromioplasty: a randomized clinical trialJ Rehabil Med2012441121822124602
- BukerNKitisAAkkayaSAkkayaNArtroskopik yardımlı mini-açık yöntem ile rotator manşet tamiri yapılan hastalarda gözetimli fizyoterapi programı ile ev egzersiz programının sonuçlarının karşılaştırılması [Comparison of the results of supervised physiotherapy program and home-based exercise program in patients treated with arthroscopic-assisted mini-open rotator cuff repair]Eklem Hastalik Cerrahisi201122313413922085347
- LeeBGChoNSRheeYGEffect of two rehabilitation protocols on range of motion and healing rates after arthroscopic rotator cuff repair: aggressive versus limited early passive exercisesArthroscopy2012281344222014477
- HensleyCPSumJPhysical therapy intervention for a former power lifter after arthroscopic microfracture procedure for grade iv glenohumeral chondral defectsInt J Sports Phys Ther201161102621655454
- DiercksRLStevensMGentle thawing of the frozen shoulder: a prospective study of supervised neglect versus intensive physical therapy in seventy-seven patients with frozen shoulder syndrome followed up for two yearsJ Shoulder Elbow Surg200413549950215383804
- CoudeyreEJardinCGivronPRibinikPRevelMRannouFCould preoperative rehabilitation modify postoperative outcomes after total hip and knee arthroplasty? Elaboration of French clinical practice guidelinesAnn Readapt Med Phys200750318919717343953
- BayramASCandanTGebitekinCPreoperative maximal exercise oxygen consumption test predicts postoperative pulmonary morbidity following major lung resectionRespirology200712450551017587416
- LoewenGMWatsonDKohmanLPreoperative exercise Vo2 measurement for lung resection candidates: results of cancer and leukemia group B protocol 9238J Thorac Oncol20072761962517607117
- NagamatsuYShimaIYamanaHFujitaHShirouzuKIshitakeTPreoperative evaluation of cardiopulmonary reserve with the use of expired gas analysis during exercise testing in patients with squamous cell carcinoma of the thoracic esophagusJ Thorac Cardiovasc Surg200112161064106811385372
- AckermanINBennellKLDoes pre-operative physiotherapy improve outcomes from lower limb joint replacement surgery? A systematic reviewAust J Physiother2004501253014987189
- FortinPRClarkeAEJosephLOutcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgeryArthritis Rheum19994281722172810446873
- GilbeyHJAcklandTRWangAWMortonARTrouchetTTapperJExercise improves early functional recovery after total hip arthroplastyClin Orthop Relat Res200340819320012616059
- ValkenetKvan de PortIGDronkersJJde VriesWRLindemanEBackxFJThe effects of preoperative exercise therapy on postoperative outcome: a systematic reviewClin Rehabil20112529911121059667
- Archetti NettoNTamaokiMJLenzaMTreatment of Bankart lesions in traumatic anterior instability of the shoulder: a randomized controlled trial comparing arthroscopy and open techniquesArthroscopy201228790090822342199
- PaxtonESBackusJKeenerJBrophyRHShoulder arthroscopy: basic principles of positioning, anesthesia, and portal anatomyJ Am Acad Orthop Surg201321633234223728958
- ValenciaCFillingimRBGeorgeSZSuprathreshold heat pain response is associated with clinical pain intensity for patients with shoulder painJ Pain201112113314020692209
- CleelandCSRyanKMPain assessment: global use of the Brief Pain InventoryAnn Acad Med Singapore19942321291388080219
- JensenMPTurnerLRTurnerJARomanoJMThe use of multiple-item scales for pain intensity measurement in chronic pain patientsPain199667135408895229
- JensenMPTurnerJARomanoJMFisherLDComparative reliability and validity of chronic pain intensity measuresPain199983215716210534586
- BeatonDEKatzJNFosselAHWrightJGTarasukVBombardierCMeasuring the whole or the parts? Validity, reliability, and responsiveness of the disabilities of the arm, shoulder and hand outcome measure in different regions of the upper extremityJ Hand Ther200114212814611382253
- BeatonDRichardsRRAssessing the reliability and responsiveness of 5 shoulder questionnairesJ Shoulder Elbow Surg1998765655729883415
- GummessonCAtroshiIEkdahlCThe disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgeryBMC Musculoskelet Disord200341112809562
- MacDermidJCDrosdowechDFaberKResponsiveness of self-report scales in patients recovering from rotator cuff surgeryJ Shoulder Elbow Surg200615440741416831642
- MichaelESBurnsJWCatastrophizing and pain sensitivity among chronic pain patients: moderating effects of sensory and affect focusAnn Behav Med200427318519415184094
- GreenlandSKleinbaumDGCorrecting for misclassification in two-way tables and matched-pair studiesInt J Epidemiol198312193976840961
- SullivanMJBishopSRPivikJThe pain catastrophizing scale: development and validationPsychol Assess19957524532
- RodgersJAGarvinKLWalkerCWMorfordDUrbanJBedardJPreoperative physical therapy in primary total knee arthroplastyJ Arthroplasty19981344144219645522
- D’LimaDDColwellCWJrMorrisBAHardwickMEKozinFThe effect of preoperative exercise on total knee replacement outcomesClin Orthop Relat Res19963261741828620638
- WeidenhielmLMattssonEBrostromLAWersall-RobertssonEEffect of preoperative physiotherapy in unicompartmental prosthetic knee replacementScand J Rehabil Med199325133398465163
- BobbioAChettaAAmpolliniLPreoperative pulmonary rehabilitation in patients undergoing lung resection for non-small cell lung cancerEur J Cardiothorac Surg2008331959818006327
- JonesLWPeddleCJEvesNDEffects of presurgical exercise training on cardiorespiratory fitness among patients undergoing thoracic surgery for malignant lung lesionsCancer2007110359059817582629
- BeaupreLALierDDaviesDMJohnstonDBThe effect of a preoperative exercise and education program on functional recovery, health related quality of life, and health service utilization following primary total knee arthroplastyJ Rheumatol20043161166117315170931
- RooksDSHuangJBierbaumBEEffect of preoperative exercise on measures of functional status in men and women undergoing total hip and knee arthroplastyArthritis Rheum200655570070817013852
- CroweJHendersonJPre-arthroplasty rehabilitation is effective in reducing hospital stayCan J Occup Ther2003702889612704972
- CookJWPiersonLMHerbertWGThe influence of patient strength, aerobic capacity and body composition upon outcomes after coronary artery bypass graftingThorac Cardiovasc Surg2001492899311339458
- WhitneyJAParkmanSPreoperative physical activity, anesthesia, and analgesia: effects on early postoperative walking after total hip replacementAppl Nurs Res2002151192711840406
- CharoussetCGrimbergJDuranthonLDBellaicheLPetroverDKalraKThe time for functional recovery after arthroscopic rotator cuff repair: correlation with tendon healing controlled by computed tomography arthrographyArthroscopy2008241253318182198
- FengSGuoSNobuharaKHashimotoJMimoriKPrognostic indicators for outcome following rotator cuff tear repairJ Orthop Surg (Hong Kong)200311211011614676334
- ManakaTItoYMatsumotoITakaokaKNakamuraHFunctional recovery period after arthroscopic rotator cuff repair: is it predictable before surgery?Clin Orthop Relat Res201146961660166621107925
- GeorgeSZWallaceMRWrightTWEvidence for a biopsychosocial influence on shoulder pain: pain catastrophizing and catechol-O-methyltransferase (COMT) diplotype predict clinical pain ratingsPain20081361–2536117686583
- GeorgeSZHirshATPsychologic influence on experimental pain sensitivity and clinical pain intensity for patients with shoulder painJ Pain200910329329919070551
- HillJCFritzJMPsychosocial influences on low back pain, disability, and response to treatmentPhys Ther201191571272121451093
- HolmgrenTBjornsson HallgrenHObergBAdolfssonLJohanssonKEffect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled studyBMJ2012344e78722349588