Abstract
Background and objective
In previous short-term and 2-year follow-ups, a pain and stress self-management group intervention (PASS) had better effect on pain-related disability, self-efficacy, catastrophizing, and perceived pain control than individually administered physiotherapy (IAPT) for patients with persistent tension-type neck pain. Studies that have evaluated long-term effects of self-management approaches toward persistent neck pain are sparse. The objective of this study was to compare pain-related disability, self-efficacy for activities of daily living (ADL), catastrophizing, pain, pain control, use of analgesics, and health care utilization in people with persistent tension-type neck pain 9 years after they received the PASS or IAPT.
Materials and methods
Of 156 people (PASS, n = 77; IAPT, n = 79) originally included in a randomized controlled trial, 129 people (PASS, n = 63; IAPT, n = 66) were eligible and were approached for the 9-year follow-up. They were sent a self-assessment questionnaire, comprising the Neck Disability Index, the Self-Efficacy Scale, the Coping Strategies Questionnaire, and questions regarding pain, analgesics, and health care utilization. Mixed linear models for repeated measures analysis or generalized estimating equations were used to evaluate the differences between groups and within groups over time (baseline, previous follow-ups, and 9-year follow-up) and the interaction effect of “time by group”.
Results
Ninety-four participants (73%) responded (PASS, n = 48; IAPT, n = 46). At 9 years, PASS participants reported less pain-related disability, pain at worst, and analgesics usage, and a trend toward better self-efficacy compared to IAPT participants. There was a difference between groups in terms of change over time for disability, self-efficacy for ADL, catastrophizing, perceived pain control, and health care visits in favor of PASS. Analyses of simple main effects at 9 years showed that the PASS group had less disability (p = 0.006) and a trend toward better self-efficacy (p = 0.059) than the IAPT group.
Conclusion
The favorable effects on pain-related disability of PASS were sustained 9 years after the intervention.
Introduction
Musculoskeletal neck pain of extended duration is common, affecting approximately one-fifth of the adult population.Citation1,Citation2 Of people who experience neck pain at some time point, almost 50% will report recurring or persistent pain complaints some years later.Citation3,Citation4
Founded in a biopsychosocial perspective on pain, there is a growing awareness of the significance of applying cognitive–behavioral principles in pain rehabilitation in primary health care (PHC).Citation5,Citation6 Rehabilitation strategies that address cognitive and behavioral factors involved in the maintenance of musculoskeletal pain by promoting active pain-coping skills and self-management have shown to have a beneficial effect on pain-related disability.Citation7–Citation9 The rationale for self-management interventions is to induce health behavior changes that are assumed to produce sustainable long-term effects on disability.Citation10 Pain self-management interventions aim to empower people to take control of their pain condition and thus reduce disability and improve quality of life outcomes. However, studies of treatment approaches involving components of self-management or self-care education specifically intended for people with neck pain are sparse, and there is no clear support for beneficial long-term effects on disability.Citation11–Citation14 The effectiveness of pain self-management interventions to enhance adherence to favorable coping skills, likewise to induce sustainable health behavior change, is sparsely investigated, and results on long-term maintenance of treatment gains are inconclusive.Citation15–Citation17
In previously reported short-term and long-term follow-ups, a multicomponent pain and stress self-management group intervention (PASS) had better effect on pain control, pain-related self-efficacy for activities of daily living (ADL), disability and catastrophizing than a control treatment: individually administered physiotherapy (IAPT), for patients with persistent tension-type neck pain in PHC.Citation18,Citation19 Likewise, analysis showed that treatment gains, as measured by post-treatment scores at the 20-week follow-up, in disability, self-efficacy and pain intensity were associated with long-term outcome in pain-related disability at 2 years in patients with persistent neck pain participating in the PASS.Citation20
When compared with the IAPT, a larger proportion of participants attending the PASS program reported that they used skills, which were gained during the intervention, to cope with pain in everyday life situations. The differences between the groups were less apparent at the 2-year follow-up, raising questions as to the sustainability of treatment effects, which warrants further investigation of the long-term effects of the intervention.
The objective of this study was to compare pain-related disability, self-efficacy for ADL, catastrophizing, pain, pain control, use of analgesics, and health care utilization in people with persistent tension-type neck pain 9 years after they received the PASS or IAPT.
Materials and methods
Study design
This study was a 9-year follow-up of a pragmaticCitation21 randomized controlled trialCitation22 evaluating the effects of a group-based pain self-management intervention as compared to IAPT in PHC.
Study participants
The inclusion criteria for this 9-year follow-up were as follows: all participants who had originally been included in the randomized controlled trial and who had not actively declined further participation at previous follow-ups. Of those 156 people (PASS, n = 77; IAPT, n = 79) originally included in the study, 129 people (PASS, n = 63; IAPT, n = 66) were eligible for inclusion in the 9-year follow-up. The participants’ current addresses were found by using the National Population Register.
Study procedure
In summary, patients with neck pain seeking physiotherapy treatment at nine PHC centers in eight towns in Sweden were consecutively recruited from September 2004 to April 2006. They were examined by a physiotherapist (PT) and considered eligible if they were 18–65 years of age and had tension-type neck pain of persistent duration, ie, >3 months. The reasons for exclusion were as follows: insufficient fluency in Swedish, medical history of psychotic disorder, pregnancy, ongoing treatment for neck pain, previously received PASS, or possible depression indicated by a score of ≥11 points on the depression subscale of the Hospital Anxiety and Depression Scale (HADS-D).Citation23 After completing the baseline self-assessment questionnaire, the participants were randomly allocated to either the experimental treatment PASS or the control treatment IAPT. The allocation sequence was prepared prior to the study with a random table, in randomly permuted blocks of two, four and eight, and stratified by the PHC center. An assistant who was not involved in delivering the interventions administered the opening of sealed opaque envelopes containing group allocation. PASS or IAPT treatment was delivered at the PHC center by experienced PTs. All participating PHC centers had at least three PTs employed. Each PT delivered only one of the interventions: PASS or IAPT. Prior to the study, the PTs delivering PASS attended a course that included the theories and the rationale behind the intervention, as well as detailed instructions and practical exercises from a manual of the eight PASS sessions. They were then provided with the manual and instructed to faithfully adhere to it. During the study, the PTs received performance feedback sessions. The other PTs working at the PHC centers provided IAPT in accordance with the current practice at their clinics.
Follow-ups were conducted 20 weeks, 1 year and 2 years after inclusion by using similar self-assessment questionnaires, which were mailed to the participants. In the present study, the same self-assessment questionnaire was mailed to the participants’ home addresses together with an information letter and a form for informed consent. The participants who agreed to participate returned the questionnaire and the signed informed consent by mail. Two reminders were sent to the participants who did not respond to the first letter.
Detailed descriptions of design and methods have been reported in previous publications on posttreatment effectsCitation18 and 2-year follow-up of effects.Citation19 The trial was approved by the ethics committee of Uppsala University (Ups 02-088), as was the 9-year follow-up (Ups 2013/345).
Interventions
PASS was a multicomponent group intervention consisting of seven weekly group sessions of 1.5 hours each and an additional booster session at 20 weeks after the initial session targeting the maintenance of coping skills. Each session consisted of applied relaxation training, body-awareness exercises and interactive lectures, emphasizing two-way communication and group discussions concerning issues related to pain self-management, according to a written manual.Citation18 The applied relaxationCitation24 comprised progressive and autogenic relaxation methods and conditioned relaxation exercises, eg, cue-controlled relaxation by thinking “relax” while exhaling. The rationale was to teach the patient active pain- and stress-coping skills by identifying personal “risk situations” in everyday life (ie, activities, movements or thoughts believed to cause pain or stress) and applying the relaxation techniques in these situations to manage physical arousal and thereby prevent the pain from starting or to control it. The body-awareness exercisesCitation25 were standing movement exercises that aimed to increase the awareness of oneself in the present moment, ie, the ability to sustain the attention on mental and bodily signals in nonevaluative, moment-to-moment awareness and to provide an opportunity to practice and apply relaxation when standing and during movement.
IAPT sessions were administered in accordance with the current practice and were not a standardized treatment procedure, in order to reflect the current practice at the participating PHC centers. The sessions involved several treatment modalities (spinal mobilization techniques and massage, acupuncture, transcutaneous electrical nerve stimulation and introduced the patient to individually tailored exercise programs (home-exercise programs, gym-based exercise programs, water-exercise programs). The type of treatment, frequency of visits and duration of contact were left to the judgment of and mutual agreement between the PT and the patient. The participants in the IAPT group were not to receive the PASS, but in no other way was treatment restricted.
The PASS participants attended an average of seven (range four to eight) group sessions, and the IAPT participants received an average of 11 (range 1–52) individual sessions over the 20-week intervention period. Detailed descriptions of the contents of the experimental treatment PASS and the control treatment IAPT have previously been reported.Citation18
Data collection
The self-assessment questionnaire used for this 9-year follow-up comprised questions on pain-related disability, self-efficacy for ADL, catastrophizing, pain intensity, perceived pain control, analgesics and health care utilization, as well as a question on the use of coping skills acquired during treatment and a question on satisfaction with care:
Disability: Perceived interference with ADL due to neck pain was assessed using the Neck Disability Index (NDI)Citation26,Citation27 containing 10 Likert-type questions each with five response options. Summed responses were expressed as an index of 0–100, where a higher value reflected more disability.
Self-efficacy for performing ADL: This was assessed by the Self-Efficacy Scale (SES).Citation28,Citation29 The participants rated how confident they were that they could do 20 activities despite pain on an 11-point numeric rating scale (0 = not at all confident, 10 = very confident).
Catastrophizing: The propensity to engage in negative thinking and worry in response to pain was assessed by the Coping Strategies Questionnaire – catastrophizing subscale (CSQ-CAT),Citation30–Citation32 entailing six items with response options by numeric rating scales rating from 0 = never to 6 = always.
Pain intensity: This was measured by three variables, ie, “at present”, “on average the previous week” and “at worst the previous week”, with response options by numeric rating scales ranging from 0 = no pain to 10 = worst possible pain.Citation33
Pain control: This was measured by the two questions from the CSQ,Citation30,Citation31 assessing the overall effectiveness of coping strategies. Participants rated the extent to which they were able to control or reduce pain (0 = no control/cannot reduce, 6 = complete control/can reduce completely).
Use of analgesics: Usage of analgesics for neck pain was measured by a 5-point Likert-type scale reflecting frequency, with the following response options: “every day”, “every second day”, “about 1 or 2 days per week”, “about 1 or 2 days per month” and “never”.
Health care utilization: Information on the number of health care visits due to neck pain during the preceding 3 months and on the number of days on sick leave due to neck pain during the preceding 3 months was collected by self-report in the questionnaire.
Satisfaction with care (allocated treatment): This was assessed by the question “How satisfied are you with the care that you received during the intervention period?”, measured by a 5-point Likert-type scale, with response options from “very content/satisfied” to “very discontent/dissatisfied”.
Use of skills acquired during the intervention to cope with pain: This was assessed by the question “Can you use/apply things you learned during the intervention in everyday life situations to cope with pain?”, measured by a 5-point Likert-type scale reflecting frequency, with response options “every day”, “often”, “sometimes”, “seldom” and “never”.
Statistical analyses
The number of participants included in the original study was based on power calculations of the primary outcome variables “disability” and “self-efficacy”, and it was estimated that a sample size of 150 would be sufficient to detect a 10% difference between groups (allowing for an estimated withdrawal of 30%, power 0.80, p = 0.05). However, the power calculations did not accommodate for a long-term follow-up.Citation34,Citation35
The primary analysis was simple main effects at 9 years. Mixed linear models for repeated measures analysisCitation36 were conducted for the primary outcome variables disability and self-efficacy and for the secondary outcome variables. “Time” and “group” were fixed effects in the analyses and participants the random effect. The interaction term time by group was included in the model to evaluate the interaction effect of differences between groups at each follow-up and within-group differences over time. The analyses were based on five time points of assessment (ie, baseline, 20-week, 1-year, 2-year and 9-year follow-ups). The baseline value of the dependent variable was included in the outcome vector. The Schwarz’s Bayesian Information Criterion suggested that an unstructured covariance structure yielded the best fit in all mixed model analyses. The ordinal responses were analyzed by fitting a generalized estimating equation (GEE) model with the GENMOD procedure in SAS® 9.3. The GEE strategy is a useful approach for repeated measurements analysis of ordered categorical outcomes. The model was set up with the same factors as in the mixed linear model mentioned earlier. The correlation structure used in the analyses was “independent”, and the link function was “cumulative logit”. The parameter estimates from the GEE model were presented as odds ratio and 95% confidence interval. Pairwise comparisons of simple main effects based on the mixed models were conducted to investigate differences between groups at the 9-year follow-up.
The chi-square test was applied for analyses of between-group differences at the 9-year follow-up on questions regarding “satisfaction with care” and “use of acquired skills in everyday life”.
A p-value ≤0.05 was accepted as statistically significant. Analyses were conducted using SAS 9.3 for mixed linear models and GEE analyses. IBM SPSS Statistics 21 for Windows was used for chi-square test (differences between groups on questions regarding “satisfaction with care” and “use of coping skills”) and for calculating differences between responders and nonresponders.
Data analyses were based on participants with available data at the 9-year follow-up, and their data from all previous follow-ups were analyzed according to group allocation at baseline. Occasional single missing items in the instruments SES and CSQ-CAT were substituted with the median of the participant’s responses to the other items included in the sum score on the same instrument.Citation37 This was done for five participants on SES at 9-year follow-up, for two participants on SES at 2-year follow-up and for one participant on SES and one participant on CSQ-CAT at 1-year follow-up. That is, it was done in <4% of the cases at 9 years and even less at previous follow-ups.
Results
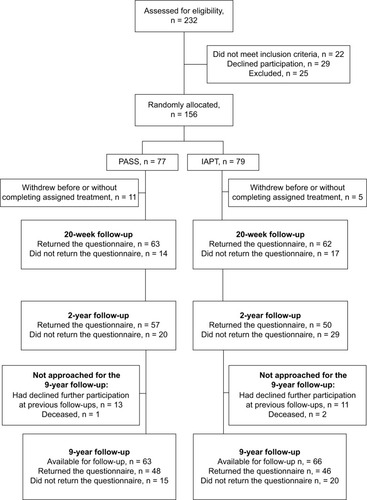
Eighty percent of those originally included in the randomized controlled trial were eligible and approached for the 9-year follow-up. The remaining participants were not approached due to either that they had declined further participation at a previous follow-up (n = 24) or that they were deceased (n = 3). Ninety-four people (73%) responded to the 9-year follow-up by returning the questionnaire (PASS, n = 48; IAPT, n = 46). The remaining 35 participants did not respond to the mailed invitation. provides a flow chart illustrating participation in the study over the follow-ups.
Figure 1 A flowchart illustrating participation in the study over the follow-ups.
The baseline characteristics of the participants are displayed in , separately for all originally included participants and for responders to the 9-year follow-up. Baseline assessments are displayed in , likewise separately for all originally included participants and for responders to the 9-year follow-up. Responders to the 9-year follow-up in the PASS group did not differ from all originally included PASS participants at baseline, nor to nonresponders to the 9-year follow-up. At baseline, responders in the IAPT group rated better self-efficacy for ADL as measured by SES (p = 0.024) compared to all originally included participants in IAPT and nonresponders to the 9-year follow-up.
Table 1 Baseline characteristics for PASS group and IAPT group
Table 2 Between- and within-group comparisons for PASS and IAPT
The results on outcome measures at 9 years are reported in . Mixed linear models and GEE analyses showed that there was an interaction “time by group” effect for disability, self-efficacy, catastrophizing, ability to pain control pain and number of health care visits due to neck pain. Analyses of simple main effects, ie, between-group comparison at the 9-year follow-up for variables with significant interaction effect, showed that there was a between-group difference at 9 years for disability (p = 0.006) and a trend for self-efficacy (p = 0.059) in favor of PASS. There were no significant differences between groups at 9 years regarding the other secondary outcome measures.
Between-group comparisons for categorical data are presented in . At 9 years, there were no longer differences between the groups with regard to the questions on “satisfaction with care” or “use of coping skills acquired during the intervention”, as previously seen at 1 year and 2 years. There was a trend that the PASS group reported that during treatment they had learned useful skills, which they could apply in everyday life to cope with pain, to a higher degree than the IAPT group (p = 0.061).
Table 3 Comparisons between PASS and IAPT groups regarding satisfaction with care and use of coping skills acquired during the intervention at follow-ups based on all individuals with available data
The self-reported number of days on sick leave due to neck pain during the preceding 3 months was similar in both groups both at baseline and at the 9-year follow-up. An analysis of those participants who were ≤56 years old at inclusion to the study (PASS, n = 62; IAPT, n = 62) showed that half of the participants in each group had no preceding sick leave due to neck pain at baseline and 16% in the PASS group and 25% in the IAPT group had 90 days of sick leave during the 3 months preceding baseline. At the 9-year follow-up, half of the participants in each group had no sick leave during the preceding 3 months and two people in the PASS group and three people in the IAPT group had 90 days of sick leave during the preceding 3 months, ie, were completely on sick leave.
Discussion
To the best of our knowledge, this is the first extended long-term follow-up of the treatment effects of a self-management intervention for people with persistent tension-type neck pain. Indeed, at this 9-year follow-up, a difference in disability in favor of PASS and a trend for better self-efficacy for ADL were still present. There were also between-group differences at 9 years in favor of PASS in terms of one aspect of pain and use of analgesics due to neck pain. Our findings indicate that this self-management group intervention appears to render sustainable favorable effects on disability.
It is an important finding that there was still a difference between the groups in disability with regard to ADL as measured by NDI. Previous research on self-management programs for chronic pain conditions has failed to provide convincing evidence for long-term effects on disability.Citation12,Citation16 Our finding that PASS reduced neck disability resonates with the primary objective of self-management interventions: to impact the consequences of illness, ie, disability, rather than to reduce symptoms, in this case pain.Citation10 Learning to self-manage pain is a key to attaining favorable pain-coping skills and thereby regaining control over one’s life, rather than letting pain control one’s life.Citation38,Citation39 Regaining control can be the first step toward reduction in perceived pain interference.Citation8,Citation40 Likewise, it has been suggested that interventions toward persistent nonmalignant pain conditions should first and foremost target the reduction in the pain-related disability rather than the pain intensity.Citation8,Citation41
There was a difference between groups only with regard to one of the three pain measures: “pain at worst”. Our results may indicate that differences in disability were not dependent on differences in pain-intensity measures. This is in line with research showing weak correlations between pain intensity and disability.Citation1,Citation42,Citation43 Also, a previous research has suggested that rather ability to control pain and coping may contribute to less disability.Citation35 In the light of the latter, the difference between groups with regard to “pain at worst” in favor of PASS at 9 years is worthy of note and important to discuss. It could be argued that the difference in perceived “pain at worst” might reflect a shift in perception, ie, change in the cognitive and affective processing in the brain, of when pain becomes intolerable/uncontrollable,Citation44 and is thus an indication of better perceived control over pain. Experimental studies have shown that when given the possibility to execute personal control over an experimentally induced painful procedure, the experience of pain intensity and unpleasantness is reduced.Citation44–Citation46 In addition, the results on the pain measure “pain at worst” and the measure of analgesics consumption “use of analgesics due to neck pain” strengthen each other by pointing in the same direction, ie, the PASS participants perceived less pain at worst and had a lower frequency of use of analgesics. A shift in coping strategies is another possible explanation for the difference between the groups in frequency of taking analgesics due to neck pain. In the population of people with tension-type neck pain, taking medication has been suggested to be a passive coping strategy.Citation7,Citation47
The self-management intervention aimed to reinforce active coping strategies, such as applying relaxation and body-awareness techniques, ie, physically and mentally tension-reducing techniques, in self-identified risk situations. It is plausible that the PASS group used such active coping strategies instead of taking pain medication. On the other hand, the result on the question “use of coping skills acquired during the intervention” may just point in the opposite direction: it showed that there was no longer a difference between groups as previously seen at 1 year and 2 years (although a possible trend [p = 0.061] in favor of PASS). However, it could also indicate that the PASS participants had integrated their skills to the extent that the coping strategies were no longer perceived as conscious thoughts and actions but instead as habitual behaviors in the person’s everyday life. If so, it is conceivable that an actual and profound behavior change had taken place. A somewhat similar suggestion could be applied to a 3-year follow-up of a physical activity intervention in which treatment effects were largely maintained, although adherence to the specific home training program faltered considerably.Citation48 This raises the question of whether coping skills gradually become integrated behaviors in ordinary life and if they become, then they are no longer perceived to be intentional actions or specific exercises. However, the present study was not designed to address this research question. Such an assumption could not be confirmed by the methods for data collection and results of this study. Exploration of such experiences needs to be further investigated in future studies. In addition, one should bear in mind the obvious risk of memory biasCitation49 when asking people about things that happened several years ago. It is unarguably very difficult to remember what was learned during an intervention that took place 9 years ago. Likewise, responses to the question regarding “satisfaction with care” were possibly subject to memory bias. There was no longer a difference between the groups regarding “satisfaction with care”, as was previously seen at 1 year and 2 years.
Work-related disability as measured by self-reported days on sick leave due to neck pain was similar and low in both groups at both baseline and at the 9-year follow-up. Half of the participants (≤56 years old) in each group had no sick leave days during the 3 months preceding baseline and 16% in the PASS group and 25% in the IAPT group had 90 days of sick leave during the 3 months preceding baseline. At the 9-year follow-up, very few participants in either group (PASS, n = 2; IAPT, n = 3) had long-term sick leave, ie, had 90 days of sick leave due to neck pain during the preceding 3 months. The low number of days on sick leave might reflect a difference in the population of people with neck pain, as compared to other populations with pain, for example, people with low back pain, where work-related disability is much more common and the number of days of sick leave is often larger.Citation4,Citation50
It has been suggested that self-efficacy for ADL despite pain is important to target in pain self-management interventions to achieve favorable health outcomes.Citation10,Citation39 Self-efficacy is a key factor for ability to adopt and also maintain self-management behavior.Citation39,Citation51 There is strong evidence suggesting that self-efficacy is an important mediator between pain and disabilityCitation29,Citation52,Citation53 and that targeting self-efficacy in pain self-management programs is associated with reduction in disabilityCitation20,Citation54,Citation55 and beneficial for other health outcomes.Citation15,Citation19 The concept of self-efficacy, according to the social cognitive theory,Citation56 was an important theoretical basis for the PASS. The concept emphasizes how self-efficacy beliefs are influenced by personal experiences of accomplishment, ie, “mastery experiences”, social reinforcements and social modeling, ie, “vicarious” experiences by observing others and verbal persuasion and the affective state within the individual. All these factors were addressed in PASS by the application of coping skills in ADL to reinforce personal mastery experiences and techniques for dealing with fear or other aversive emotional arousal that could impede performance.Citation57 The intervention was offered in a group setting with ample opportunities for social reinforcement through the observation of others and the receiving of feedback on accomplishments from the therapist and fellow group participants. At the 9-year follow-up, there was no difference between the groups, but there was a trend that the PASS group had better self-efficacy for ADL. In this 9-year follow-up, the participants in the IAPT group had better self-efficacy at baseline than all participants originally included in the IAPT. By having participants in the IAPT group who differed by baseline self-efficacy compared to the original IAPT participants, we might have diminished existing differences between the groups at the 9-year follow-up.
For self-management interventions to be perceived as beneficial with regard to producing sustainable behavior change, the effects need to be maintained over time. We believe that there are several important reasons for the beneficial long-term effects of PASS: 1) the design of the program, ie, the theoretical base grounded in social cognitive theory and especially targeting the enhancement of self-efficacy beliefs for active pain self-management,Citation58 and likewise the use of behavior-change techniques to promote health behavior change toward active coping skills;Citation59,Citation60 2) using a combination of treatment components (not relying on one single component), ie, applied relaxation,Citation24 body-awareness exercisesCitation25 and interactive group discussions that targeted pain educationCitation61 and enhancing personalized plans, goal setting and problem-solving skills;Citation10,Citation59 and 3) foremostly, the format and administration of the program, ie, the focus on applyingCitation60 everything that was targeted during sessions (ie, self-management skills, personalized plans and goal setting, problem-solving skills), in-between sessions through homework assignments and subsequently at the next session receiving feedback on homework assignments and support from the health care provider and the peers in the group.
The PASS entailed only seven weekly administered group sessions and one booster session 3 months later. Studies have suggested that in interventions that require active patient participation and readiness to adopt new behaviors, it is important to include repeated checkups on adherence and/or a considerable amount of maintenance supporting behavioral techniques in order to produce sustainable treatment effects.Citation48,Citation62,Citation63 Other pain self-management group interventions have included more extensive maintenance components to reinforce the class sessions, for example, additional individual sessionsCitation64 or telephone callsCitation55 monthly over a year, or follow-up group sessions after the main program.Citation63 The PASS intervention entailed only one additional booster session at 20 weeks after the initial session that exclusively targeted the maintenance of coping skills. However, the preceding seven weekly group sessions were thoroughly designed to induce sustainability by applying evidence-based behavior-change techniques:Citation59 ie, the application of relaxation and body-awareness exercises through homework assignments and self-monitoring in personally identified risk situations for pain flare-ups and likewise, receiving performance feedback on homework assignments and encouragement to apply problem-solving techniques to progressively refine the practice. With this procedure, coping skills were supposed to profoundly affect both bodily and cognitive dimensions of the individual. After the seventh session, participants were supposed to be well acquainted and prepared to independently use the coping strategies and to apply problem-solving skills as needed. The results of this study suggest that the treatment procedure, ie, the number of sessions and distribution over time, of the PASS intervention was sufficient to produce a sustainable behavior change and reduce disability, thus indicating that key components for the enhancement of long-term effectiveness in self-management behaviors were sufficiently targeted in the intervention and support the assumptions and rationale for this pain self-management program. However, it could not be ruled out that additional sessions with checkups of adherence to self-management strategies could have produced even more exhaustive treatment gains.
A strength of the study is that comparison of simple main effects for the 9-year follow-up based on mixed linear models and GEE analyses enabled accommodating for differences over time and by group. Another strength of this study is that the responders to this 9-year follow-up did not differ with regard to baseline characteristics/measures; this was the case with both all originally included participants and those who were eligible and approached for this follow-up, with the exception that responders in IAPT had better self-efficacy than all the participants included in IAPT. However, the vast majority of participants were women, which limits the generalizability of the results. The results could not be generalized to men.
A limitation of the study is that that all participants eligible for this 9-year follow-up did not respond despite reminders. Responses to the 9-year follow-up were obtained from 73% of those eligible at 9 years, corresponding to 60% of the original number of participants in the randomized controlled trial. Thus, the number of participants was acceptable but limited the capacity to ensure power to detect important differences. It is possible that we failed to detect differences in treatment effects that were present.
Author contributions
Both authors have substantially contributed to all parts of the study: the study design, acquisition and analysis of data, interpretation of results, and drafting of the manuscript. Both authors have approved the final version of the manuscript and are accountable for all aspects of the work.
Acknowledgments
The authors thank the statistician Elisabeth Berg (Karolinska Institutet, Stockholm) for statistical advice. The study was funded by grants from the Center for Clinical Research Dalarna and Karolinska Institutet.
Disclosure
The authors report no conflicts of interest in this work.
References
- Hogg-JohnsonSvan der VeldeGCarrollLJBone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersThe burden and determinants of neck pain in the general population: results of the bone and joint decade 2000–2010 task force on neck pain and its associated disordersSpine2008334 SupplS39S5118204398
- GuezMHildingssonCNilssonMToolanenGThe prevalence of neck pain: a population-based study from northern SwedenActa Orthop Scand200273445545912358121
- HillJLewisMPapageorgiouACDziedzicKCroftPPredicting persistent neck pain: a 1-year follow-up of a population cohortSpine200429151648165415284511
- EnthovenPSkargrenEObergBClinical course in patients seeking primary care for back or neck pain: a prospective 5-year follow-up of outcome and health care consumption with subgroup analysisSpine200429212458246515507811
- LintonSJAnderssonTCan chronic disability be prevented? A randomized trial of a cognitive-behavior intervention and two forms of information for patients with spinal painSpine200025212825283111064530
- GreenAJJacksonDAKlaber MoffettJAAn observational study of physiotherapists’ use of cognitive-behavioural principles in the management of patients with back pain and neck painPhysiotherapy200894306313
- BlythFMMarchLMNicholasMKCousinsMJSelf-management of chronic pain: a population-based studyPain2005113328529215661435
- TurkDCSwansonKSTunksERPsychological approaches in the treatment of chronic pain patients – when pills, scalpels, and needles are not enoughCan J Psychiatry200853421322318478824
- SmeetsRJVlaeyenJWHiddingAActive rehabilitation for chronic low back pain: cognitive-behavioral, physical, or both? First direct post-treatment results from a randomized controlled trial [ISRCTN22714229]BMC Musculoskelet Disord20067516426449
- LorigKRHolmanHSelf-management education: history, definition, outcomes, and mechanismsAnn Behav Med20032611712867348
- HurwitzELCarrageeEJvan der VeldeGBone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated DisordersTreatment of neck pain: noninvasive interventions: results of the bone and joint decade 2000–2010 task force on neck pain and its associated disordersSpine2008334 SupplS123S15218204386
- DuSYuanCXiaoXChuJQiuYQianHSelf-management programs for chronic musculoskeletal pain conditions: a systematic review and meta-analysisPatient Educ Couns2011853e299e31021458196
- GrossARKaplanFHuangSPsychological care, patient education, orthotics, ergonomics and prevention strategies for neck pain: an systematic overview update as part of the ICON ProjectOpen Orthop J2013753056124133554
- LeaverAMRefshaugeKMMaherCGMcAuleyJHConservative interventions provide short-term relief for non-specific neck pain: a systematic reviewJ Physiother2010562738520482474
- DamushTMKroenkeKBairMJPain self-management training increases self-efficacy, self-management behaviours and pain and depression outcomesEur J Pain20162071070107826849410
- OliveiraVCFerreiraPHMaherCGPintoRZRefshaugeKMFerreiraMLEffectiveness of self-management of low back pain: systematic review with meta-analysisArthritis Care Res (Hoboken)201264111739174822623349
- BoyersDMcNameePClarkeACost-effectiveness of self-management methods for the treatment of chronic pain in an aging adult population: a systematic review of the literatureClin J Pain201329436637523042472
- GustavssonCDenisonEKochLSelf-management of persistent neck pain: a randomized controlled trial of a multi-component group intervention in primary health careEur J Pain2010146630.e1630.e1119939717
- GustavssonCDenisonEvon KochLSelf-management of persistent neck pain: two-year follow-up of a randomized controlled trial of a multicomponent group intervention in primary health careSpine (Phila Pa 1976)201136252105211521358487
- GustavssonCBergstromJDenisonEvon KochLPredictive factors for disability outcome at twenty weeks and two years following a pain self-management group intervention in patients with persistent neck pain in primary health careJ Rehabil Med201345217017623250561
- JadadARandomised Controlled Trials A User’s GuideLondonBMJ Books1998
- BoutronIMoherDAltmanDGSchulzKFRavaudPCONSORT GroupExtending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaborationAnn Intern Med2008148429530918283207
- ZigmondASSnaithRPThe Hospital Anxiety and Depression ScaleActa Psychiatr Scand19836763613706880820
- OstLGApplied relaxation: description of a coping technique and review of controlled studiesBehav Res Ther19872553974093318800
- RoxendalGBody Awareness Therapy and Body Awareness Scale: Treatment and Evaluation in Psychiatric Physiotherapy [Doctoral thesis]GöteborgDepartment of Psychiatry, University of Gothenburg1985
- VernonHMiorSThe Neck Disability Index: a study of reliability and validityJ Manipulative Physiol Ther19911474094151834753
- Helmerson AckelmanBLindgrenUValidity and reliability of a modified version of the Neck Disability IndexJ Rehabil Med200234628428712440803
- AltmaierERussellDKaoCLehmannTWeinsteinJRole of self-efficacy in rehabilitation outcome among chronic low back pain patientsJ Couns Psychol199340335339
- DenisonEAsenlofPLindbergPSelf-efficacy, fear avoidance, and pain intensity as predictors of disability in subacute and chronic musculoskeletal pain patients in primary health carePain2004111324525215363867
- RosenstielAKKeefeFJThe use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustmentPain198317133446226916
- JensenIBLintonSJCoping Strategies Questionnaire: reliability of the Swedish version of the CSQScand J Behav Ther199322139145
- WaddellGNewtonMHendersonISomervilleDMainCJA Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disabilityPain1993532157168
- JensenMPKarolyPSelf-Report Scales and Procedures for Assessing Pain in AdultsNew York, NYGuilford Press1992
- PolitDFNursing Research: Principles and MethodsPhiladelphia, PALippincott Williams & Wilkins2004
- GustavssonCvon KochLApplied relaxation in the treatment of long-lasting neck pain: a randomized controlled pilot studyJ Rehabil Med200638210010716546766
- WeissREModeling Longitudinal DataNew York, NY; LondonSpringer2005
- TabachnickBGFidellLSUsing Multivariate Statistics5th edBoston, MAPearson Education. Allyn and Bacon2007
- MercadoACCarrollLJCassidyJDCotePPassive coping is a risk factor for disabling neck or low back painPain20051171–2515716043291
- JensenMPNielsonWRKernsRDToward the development of a motivational model of pain self-managementJ Pain20034947749214636816
- JensenMPNielsonWRTurnerJARomanoJMHillMLChanges in readiness to self-manage pain are associated with improvement in multidisciplinary pain treatment and pain copingPain20041111–2849515327812
- SullivanMAdamsHPsychosocial treatment techniques to augment the impact of physiotherapy interventions for low back painPhysiother Can201062318018921629595
- SullivanMJToward a biopsychomotor conceptualization of pain: implications for research and interventionClin J Pain200824428129018427226
- KovacsFMAbrairaVZamoraJKovacs-Atención Primaria GroupCorrelation between pain, disability, and quality of life in patients with common low back painSpine (Phila Pa 1976)200429220621014722416
- CampbellCMEdwardsRRMind-body interactions in pain: the neurophysiology of anxious and catastrophic pain-related thoughtsTransl Res200915339710119218091
- WallPDPain in the brain and lower parts of the anatomyPain19956233893938657442
- OchsnerKNGrossJJThe cognitive control of emotionTrends Cogn Sci20059524224915866151
- BussingAOstermannTNeugebauerEAHeusserPAdaptive coping strategies in patients with chronic pain conditions and their interpretation of diseaseBMC Public Health20101050720727191
- YlinenJHakkinenANykanenMKautiainenHTakalaEPNeck muscle training in the treatment of chronic neck pain: a three-year follow-up studyEura Medicophys200743216116917525699
- KazdinAEResearch Design in Clinical Psychology4th edBostonAllyn & Bacon Pearson Education2003
- BreivikHCollettBVentafriddaVCohenRGallacherDSurvey of chronic pain in Europe: prevalence, impact on daily life, and treatmentEur J Pain200610428733316095934
- RhodesREPlotnikoffRCCourneyaKSPredicting the physical activity intention-behavior profiles of adopters and maintainers using three social cognition modelsAnn Behav Med200836324425219057976
- LeeHHubscherMMoseleyGLHow does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck painPain2015156698899725760473
- Van LiewCBrownKCCronanTABigattiSMKothariDJPredictors of pain and functioning over time in fibromyalgia syndrome: an autoregressive path analysisArthritis Care Res (Hoboken)201365225125622807468
- NicholsonRAHurseyKGNashJMModerators and mediators of behavioral treatment for headacheHeadache200545551351915953268
- DamushTMWeinbergerMPerkinsSMThe long-term effects of a self-management program for inner-city primary care patients with acute low back painArch Intern Med2003163212632263814638564
- BanduraASelf-efficacy: toward a unifying theory of behavioral changePsychol Rev1977842191215847061
- BanduraASelf-Efficacy: The Exercise of ControlBasingstokeW. H. Freeman1997
- BanduraAHealth promotion by social cognitive meansHealth Educ Behav200431214316415090118
- MichieSRichardsonMJohnstonMThe behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventionsAnn Behav Med2013461819523512568
- BaldwinJDBaldwinJIBehavior Principles in Everyday Life4th edUpper Saddle River, NJPrentice Hall2001
- MoseleyGLButlerDSFifteen years of explaining pain: the past, present, and futureJ Pain201516980781326051220
- WestmanALintonSJTheorellTOhrvikJWahlenPLeppertJQuality of life and maintenance of improvements after early multimodal rehabilitation: a 5-year follow-upDisabil Rehabil200628743744616507506
- CarsonJWKeefeFJAffleckGA comparison of conventional pain coping skills training and pain coping skills training with a maintenance training component: a daily diary analysis of short- and long-term treatment effectsJ Pain20067961562516942947
- MultonKDParkerJCSmarrKLEffects of stress management on pain behavior in rheumatoid arthritisArthritis Rheum200145212212811324774
