Abstract
In idiopathic trigeminal neuralgia (TN) the neuroimaging evaluation is usually normal, but in some cases a vascular compression of trigeminal nerve root is present. Although the latter condition may be referred to surgery, drug therapy is usually the first approach to control pain. This study compared the clinical outcome and direct costs of (1) a traditional treatment (carbamazepine [CBZ] in monotherapy [CBZ protocol]), (2) the association of gabapentin (GBP) and analgesic block of trigger-points with ropivacaine (ROP) (GBP+ROP protocol), and (3) a common TN surgery, microvascular decompression of the trigeminal nerve (MVD protocol). Sixty-two TN patients were randomly treated during 4 weeks (CBZ [n = 23] and GBP+ROP [n = 17] protocols) from cases of idiopathic TN, or selected for MVD surgery (n = 22) due to intractable pain. Direct medical cost estimates were determined by the price of drugs in 2008 and the hospital costs. Pain was evaluated using the Numerical Rating Scale (NRS) and number of pain crises; the Hospital Anxiety and Depression Scale, Sickness Impact Profile, and satisfaction with treatment and hospital team were evaluated. Assessments were performed at day 0 and 6 months after the beginning of treatment. All protocols showed a clinical improvement of pain control at month 6. The GBP+ROP protocol was the least expensive treatment, whereas surgery was the most expensive. With time, however, GBP+ROP tended to be the most and MVD the least expensive. No sequelae resulted in any patient after drug therapies, while after MDV surgery several patients showed important side effects. Data reinforce that, (1) TN patients should be carefully evaluated before choosing therapy for pain control, (2) different pharmacological approaches are available to initiate pain control at low costs, and (3) criteria for surgical interventions should be clearly defined due to important side effects, with the initial higher costs being strongly reduced with time.
Introduction
Trigeminal neuralgia (TN) is a neuropathic pathology considered one of the most painful experiences patients can report, and no universal treatment is capable of reverting completely and definitely its intermittent paroxysmal excruciating pain crises.Citation1 TN is associated with impairment of daily functionality, reduced quality of life,Citation2,Citation3 and depression,Citation4 to which contributes the overwhelming fear that pain can suddenly return again. Although the huge impact of pain in TN, which has an incidence of 4–5 per 100,000Citation5 or even higher,Citation6 and a high prevalence in older patients should have been capable of resulting in clinical standards for TN treatment, this pathology is far from being well known and treated. In most cases the pathophysiology underlying TN is unknown or incompletely understood. Classical or idiopathic TN includes all cases without an established etiology (most of them) as well as those with potential vascular compression of the trigeminal nerve, whereas symptomatic TN results secondarily to cases such as tumors or multiple sclerosis.Citation7
TN is not controlled by classical analgesics, but the first-line therapy is pharmacological, being based on anticonvulsants (ACs), usually considered adjuvant analgesics in other pathologies but essential for neuropathic pain. Phenytoin in the pastCitation8,Citation9 and now carbamazepine (CBZ)Citation1,Citation10–Citation12 are first-line drugs in TN, followed by several second-line ACs such as lamotrigine,Citation11,Citation13 oxcarbazepine,Citation14 gabapentin (GBP),Citation1 and CBZ or GBP associated with peripheral block of trigger-points with the local anesthetic ropivacaine (ROP);Citation3,Citation15 these treatments changed the management of TN, as previously it was almost exclusively surgical. Surprisingly, combination therapies, although common in epilepsy, have not been explored for TN management.Citation3,Citation15,Citation16
Surgical intervention for TN is usually reserved for patients with intractable pain refractory to an adequate trial of at least 3 drugs including CBZ.Citation1 The decision to perform a surgical approach should be based on the clinical presentation (including co-morbilities) of the patient and not primarily or exclusively on neuroimaging,Citation1 as craniotomy is not without risks and fine detail alone at actual MRI spatial resolution cannot distinguish the pathological from the incidental when a vessel course is along the trigeminal nerve root.Citation17,Citation18 However, some patients may request surgical treatment due to intractable pain or strong adverse side effects.Citation1 Microvascular decompression (MVD) of the trigeminal nerve root is a well established and superior method of choice among neurosurgical proceduresCitation19 in immediate (91%–97%) and long-term (53%–70%) relief of TN,Citation12,Citation20–Citation22 but is associated with several risks, including different degrees of facial sensory loss as well as a small risk of mortality.Citation1 Other surgical options include Gasser ganglion compression, glycerol gangliolysis, and radiofrequency thermocoagulation of the nerve, with the last producing initial pain relief in more than 90% and a complete pain relief after 5 years reaching 57% of patients;Citation23 however, these cases are associated with a risk of anesthesia dolorosa (0.6%–6%) and cases of transient or permanent cranial nerve palsies.Citation1,Citation23 Gamma knife radiosurgery is less invasive, the onset of pain relief following procedure possibly requiring 1–2 months to occur, but then 30%–80% of cases report complete absence of pain;Citation24–Citation27 however, again, frequency of paresthesia and dysesthesia ranges from 3%–54%,Citation28,Citation29 there is a steady rate of late failure,Citation25 and the details of operative technique have a major influence on the clinical results.Citation30,Citation31 Nevertheless, in radiosurgical centers, this is a major surgery treatment for TN.Citation27
From the above data, we should consider that the choice of drug and whether or not to operate and which procedure to choose should be individualized to the particular needs and conditions of each patient.Citation1 The role of surgery versus pharmacotherapy in TN management remains uncertain as there are no studies dealing specifically with issues like “when should surgery be offered?”.Citation12 Additionally, only a few studies have evaluated the impact of TN costs to the patients, and compared only the cost-effectiveness of different surgical procedures. At longer follow-up intervals, MVD is predicted to be the most cost-effective surgery and should be considered the preferred operation for patients, compared with glycerol rhizotomy and stereotactic radiosurgery,Citation32 whereas cyberknife radiosurgery is a cost-saving alternative compared with MVD.Citation33 On the other hand, to the best of our knowledge, the costs associated with TN drug treatments have been analyzed only for pregabalin.Citation34,Citation35 However, no studies have evaluated the costs associated with different drug treatments compared with surgery. The objective of the present study was to compare the clinical outcome and direct costs of (1) a first-line pharmacological treatment (CBZ), (2) the therapeutical association of GBP and the peripheral analgesic block of TN trigger-points with ROP (GBP+ROP) and (3) a common TN surgery (MDV) in patients recruited from the same country region.
Methods
Patients – inclusion and exclusion criteria
This retrospective study includes a total of 62 TN patients from the Hospital Center of Alto Ave – Fafe Pain Unit and the Hospital São Marcos in Braga, who were selected by different clinical teams as follows: patients under the traditional approach to TN were given CBZ in monotherapy (CBZ protocol; n = 23) and were randomly selected in the continuation of a previous study of our group;Citation15 patients submitted to an alternative TN approach were given GBP associated with the peripheral analgesic block of trigger-points with ROP (GBP+ROP protocol; n = 17) and were randomly selected in the continuation of another previous study of our group;Citation3 patients submitted to microvascular decompression of the trigeminal nerve (MVD protocol; n = 22) were all those arriving at the Neurosurgery Department of Hospital São Marcos between 2005 and 2008 and indicated for surgery by this Hospital team ().
Table 1 Baseline characteristics of the patients
Patients from CBZ and GBP+ROP protocols were eligible for the study if they presented a pain intensity with a score ≥ 6 measured by the Numerical Rating Scale (NRS), and met the consensus criteria for the diagnosis of primary (idiopathic) TN.Citation36 The inclusion criteria were (1) the occurrence of episodes of facial paroxysmal pain in territory innervated by a branch of the trigeminal nerve (NRS score ≥ 6), (2) presence of a normal neurological profile, and (3) presence of normal neuroimaging analysis. On the other hand, several exclusion criteria were also considered,Citation3,Citation15 including patient refusal to participate, clinical depressive condition, anticlotting therapy, secondary (symptomatic) TN, altered neurological profile, neuroimaging alterations, association with other cranial nerve neuralgias, and proposed surgical intervention.
Patients following the surgical protocol (MVD) were selected by their intense intractable pain refractory to pharmacological therapy, or intolerable side effects of drugs.Citation37 Thus, when arriving at the Neurosurgery Department of Hospital São Marcos (day 0), 21 of 22 patients showed NRS = 10 and all were being medicated (12 patients were taking 600 mg/day of CBZ and 10 were taking 600 mg/day of CBZ plus 600 mg/day of GBP). This Neurosurgery Department does not have equipment for radiosurgery, thus MVD constitutes the major surgical approach for TN patients with intractable pain.
The therapeutical protocols used were accepted by the Hospital Ethical Committees (all three are actual therapies for TN pain control) and the patients were informed by the different clinical teams that: (1) they were going to be submitted to one of three (GBP+ROP protocol; see reference Citation3) or one of two (CBZ protocolCitation15) pharmacological therapies, or to surgery (MVD protocol); (2) they could drop or change treatment if no pain control was achieved (CBZ and GBP+ROP protocols) or they would be continuing to take pharmacological agents if needed (MDV protocol). Patients signed an informed consent.
Treatment protocols
Patients were submitted to one of the following treatment protocols:
CBZ protocol – Treatment using only oral CBZ in monotherapy; patients entering this protocol received additionally a control injection of saline (the vehicle of ROP administered to the other protocol, CBZ+ROP applied in another studyCitation15) at facial trigger-points each 7 days of treatment (days 0, 7, 14, 21, and 28), during 4 weeks. The usual effective CBZ dosage ranges from 400 to 1000 mg/day.Citation38 Since these patients arrived at the Fafe Pain Unit from other Health Institutions with uncontrolled pain (day 0), their CBZ dose (whatever it was) was increased by 200 mg/day; thus, no CBZ titration was performed. Each 7 days, during their visit to the Unit, the NRS score of the patients was recorded and CBZ dose adjusted if necessary. For statistical purposes patients were evaluated at day 0 (arrival to the pain unit) and after a follow-up of 5 months after the end of the 4-week treatment (month 6).
GBP+ROP protocol – Treatment using oral GBP plus administration of a superficial analgesic block with ROP to facial trigger-points, as described elsewhere.Citation3 The peripheral block with ROP was performed at the Pain Unit under sterile conditions, using a 27-gauge needle for administering subcutaneously 2 mL of a 2 mg/mL ROP solution.Citation3,Citation39 Each local block was peformed once a weekCitation3,Citation40 during the 1-month therapy (days 0, 7, 14, 21, and 28, when the patient was received by the Unit staff). At day 0, an ROP block was performed and 100 mg GBP administered at night to each patient. On subsequent days, daily GBP increase followed the rationale described in Lemos et al.Citation3 For statistical purposes patients were evaluated at day 0 (arrival to the pain unit) and after a follow-up of 5 months (month 6).
MVD protocol – This technique is thoroughly described elsewhere.Citation37 During pre-surgery, MVD patients undergo tests (blood, electrocardiogram, chest X-ray, computed tomography (CT scan)) several days before surgery. During surgery, patients are anesthetized always using the same protocol (endovenous general anesthesia) and are positioned on their back with their head turned or on their side with the symptomatic side facing up. A vertical incision is made behind the ear, 3–5 mm medial to the mastoid notch and extending about the length of the ear. A circular portion of the skull is removed exposing the underlying dura, which is opened to expose the cerebellum and reach the posterior fossa. The cerebellum is allowed to fall out of the way exposing the side of the brainstem. By advancing over the superior surface of the cerebellum, the VII and VIII cranial nerves are avoided. The arachnoid membrane is dissected allowing visualization of the VII, VIII, and finally the trigeminal nerve. The offending loop of blood vessel is then mobilized. Venous vessels above or below the nerve are dissected away from the nerve and are coagulated and divided if needed. A sponge-like material (Teflon) is inserted between the vessel in contact with the nerve (usually the superior cerebellar artery).Citation41 Frequently a groove or indentation is seen in the nerve where the offending vessel was in contact with the nerve. The sponge-like material is placed between the nerve and the offending blood vessel to prevent the vessel from returning to its native position. If venous vessels alone are in contact with the nerve, no prosthesis is required as they are coagulated and divided.Citation37 After the decompression is complete, the wound is flushed clean with saline solution. The dura is sewn closed. The skull is reconstructed and the overlying tissues are closed in multiple layers. The patient is allowed to wake up and is taken to an intensive care unit or other close observation unit for 3–5 days before returning home. For statistical purposes patients were evaluated at day 0 (day before surgery) and after a follow-up of 6 months (month 6).
Clinical outcome
The predefined outcome measures were:
Evaluation of pain intensity using the NRS scale. Evaluation points were the following: at the arrival at the Pain Unit (CBZ and GBP+ROP protocols) or the day before surgery at the Neurosurgical Department (MVD protocol) (day 0) and 6 months later (month 6). Patients were told to locate their relative pain in a line marked with numbers, from 0 (no pain) in the extremity on the left to 10 (the worst pain imaginable) in the extremity on the right. Moderate pain was considered to be > 3 (NRS > 3) and severe pain > 6 (NRS > 6).Citation42 A pain reduction of 2 points in the 11-point NRS scale from the baseline pain score (day 0) was considered to be clinically significant.Citation43–Citation45
Daily number or paroxysmal pain episodes. Although this variable was evaluated every day, only data obtained at day 0 and month 6 were used for statistical analysis.
Adverse side effects, especially those involving sensory alterations. For each patient of the protocols evaluated, the types of sensory deficits were recorded before (day 0) and 6 months after the beginning of therapeutical intervention.
The Hospital Anxiety and Depression Scale (HADS) questionnaireCitation46,Citation47 is a self-screening evaluation for depression and anxiety. It consists of 14 questions, 7 for anxiety and 7 for depression, which were presented to patients of the three protocols at day 0 and month 6.
Evaluation of life quality using the Sickness Impact Profile (SIP).Citation48–Citation50 This questionnaire, adapted to the Portuguese population,Citation49 evaluated the evolution of the quality of life of patients submitted to the three protocols, from day 0 to month 6. SIP evaluates the descriptive profile of patients in terms of impact of the pathology analyzed upon specific daily life behaviors. We analyzed the answers obtained at day 0 and month 6 to 136 questions distributed along the following categories: “Domestic Work”, “Mobility”, “Communication”, “Locomotion”, “Eating”, “Recreation-Pastimes”, “Emotion”, “Social Interaction”, “Alertness”, and “Rest”.
Questionnaire on the satisfaction with the treatment and medical team (QUASU). It contains 47 items that evaluate patient satisfaction at different levels: Access, Expenses, Technical Quality, Communication/Information, Interpersonal Relations, Team Coordination, and Global Evaluation (created by McIntyre et alCitation51 based on the Portuguese population).
The follow-up evaluation was performed at the end of the day, on completion of month 6, during a phone interview to each patient. For NRS evaluation the patient was asked to reveal (1) the pain felt at that moment as a number on the NRS scale with which they were used to dealing with or, in case of no pain, (2) which was the pain felt in the worst day of the last week before the interview. For the number of pain crisis, each patient was asked (3) how many pain attacks they had suffered during that day or, in case of no pain, (4) how many pain crises they had suffered in the worst day of the last week before the interview. If no pain was recorded following these four questions, the staff recorded 0 (zero) pain crisis for the patient. The adverse side effects were also recorded and patients completed the SIP and HADS questionnaires.
Direct cost analysis: pharmacological and hospital costs
For patients submitted to pharmacological (CBZ and GBP+ROP protocols) or surgical (MVD protocol) therapies, direct medical cost estimates were determined using hospital cost accounting data published in Diário da República, the “Simposium Terapêutico 2008”, and the price lists included in the latter.Citation52,Citation53 Medical costs were calculated using the patient-reported dosage and number of doses taken daily and Hospital internment, which were converted to the cost between day 0 and 1 month (according to the 4-week treatment in protocols GBP+ROP and CBZ) and between month 1 and month 6 (follow-up for the three protocols) ().
Table 2 Average direct healthcare cost per patient
Statistics
Data are presented as mean ± standard deviation (SD) along the several variables under study. The normal distribution of the results was verified using the Kolmogorov–Smirnov test, whereas the equality of variances was evaluated by the Levene test. A logarithmic transformation of data has been used whenever the homogeneity of variances was not verified. Mean NRS scores, number of pain crisis, direct costs, SIP, and HADS values at day 0 and month 6 (or only at month 6 for costs data) were compared using paired-samples Student’s t-test whenever possible, or the one-sample t-test when one of the means showed absence of variation (see Results section). Mean NRS scores following protocols CBZ, GBP+ROP, and MVD were compared at month 6 using a one-way analysis of variance (ANOVA) followed by the Tukey post hoc test.
Results
Patient baseline characteristics
The baseline data for the demographic characteristics of patients selected for the three protocols are shown in .
Effect of CBZ, GBP+ROP and MVD protocols in pain control
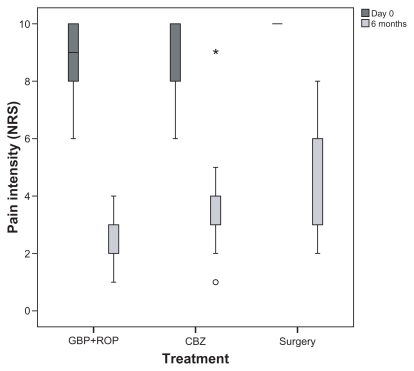
No differences in pain intensity were found between patients from GBP+ROP protocol (NRSd0 = 8.8 ± 1.4) and CBZ protocol (NRSd0 = 9.1 ± 1.4) (P = 0.41, t-test) () at the beginning of the treatment [day 0 (d0)], whereas 21 of 22 MVD patients presented an NRS score of 10, the most painful condition imaginable (NRSd0 = 9.9 ± 0.4). Five months after the 4-week treatment followed in CBZ and GBP+ROP protocols [month 6 (6m)], both pharmacological approaches had decreased significantly, pain measured by NRS scores (GBP+ROPd0 × GBP+ROP6m, P < 0.0001; CBZ0 × CBZ6m, P < 0.0001, paired-samples t-tests), while 6 months after MVD surgery NRS scores were also significantly reduced (MDVd0 × MDV6m, P < 0.001, one-sample t-test). Although the three protocols reduced pain intensity, GBP+ROP therapy resulted in a significantly lower NRS score than patients following CBZ or MVD protocols (GBP+ROP, NRS6m = 2.6 ± 1.00; CBZ, NRS6m = 3.9 ± 1.5; MVD, NRS6m = 4.2 ± 1.7, one-way ANOVA, P = 0.002; GBP+ROP6m × CBZ6m, P = 0.011, GBP+ROP6m × MVD6m, P = 0.002, Tukey tests) (). With respect to the NRS observed at month 6 for MVD patients, it can be concluded by a one-sample t-test that the NRS value is significantly different from 10 (P < 0.001), the value observed before surgery (day 0).
Figure 1 Effect of the three protocols (GBP+ROP, CBZ, and MVD) on the pain intensity of patients 6 months after day 0. For significant differences see the Results section.
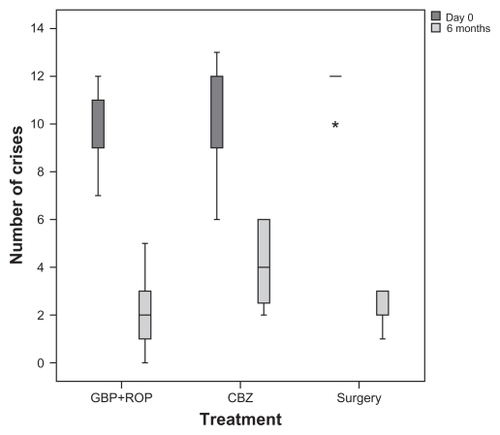
The baseline number of daily crises of paroxysmal sudden and intense pain was similar between patients of both pharmacological protocols (day 0: GBP+ROP, ncrises = 9.6 ± 1.5; CBZ, ncrises = 10.7 ± 2.2; P = 0.114, t-test), whereas 21 of 22 MVD patients presented 12 pain crises per day (MVD, ncrisis = 11.8 ± 0.6) (). Five months after the 4-week treatment followed in CBZ and GBP+ROP protocols (month 6), all three protocols had decreased significantly the number of daily pain crises (month 6: GBZ+ROP, ncrises = 2.0 ± 1.6; CBZ, ncrises = 4.1 ± 1.7; MVD, ncrisis = 2.6 ± 0.6 − GBP+ROPd0 × GBP+ROP6m, P < 0.0001; CBZd0 × CBZ6m, P < 0.0001, paired samples t-tests; MDVd0 × MDV6m, P < 0.001, one-sample t-test) (). Again, with respect to the number of daily pain crises observed at month 6 in MVD patients, it can be concluded by a one-sample t-test that the number of crises is significantly different from 12 (P < 0.001), the value observed before surgery (day 0).
Figure 2 Effect of the three protocols (GBP+ROP, CBZ, and MVD) on number of daily episodes of pain before (day 0) and after a 5-month follow-up (month 6). For significant differences see the Results section.
Daily dose of anticonvulsants
The three protocols showed a different evolution in the consumption of anticonvulsants CBZ or GBP. At day 0 and 1 GBP+ROP patients took 100 mg/day of GBP; at day 7, these patients were taking 200 or 300 mg/day (mean = 266,67 mg/day); at the end of the 4-week treatment patients were taking 300 mg/day of GBP, which was maintained during the next 5 months, until month 6.Citation3 Patients following CBZ protocol arrived to the Hospital and began taking 626 ± 163 mg/day of CBZ; at the end of the 4-week treatment, CBZ intake increased to 757 ± 200 mg/day, which was increased even at month 6 to 826 ± 291 mg/day.Citation15 Finally, MVD protocol patients were taking 600 mg/day of CBZ in monotherapy (12 of the 22 patients) or GBP+ROP (600 + 600 mg/day); at the end of the follow-up (month 6), MVD patients were still assisted by drugs, although at lower doses, namely 200 mg/day of CBZ or 300 mg/day of GBP, both in monotherapy.
Adverse side effects
The GBP+ROP protocol resulted in no significant side effects and no sensory deficits.Citation3 Patients following the CBZ protocol showed no sensory deficits, but 7 of the 21 patients presented adverse side effects (dizziness).Citation15 On the contrary, 5 of the 22 patients submitted to MVD protocol presented hypesthesia of the hemiface affected, 3 were anesthetized in the hemiface, 1 showed paresthesias, and 1 patient died in the immediate postoperative period due to brain hemorrhage, with a total of 10 in 22 patients with sensory sequelae; additionally, 5 of the 22 patients presented dizziness as an adverse side effect and 7 in 22 showed a complete absence of side effects or sequelae.
Direct costs
Data on direct costs of resources consumption show that MVD full cost was €1056.78 ± 22.5 per patient while, on the contrary, CBZ (€384.2 ± 1.5) and especially GBP+ROP (€252.47) were far less expensive between day 0 (before treatment/surgery) and the end of the first month (GBP+ROPeuro × CBZeuro, P < 0.0001; GBP+ROPeuro × MVDeuro, P < 0.0001, one-sample t-tests; CBZeuro × MVDeuro, P < 0.0001, paired-samples t-test) (). It can be concluded by one-sample t-tests that the total direct cost during the first month per patient submitted to CBZ or MVD protocols is significantly different from €252.47 (P < 0.001), the average total cost value observed for each GBP+ROP patient. The difference is mostly explained by 2 factors: the cost of the surgical procedure and the cost of hospital stay for MVD patients. However, during months 2–5, the financial situation alters: GBP+ROP protocol becomes the most expensive treatment (GBP+ROPmonths 2–6 = €314.3), as GBP is more expensive than CBZ (CBZmonths 2–6 = €255.0 ± 6.3) and MVD patients take a low dosage of anticonvulsants (MVDmonths 2–6 = €254.7 ± 40.9) ().
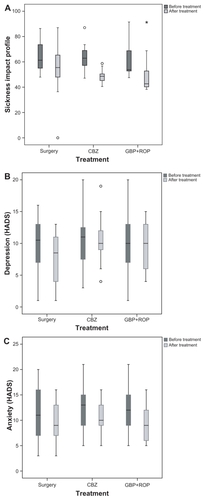
Functional quality of life and patient satisfaction
Quality of life measured by the scores obtained through the SIP questionnaire for patients in both GBP+ROP and CBZ protocols showed a significant improvement in functionality (GBP+ROPd0 × GBP+ROP6m, P < 0.0001), which was not achieved at a significant level by MVD patients (MVDd0 × MVD6m, P = 0.086, paired-samples t-tests) (). Interestingly, however, both anxiety and depression scores were significantly improved in MVD patients from day 0 to month 6, as measured by HADS questionnaire (MVDANXd0 × MVDANX6m, P < 0.001; MVDDEPd0 × MVDDEP6m, P < 0.0001, paired-samples t-test) (), whereas CBZ patients showed a significant improvement only in anxiety scores (CBZANXd0 × CBZANX6m, P = 0.036, paired-samples t-test) and GBP+ROP patients did not improve in any of the dimensions evaluated by the HADS questionnaire ().
Figure 3 Effect of GBP+ROP, CBZ, and MVD protocols on the total SIP score of quality of life (A) and on the anxiety (B) and depression (C) scores measured by the HADS questionnaire. For significant differences see the Results section.
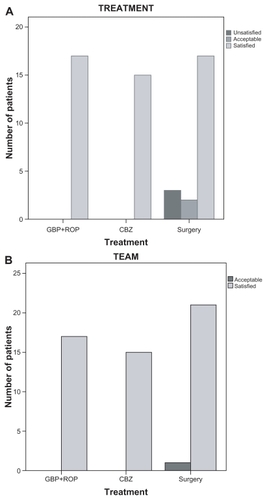
The satisfaction of the patients with the treatment and with the clinical team, measured by the QUASU questionnaire, revealed a complete or high level of satisfaction of patients (). While all patients allocated to protocols GBP+ROP and CBZ were totally satisfied with the treatment and clinical team, 5 out of 22 MVD patients were acceptably satisfied or unsatisfied with the treatment () due to sensory adverse side effects, and 2/22 MVD patients were just acceptably satisfied with the team ().
Discussion
Economic evaluation of different therapeutical approaches is intended to support health-related decision-making by informing clinical decision-makers of estimates of costs and benefits of surgery and comparing them with the prevalent pharmacological intervention. Although the three branches of the present study were randomly obtained at 3 different times, the clinical outcomes obtained and the direct costs associated reinforce the necessity of careful evaluation of the patient before the decision to make an invasive surgical intervention. All protocols, GBP+ROP, CBZ, and MVD, decreased pain behavior significantly in TN patients, as measured by the NRS scale and number of daily pain crises, and total or a high satisfaction with both the treatment and clinical team was achieved. However, the degree of adverse side effects was different between protocols, GBP+ROP showing no side effects and MVD presenting several facial sensorial deficits, with different levels of severity. Additionally, during the first month of treatment, a much higher cost was attributed to MDV protocol due to surgical procedures, hospital stay, and maintenance of drug therapy, whereas pharmacotherapy costs were mainly drug costs. On the contrary, during the follow-up the surgical protocol was the less costly protocol and GBP+ROP was the most expensive, indicating that in longer follow-ups the MVD is less expensive than a prolonged drug treatment.
Methodological considerations
The rationale of the present study was to compare the efficacy of different therapeutical approaches to TN and evaluate the direct costs associated with each one. The GBP+ROP protocol was chosen due to its improved efficacy as an association of an anticonvulsant and the analgesic block of TN trigger-points,Citation3 which can constitute a valid alternative whenever the classic first-choice pharmacological treatment, CBZ in monotherapy,Citation1 cannot be used. The CBZ protocol is still considered the first-line choice for TN treatment.Citation1,Citation54–Citation56 In order to eliminate the possibility that any beneficial effect could depend on the physical action of local administration of the analgesic ROP solution by clearing adhesions or inflammatory molecules from the vicinity of the nerve,Citation40 the CBZ protocol was accompanied by injection of saline to TN trigger-points. Thus, the improvements observed in the different outcomes analyzed resulted exclusively from the pharmacological action of GBP+ROP and CBZ and not from the manipulation and liquid introduction at trigger-points.Citation3,Citation15 The frequency of ROP analgesic block applied subcutaneously to TN patients followed the practice guidelines for the interventional techniques:Citation40 a patient received an injection at intervals of no less than 1 week, which was the period chosen to mediate between each ROP (or saline) administration. The MVD protocol is still considered the first-line surgical treatment for medically unresponsive TN,Citation57–Citation59 mainly in younger patients,Citation28 although radiosurgery is the main option in radiosurgery centers, especially when applied in older people.Citation28
Clinical impact of the three TN treatment protocols
Since a 2-point decrease in the mean NRS scale (0–10 scale) is considered the minimum clinical relevant difference in pain intensity when comparing the effect of 2 treatments,Citation43–Citation45 the GBP+ROP, CBZ, and MVD protocols, by decreasing pain intensity in 6.1, 5.3, and 5.7 (respectively) points, were clinically effective in reducing pain at month 6; additionally, all protocols also reduced significantly the number of daily pain crises. These results are in accordance with the literature in terms of efficacy in controlling pain in TN.Citation3,Citation15,Citation37 Since this study is a retrospective and observational evaluation of 3 sets of patients who were randomly allocated in 3 different studies, the degrees of reduction of pain values cannot be compared among protocols (both NRS scale values and number of daily pain crises). Another study has compared outcomes in a group of patients who have had both pharmacological and surgical TN treatments. Patients treated with oxcarbazepine and different surgeries (MVD and Gasser ganglion surgery) were compared and patients would prefer to have had surgery before.Citation60 Although sensory deficits and necessity for repeating surgery have occurred, pain relief was significantly longer after surgery than after pharmacological treatment, recurrence being 10 months after oxcarbazepine and 28 months after surgery. As these data cannot be extrapolated to other anticonvulsivant drugs, similar comparative studies should be performed in the future.
When comparing the effect of GBP+ROP, CBZ and MVD protocols between baseline (day 0) and month 6, other indications of the clinical outcome can be performed using specific questionnaires. The functional analysis of quality of life measured by the SIP indicated that functional improvement was significant after pharmacological protocols but not after MVD. This may result from the several patients with sensory deficits occurring after the latter, which may counteract the functional improvement resulting from pain control. This study shows that, in addition to GBP+ROP protocol,Citation3 CBZ improves functionality. Only 1 paper has evaluated SIP in a surgical context,Citation61 indicating improvement in TN patients after epidural motor cortex stimulation. HADS showed that only patients submitted to MVD showed a significant improvement in both anxiety and depression scores, probably because patients who are hospitalized for surgery have a very high degree of anxiety and expectation.Citation62 On the contrary, all GBP+ROP and CBZ patients were completely satisfied with the treatment protocol and the clinical team, whereas some MVD patients were unsatisfied or acceptably satisfied with the treatment protocol; this may result from the sequelae that were present in a significant number of MVD patients. Finally, CBZ protocol resulted in dizziness only in some patients and GBP+ROP patients showed virtually no adverse side effects.
Another important therapeutical improvement of GBP+ROP and MVD protocols is the demonstration of a large decrease in the daily dose of anticonvulsivant drug intake from baseline (day 0), both at the end of the treatment (day 29, GBP+ROP protocol) and, even further, after the 5-month follow-up (month 6).Citation3 On the contrary, in CBZ monotherapy a progressive increase was observed in daily CBZ dosage.Citation15 These data show that the clinical results of NT treatment with GBP+ROP and MVD are superior to those for CBZ monotherapy, because the significantly lower dose of drugs used strongly decreased the presence/intensity of adverse side effects.
Direct costs
The data presented in this study point to a much higher cost of the surgical approach to TN treatment than the other two pharmacological protocols. This results directly from the high costs of surgical intervention and hospital stay before, during, and after the MVD. However, during follow-up, the maintenance of pain control in TN patients submitted to surgery requires less medical therapy than the other two protocols. Although being clearly the less expensive treatment during the first 4-week treatment period, the GBP+ROP protocol tends to be the most expensive therapy after stabilization of TN pain control (follow-up) due to the higher cost of GBP drug (Neurontin® [Pfizer Laboratories, Porto Salvo, Portugal] or Gabamox® [Pentafarma, Prior Velho, Portugal]) versus CBZ drug (Tegretol® [Novartis Farma, Sintra, Portugal]). Data suggest that larger follow-up periods may reveal that the MVD approach is less expensive than the drug therapies. Only a few studies have evaluated the effects of drugs in the reduction of costs in TN,Citation34 or have compared the cost of different TN surgical protocols.Citation32,Citation33 In accordance with a less expensive experience resulting from MVD surgery, in a comparison between this surgery, glycerol rhizotomy, and stereotactic radiosurgery, it was shown that in longer follow-up intervals MVD is predicted to be the most cost-effective surgery and should be considered the preferred operation for patients.Citation32 However, recent data point to cyberknife radiosurgery being a cost-saving alternative to MVD.Citation33 The only study showing cost-saving using drug therapy in TN point to the use of pregabalin.Citation34 Finally, to the best of our knowledge, the present paper is the first attempt to compare clinical outcomes and costs among pharmacological protocols and the most common surgical approach in TN (excluding radiosurgery centers).
Limitations of the study
This study has some limitations. First, the rates of pain improvement in the three groups of patients are not directly comparable; although they were randomly selected, patients allocated to the CBZ and GBP+ROP branches were recruited from 2 different studiesCitation3,Citation15 and only the MVD patients were retrospectively selected for this specific study. Second, patients from MVD protocol had pain scores in the NRS scales significantly higher at baseline (day 0) than patients from CBZ and GBP+ROP protocols; the difference in patients’ characteristics is explained by the fact that MVD is usually not seen as an alternative to pharmacological protocols but, rather, as a second-line strategy whenever first-line or second-line drugs cause intolerable side effects or cannot control TN pain. Accordingly, the group of MVD patients had already failed the pharmacological therapy and thus had also longer pain periods than the patients from the other two protocols. Third, the complication rate of MVD patients may be higher than that in other published series, which is likely to be due to the small number of patients included in the study. Fourth, the cost analysis does not include costs associated with loss of productivity by patients during the admission and evaluation periods at the Hospital/Pain Unit and insurance contributions (indirect costs). Fifth, although the pain intensity and number of paroxysmal crises were significantly improved after 6 months of treatment with CBZ+ROP, CBZ, and MVD protocols, the follow-up period may not have been sufficient to determine the potential long-term effects of the treatments. Consequently, studies with larger numbers of patients, sequential allocation of patients for surgical and pharmacological branches, and longer follow-up periods should be undertaken to verify data obtained in the present study.
Conclusion
Although CBZ has long been known, and is still recognized, as the first-line drug choice for pain control in TN, an improvement of second-line drug therapy has been achieved by combining GBP intake with the peripheral analgesic block of TN trigger-points by ROP (GBP+ROP). Whenever pharmacological approaches fail, microvascular decompression is a surgical method of choice (MVD). We show that the three protocols resulted in a clinically significant improvement in pain, as shown by the NRS scale and number of paroxysmal pain crises, which were accompanied by a clear decrease in the daily CBZ/GBP dosage needed for TN pain control, with a consequent reduction in associated adverse side effects. The cost analysis indicates that the first 4-week period of treatment (or admission, surgery, and treatment in MVD patients) results in GBP+ROP being by far the least expensive protocol and MVD the most expensive. However, over time (follow-up), GBP+ROP protocol tended to be the most costly treatment and MVD the least expensive (very similar to CBZ protocol). Longer follow-up periods will potentially indicate that MVD is a less costly approach to TN than the drug treatments.
Acknowledgements
The authors thank the Clinical Director of the Hospital Center of Alto Ave (Fafe Unit) in 2008 and the Chronic Pain Unit team of the same Hospital for collaboration in this study. This study was supported by Project Nr. PTDC/SAU-NEU/108557/2008 from Fundação para a Ciência e Tecnologia (FCT) and FEDER.
Disclosure
No competing financial interests exist. All authors meet the criteria for authorship. We disclose that Armando Almeida and Laurinda Lemos serve as occasional speakers for Grünenthal SA (Portugal). Funding for the editorial support (not for the research) of this article was provided by Grünenthal SA.
References
- CheshireWPTrigeminal neuralgia: for one nerve a multitude of treatmentsExpert Rev Neurother200771565157917997704
- TölleTDukesESadoskyAPatient burden of trigeminal neuralgia: results from a cross-sectional survey of health state impairment and treatment patterns in six European countriesPain Pract2006615316017147591
- LemosLFloresSOliveiraPAlmeidaAGabapentin supplemented with Ropivacaine block of trigger-points improves pain control and quality of life in Trigeminal Neuralgia patients when compared with gabapentin aloneClin J Pain200824647518180639
- MarbachJJLundPDepression, anhedonia and anxiety in temporomandibular joint and other facial pain syndromesPain19811173847301402
- KatusicSWilliamsDBBeardCMBergstralhEJKurlandLTEpidemiology and clinical features of idiopathic trigeminal neuralgia and glossopharyngeal neuralgia: similarities and differences, Rochester, Minnesota, 1945–1984Neuroepidemiology1991102762811798430
- MacDonaldBKCockerellOCSanderJWShorvonSDThe incidence and lifetime prevalence of neurological disorders in a prospective community-based study in the UKBrain200012366567610733998
- Headache Classification Subcommittee of the International Headache SocietyThe International Classification of Headache Disorders, 2nd EditionCephalalgia200424Suppl 1S16S149
- CheshireWPTrigeminal neuralgia: a guide to drug choiceCNS Drugs1997798110
- SindrupSHJensenTSPharmacotherapy of trigeminal neuralgiaClin J Pain200218222711803299
- CampbellFGGrahamJGZilkhaKJClinical trial of carbazepine (tegretol) in trigeminal neuralgiaJ Neurol Neurosurg Psychiatry1966292652675327969
- JornsTPZakrzewskaJMEvidence-based approach to the medical management of trigeminal neuralgiaBr J Neurosurg20072125326117612914
- CruccuGGronsethGAlksneJAAN-EFNS guidelines on trigeminal neuralgia managementEur J Neurol2008151013102818721143
- ZakrzewskaJMChaudhryZNurmikkoTJPattonDWMullensELLamotrigine (lamictal) in refractory trigeminal neuralgia: results from a double-blind placebo controlled crossover trialPain1997732232309415509
- RoyalMWieneckeGMovvaVOpen label trial of ox carbamazepine in neuropathic painPain Med20012250151
- LemosLFontesRFloresSOliveiraPAlmeidaAEffectiveness of the association between carbamazepine and peripheral analgesic block with ropivacaine for the treatment of trigeminal neuralgiaJ Pain Res2010320121221197324
- SolaroCMessmer UccelliMUccelliALeandriMMancardiGLLow-dose gabapentin combined with either lamotrigine or carbamazepine can be useful therapies for trigeminal neuralgia in multiple sclerosisEur Neurol200044454810894995
- CheshireWPCan MRI distinguish injurious from innocuous trigeminal neurovascular contact?J Neurol Neurosurg Psychiatry2005a761470147116227531
- LangENaraghiRTanrikuluLNeurovascular relationship at the trigeminal root entry zone in persistent idiopathic facial pain: findings from MRI 3D visualisationJ Neurol Neurosurg Psychiatry2005761506150916227540
- PagniCAFariselliLZemeSTrigeminal neuralgia. Non-invasive techniques versus microvascular decompression. It is really available any further improvement?Acta Neurochir Suppl2008101273318642630
- CheshireWPTrigeminal neuralgia: diagnosis and treatmentCurr Neurol Neurosci Rep2005b5798515743543
- BarkerFGIIJannettaPJBissonetteDJThe long-term outcome of microvascular decomplression for trigeminal neuralgiaN Engl J Med1996334107710838598865
- LovelyTJJannettaPJMicrovascular decompression for trigeminal neuralgia. Surgical technique and long-term resultsNeurosurg Clin N Am1997811299018702
- KanpolatYSavasABekarABerkCPercutaneous controlled radiofrequency trigeminal rhizotomy for the treatment of idiopathic trigeminal neuralgia: 25-year experience with 1,600 patientsNeurosurgery20014852453211270542
- FountasKNLeeGPSmithJROutcome of patients undergoing gamma knife stereotactic radiosurgery for medically refractory idiopathic trigeminal neuralgia: Medical College of Georgia’s experienceStereotact Funct Neurosurg200684889616825804
- DhopleAAAdamsJRMaggioWWNaqviSARegineWFKwokYLong-term outcomes of Gamma Knife radiosurgery for classic trigeminal neuralgia: implications of treatment and critical review of the literatureJ Neurosurg200911135135819326987
- KnafoHKennyBMathieuDTrigeminal neuralgia: outcomes after gamma knife radiosurgeryCan J Neurol Sci200936788219294893
- RégisJMetellusPHayashiMProspective controlled trial of gamma knife surgery for essential trigeminal neuralgiaJ Neurosurg200610491392416776335
- KondziolkaDZorroOLobato-PoloJGamma knife stereotactic radiosurgery for idiopathic trigeminal neuralgiaJ Neurosurg201011275876519747055
- GorgulhoADe SallesAAMcArthurDBrainstem and trigeminal nerve changes after radiosurgery for trigeminal painSurg Neurol20066612713516876597
- RegisJArkhaYYomoSRadiosurgery in trigeminal neuralgia: long-term results and influence of operative nuancesNeurochirurgie20095521322219339026
- MassagerNMurataNTamuraMInfluence of nerve radiation dose in the incidence of trigeminal dysfunction after trigeminal neuralgia radiosurgeryNeurosurgery20076068168717415205
- PollockBEEckerRDA prospective cost-effectiveness study of trigeminal neuralgia surgeryClin J Pain20052131732215951649
- TarriconeRAguzziGMusiFFariselliLCasascoACost-effectiveness analysis for trigeminal neuralgia: Cyberknife vs microvascular decompressionNeuropsychiatr Dis Treat2008464765218830392
- PérezCSaldañaMTNavarroAMartínezSRejasJTrigeminal neuralgia treated with pregabalin in family medicine settings: its effect on pain alleviation and cost reductionJ Clin Pharmacol20094958259019299534
- NavarroASaldanaMTPérezCTorradesSRajasJA cost-consequences analysis of the effect of pregabalin in the treatment of peripheral neuropathic pain in routine medical practice in primary care settingsBMC Neurol20011117201121251268
- ZakrzewskaJMTrigeminal, eye, and ear painMelzackRWallPDHandbook of Pain Management – a clinical companion to Wall and Melzack’s Textbook of PainLondonChurchill Livingstone2003199215
- LonserRRApfelbaum. Neurovascular decompression in surgical disorders of cranial nerves V, VII, IX, and XSchmidekHHRobertsDWSchmidek and Sweet’s Operative Neurosurgical Techniques: Indications, Methods, and Results5th ed2PhiladelphiaSaunders/Elsevier200215311543
- AhmadMGouckeCRManagement strategies for the treatment of neuropathic pain in the elderlyDrugs Aging20021992994512495368
- BreivikHLocal anesthetic blocks and epiduralsMcMahonSBKoltzenburgMMelzack’s Textbook of Pain5th edLondonElsevier-Churchill Livingstone2006903925
- ManchikantiLSinghVTrescotAMDeerTRBoswellMVGuidelines for the Practice of Interventional TechniquesBoswellMVColeBEWeiner’s Pain Management: a practical guide for clinicians7th edLondonCRS Press2006847878
- LorenzoniJDavidPDevriendtDPatterns of neurovascular compression in patients with classic trigeminal neuralgia: a high-resolution MRI-based studyEur J Radiol200910.1016/j.ejrad.2009.09.017.
- CollinsSLMooreRAMcQuayHJThe visual analogue pain intensity scale: what is moderate pain in millimeters?Pain19977295979272792
- FarrarJTPortenoyRKBerlinJAKinmanJLStromBLDefining the clinically important difference in pain outcome measuresPain20008828729411068116
- FinnerupNBSindrupSHBachFWJohannesenILJensenTSLamotrigine in spinal cord injury pain: a randomized controlled trialPain20029637538311973012
- SalaffiFStancatiASilvestriCACiapettiAGrassiWMinimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scaleEur J Pain2004828329115207508
- ZigmondASSnaithRPThe hospital anxiety and depression scaleActa Psychiatr Scand1983673613706880820
- BjellandIDahlAAHaugTTNeckelmannDThe validity of the Hospital Anxiety and Depression Scale. an updated literature reviewJ Psychosom Res200252697711832252
- BergnerMBobbittRACarterWBThe sickness impact profile: development and final revision of a health status measureMed Care1981197878057278416
- TurnerJARomanoJMPsychological and psychosocial evaluationLoeserJDButlerSHChapmanCRTurkDCBonica’s Management of Pain3rd edPhiladelphiaLippincott Williams & Williams2001329341
- JamisonRNThe role of psychological testing and diagnosis in patients with painDworkinRHBreitbartWSPsychological Aspects of Pain: a handbook for health care providers. Progress in Pain Research and Management27SeattleIASP Press2004117137
- McIntyreTJohnstonMGouveiaJLResultados psicossociais na reabilitação pós enfarte do miocárdio em mulheres portuguesase escocesasProject POCTI/ESP/35749/1999, from the Foundation for Science and Technology (Portugal) http://alfa.fct.mctes.pt/apoios/projectos/consulta/vglobal_projecto.phtml.en?idProjecto=35749&sapiens=1999Accessed June 14, 2011
- Diário da República article 132/2008 (Portugal) Available at: http://www.dre.pt/Accessed June 29, 2011
- Simposium Terapêutico 2008 (Portugal) Available at: http://www.simposium.pt/pagina_inicioAccessed June 29, 2011
- ZakrzewskaJMLopezBCTrigeminal and glossopharyngeal neuralgiaMcMahonSBKoltzenburgMMelzack’s Textbook of Pain5th edLondonElsevier-Churchill Livingstone200610011010
- CanaveroSBonicalziVDrug therapy of trigeminal neuralgiaExpert Rev Neurother2006642944016533146
- AttalNCruccuGBaronREFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revisionEur J Neurol2010171113112320402746
- FujimakiTFukushimaTMiyazakiSPercutaneous retrogasserian glycerol injection in the management of trigeminal neuralgia: long-term follow-up resultsJ Neurosurg1990732122162195139
- LeeKHChangJWParkYGChungSSMicrovascular decompression and percutaneous rhizotomy in trigeminal neuralgiaStereotact Funct Neurosurg1997681961999711716
- ApfelbaumRINeurovascular decompression: the procedure of choice?Clin Neurosurg20004647349810944696
- ZakrzewskaJMPatsalosPNLong-term cohort study comparing medical (oxcarbazepine) and surgical management of intractable trigeminal neuralgiaPain20029525926611839425
- LefaucheurJPDrouotXCuninPMotor cortex stimulation for the treatment of refractory peripheral neuropathic painBrain20091321463147119336459
- CastroARSiqueiraSRPerissinottiDMTeixeiraMJSiqueiraJTEmotional aspects of chronic orofacial pain and surgical treatmentInt J Surg2009719619919281877