Abstract
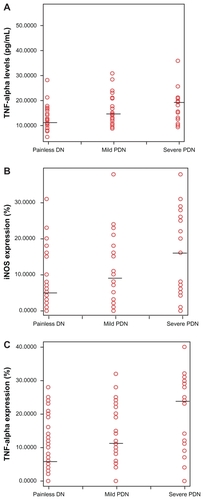
Painful diabetic neuropathy (PDN) is one of the most common complications of diabetes mellitus. Recently it has become clear that nitric oxide (NO) and proinflammatory cytokines play an important role in the pathogenesis of PDN. We investigated whether the cytokine tumor necrosis factor alpha (TNF-α) and NO play a role in PDN pathogenesis by performing a cross-sectional and a case–control study in 110 type 2 diabetic patients. Of 110 subjects, 59 patients suffered from PDN (cases) and the remaining were painless DN (controls). Cross-sectionally, plasma TNF-α levels and immunoreactivity for inducible NO synthase (iNOS) and TNF-α were higher in patients with more severe pain on the visual analog scale. There were statistically significant differences between mild and severe pain for TNF-α levels, iNOS immunoreactivity, and TNF-α immunoreactivity. There were statistically significant differences between mild and severe pain for TNF-α levels (mean 15.24 pg/mL ± 5.42 vs 20.44 ± 10.34), iNOS immunoreactivity (9.76% ± 8.60% vs 15.48% ± 11.56%), and TNF-α immunoreactivity (13.0% ± 9.48% vs 20.44% ± 11.75%). The case–control study showed that TNF-α had an odds ratio of 5.053 (P < 0.001), TNF-α immunoreactivity of 4.125 (P < 0.001), and iNOS immunoreactivity of 3.546 (P = 0.002). DN patients with high TNF-α levels, and high iNOS and TNF-α expression in macrophages are at risk of suffering from pain. The higher the TNF-α level, and iNOS and TNF-α immunoreactivity, the more severe the pain. These findings could form the basis of further research into better management of PDN.
Background
Uncontrolled diabetes can lead to acute and chronic complications, disability, and death. Diabetic neuropathy (DN) is a common complication of diabetes that can cause significant morbidity and mortality. It can be painful or painless. The reason for this difference in clinical presentation is as yet unknown.Citation1 The prevalence of painful diabetic neuropathy (PDN) in a population-based sample is 26.4%.Citation2 It can have a serious impact on quality of life, leading to severe depression and even suicide. The pathogenesis of PDN is complex and still poorly understood. In the past, research on neuropathic pain was focused on neurons and neurotransmitters. Recently it has become clear that nitric oxide (NO) and proinflammatory cytokines play an important role in the pathogenesis and maintenance of neuropathic pain. Neuroinflammation and neuroimmune activation occur following injury to peripheral nerves and nerve roots as well as in peripheral inflammatory models of persistent pain.Citation3,Citation4
The role of cytokines in the induction and maintenance of pain has been established in animal models, and clinical research has also provided evidence for the involvement of cytokines in painful and painless neuropathies.Citation5 Peripheral nerve injury induces activation of resident immune cells as well as recruitment of inflammatory cells to the site of lesion. There is increasing knowledge of the intracellular cascades that are activated in nociceptors by some mediators such as tumor necrosis factor alpha (TNF-α), interleukin (IL)-1β, IL-6, NO, prostaglandins (PG), nerve growth factor (NGF), and cyclo-oxygenase 2 (COX-2), which ultimately either activate or sensitize these neurons. Nerve injury also initiates Schwann cell de-differentiation and the release of several algesic mediators such as pro-inflammatory cytokines, NGF, prostaglandin E2 (PGE2), and ATP. This cocktail of mediators serves as a mechanism of enhanced inflammatory response in the injured nerve and contributes to neuropathic pain.Citation6,Citation7
TNF-α has been shown to be directly involved in the production of pain in several models of nerve injury. The effect of TNF-α on neurons seems to be mediated, directly and/or indirectly, by the phosphorylation of extracellular-regulated kinase and p38 mitogen-activated protein kinase,Citation8 translocation of nuclear factor kappa B (NFκB) to the nucleus, and activation of COX-2-dependent prostanoid release.Citation9 The phosphorylation of p38 mitogen-activated protein kinase may mediate mechanical allodynia via a modulation of tetrodotoxin-resistant Na channels.Citation10 TNF-α also activates NFκB for initiation of NOS (NO synthase), and NO production whereas NO is a pain neurotransmitter.Citation11 Inhibition of serum TNF-α and NO levels with insulin and its combinations with resveratrol and curcumin contribute in attenuating DN pain, since TNF-α plays an important role in the development of DN.Citation12
The role of NO in pathogenesis of PDN seems to be via upregulation of inducible NO synthase (iNOS) as a result of chronic inflammation. Lowenstein et al showed that there were reciprocal interactions between NO and PG, high levels of NO increased PDN, and iNOS inhibitor attenuated PDN.Citation11 With this background, the present study was designed to explore the plasma levels of TNF-α and iNOS and TNF-α expression in macrophages as risk factors for PDN.
Methods
Subjects
One hundred and ten type 2 diabetic patients who fulfilled inclusion criteria were enrolled in this study (61 women and 59 men, mean age 54.1, range 37–65 years). Patients were recruited consecutively at the outpatient Clinic of Neurology and Internal Medicine Sanglah Hospital Denpasar, Bali from 1 October 2008 until 31 July 2009. The patients had a mean duration of diabetes of 5.30 years (2–10 years). Of 110 subjects, 59 patients suffered from PDN (cases) and the remaining 51 patients had painless DN (controls). The clinical characteristic of subjects and comparison of case and control group are given in and .
Table 1 Characteristics of diabetic neuropathy patients
Table 2 Comparison of clinical data of painful DN (cases) and painless DN (controls)
Inclusion criteria for the cross-sectional study were type 2 diabetes patients, age 20–65 years, duration of diabetes 2–10 years, and signed written informed consent. For the case–control study, the criteria were the same as for the cross-sectional study plus painless DN for control and PDN for case.
Exclusion criteria included: ongoing local and systemic infection (documented with a blood cell count and erythrocyte sedimen rate), active ulcer in the leg, patients under treatment with glyceryl trinitrate or sildenafil, herbal or synthetic medications containing antioxidant or anti-inflammatory substances, and patients suffering from other types of neuropathic pain. To minimize confounding factors for blood cytokine levels, the study conditions were standardized by applying the following exclusion criteria: heavy physical activity in the last 3 days, food intake within 60 minutes before blood sampling, alcohol consumption up to 24 hours before the examination, and any current infectious disease or fever.
Procedure
The study was carried out in two steps. The first step was cross-sectional study and the second step was a case–control study. In the cross-sectional study, type 2 diabetic patients who visited the outpatient Neurology and Internal Medicine Clinic Sanglah Hospital underwent anamnesis, neurological, laboratory, and electromyoneurography (ENMG) examinations. Anamnesis included: sensory, motor, and autonomic symptoms of DN. The neurologic examination included: sensory, motor, autonomic functions, and reflexes. The diagnosis of a DN was based on a typical history and thorough neurologic and ENMG examinations. Laboratory studies included: erythrocyte sedimentation rate, whole blood, blood sugar, glycosylated hemoglobin (HbA1C), urea, creatinine, and liver function test. A complete electrophysiologic assessment with standard nerve conduction studies in motor and sensory nerves at upper and lower extremities was performed in all diabetic patients. Nerve conduction studies revealed low compound muscle action potentials and sensory nerve action potentials or low conduction velocities.
Patients who had DN and fulfilled inclusion criteria were recruited in the case–control study and were asked to assess their pain intensity on a visual analog scale (VAS), with 0 representing no pain and 10 representing the worst pain imaginable. Patients were assigned to two groups according to their VAS: 1–5 mild pain and 6–10 severe pain. Patients were examined by blood tests for plasma TNF-α levels by ELISA and for iNOS and TNF-α expression in macrophages immunohistochemically.
Blood for TNF-α analysis was drawn in the morning, stored at 4°C, centrifuged at 1500 rpm for 10 minutes, and the plasma was stored at −20°C until assayed. The presence of TNF-α in plasma was detected by a commercially available ELISA Kit (R&D system, Wiesbaden, Germany).
Detection of TNF-α and iNOS expression in macrophages was performed immunohistochemically. Approximately 3 mL blood was collected from DN patients. The blood was centrifuged at 1500 rpm for 10 minutes and the plasma collected into small aliquots. Buffy coat layer at the interface was collected into a clean centrifuge tube. Red blood cells present in the buffy coat were lyzed using 0.8% NH4Cl for 1 minute and leukocytes were pelleted by centrifugation as above. Leukocytes were washed twice by repeated centrifugation and a thin smear of leukocytes at a density of 1 million per 1 mL phosphate-buffered saline (PBS) was prepared on poly-L-lysine microscope slides. After air drying, the leukocytes were fixed with cold acetone for 20 minutes. The endogenous peroxidase of the leukocytes was then inactivated by 3% H2O2 in PBS for 30 minutes at room temperature. After blocking with 2% skim milk in PBS, monoclonal antibodies (Mab) against TNF-α (BIODESIGN International®, Saco, ME) and against iNOS (Santa Cruz Biotechnology, Inc, Santa Cruz, CA) was added into leukocytes smear on microscope slides. After three washes with PBS (pH. 7.4) and incubation for 1 hour at room temperature, the bound Mabs were detected by biotinylated goat anti-mouse IgG (BIODESIGN International) and avidin-horse radish peroxidase (Sigma-Aldrich, St Louis, MO). The expression of TNF-α and iNOS was then visualized by adding diazinobenzidine substrates (Sigma-Aldrich; 50 mg/50 mL PBS containing 0.07% H2O2). The mononuclear cells expressing iNOS and TNF-α were counted under 450× magnification by observation of 100 cells.
Data obtained from this study comprised descriptive analysis, Student’s t-test, bivariate correlation test, and cross tab (chi-square test and odds ratio). The data were analyzed using SPSS software, version 15, with significance set at P < 0.05.
Results
Cross-sectional study
Of 110 subjects, 59 patients suffered from PDN which consisted of mild pain in 34 and severe pain in 25. Plasma TNF-α levels, and iNOS and TNF-α expression were higher in patients with more severe pain in the VAS (P < 0.05) as shown in .
Figure 1 Scatter plots illustrating plasma TNF-α levels, iNOS and TNF-α expression in patients with Painless DN (n = 51), mild PDN (n = 34) and severe PDN (n = 25). The short horizontal line marks median values. (A) Patients with severe PDN had higher plasma TNF-α levels than patients with mild PDN (P < 0.001) and Painless DN (P < 0.001) (B) Patients with severe PDN had higher iNOS expression than patients with mild PDN (P < 0.001) and Painless DN (P < 0.001). (C) Patients with severe PDN had higher plasma TNF-α levels than patients with mild PDN (P < 0.001) and Painless DN (P < 0.001). In patients with PDN plasma TNF-α levels were 1.4 (P < 0.05), iNOS expression was 2.1 (P < 0.05), and TNF-α expression were 1.98 (P < 0.05) fold higher than in Painless DN.
Correlation between pain intensity and risk factors for PDN (age, duration of diabetes, blood sugar level, HbA1C, plasma TNF-α level, TNF-α, and iNOS expression) are given in .
Table 3 Correlation between pain intensity and some risk factors of painful diabetic neuropathy
Correlation between pain intensity and age, duration of diabetes, fasting blood sugar, blood sugar 2 hours postprandial, and HbA1C were not statistically significant (P > 0.05) whereas correlation between pain intensity and plasma TNF-α level, TNF-α, and iNOS expression were statistically significant (r = 0.330, 0.284, and 0.275, respectively; P < 0.05). To investigate the correlation between plasma TNF-α, and iNOS and TNF-α expression in macrophages as risk factors of PDN, a bivariate correlation test was conducted. There were positive correlations between 3 risk factors above that statistically significant (P < 0.05). Correlation between plasma TNF-α and iNOS expression was moderate (r = 0.351), correlation between plasma TNF-α and TNF-α expression was also moderate (r = 0.389), whereas correlation between TNF-α and iNOS expression was strong (r = 0.708).
Cross-sectionally the higher the plasma TNF-α levels, and the iNOS and TNF-α expression in macrophages, the more severe the pain. There were positive correlations between pain intensity and plasma TNF-α levels, and iNOS and TNF-α expression, and also moderate to strong correlations between the three risk factors above.
Case-control study
DN patients with high plasma TNF-α levels had a higher risk of getting PDN than those with low plasma TNF-α levels (odds ratio [OR] 5.053, 95% confidence interval [CI] 2.241–11.392; P < 0.001).
DN patients with high TNF-α expression had a higher risk of getting PDN than those with low TNF-α expression (OR 4.125; 95% CI, 1.805–9.425; P < 0.001).
DN patients with high iNOS expression had a higher risk of getting PDN than those with low TNF-α expression (OR 3.546; 95% CI, 1.613–7.795; P < 0.002).
High HbA1C levels did not increase the risk of getting PDN compared with low plasma HbA1C levels (OR 2.380; 95% CI, 0.996–5.688; P > 0.05).
In the case-control study, plasma TNF-α was consistently the most important risk factor for PDN, both directly and indirectly, by increasing macrophage expression of TNF-α and iNOS.
Discussion
In this study of 110 subjects who fulfilled cross-sectional inclusion criteria, all subjects also fulfilled inclusion criteria for the case–control study; 59 subjects suffered from PDN and 51 subjects suffered from painless DN. All patients who had had diabetes for 2 years or more suffered from DN, a finding supported by previous work that showed that DN as a complication of diabetes was already present in the early stage of hyperglycemia before clinical diagnosis.Citation13
Plasma TNF-α and expression of iNOS and TNF-α in macrophages according to pain intensity are compared in . The higher the plasma TNF-α levels, and the iNOS and TNF-α expression in macrophages, the more severe the pain. These differences were statistically significant. These results are in agreement with those of a previous study of cytokine expression in nervus suralis biopsy specimen of neuropathy patients. Patients with painful neuropathies showed a stronger TNF-α immunoreactivity than patients with nonpainful neuropathy.Citation14 Another study reported that patients with a painful neuropathy had about 2-fold higher TNF-α mRNA and protein levels than healthy control subjects, and about 2-fold higher IL-2 and TNF mRNA and protein levels than patients with painless neuropathy (all differences significant).Citation15
Our study showed plasma TNF-α level in PDN was almost 1.5 × higher than PDN, and TNF-α expression in PDN was nearly 2 × higher than PDN. Doganay et al investigated the relationship between the stages of DR (diabetic retinopathy) and serum levels of NO and many inflammatory cytokine such as NO, sIL-2R, IL-1β, IL-6, IL-8, and TNF-α. Serum NO levels ranged from 80 to 188 μmol/l, with the highest values obtained in patients with PDR (proliferative diabetic retinopathy). The mean serum NO, sIL-2R, IL-8, and TNF-α levels increased with the stage of DR and the highest levels were found in patients with PDRCitation16. Patients with small fiber neuropathy (SFN) had a 2-fold higher gene expression for IL-2 (P < 0.0001), IL-10 (P = 0.01), and transforming growth factor-β1 (P = 0.001) in peripheral blood whereas patients with length-dependent SFN had higher gene expression in the affected distal skin than in nonaffected skin for TNF-α (2.6-fold; P = 0.04), IL-1β (2-fold; P = 0.02), IL-6 (>200-fold; P = 0.01), and IL-8 (>500-fold; P = 0.046).Citation17
In our study, the highest levels of plasma TNF-α, and iNOS and TNF-α expression, were also found in patients with PDN. Pro-inflammatory cytokines (IL-1β, IL-2, IL-6, IFN-γ, TNF-α) in the plasma were correlated with increasing pain intensity. Chronic pain patients show a significant increase in plasma levels of NO in comparison with healthy controls.Citation4 Another study also showed a correlation between pro-inflammatory cytokine and pain intensity or severity of the disease in juvenile rheumatoid arthritisCitation18 and fibromyalgia.Citation19
There were positive correlations between pain intensity and plasma TNF-α level, and iNOS and TNF-α expression, and also a moderate to strong correlation between these three risk factors. Correlation between pain intensity and age, duration of diabetes, fasting blood sugar, blood sugar 2 hours postprandial and HbA1C were not statistically significant, indicating that above factors were not proven to increase PDN.
According to these results and those of some other investigations, a pathophysiological relationship can be shown between TNF-α, iNOS, and PDN, as depicted in .
Figure 2 Pathophysiological relationship between TNF-α, iNOS, and painful diabetic neuropathy.
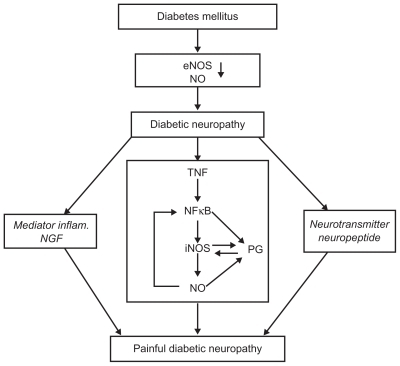
Prolonged hyperglycemia in diabetic patients can cause diabetic pain through many mechanisms, including metabolic, oxidative stress, immunologic, advanced glycosylation of end products, and vascular. All of these mechanisms are closely related to decreased endothelial NOS (eNOS), which is followed by a decrease in NO. NO derived from the eNOS could inhibit platelet aggregation and proliferation of smooth muscle. NO also a potent vasodilator.Citation20 A decrease in NO will result in vessel endothelium disruption followed with nerve fiber disruption. Under chronic hyperglycemia, endogenous TNF-α production is accelerated in microvascular and neural tissues, which may undergo increased microvascular permeability, hypercoagulability, and nerve damage, thus initiating and promoting the development of DN.Citation21
Dysfunction or lesion in peripheral nerve fibers leads to membrane remodeling and hyperexcitability which in turn cause diabetic pain. Lesion in primary afferent nerve fibers will induce activation of immune resident cells and recruitment of inflammatory cells to the inflamed cell. Then inflammation cascade takes place as activated mast cells release TNF-α which sensitizes nociceptors and contribute to neutrophils and macrophages recruitment. In nerve cells, neutrophils and macrophages produce and secrete neurotransmitter, neuropeptide and inflammatory mediators such as TNF-α, PGE2, bradykinin, serotonin, histamine, and NGF. These mixed mediators activate nociceptors directly, cause sensitization, and contribute to neuropathic pain, which result in pain, spontaneous or primary hyperalgesia.Citation6
Binding of TNF-α to its receptors on the cell surface initiates several signalling events, such as activation of p38 MAP kinase signalingCitation8 and translocation of NFκB into the nucleus.Citation9 NFκB then upregulates transcription of several genes, including COX-2, iNOS, TNF-α, IL-1β, and IL-6.Citation22 NFκB itself can be activated by oxygen radicals, suggesting a positive feedback loop in which NO might activate transcription factors, which in turn could increase NO synthesis by causing additional iNOS expression.
The role of NO is thought to be through increased iNOS following chronic inflammation in diabetic pain. Strong evidence supports a reciprocal relationship between NO and PGs biosynthetic pathways.Citation23 The interaction between NO and PGs biosynthesis occurs in some levels. NO directly influences COX expression and PGs biosynthesis. Conversely, arachidonic acid and its metabolites, which are produced by COX isoform, also have an effect on NO biosynthesis. The ability of NO to directly activate COX-2 is supported by evidence that NO increases purified COX-2 recombinant enzymes. NO also influences COX-2 enzyme activities by post-transcription and translation processes which make macrophages increase their PGs production. There is evidence that NO also activates COX-2.Citation24 NO release by constitutive NOS in basal conditions deactivates iNOS by inhibition of NFκB signal. NFκB signal is one of the signaling pathways for iNOS expression by means of extracellular mediators, including TNF-α (proinflammatory cytokine) and endotoxin.Citation16 At low NO concentration, NFκB remains inactive,Citation23 while at high NO concentration, NFκB is not suppressed by NO, so that it activates iNOS by producing combination anion superoxide from peroxynitrite. NFκB is a strong COX-2 inducer and the inhibitory role of NO in COX-2 is mediated by NFκB inhibition. NO is produced by many types of cells in peripheral tissues after inflammation has occurred. Once expressed, iNOS produces NO in large amounts for a long period.Citation25
High NO is related to PDN while iNOS inhibitor can decrease PDN symptoms.Citation12,Citation26,Citation27 Evidence that TNF-α and iNOS have important roles in the pathogenesis of PDN can lead to a new strategy of therapy – that of modulating the NO pathway and neuroimmune system. Modulation can be achieved by specifically inhibiting iNOS, antibody cytokine receptors, and TNF-α.
Conclusion
DN patients with high TNF-α levels, and high iNOS and TNF-α immunoreactivity of macrophages, are at risk of suffering from pain. The higher the TNF-α level, and iNOS and TNF-α immunoreactivity, the more severe the pain. This supports the hypothesis that TNF-α and iNOS have a role in PDN pathogenesis. The results of this research could be used as a basis for further research in pursuit of better management of PDN.
Acknowledgments
The author would like to acknowledge Claudia Sommer from Wuerzburg University West Germany for critically reading this manuscript, Djoenaidi Widjaja from Airlangga University Surabaya, Ketut Suastika and Nyoman Mantik Astawa from Udayana University Bali for his support in this research.
This research was funded by Indonesian Department of Health as part of dissertation from doctoral study of the author.
Disclosure
The author declares no conflicts of interest in relation to this work.
References
- UceylerNSommerNStatus of immune mediators in painful neuropathiesCurrent Pain and Headache Report200812159164
- DaviesMWilliamRBrophySTaylorAThe prevalence, severity and impact of painful diabetic peripheral neuropathy in type 2 diabetesDiabetes Care2006291518152216801572
- MoalemGTraceyDJImmune and inflammatory mechanisms in neuropathic painBrain Res Rev20065124026416388853
- KochAZacharowskiKBoehmONitric oxide and pro-inflammatory cytokines correlate with pain intensity in chronic pain patientsInflamm Res200756323717334668
- SommerCSchäfersMMechanisms of neuropathic pain: the role of cytokinesDrug Discov Today20041441446
- MoalemGTraceyDJImmune and inflammatory mechanisms in neuropathic painBrain Res Rev20065124026416388853
- ThackerMAClarkAKMarchandFMcMahonSBPathophysiology of peripheral neuropathic pain: immune cells and moleculesAnesth Analg200710583884717717248
- SchäfersMSvenssonCISommerCSorkinLSTumor necrosis factor-alpha induces mechanical allodynia after spinal nerve ligation by activation of p38 MAPK in primary sensory neuronsJ Neurosci2003232517252112684435
- DinarelloCA1999Overview of inflamatory cytokines and their role in painWatkinsLRMaierSFCytokines and PainBaselBirkhauser Verlag2003139
- JinXGereanRAcute p38-mediated modulation of tetrodotoxin-resistent sodium channels in mouse sensory neuron by tumor necrosis factor-αJ Neurosci20062624625516399694
- LowensteinCJDinermanJLSnyderSHNitric oxide: a physiologic messengerAnn Intern Med19941202272378273987
- SharmaSChopraKKulkarniSKEffect of insulin and its combination with resveratrol or curcumin in attention of diabetic neuropathic pain: participation of nitric oxide and TNF-alphaPhytother Res20072127828317199240
- QuanDDiabetic neuropathy http://emedicine.medscape.com/article/1170337-overviewAccessed Sep 20, 2008
- EmpMRenaudSErneBTNF-alpha expression in painful and nonpainful neuropathiesNeurology2001561371137711376190
- ÜçeylerNRogauschJPToykaKVSommerCDifferential expression of cytokines in painful and painless neuropathiesNeurology200769424917606879
- DogonaySEverekliogluCTurkozYServincAMehmetNSavliHComparison of serum NO, TNF-α, sIL-2R, IL-6 and IL-8 levels with grades of retinopathy in patients with diabetes mellitusEye20021616317011988817
- ÜçeylerNKafkeWRiedigerNElevated proinflammatory cytokine expression in affected skin in small fiber neuropathyNeurology2010741806181320513817
- ChenDYLanJLLinFJHsiehTYProinflammatory cytokine profiles in sera and pathological tissues of patients with active untreated adult onset Still’s diseaseJ Rheumatol2004312189219815517632
- GurAKarakocKCevikRDenliASaracJCytokine and depression in cases with fibromyalgiaJ Rheumatol20022935836111838856
- De CaterinaRLibbyPPengHBNitric oxide decreases cytokine-induced endothelial activation: nitric oxide selectively reduces endothelial expression of adhesion molecules and proinflammatory cytokinesJ Clin Invest19959660687542286
- SatohJYagihashiSToyotaTThe possible role of tumor necrosis factor-alpha in diabetic polyneuropathyExp Diabesity Res20034657114630568
- TegederLNiederbergerESchmidtRSpecific inhibition of IkappaB kinase reduces hyperalgesia in inflammatory and neuropathic pain models in ratsJ Neurosci2004241637164514973242
- MollaceVMuscoliCRotirotiDNisticomGSpontaneous induction of nitric oxide- and prostaglandin E2-release by hypoxic astroglial cells is modulated by interleukin 1 betaBiochem Biophys Res Commun19972389169199325192
- TogashiHSasakiMFrohmanENeuronal (type I) nitric oxide synthase regulates nuclear factor kappaB activity and immunologic (type II) nitric oxide synthase expressionProc Natl Acad Sci U S A199794267626809122255
- NathanCNO as a secretory product of mammalian cellsFASEB J19926305130641381691
- De AlbaJDClaytonNMCollinsSDColthupPChessellIKGW 274150, a novel and highly selective of the iNOS, shows analgesic effects in rat models of inflammatory and neuropathic painPain200612017018116360270
- MellerSTCummingsCPTraubRJGebhartGFThe role of nitric oxide in the development and maintenance of the hyperalgesia produced by intraplantar injection of carrageenan in the ratNeuroscience1994603673748072688