Abstract
Background
The aim of this study was to evaluate nondrug management practices concerning pain induced by blood sampling in newborns in a Moroccan neonatal unit and to determine whether the results reported from a randomized clinical study of nondrug analgesia could be reproduced in a routine care setting.
Methods
Standardized prospective observation of analgesic practices used during blood sampling was performed. Pain was assessed using the Douleur Aiguë Nouveau-né (DAN, [Newborn Acute Pain]) scale that incorporates facial expression, vocal expression, and limb movements of the newborn during realization of a painful procedure. Five different nondrug analgesic practices were investigated in 125 infants.
Results
Median DAN scores for the five methods were 6 (1–10) for venous sampling with oral administration of 30% glucose, 5 (1–10) for venous sampling with sucking, 3 (0–6) for venous sampling with oral administration of 30% glucose combined with sucking, 4 (0–10) for venous sampling with oral administration of 30% glucose combined with sucking and administration of 2 mL of adapted infant formula, and 6 (3–8) for venous sampling with administration of 2 mL of adapted infant formula.
Conclusion
Oral administration of 30% glucose combined with sucking provided better control of pain induced by blood sampling in newborns at our neonatal unit.
Keywords:
Introduction
The reality of neonatal pain is no longer questioned, but its management in clinical practice remains a challenge. Nonpharmacological strategies are an important aspect of neonatal pain management, and can be used either alone or combined with drug treatment. These methods are not necessarily substitutes for pharmacological treatment, but are complementary strategies and particularly attractive for management of acute pain such as that associated with a blood test. They include sucrose (not available in our hospital pharmacy), milk, non-nutritive sucking, and glucose 30%. The objective of this study was to compare the analgesic effects of oral administration of glucose 30%, milk, or sucking a pacifier, and the synergistic analgesic effect of 30% glucose, milk, and a teat during venous punctures in the newborn.
Materials and methods
This was a randomized, prospective, observational, comparative study conducted at the National Reference Center of Neonatology and Nutrition in the Children’s Hospital at Rabat over a period of 3 months from July to September 2007. Included in the study were full-term or premature neonates (28–37 weeks of gestation) who were older than 24 hours and required a blood sample as part of their routine care. Parental consent was obtained in all cases. Unstable infants, those with neurological disease or a contraindication to enteral nutrition, those who had received an analgesic in the 24 hours prior to sampling, and those who were crying before venous sampling were excluded from the study.
Methodology
An information sheet was established for each newborn, and included gender, gestational age, corrected age, weight on day of sampling, duration of hospitalization, and trophicity (estimated using the curves of Leroy and Lefort), along with parameters associated with venipuncture, including the reason for sampling, the site of venipuncture, and number of attempts and bottles collected. Feeding was withheld in the hour before sampling. Glucose and milk were administered in a volume of 2 mL on the tongue of the newborns using a sterile syringe over a period of 2 minutes before venipuncture. The teat was placed in the mouth of the baby during blood sampling, which was performed by the same nurse.
Outcome measures
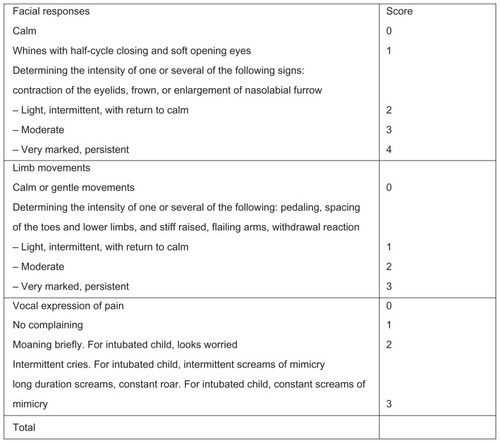
The main criterion used to assess the analgesic efficacy of these nondrug methods was observation of pain in the newborn during blood sampling. This was performed using the Douleur Aiguë Nouveau-né (DAN, [Newborn Acute Pain]) behavioral pain scale () that incorporates facial expression, vocal expression, and limb movements of the newborn upon realization of a painful stimulus.Citation1 The scores were calculated by a single observer who was blinded to the purpose of the study.
Determination of group size
We calculated that we would need 25 infants in each group to detect a difference of two points in the DAN scale with 80% power and 5% significance. The 125 neonates were randomly assigned to one of five groups as follows:
Group 1 – oral administration of 2 mL of glucose 30%
Group 2 – non-nutritive sucking of a teat
Group 3 – oral administration of glucose 30% (taken from an intravenous bag) prior to venipuncture, with sucking triggered using a nipple at the end of administration of glucose and maintained until completion of venipuncture
Group 4 – oral administration of glucose 30%, prior to venipuncture, with sucking triggered at the end of administration of glucose and maintained until completion of venipuncture using a prefilled nipple with age-appropriate (preterm or full term) formula milk
Group 5 – oral administration of age-appropriate formula milk.
Statistical analysis
The data collected were analyzed using the Statistical Package for the Social Sciences version 9.0 (SPSS Inc, Chicago, IL). The analysis was done at the Laboratory of Biostatistics and Epidemiology and Clinical Research, Faculty of Medicine and Pharmacy in Rabat. Comparisons between normally distributed data were made using the Student’s t-test for comparison of two groups and analysis of variance for comparisons involving three or more groups. Data which were not normally distributed were compared using the nonparametric Kruskal-Wallis test for more than two groups and using the Mann-Whitney test for pairwise comparisons. Qualitative data were compared using Pearson’s Chi-square test. Factors recorded during sampling that may influence pain scores were explored in univariate analysis. For comparisons of all modalities of care, the statistical significance level was set at P < 0.05.
Results
One hundred and twenty-five infants were included in the study, of whom 61% were female, 50% were premature, and 45% were small for gestational age. Mean gestational age was 34 ± 3.2 weeks. The five treatment groups were similar with regard to gender, weight, gestational age, postnatal age, length of hospitalization, and distribution according to whether the infant was awake or asleep without crying before venipuncture. There were no significant differences between the groups with regard to sampling site, number of attempts before a successful blood collection, and the number of tubes collected from each newborn ().
Table I Epidemiological characteristics of newborn (Mean and range) and Comparison of different groups for the site of sampling the number of attempts and the number of bottles collected
Analysis of pain scores showed that venipuncture associated with 30% glucose or artificial milk gave a median DAN score (on a scale of 0–10) of 6 in both groups. The upper limit of the interquartile range was 8 for 30% glucose and 7 for milk in the groups, which meant that only 25% of infants receiving milk felt pain scored over 7, while pain was scored more than 8 in the 30% glucose group. The use of 30% glucose and a nipple alone resulted in median DAN scores of 6 and 5, respectively. The upper limit of the interquartile range was 8 for 30% glucose and 7 for the nipple, meaning that 25% of neonates in the nipple group had a pain score over 7, while the pain score was greater than 8 in the glucose 30% group. The analgesic effect was significant in the group receiving the combination of 30% glucose + nipple because the median score was 3, with an upper limit of 4 for the interquartile range, meaning that 75% of neonates had a pain score less than 4. Indeed, when comparing pain scores obtained in the 30% glucose group with those obtained in the 30% glucose + nipple group, a very significant difference was found, whereas this difference was not significant in the glucose group compared with the 30% + teat + milk group (). Furthermore, the clinical condition of neonates after venipuncture was compared between the groups to determine if the method of pain management had an influence on recovery. About 80% of neonates in the 30% glucose, milk, and nipple groups did not cry after their painful blood sampling procedures, but this figure reached 100% in the 30% glucose + nipple group, in which no baby cried after venipuncture.
Table 2 DAN scores achieved during venipuncture
Discussion
This study has shown that 30% glucose, artificial milk, or sucking a pacifier has an analgesic effect in the management of pain in the neonate during peripheral venous puncture. The most effective synergistic combination that can be recommended in this context is sucking a nipple combined with administration of glucose 30%. Indeed, the effectiveness of a sugar solution as an analgesic in the newborn during venipuncture is now well established.Citation2–Citation6 Sucrose and glucose are the substances most commonly used, either alone or associated with sucking. The analgesic effect of oral glucose at concentrations ranging from 25% to 30% has been confirmed by several studies in term neonates during venipuncture and in preterm infants during subcutaneous injection and venipuncture.Citation2,Citation3 The sugar might work by releasing endogenous opioids,Citation7 and the sweet taste has an immediate and short-acting effect which calms the crying neonate.Citation8 Furthermore, the analgesic effect of non-nutritive sucking from a nipple has been reported by several authors. The analgesic effect of sucking along with cuddling can be used as a consoling measure.Citation9
Carbajal et al found that non-nutritive sucking of a teat had a better analgesic effect than administration of a sweet solution, but that there was a synergistic effect between sucking a pacifier and administration of a sugar solution.Citation3 We have verified this observation in the present study, given that non-nutritive sucking of a teat had the same analgesic effect as glucose 30%. The median DAN score was 5 for non-nutritive sucking versus 6 in the 30% glucose group. The effect of glucose 30% combined with a nipple was better than that of 30% glucose alone (P = 0.0001) or the nipple alone (P = 0.002).
Several scoring systems are used in daily practice for assessment of pain. We opted for the DAN scale on the grounds of its simplicity. It has been validated in terms of its metric qualities, and it has demonstrated high intraindividual and interindividual sensitivity.Citation10 Neonatal pain in this study was assessed by a single observer. Several studies have shown that most preterm infants have less pronounced facial and body responses to pain than near-term children.Citation11,Citation12 In our study, the proportion of full-term and preterm infants was observed in each group and the mean gestational age was the same 34 weeks of gestation. Postnatal age and duration of hospitalization were also considered, because these could influence the number of repeated painful procedures that infants are exposed to as well as changes in their response to pain. Taddio et al, Johnston and Stevens showed that full-term newborns who underwent multiple heel punctures during the first hours of life learned to anticipate pain and exhibited more intense pain responses during a subsequent venipuncture.Citation13,Citation14 The same applies to the distribution of neonates according to stages of sleep-wake. This is important to check, given the evidence that facial expression is more pronounced if the painful procedure is performed when a child is awake.Citation15
In 1997, Blass published a study which aimed to determine whether milk and its components could reduce the duration of crying during and after taking of blood samples for determination of phenylketonuria in neonates.Citation16 The results showed that administration of milk reduced crying time during collection, and that administration of sucrose, lipids, and proteins were effective 3 minutes after sampling, while water containing lactose had no effect. Blass concluded that milk and some of its components had an antinociceptive effect. Artificial milk delivered orally using a syringe yielded a median DAN score of 6, which was similar to that obtained with 30% glucose alone. The milk used in our study, in the absence of breast milk, was appropriate for gestational age. Breastfeeding, when available, remains an interesting alternative when studying the analgesic effect of combining milk and sucking during heel stick and venipuncture procedures.Citation17,Citation18 A systematic review by Shah et al of the effectiveness of breastfeeding or supplemental breast milk in relieving procedural pain in neonates showed that breastfeeding and supplemental breast milk (ie, given via a bottle or nasogastric tube) reduces signs of pain and distress, that breastfeeding is more effective than swaddling or use of a pacifier, and has a similar efficacy to that of administration of sucrose.Citation19 Other studies support these conclusions. Efe and Ozer found that breastfeeding was an effective way of relieving pain during neonatal immunization,Citation20 and Efe and Savaser found no difference in the analgesic effect of breastfeeding and administration of sucrose during venipuncture.Citation21
No adverse effects were observed in our patients after administration of glucose. There is no risk of hyperglycemia using the glucose strategy, because the doses used (0.1–0.15 g/kg) represent only 1%–2% of the daily glucose requirement of the newborn.
Conclusion
Administration of 30% glucose, which is readily available in all hospitals, when combined with sucking a nipple, showed at least the same efficacy as that described in the literature for 30% sucrose when used as analgesia for peripheral venous punctures. However, breastfeeding if available is a better alternative.
Disclosure
The authors report no conflicts of interest in this work.
References
- CarbajalRPaupeAHoennELenclenROlivier-MartinMAPH: evaluation of behavioural scale of acute pain in newborn infantsArch Pediatr199746236289295899
- SkogsdalYErikssonMSchollinJAnalgesia in newborns given oral glucoseActa Paediatr1997862172209055897
- CarbajalRLenclenRGajdosVJugieMPaupeACrossover trial of analgesic efficacy of glucose and pacifier in very preterm neonates during subcutaneous injectionsPediatrics200211038939312165596
- HaouariNWoodCGriffithsGLeveneMThe analgesic effect of sucrose in full term infants: a randomised controlled trialBMJ1995310149815007787595
- Committee on Fetus and Newborn Committee on Drugs, Section on Anesthesiology, Section on Surgery and Canadian Paediatric Society, Fetus and Newborn CommitteePrevention and management of pain and stress in the neonatePediatrics200010545446110654977
- BacharyaAAnnamaliSTaubNAFieldDOral sucrose analgesia for preterm infant venepunctureArch Dis Child Fetal Neonatal Ed200489F17F1814711847
- GradinMSchollinJThe role of endogenous opioids in mediating pain reduction by orally administered glucose among newbornsPediatrics20051151004100715805377
- HarrisonDJohnstonLLoughnanPOral sucrose for procedural pain in sick hospitalized infants: a randomized-controlled trialJ Paediatr Child Health20033959159714629524
- HarrisonDLoughnanPManiasEGordonIJohnstonLRepeated doses of sucrose in infants continue to reduce procedural pain during prolonged hospitalizationsNurs Res20095842743419918153
- DebillonTGras-LeguenCBosherCFleuryMALes grilles d’évaluation de la douleur chez le nouveau né: revue de la littératureDouleur et Analgésie19984167172
- GrunauRVECraigKDWhitielMFLintionJHadjistavropoulosHDPain in the preterm neonate: behavioural and physiological indicesPain1993522872998460047
- JohnstonCStevensBCraigKDGrunauRVEDevelopmental changes in pain expression in premature, fullterm, two and four month-old infantsPain1993522012088455968
- TaddioAKatzJIlrsichAKorenGEffect of neonatal circumcision on pain response during subsequent routine vaccinationLancet19973495996039057731
- JohnstonCCStevensBJExperience in neonatal intensive care unit affects pain responsePediatrics1996989259308909487
- GrunauRVECraigKDPain expressions in neonates: facial actions and cryPain1987283954103574966
- BlassEMilk induced hypoalgesia in human newbornsPediatrics1997998258299164777
- GrayLMillerLPhilippBBlassEBreastfeeding is analgesic in healthy newbornsPediatrics200210959059311927701
- CarbajalRVeerapenSCoudercSJugieMAnalgesic effect of breast feeding in term neonates: randomised controlled trialBMJ200313326
- ShahPSAliwalasLIShahVBreastfeeding or breast milk for procedural pain in neonatesCochrane Database Syst Rev20063CD00495016856069
- EfeEOzerZCThe use of breastfeeding for pain relief during neonatal immunization injectionsAppl Nurs Res200720101617259038
- EfeESavaserSThe effect of two different methods used during peripheral venous blood collection on pain reduction in neonatesAgrı Dergisi2007194956