Abstract
Continuous peripheral nerve block is a relevant part of multimodal treatment of postoperative pain. In this context the continuous popliteal nerve block is described as an option for postoperative pain management for surgical procedures on the leg, and particularly on the ankle and foot. We applied continuous popliteal nerve block for different types of anesthesia and postoperative pain management via the same catheter. No clear evidence of this specific use has been described in the literature. A 38 year-old patient wounded in combat with a displaced fracture of left tibia and extensive loss of substance needed orthopedic surgeries as well as several reconstructive procedures. A continuous popliteal nerve block was applied via ultrasound-guided catheter for anesthesia at different times, and postoperative pain control for all surgical procedures. The continuous popliteal nerve block and its long-term positioning, of non-common evidence in literature, was utilized to treat a poly-traumatized patient, thereby avoiding repeated general anesthesia and opioid use and their adverse effects. This technique, within a complicated combat field environment, was demonstrated to be clinically effective with high patient satisfaction.
Introduction
Peripheral nerve blocks and regional anesthesia are an integral and relevant part of multimodal treatment of postoperative pain, encouraging postoperative recovery, patients’ discharge, and reduction of opioid use.Citation1 The continuous popliteal nerve block is undoubtedly an option in the treatment of postoperative pain in elective surgery as well as in traumatology surgery of the foot and ankle.Citation2 Cases of use have also been reported for postoperative pain management in surgical procedures for the treatment of burns.Citation3 This study reports the application of an ultrasound-guided continuous popliteal nerve block both for anesthesia and for the treatment of postoperative pain in a poly-traumatized patient. Specifically, the patient had exposed and displaced fractures of the tibia and fibula with extensive loss of skin substance, due to firearm injuries, and was treated in a combat field environment in Libia, characterized by typical limitations such as: little infrastructure, personnel and equipment constraints, possible numerous casualties access and difficult re-supply.Citation4 This specific technique was effective and particularly suitable, and we could not find other similar descriptions in the literature.
Case presentation
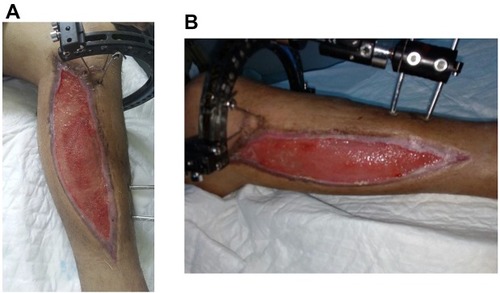
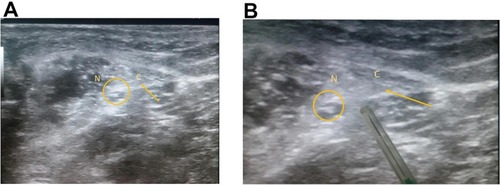
A 38 year-old, 65 kg man with no known disease history, was admitted to the field health facility in Libia with a right-sided compound fracture, bilateral costal fractures, and a displaced fracture of the left tibia with extensive loss of substance due to firearm shots. The patient firstly needed treatment for left tibia bone osteosynthesis through an external fixator and numerous medications and treatments of a reconstructive nature for the wound, as well as conservative treatment for the other lesions. Therefore, on the second day of hospitalization, and after written informed consent was obtained, an E-Catheter (Pajunk), 20 G, was placed via ultrasound-guided high frequency linear probe (6–12 MHz), in-plane position at the level of the left popliteal nerve, surrounding it (). Administration of 10 mL of 2% mepivacaine and 10 mL of 0.75% ropivacaine through the catheter allowed, within 10 minutes, a sensory block level suitable for the osteosynthesis procedure with external fixator. During the surgical procedure, the patient underwent sedation with fentanyl e.v. 100 µg and midazolam e.v. 2 mg, maintaining spontaneous respiration with 50% FiO2 oxygen. At the end of the intervention, which lasted 82 minutes, 0.2% ropivacaine administration was started at 7 mL/hour for the initial postoperative 24 hours. The patient did not indicate a pain score on visual analog scale (VAS) greater than 2 during surgery, and 3 in the initial postoperative 24 hours, measured every 4 hours. Every 4 days, the patient received multiple deep wound dressing changes with specific substances (ligasan, aquagel), associated with demarcation of wound margins and escharotomies, and sometimes with concomitant partial closure of the flaps (). The same anesthetic and analgesic protocol used for osteosynthesis was used for each dressing change. Intraoperative VAS was greater than 4 on only two occasions, a supplementary bolus of 100 µg of fentanyl was therefore provided; for the remainder and still within the initial postoperative 24 hours, the score was less than 3. On the 32nd day after the first bone osteosynthesis, a partial repositioning of the external fixator was necessary, and immediately thereafter the reconstructive procedure was performed, and the anesthetic protocol did not change. During admission, the patient received low molecular weight heparin therapy (4,000 IU/once a day) for several days. On day 68 after admission, the continuous nerve block catheter which had been inserted on day two, was removed, with almost complete healing of the surgical wound and proper alignment of the tibia’s bone abutments. After each procedure the patient reported a high degree of overall satisfaction (values of 8 and 9 on a scale from 0–10) and pain control in particular. No adverse events or changes in the catheter application site were identified.
Discussion and conclusions
The majority of studies on the use of continuous peripheral nerve block focus their attention only on postoperative analgesia in comparison with the single block, or in any case, for anesthesia in the case of a type of procedure.Citation5,Citation6 This statement is also valid for the continuous popliteal nerve block which, in particular, has only been used in reconstructive treatment of skin lesions in some selected and rare cases.Citation7 The early use of continuous peripheral nerve blocks in traumatized patients has also not yet been investigated in emergency departments, while it has been found in the treatment of traumatic injuries typical of combat.Citation8 Furthermore, within the context of multimodal pain treatment in traumatized patients, it is widely recognized that avoiding the use of opioids is an important result to be pursued in patients with potential comorbidities, as this is connected to the potential clinical consequences of excessive use of opioids.Citation6 In this case, the catheter at the popliteal level allowed administration of anesthesia during two tibia bone osteosynthesis procedures, and during several reconstructive surgery procedures. In addition, the procedure allowed control of postoperative pain through the continuous infusion of 0.2% ropivacaine. The patient, particularly considering the concomitant rib fractures, avoided a significant number of deep sedations with a significant reduction of opioid consumption. As a result, the treatment was not potentially exacerbated of any complication due to the use of unnecessary drugs, thus considerably facilitating the clinical course. The absence of catheter-related infections or other adverse effects despite the long-term placement (68 days), although very uncommon in literature, is in line with medical literature,Citation9 as well as the lack of bleeding related to the administration of low molecular weight heparin.Citation10 The absence of infections due to the catheter, is probably due to the correct management of the medication and the antibiotic therapy provided, at intervals, during the surgical procedures. It is noteworthy, however, that in contrast to what has been reported in medical literature, in our case, such administration of heparin lasted several days. The general satisfaction of the patient was always high, showing the effectiveness of the continuous popliteal nerve block administered, confirmed by the low intraoperative and postoperative VAS levels reported. The technique has allowed, within a combat field environment, via a relatively easy method of execution with only the need for a portable ultrasound system and a continuous plexus kit described previously, a clinically satisfactory analgesic and antalgic treatment in a poly-traumatized patient with significant bone and skin lesions due to firearm shots. This technique can be used for adequate management of the surgical treatment of traumatic injuries both in the acute phase, and in the subsequent phases.
This study provides evidence of the feasibility of this approach in austere environments to achieve a reduction in opioid administration and avoiding their prolonged use, which is one of the most common postsurgical complications.Citation11
Informed consent
Written informed consent was obtained from the patient for publication of this case report and associated images.
Acknowledgment
The authors received no financial support for this research.
Disclosure
The authors report no conflicts of interest in this work.
References
- Brian M, Ilfeld MS. Continuous peripheral nerve blocks: an update of the published evidence and comparison with novel, alternative analgesic modalities. Anesth Analg. 2017;124:308. doi:10.1213/ANE.000000000000158127749354
- Ding YD, Manolk A III, Galos DK, Jain S, Tejwani NC. Continuous popliteal sciatic nerve block versus single injection nerve block for ankle fracture surgery: a prospective randomization comparative trial. J Orthopedic Trauma. 2015;29:393–398. doi:10.1097/BOT.0000000000000374
- Shanck ES, Martyn JA, Donelan MB, Perrone A, Firth PG, Driscoll DN. Ultrasound-guided regional anesthesia for pediatric burn reconstructive surgery; A prospective study. J Burn Care Res. 2016;37:213–217. doi:10.1097/BCR.0000000000000174
- Buckenmaier CC III, Evan HL, Shields CH, Sampson JB, Chiles JH. Regional anesthesia in austere environments. Reg Anesth Pain Med. 2003;28(4):321–327.12945026
- Gadsden J, Warlick A. Regional anesthesia for the trauma patient: improving patient outcomes. Local Reg Anesth. 2015;8:45. doi:10.2147/LRA26316813
- Joshi G, Gandhi K, Shah N, Gadsen J, Selby L. Peripheral nerve blocks in the management of postoperative pain: challenges and opportunities. J Clin Anesth. 2016;35:524–529. doi:10.1016/j.jclinane.2016.08.04127871587
- Shick V, Lebovitz EE, Conrad E. The benefits of ultrasound-guided continuous sensory nerve setting of burn injury: a case report of bilateral continuous superficial peroneal nerve block in a patient with severe sleep apnea. J Clin Anesth. 2017;36:62–66. doi:10.1016/j.jclinane.2016.10.00228183576
- Vallerana AH, Cosler P, Henningfield JE, Galassini P. Pain management strategies and lessons from the military: a narrative review. Pain Res Manag. 2015;20:261–268. doi:10.1155/2015/19602526448972
- Borgeat A, Blumenthal S, Lambert M, Teodorou P, Vienna P. The feasibility and complications of the continuous popliteal nerve block: a 1001 - case survey. Anesth Analg. 2006;103:229–233. doi:10.1213/01.ane.0000221462.87951.8d16790658
- Buckenmaier CC III, Shields CH, Auto AA, et al. Continuous peripheral nerve block in combat casualties receiving low - molecular Leigh heparin. Br J Anesthesia. 2006;97:874–877. doi:10.1093/bja/ael269
- Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6):1–9. doi:10.1001/jamasurg.2017.0504