Abstract
Background
Vortioxetine is an investigational multimodal antidepressant. We conducted this meta-analysis to assess the efficacy and safety of 10 mg vortioxetine in the treatment of major depressive disorder (MDD).
Methods
Randomized controlled trials (RCTs) published in PubMed, Web of Science, Embase, and ClinicalTrials.gov were systematically reviewed to assess the treatment effects and safety profiles of patients with MDD who were treated with 10 mg vortioxetine. The outcome measures included response rate, remission rate, changes from baseline in Montgomery–Asberg Depression Rating Scale (MADRS), Hamilton Rating Scale for Depression (24-items) (HAM-D24), Clinical Global Impression-Severity (CGI-S), and Clinical Global Impression-Improvement (CGI-I) scores. Results were expressed with risk ratio or weighted mean difference with 95% confidence intervals. Pooled results were calculated using a fixed-effects model or a random-effects model according to the heterogeneity among included trials.
Results
Six RCTs with a total of 1,801 patients met the inclusion criteria and were included in this meta-analysis. The 10 mg vortioxetine dose significantly increased the response rate and remission rate in the treatment of MDD compared with placebo. Moreover, there was a statistically significant reduction from baseline in the MADRS, HAM-D24, CGI-S, and CGI-I scores with 10 mg vortioxetine vs placebo. The incidence of treatment-emergent adverse events such as nausea, vomiting, constipation, and hyperhidrosis was higher in the 10 mg vortioxetine group than in the placebo group.
Conclusion
Vortioxetine 10 mg can significantly increase the response rate and remission rate, and reduce the MADRS, HAM-D24, CGI-S, and CGI-I scores in patients with MDD with an acceptable risk of treatment-emergent adverse events. Further well-conducted, large-scale trials are needed to validate these findings.
Introduction
Major depressive disorder (MDD) is a common mental disorder that is associated with deficits in cognitive function.Citation1 It ranks fourth as the leading cause of overall disease burden worldwide and is the predominant reason of lost disability-adjusted life-years among developed countries.Citation2 MDD can lead to a reduction in the quality of life and overall health, and enhanced economic costs. Moreover, it is also associated with a higher risk of suicide.Citation3,Citation4
There are many antidepressants available for the treatment of MDD; however, only ~50% of patients respond to these drugs and ~30% achieve remission.Citation5–Citation7 Moreover, antidepressant treatment could result in several adverse events, such as weight changes, sexual dysfunction, and insomnia, which can influence patients’ compliance with therapy.Citation8–Citation10
Vortioxetine is a novel antidepressant that has been approved for the treatment of MDD.Citation11,Citation12 In October 2013, the US Food and Drug Administration (FDA) approved vortioxetine for the treatment of MDD.Citation13 The mechanism of action of vortioxetine lies in its multimodal activity. It combines two pharmacologic modes of action: direct modulation of serotonin (5-HT) receptor activity and inhibition of the 5-HT transporter. In vitro studies demonstrate that vortioxetine is a 5-HT3, 5-HT7, and 5-HT1D receptor antagonist; a 5-HT1B receptor partial agonist; a 5-HT1A receptor agonist; and an inhibitor of the 5-HT transporter.Citation14,Citation15 The precise contribution of the individual targets to the observed pharmacodynamic profile remains unclear. However, preclinical trials indicate that the targets interact in a complex fashion, which result in modulation of neurotransmission in several systems, including serotonin, norepinephrine, dopamine, histamine, and acetylcholine systems, within the rat forebrain.Citation14,Citation15
The current recommend dosage of vortioxetine for the treatment of MDD is 5–20 mg/day,Citation15 and 10 mg/day is recommended as the starting dose. However, a dose of 5 mg/day vortioxetine is recommended for patients who do not tolerate this high dose of 10 mg. Several multicenter, large-scale trials have evaluated the treatment effects of 10 mg vortioxetine in the treatment of MDD; however, these trials have shown inconsistent results. Thus, we conducted a meta-analysis of randomized controlled trials (RCTs) to assess the efficacy and safety of 10 mg vortioxetine in the treatment of patients with MDD.
Materials and methods
Search strategy
A comprehensive search was conducted to identify relevant studies published in PubMed, Embase, and Web of Science databases before October 22, 2015. The search terms were (“depressive disorder, major”[MeSH Terms] OR (“depressive”[All Fields] AND “disorder”[All Fields] AND “major”[All Fields]) OR “major depressive disorder”[All Fields] OR (“major”[All Fields] AND “depressive”[All Fields] AND “disorder”[All Fields]) OR “major depressive disorder”[All Fields] OR “depressive disorder”[MeSH Terms] OR (“depressive”[All Fields] AND “disorder”[All Fields]) OR “depressive disorder”[All Fields] OR (“major”[All Fields] AND “depressive”[All Fields] AND “disorder”[All Fields])) AND (“vortioxetine”[Supplementary Concept] OR “vortioxetine”[All Fields]). The search was limited to human subjects and clinical trials. No language restriction was imposed. Furthermore, we also identified relevant studies through a review of ClinicalTrials.gov in case of missing unpublished studies. The reference lists of included studies and recent reviews were also manually searched until no additional potential studies could be found.
Study inclusion criteria
All clinical trials that assessed the efficacy and safety of vortioxetine/Lu AA21004 in the treatment of MDD were considered eligible for the analysis. The following study inclusion criteria were applied: 1) population: patients were diagnosed with MDD according to the Diagnostic and Statistical Manual of Mental Disorders 4th ed, 2) intervention: vortioxetine/Lu AA21004 10 mg/day, 3) comparison: placebo alone, 4) outcomes: response rate; remission rate; absolute changes in the Montgomery–Asberg Depression Rating Scale (MADRS), Hamilton Rating Scale for Depression (24-items) (HAM-D24), Clinical Global Impression-Severity (CGI-S), and Clinical Global Impression-Improvement (CGI-I) scores; and the incidence of treatment-emergent adverse events, and 5) study design: RCT. MADRS response rate was defined as ≥50% decrease in MADRS total score from baseline, and MADRS remission rate was defined as a MADRS total score ≤10.
Data extraction and quality assessment
Data extraction and quality assessment were conducted by two independent investigators (Guangjian Li and Dihui Ma) using a standardized data extraction form. The information extracted included: first author, year of publication, regimen, study design, number of patients in the study and control group, medical dose, duration of therapy, baseline depression rating scores and posttreatment mean change scores from baseline, incidence of treatment-related adverse events in the study and control group, response rate, and remission rate. For the trials that compared different doses of vortioxetine to placebo, we only included the data comparing the 10 mg/day dose to the placebo dose.
We used the Jadad scale to assess the methodological quality of the included studies. The Jadad scale consists of three items describing randomization (0–2 points), masking (0–2 points), and dropouts and withdrawals (0–1 points) in the report of an RCT.Citation16 The quality scale ranges from 0 to 5 points, and a higher score indicates higher quality. Any study with a score ≥3 is considered to be of high quality.Citation17
Statistical analysis
This meta-analysis was conducted using STATA version 12.0 (StataCorp LP, College Station, TX, USA). Dichotomous variables, such as response rate, remission rate, and incidence of adverse events, were expressed as risk ratio (RR) with 95% confidence intervals (95% CIs). Continuous variables, including the change in MADRS and HAM-D24 scores from baseline, were expressed as weighted mean differences (WMDs) with 95% CIs. Before the data were pooled, we first tested the heterogeneity among the studies using the Cochrane Q chi-square test and I2 statistics, in which P-value <0.10 or I2>50% were considered as heterogeneity.Citation18 A random-effects model (DerSimonian–Laird method)Citation19 or a fixed-effects model (Mantel–Haenszel method)Citation20 was used to pool the estimates according to the presence or absence of heterogeneity. Whenever heterogeneity was found, subgroup analysis and sensitivity analysis were performed to explore the potential sources. Because the number of included studies in each analysis was less than ten, publication bias was not assessed. A P-value of less than 0.05 was considered statistically significant.
Results
Search results
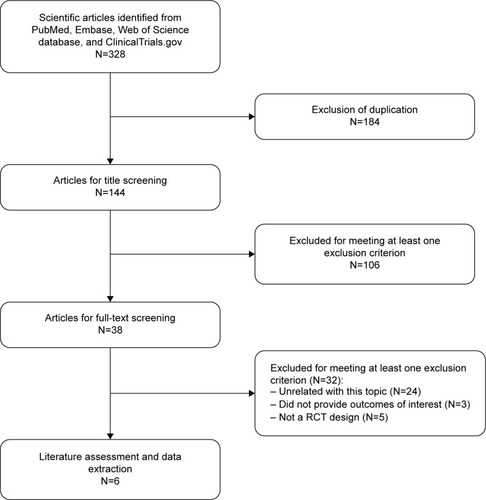
The initial search yielded 328 relevant records, of which 322 were excluded because of duplicate records and various reasons (case reports, reviews, letters, non-RCTs, or unrelated with our topics). Eventually, six RCTs with a total of 1,801 patients met the inclusion criteria and were included in this meta-analysis ().Citation21–Citation26 We obtained the full texts of the six papers through various means.
Study characteristics
The main characteristics of the six RCTs included in this meta-analysis are presented in . These studies were published between 2012 and 2015. The sample size of these trials ranged from 205 to 391. Of the studies included, two were conducted in US, three outside US, and one in US and non-US sites. All the trials were placebo-controlled, and two trials also included active comparator arm (one trial included duloxetine and the other one included venlafaxine). These trials also studied the effect of other doses of vortioxetine, including 2.5, 5, 15, and 20 mg. In accordance with the purpose of this meta-analysis, we only compared the effects and safety between 10 mg vortioxetine and placebo. All the trials evaluated the effect of vortioxetine at 8 weeks except one,Citation25 in which the effect assessment was conducted at 6 weeks. All the included studies had a Jadad score greater than 3 (range from 4 to 5).
Table 1 Baseline characteristics of patients in the trials included in the meta-analysis
Effect of 10 mg vortioxetine on response rate and remission rate
All six RCTs reported the data on response rate.Citation21–Citation26 The aggregated results of these studies suggest that patients treated with 10 mg vortioxetine had a higher response rate than those treated with placebo (RR =1.50; 95% CI: 1.32, 1.70; P<0.001) (). The test for heterogeneity was not significant (I2=46.9%, P=0.093).
Figure 2 Forest plot showing the effect of 10 mg vortioxetine on the response rate and remission rate.
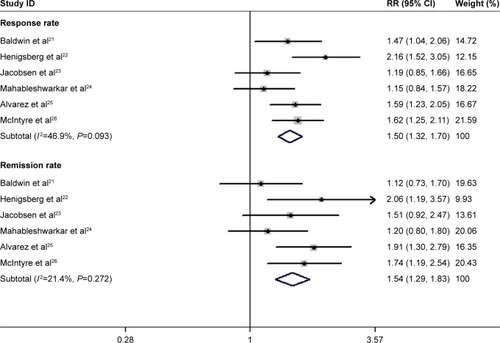
All trials reported the data on remission rate.Citation21–Citation26 The aggregated results of these studies suggest that vortioxetine 10 mg was associated with a higher remission rate than placebo (RR =1.54; 95% CI: 1.29, 1.83; P<0.001) (). The test for heterogeneity was not significant (I2=21.4%, P=0.272).
Effect of 10 mg vortioxetine on MADRS score
All six RCTs reported changes from baseline in the MADRS score.Citation21–Citation26 The aggregated results of these studies suggest that vortioxetine 10 mg significantly reduced the MADRS score (WMD =−3.27; 95% CI: −4.88, −1.66; P<0.001) (). The test for heterogeneity was significant (I2=99.8%, P<0.001). Subsequently, we performed a sensitivity analysis to explore the potential sources of heterogeneity. Exclusion of the trial that assessed the effect of vortioxetine at 6 weeksCitation25 resulted in similar combined estimates (WMD =−2.79; 95% CI: −4.51, −1.06; P=0.002), yet the heterogeneity did not disappear (I2=99.8%, P<0.001). Exclusion of the trial conducted by Mahableshwarkar et alCitation24 did not change the pooled estimates substantially (WMD =−3.77; 95% CI: −5.24, −2.29; P<0.001), and the heterogeneity was still present (I2=99.7%, P<0.001). Further exclusion of any single study did not resolve the heterogeneity and the overall combined WMD, which ranged from −3.62 (95% CI: −5.43, −1.82) to −2.79 (95% CI: −4.51, −1.06).
Figure 3 Forest plot showing the effect of 10 mg vortioxetine on the MADRS score.
Abbreviations: WMD, weighted mean difference; CI, confidence interval; MADRS, Montgomery–Asberg Depression Rating Scale.
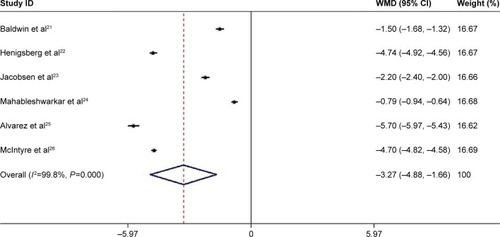
We also conducted a subgroup analysis based on region. The pooled results showed that vortioxetine 10 mg significantly reduced the MADRS score in both the US (WMD =−1.49; 95% CI: −2.88, −0.11; P=0.034) and non-US (WMD =−3.98; 95% CI: −6.49, −1.47; P=0.002) regions; patients outside the US seemed to have a greater decrease in the MADRS score than those in the US (3.98 vs 1.49).
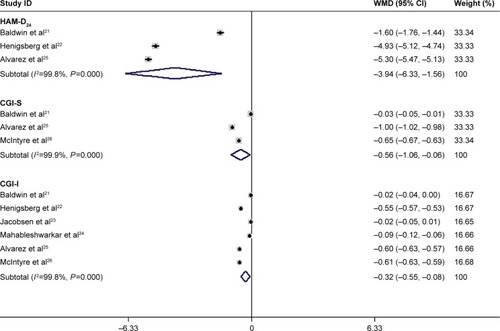
Effect of 10 mg vortioxetine on HAM-D24, CGI-S, and CGI-Iscores
Three RCTs reported changes from baseline in HAM-D24 and CGI-S scores,Citation21,Citation25,Citation26 and six RCTs reported changes from baseline in CGI-I score.Citation21–Citation26 The aggregated results of these studies suggest that vortioxetine 10 mg was associated with a greater reduction in HAM-D24 score (WMD =−3.94; 95% CI: −6.33, −1.56; P=0.001), little decrease in CGI-S score (WMD =−0.56; 95% CI: −1.06, −0.06; P=0.028), and slight reduction in CGI-I score (WMD =−0.32, 95% CI: −0.55, −0.08; P=0.010) (). The test for heterogeneity was significant for all these combined estimates. Thus, we conducted a sensitivity analysis to explore the potential sources of heterogeneity. The sensitivity analysis showed that the pooled estimates were not significantly influenced when we excluded any single trial, but the heterogeneity was still present (data not shown).
Figure 4 Forest plot showing the effect of 10 mg vortioxetine on the HAM-D24, CGI-S, and CGI-I scores.
Abbreviations: WMD, weighted mean difference; CI, confidence interval; HAM-D24, Hamilton Rating Scale for Depression (24-items); CGI-S, Clinical Global Impression-Severity; CGI-I, Clinical Global Impression-Improvement.
Adverse events
All the trials reported data on adverse events.Citation21–Citation26 The aggregated results of these studies suggest that the incidence of treatment-emergent adverse events was slightly higher in the 10 mg vortioxetine group than that in the placebo group (RR =1.11; 95% CI: 1.03, 1.20; P=0.005). The most common adverse events were nausea, headache, dizziness, diarrhea, and dry mouth. Pooled results showed that, compared to placebo, 10 mg vortioxetine was associated with a higher incidence of nausea (RR =3.44; 95% CI: 2.63, 4.48; P<0.001), vomiting (RR =2.78; 95% CI: 1.32, 5.85; P=0.007), constipation (RR =2.03; 95% CI: 1.15, 3.58; P=0.015), and hyperhidrosis (RR =4.44; 95% CI: 1.29, 15.26; P=0.018). For seven other adverse events, there were no significant differences between the vortioxetine and placebo groups. The adverse events related to vortioxetine treatment are summarized in .
Table 2 Summary of RR of adverse events in patients with major depressive disorder
Discussion
The present study was a meta-analysis with the objective of assessing the efficacy and safety of 10 mg vortioxetine in the treatment of patients with MDD. Our study demonstrated that, compared to placebo, the treatment with 10 mg vortioxetine was associated with a higher response rate and remission rate in patients with MDD. Furthermore, vortioxetine 10 mg also produced significant effects on the changes from baseline in the MADRS, HAM-D24, CGI-I, and CGI-S scores. A higher incidence of treatment-emergent adverse events was observed in the 10 mg vortioxetine group than that in the placebo group. These findings indicated that 10 mg vortioxetine seemed to be more effective and well tolerated than placebo in the treatment of patients with MDD.
In this meta-analysis, we found that 10 mg vortioxetine significantly improved the response rate and remission rate in the treatment of patients with MDD. These positive results were observed in all the included studies, in which the response rate and remission rate ranged from 33.8% to 68% and 21.4% to 49%, respectively. The highest response rate and remission rate were observed in the study conducted by Alvarez et al,Citation25 in which 205 patients from 49 psychiatric settings in eleven countries were enrolled, and 92% of them were Caucasian. At week 6, 68% (68 out of 100) of patients in the vortioxetine 10 mg group and 42.9% (45 out of 105) of patients in the placebo group achieved a MADRS response (≥50% decrease in MADRS total score)Citation25 and the corresponding value of remission rate was 49% (49 out of 100) and 25.7% (27 out of 105), respectively. Another RCT assessing the efficacy and safety of 10 mg vortioxetine, however, demonstrated a relatively lower rate of response and remission, in which 312 participants at 37 sites in the US were enrolled, and 72.4% of them were white.Citation23 The MADRS response at 8 weeks was achieved in 33.8% and 28.4% of patients in the vortioxetine 10 mg and placebo groups, respectively. The MADRS remission rate for the two groups was 21.4% and 14.2%, respectively.Citation23 Despite that both the two trials observed a significant difference in response rate and remission rate between the vortioxetine 10 mg and placebo groups, the magnitude of response rate in the former trial (68%) was almost two times greater than that in the latter trial (33.8%). One possible explanation for this was the difference in race, since the proportion of white patients in the former trial (92%) was larger than that in the latter one (72.4%).
Regarding the changes from baseline in the MADRS score, our study indicated that there was a significant reduction in the MADRS score for the vortioxetine 10 mg group compared with placebo. However, high heterogeneity was found among the trials reporting data on MADRS score. Despite sensitivity analysis was performed to explore the potential sources of heterogeneity, no significant factors that may introduce the heterogeneity were found. According to the published studies, several factors may contribute to the huge heterogeneity among the included studies.Citation27,Citation28 The inclusion criteria were an important factor for the heterogeneity among the studies. Of these included studies, the inclusion criteria for the MADRS total score varied among them. Four of the six trials included patients with a MADRS total score ≥26, and the remaining two enrolled patients with a score ≥30. The differences in the inclusion criteria of MADRS total score may result in heterogeneous patients, and thus may influence the subsequent outcomes of changes in the MADRS score. Furthermore, some other factors among the included studies were different, including age, region, and race. Among the six trials, three were conducted outside US (including Europe, Asia, and Africa), two in US, and one in US and non-US sites. Different regions have different races and social environments, which would result in heterogeneity.
In terms of safety, the incidence of treatment-emergent adverse events was higher in the 10 mg vortioxetine group than that in the placebo group. The most common adverse events of vortioxetine included nausea, dizziness, headache, dry mouth, and diarrhea. The pooled results showed that vortioxetine induced a higher incidence of nausea when compared with placebo, but the incidences of other common adverse events between the two groups were not significantly different. Some other adverse events of vortioxetine were reported in these studies, including vomiting, constipation, hyperhidrosis, fatigue, insomnia, and nasopharyngitis. Of them, the incidences of vomiting, constipation, and hyperhidrosis were higher in the vortioxetine group than those in the placebo group. Sexual dysfunction was reported in the regimens of 5-HT reuptake inhibitors for depression treatment.Citation27,Citation28 It not only adversely impacts the quality of life of antidepressant users, but also reduces the patients’ compliance with treatment.Citation28 In this meta-analysis, only two trials reported the available data on sexual dysfunction; thus, we could not investigate whether vortioxetine has adverse effects on sexual dysfunction in the treatment of patients with MDD. Future research could focus on this issue.
In this meta-analysis, we assessed the efficacy and safety of 10 mg vortioxetine in the treatment of MDD, and most of the findings were consistent with a recent published meta-analysis that evaluated the effects of 5 mg vortioxetine.Citation29 In that study, the authors included five RCTs, and found that the treatment response of 5 mg/day vortioxetine was greater than that of placebo group and the incidence of nausea was higher in the 5 mg/day vortioxetine group than that in the control group.Citation29 However, 5 mg/day vortioxetine did not have a significant antidepressant effect on remission rate for patients with MDD. Notably, huge heterogeneity among the five RCTs was also observed when performing the meta-analysis. Thus, the authors conducted a sensitivity analysis; however, only the pooled remission rate was significantly influenced when one trial was excluded.
There are some potential limitations in this meta-analysis that should be taken into account when interpreting our results. First, our study was conducted on only six RCTs, and most of them had relatively small sample size. Although the six RCTs were well conducted and of high quality (Jadad score >3), caution should be exercised when applying the pooled results into clinical practice since small trials are more likely to overestimate the treatment effect as compared to larger trials. Second, there was considerable heterogeneity among the included studies. The inclusion criteria of each trial and the population characteristics varied greatly. These factors may lead to heterogeneity and have a potential impact on our results. Third, due to limited data, we did not evaluate the effects and safety of vortioxetine on subgroup population, such as the older patients and white vs non-white patients. Fourth, it should be noted that all the trials were funded by a pharmaceutical company (Takeda), and their results may have been influenced by the inherent conflict of interest and possible bias.
Conclusion
The present meta-analysis indicated that 10 mg vortioxetine significantly increased the response rate and remission rate, and also decreased the MADRS, HAM-D24, CGI-S, and CGI-I scores. Moreover, 10 mg vortioxetine produced an acceptable and tolerable risk of nausea. Therefore, vortioxetine 10 mg is more effective than placebo for the treatment of MDD. However, considering that this study was conducted on a small number of RCTs, further large-scale, well-performed trials are needed to verify our findings.
Disclosure
The authors report no conflicts of interest in this work.
References
- McIntyreRSChaDSSoczynskaJKCognitive deficits and functional outcomes in major depressive disorder: determinants, substrates, and treatment interventionsDepress Anxiety20133051552723468126
- UstunTBAyuso-MateosJLChatterjiSGlobal burden of depressive disorders in the year 2000Br J Psychiatry200418438639215123501
- KesslerRCBorgesGWaltersEEPrevalence of and risk factors for lifetime suicide attempts in the National Comorbidity SurveyArch Gen Psychiatry19995661762610401507
- AngstJAngstFStassenHHSuicide risk in patients with major depressive disorderJ Clin Psychiatry199960Suppl 25762 discussion 75–56, 113–11610073389
- TrivediMHMajor depressive disorder: remission of associated symptomsJ Clin Psychiatry200667Suppl 6273216848674
- TrivediMHRushAJWisniewskiSREvaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practiceAm J Psychiatry2006163284016390886
- RushAJTrivediMHWisniewskiSRAcute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D reportAm J Psychiatry20061631905191717074942
- GinsbergLDImpact of drug tolerability on the selection of antidepressant treatment in patients with major depressive disorderCNS Spectr20091481420397586
- AshtonAKJamersonBDWeinsteinWLAntidepressant-related adverse effects impacting treatment compliance: results of a patient surveyCurr Ther Res Clin Exp2005669610624672116
- MorehouseRMacqueenGKennedySHBarriers to achieving treatment goals: a focus on sleep disturbance and sexual dysfunctionJ Affect Disord2011132Suppl 1S14S2021575992
- Garnock-JonesKPVortioxetine: a review of its use in major depressive disorderCNS Drugs20142885587425145538
- SanchezCAsinKEArtigasFVortioxetine, a novel antidepressant with multimodal activity: review of preclinical and clinical dataPharmacol Ther2015145435725016186
- FDA Brintellix (vortioxetine): highlights of prescribing information. Brintellix label Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/204447s000lbl.pdfAccessed November 15, 2015
- Bang-AndersenBRuhlandTJorgensenMDiscovery of 1-[2-(2,4-dimethylphenylsulfanyl)phenyl]piperazine (Lu AA21004): a novel multimodal compound for the treatment of major depressive disorderJ Med Chem2011543206322121486038
- MorkAPehrsonABrennumLTPharmacological effects of Lu AA21004: a novel multimodal compound for the treatment of major depressive disorderJ Pharmacol Exp Ther201234066667522171087
- JadadARMooreRACarrollDAssessing the quality of reports of randomized clinical trials: is blinding necessary?Control Clin Trials1996171128721797
- MoherDPhamBJonesADoes quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses?Lancet19983526096139746022
- HigginsJPThompsonSGDeeksJJMeasuring inconsistency in meta-analysesBMJ200332755756012958120
- DerSimonianRLairdNMeta-analysis in clinical trialsControl Clin Trials198671771883802833
- MantelNHaenszelWStatistical aspects of the analysis of data from retrospective studies of diseaseJ Natl Cancer Inst19592271974813655060
- BaldwinDSLoftHDragheimMA randomised, double-blind, placebo controlled, duloxetine-referenced, fixed-dose study of three dosages of Lu AA21004 in acute treatment of major depressive disorder (MDD)Eur Neuropsychopharmacol20122248249122209361
- HenigsbergNMahableshwarkarARJacobsenPA randomized, double-blind, placebo-controlled 8-week trial of the efficacy and tolerability of multiple doses of Lu AA21004 in adults with major depressive disorderJ Clin Psychiatry20127395395922901346
- JacobsenPLMahableshwarkarARSerenkoMA randomized, double-blind, placebo-controlled study of the efficacy and safety of vortioxetine 10 mg and 20 mg in adults with major depressive disorderJ Clin Psychiatry20157657558226035185
- MahableshwarkarARJacobsenPLSerenkoMA randomized, double-blind, placebo-controlled study of the efficacy and safety of 2 doses of vortioxetine in adults with major depressive disorderJ Clin Psychiatry20157658359126035186
- AlvarezEPerezVDragheimMA double-blind, randomized, placebo-controlled, active reference study of Lu AA21004 in patients with major depressive disorderInt J Neuropsychopharmacol20121558960021767441
- McIntyreRSLophavenSOlsenCKA randomized, double-blind, placebo-controlled study of vortioxetine on cognitive function in depressed adultsInt J Neuropsychopharmacol2014171557156724787143
- HermanJBBrotmanAWPollackMHFluoxetine-induced sexual dysfunctionClin Psychiatry1990512527
- HattaSDuniANgCGEffects of selective serotonin reuptake inhibitors (SSRIs) therapy on the female sexual response cycle of women with major depressionClin Ter2013164111523455735
- FuJChenYThe efficacy and safety of 5 mg/d vortioxetine compared to placebo for major depressive disorder: a meta-analysisPsychopharmacology201523271624871704