Abstract
Although antidepressants may increase the risk of switching to mania in bipolar disorder (BD), clinicians have been using antidepressants to treat patients with bipolar depression. Appropriate treatments for bipolar depression remain controversial. In BD, antidepressants comprise a double-edged sword in terms of their efficacy in treating depression and the increased risk of switching. This review presents an important table outlining the benefit in terms of depression improvement and the risk of switching in the clinical setting. It also proposes strategies based on the characteristics of antidepressants such as their pharmacology, specifically the equilibrium dissociation constant (KD) of the noradrenaline transporter. This table will be useful for clinicians while considering benefit and risk. Antidepressants augmenting noradrenaline may be effective in bipolar depression. However, it is easily presumed that such antidepressants may also have a risk of switching to mania. Therefore, antidepressants augmenting noradrenaline will be the recommended treatment in combination with an antimanic agent, or they may be used for short-term treatment and early discontinuation. The corresponding medical treatment guidelines probably need to be reevaluated and updated based on biological backgrounds. From previous studies, we understand that the stability of noradrenaline levels is important for BD amelioration, based on the pathophysiology of the disorder. It is hoped that researchers will reevaluate BD by conducting studies involving noradrenaline.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Bipolar disorder
Bipolar disorder (BD) is an episodic illness characterized by recurrent manic, mixed, and depressive episodes, with an estimated global lifetime prevalence of 1%–5%.Citation1 BD is defined in the diagnostic criteria of the International Classification of Diseases (ICD, World Health Organization, 2010)Citation2 and the Diagnostic and Statistical Manual of Mental Disorders (DSM, American Psychiatric Association, 2013)Citation3 as being different from major depressive disorder, schizophrenia, and other psychiatric disorders. The illness is associated with high levels of mortality and morbidity,Citation4 functional impairment,Citation5 and high rates of suicide.Citation6 Despite the fact that the switching is a core aspect of the clinical presentation of BD, the biological background of the pathology is still poorly understood.
In particular, the longitudinal symptomatic course of BD is chronic and dominated by depressive symptoms, rather than the characteristic manic symptoms of BD, and – surprisingly – the depressive state can be dominant for as much as ≥50% during the course of BD.Citation7–Citation9 These longitudinal depressive symptoms lead to loss of social benefits for BD patients. On the other hand, when it comes to switching to mania, patients with BD lose many aspects of their lives and experience problems such as debts and divorce. BD patients in the mixedCitation10 or depressiveCitation11 states are more prone to suicide.
Treatment for bipolar disorder
Even though many reports and guidelines have suggested that antidepressants may increase the risk of switching to mania in BD,Citation12,Citation13 clinicians have been using antidepressants to treat patients with bipolar depression.Citation14,Citation15 While this may sound strange to researchers of pharmacology, it is not unusual in the clinical field. Although antidepressants are used to treat bipolar depression currently, the specific mechanisms that are modified by antidepressants and cause the switching to mania remain unclear.
Early improvement of patients with BD during their long-term depressive symptom is beneficial to the outcome of the treatment for this disorder, but this has been a great challenge to – as well as the aim of – clinicians, who, when treating the patient, is struggling with a dilemma of having to choose between improvement of the depressive symptom and switching to mania. Therefore, clinicians need to understand the characteristics of antidepressants for their optimal use for improvement and offset the risk of switching to mania. Furthermore, researchers need to understand the pathophysiology of BD to facilitate their work on drugs that help in symptom improvement and overcome the risk of switching to mania.
Currently, the clinical guidelinesCitation6,Citation16 grade the risk of switching to mania by classifying antidepressants into groups such as selective serotonin reuptake inhibitors (SSRIs), serotonin and noradrenaline reuptake inhibitors (SNRIs), and tricyclic antidepressants (TCAs). Even though these agents have similar pharmacological effects as the monoamine reuptake inhibitor, the pharmacological characteristics are different for each medication even within the same class.
To begin with, this review summarizes the clinical evidence with particular focus on the biological characteristics underpinning the pathophysiology of BD in the section on “Biological background”. Next, this review outlines the treatment guidelines and formulates a strategy with particular focus on bipolar depression.
Overall, the proportion of patients receiving at least one mood stabilizer increases significantly every year.Citation17 The significant increases in the prescription of mood stabilizers probably reflect the increasing awareness and implementation of recent evidence-based medicine guidelines into clinical practice.Citation16
Regarding treatment with antidepressants, some studies and treatment guidelines suggest that antidepressant treatments for BD may have the potential to increase manic switching, while others recommend short-term antidepressant treatment and early discontinuation.Citation12,Citation13 Nevertheless, even now, clinicians have been using antidepressants to treat BD patients with acute bipolar depression. The possible disadvantages of longitudinal depression may be greater for BD patients than the disadvantages of switching to mania, as a matter of course, clinicians should avoid the treatment of BD patients with medicines that increase the risk of switching to mania. Regarding treatment with antidepressants for bipolar depression, antidepressants were not found to be statistically superior to placebo or other current standard treatments for bipolar depression.Citation18,Citation19 However, it is also reported that antidepressants were more effective than placebo.Citation15 Antidepressants were also reported to be effective for the short-term treatment of bipolar depression.Citation15 More interestingly, a previous study suggested that switching is a common early complication of treatment with antidepressants.Citation18 Thus, the risk of switching to mania differed widely according to the types of antidepressants. The rate of switching for TCAs was 10%, while that for all other antidepressants combined was 3.2%.Citation15 These findings show that the rates of switching differ within the same class of antidepressants. Thus, I suggest that the rate of switching is decided by the pharmacologic strength and dose of a particular drug, rather than by a simple common pharmacological action.
Based on these differences in the risk of switching, avoiding the use of TCAs has generally been proposed in clinical reports.Citation12,Citation13 Clinicians would have had suspicions that antidepressants other than TCAs are superior in terms of both the risk of switching and the efficacy against depression compared with TCAs. Furthermore, these studies do not provide evidence that all antidepressants in the same class can provide equally beneficial results in terms of similar pharmacological effects on BD patients. Antidepressants may be a double-edged sword. Clinicians should carefully consider both the risk of switching and the efficacy against depression from the point of view of pharmacology for each medication, rather than looking for similar pharmacological effects.
Considering these discussions, the pathology of BD needs to be verified. Thus, it should be acknowledged that BD can be influenced by certain types of substances. Although BD patients experience spontaneous switching, this can also be induced by antidepressants. Therefore, it is necessary to know about the existence of substances affecting the biological background during the process of switching to mania. In the next part of the review, the first paragraph describes my understanding of the biological background of BD to date.
Biological background
Spontaneous hypothesis
Retrospective data obtained from patients hospitalized between 1920 and 1959 revealed a rate of 29% for spontaneous switching from depression to hypomania.Citation20 The fact that most patients with BD receive mood stabilizers makes spontaneous switching even more difficult to estimate accurately.Citation15 In studies on genetic polymorphisms associated with responses to antidepressants, spontaneous switching was proposed to have a very different mechanism from that associated with responses to antidepressants.Citation21 Thus, although the possibility of spontaneous switching cannot be denied, many reports have suggested that a past history of multiple antidepressant trials is associated with switching to mania.Citation22 It is reasonable to think that some substances that assist antidepressants in switching to mania do exist.
Catecholaminergic hypothesis
Higher levels of urinary noradrenalineCitation23–Citation25 and dopamineCitation24,Citation25 have been associated with mania and switching to mania. In a double-blind, randomized, placebo-controlled study on bipolar depression, almost all subjects treated with l-3,4-dihydroxyphenylalanine (l-dopa), the catecholamine precursor, developed hypomanic symptoms after ~1 week.Citation26 More interestingly, the incidence of hypomania was increased with a greater dose of l-dopa, and a reduction in dose or discontinuation of l-dopa was followed by disappearance of the hypomanic symptoms within 48 hours in these patients.Citation26 Thus, in bipolar patients, hypomanic behaviors are induced more than spontaneous mania by l-dopa, and catecholamines are involved in the pathophysiology of BD. However, patients with major depressive disorder were not induced toward hypomanic symptoms when treated with l-dopa. These findings may indicate that the pathophysiology based on biological substances differs between bipolar depression and major depression. Moreover, on l-dopa administration at similar dosages to 394 patients with Parkinson’s disease, hypomania was described in only three patients (<1%).Citation26 Meanwhile, schizophrenia-like symptoms, such as organic hallucinosis, develop as the most common drug-induced side effects of l-dopa.Citation27 The increase in monoamine levels induced by l-dopa involves two substances. One is dopamine, and the other is noradrenaline. Although the switching process is correlated with monoamines, the roles of the noradrenergic and dopaminergic systems in the switching process are not clearly defined. It is easy to imagine that schizophrenia and dopamine have a strong correlation. Although mania has partially similar symptoms as schizophrenia, it is not the same disorder as a whole, and it is important to note that BD has different symptoms from schizophrenia. It is clinically important to understand that manic symptoms are different from schizophrenia-like symptoms according to the ICD and DSM.
On the other hand, in clinical studies on 3-methoxy-4-hydroxyphenylglycol (MHPG), noradrenaline metabolites, and homovanillic acid (HVA), the dopamine metabolite levels were higher in bipolar manic patients than in bipolar remission patients on antipsychotics (chlorpromazine equivalence: 380±110 and 300–600 mg/d, respectively).Citation28–Citation30 Thus, it is known that levels of dopamine, noradrenaline metabolites, HVA, and MHPG are reduced by antipsychotic drug treatment. Unfortunately, it is not clear whether the depletion of HVA or MHPG is caused by the antipsychotics or improvement in symptoms. It is important for researchers to understand that depression is a different symptom from sedation induced by antipsychotics. Likewise, the roles of the noradrenergic and dopaminergic systems in the switching process from mania to depression are not clearly defined.
Dopaminergic hypothesis
Amphetamine has been shown to trigger euphoria in healthy volunteers, mostly through increased dopamine levels in the anteroventral striatum.Citation31 In addition, Lu et alCitation32 indicated a possible relationship between manic symptoms and ketamine abuse in a case report. This relationship may be attributed to the increased dopamine level in the brain tissue brought about through dopamine release after chronic dosing with ketamine.Citation33 Thus, pharmacological evidence supports the notion that manipulation of the dopaminergic system can mimic the symptoms of BD. However, amphetamine- or ketamine-induced psychotic disorder and the manic state of BD differ in the diagnostic criteria of the ICD and DSM. Thus, some of these similar symptoms cause confusion in devising pharmacological strategies. However, the use of aripiprazole, a partial agonist of the dopamine D2 receptor,Citation34 during the maintenance phase was reported to protect against manic relapses, but not against depressive relapses.Citation35,Citation36 Furthermore, this drug was shown to be negative in treating bipolar depression.Citation37 From these clinical findings, it may be surmised that dopamine may be involved in sedation or calmness, but not in the pathophysiology of BD.
Noradrenergic hypothesis
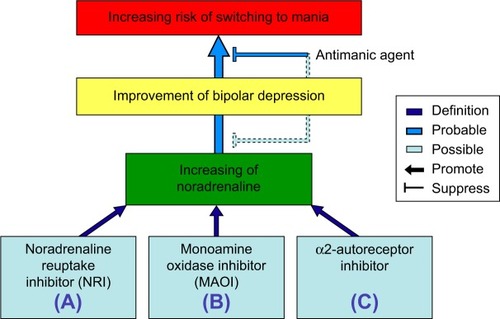
The urinary concentrations of noradrenaline and its metabolite MHPG were significantly lower in depression than in mania.Citation23 Although HVA, a dopamine metabolite, did not differ, MHPG, a noradrenaline metabolite, was greater in untreated BD patients than in healthy controls.Citation38 Recently, it was reported that MHPG is a biomarker for the switch from the manic state to the remission state in BD.Citation28 The study suggested that the effects of antipsychotics were slight with reference to chlorpromazine equivalence (average: 134 mg/d). In addition, in multiple regression analyses, the plasma levels of MHPG reflected the pathophysiology of BD from the manic state to the depressive state more clearly than did plasma HVA or brain-derived neurotrophic factor (BDNF).Citation9 Thus, noradrenaline may be involved in the pathophysiology of BD ().
Figure 1 Schematic illustration showing the improvement or switching pathways induced by various antidepressants affecting the levels of noradrenaline.
BDNFergic hypothesis
Blood BDNF levels in the manic state were reported to be highCitation39,Citation40 or lowCitation41 in different studies, compared with remission or control subjects, and the conclusions were incoherent and unclear. In our study, BD patients exhibited no significant changes in BDNF level throughout the manic state.Citation28 In the human brain, BDNF immunoreactivity was reported to be increased in postmortem hippocampal tissues obtained from subjects with major depression, BD, or schizophrenia, as well as in nonpsychiatric control subjects treated with antidepressant medications.Citation42 In contrast, chronic (21 days) treatment with the TCA desipramine, the SSRI fluoxetine, and the monoamine oxidase inhibitor (MAOI) phenelzine increased BDNF levels in the frontal cortex.Citation43 Interestingly, the increases in BDNF showed differences and were in the following order: MAOI > SSRI > TCA > vehicle. If BDNF is involved in the switching to mania, explanation of this observation becomes very difficult. In addition, BDNF was not correlated with the manic state of BD in our study.Citation28 Furthermore, BDNF did not show correlations among the depressive, remission, and manic states of BD in another report.Citation9
Noradrenaline and antidepressants
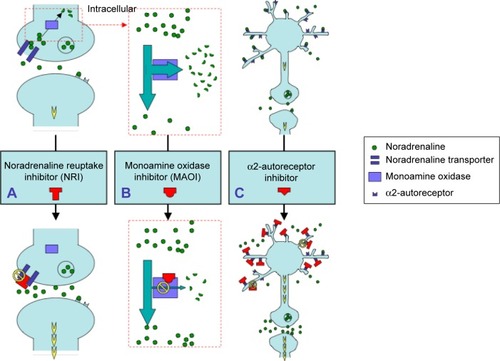
From these hypotheses, it is supported that noradrenaline is involved in the pathophysiology of BD, as well as being associated with the switch to mania. In this context, it is suggested that both the antidepressant effect of and the switching to mania caused by noradrenaline are issues of particular importance in the context of BD. Augmentation of noradrenaline can be the result of the following three actions ( and ): (A) increasing noradrenaline in the synaptic cleft by noradrenaline reuptake inhibitory action; (B) inhibition of noradrenaline deactivation by MAOIs; and (C) release of noradrenaline by α2-autoreceptor blockage. The following three sources underlie this evidence. For (A), antidepressants are involved with noradrenaline reuptake transporter (NRT), and noradrenaline reuptake inhibitors (NRIs) were more effective than placebo for bipolar depression.Citation15 In addition, avoiding antidepressant use has generally been proposed in clinical guidelines, considering the potential risk for switching to mania or rapid cycling during the treatment.Citation16,Citation44 Thus, NRT may participate in the pathophysiology of BD. For (B), the development of an 11C-harmine brain-imaging technique led to the interesting observation that brain monoamine oxidase (MAO) levels were elevated in a number of cortical, striatal, and midbrain areas in subjects suffering from major depressive disorder.Citation45 However, even after the complete characterization of MAO-A and MAO-B subtypes, many aspects of the physiological actions of these enzymes are unclear.Citation46 MAO is localized intracellularly.Citation47 Thus, in the cell, pathway (B) works through pathway (A). From the pharmacological point of view, pathway (A) takes precedence over pathway (B) in the mechanism of switching to mania (). For (C), mirtazapine is an antidepressant that blocks the α2-autoreceptor. It was shown in a case report that mirtazapine induced switching to a manic state.Citation48 In contrast, another report showed that this medicine did not induce switching to a manic state.Citation49 Large-scale follow-up studies are needed to understand the effects of mirtazapine.
Figure 2 Schematic illustration of the pathways leading to increasing noradrenaline levels as caused by the administration of various antidepressants.
Abbreviations: MAOI, monoamine oxidase inhibitor; NRI, noradrenaline reuptake inhibitor.
Antidepressants and bipolar depression
Classification of antidepressants as TCAs or SSRIs is confusing for clinicians. For a focus on NRIs, it might be necessary to verify both the manic risk and antidepressive effect for each medication. In the treatment of bipolar depression, a pharmaceutical class effect is the exception rather than the rule, and such class effects only involve the switching to mania and the drug class of antidepressants. Thus, the effect of the individual drug is more important than the drug class.
It is interesting to note that two naturalistic studies found significantly lower rates of switching to mania when patients were treated with SSRIs compared with those on TCAs.Citation50,Citation51
As can be seen from the values of the equilibrium dissociation constant (KD) for noradrenaline transporter (NET), TCAs are substantially more potent with reference to noradrenaline reuptake action in comparison with all SSRIs. In this review, it was reported that a potent positive correlation between the mania rating scale and noradrenaline metabolite levels are correlated in two reports. Therefore, it is suggested that the strength of noradrenaline reuptake action, based on the KD value of NET, indicates a potent risk factor for switching to mania when BD patients are treated with antidepressants. The relative risk factors of various antidepressant drugs using the KD values of NETCitation52 for switching to mania are shown in .
Table 1 Various antidepressants showing the improvement of depression or the risk of switching to mania based on their affinities for NET
These risk factors for switching to mania were determined based on this simple premise and are indicated as no possibility (−), possibility (+), strong possibility (++), or very strong possibility (+++). It is suggested that high-KD NET drugs should be recommended more often relative to very low-KD NET drugs such as secondary amine TCAs. Additionally, antidepressants should be carefully considered in terms of the balance between the risk of switching and the efficacy against depression before recommending low-KD NET drugs for bipolar depression. Further studies with larger naturalistic study populations may be necessary to confirm the benefits of NET KD information in the treatment of bipolar depression.
Interestingly, the effects of antidepressants are different from the effects of noradrenaline, even if the classifications are the same. The data do not suggest that switching is a common early complication of treatment with antidepressants. It is suggested that both the risk of switching and the efficacy against depression should be evaluated for each medication, rather than by similar pharmacological effects. A recent double-blind, placebo-controlled study evaluating paroxetine monotherapy in the treatment of bipolar depression failed to show any advantage compared with placebo.Citation53 This finding for paroxetine is consistent with those in .
Augmentation of noradrenaline is effective for treating the depressive state in BD but entails the risk of switching to mania in BD. Therefore, if the depressive symptom is severe, the short-term treatment to augment noradrenaline will be recommended for severe bipolar depression. However, if the depressive symptom is mild or in remission, augmentation of noradrenaline will increase the risk of switching to mania. Consequently, NRIs will not be recommended for maintenance treatment. Thus, antidepressants with strong indications should be used in the short-term treatment for severe bipolar depression.
Conclusion
In summary, the results for plasma levels of MHPG may reflect the pathophysiology of BD from the manic state to the depressive state more than the plasma levels of HVA or BDNF. These data suggest that peripheral MHPG, which is associated with noradrenaline levels in the brain, could be used as a biomarker for whole mood states in BD. The MHPG levels, reflecting the noradrenaline levels in the brain, are likely to reflect the clinical characteristics of the switching process in BD and to have prognostic significance for the treatment of manic and depressive states. Therefore, it is suggested that antidepressant treatment for BD should be considered on the basis of the KD values for NET. Antidepressants may be effective for the short-term treatment of bipolar depression. In addition, clinicians should carefully consider treatment strategies based on the biological background. From our study, the augmentation of noradrenaline will have beneficial effects in bipolar depression, while being associated with an increased risk of switching in BD. Thus, augmentation of noradrenaline is a double-edged sword. Consequently, antidepressants may need to be used in combination with an antimanic agent, such as lithium, as suggested in the guidelines. It is hoped that agents such as noradrenaline stabilizers are developed for BD in the future. Antidepressants augmenting noradrenaline may be effective for bipolar depression. However, it is easily presumed that such antidepressants will also have a risk of switching to mania. Therefore, antidepressants will be the recommended treatment in combination with an antimanic agent, or for short-term treatment with early discontinuation, as suggested in other reports. Guidelines for medicinal treatment should probably be reevaluated and updated based on the biological background.
Acknowledgments
The publication fees for this review were supported by funding from the Sato Hospital, Koutokukai, Japan. The review did not receive funding from any pharmaceutical corporations.
Disclosure
The author reports no conflicts of interest in this work.
References
- KastrupMCRamosABGlobal mental healthDan Med Bull2007541424317349222
- World Health OrganizationInternational Classification of Diseases. 10th revisionGeneva, SwitzerlandWorld Health Organization2010
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders5th edWashington, DCAmerican Psychiatric Association2013
- RushAJToward an understanding of bipolar disorder and its originJ Clin Psychiatry200364suppl 648 discussion 2812720474
- RosaARFrancoCMartinez-AranAFunctional impairment in patients with remitted bipolar disorderPsychother Psychosom200877639039218716425
- AssociationAPPractice guideline for the treatment of patients with bipolar disorder (revision)Am J Psychiatry20021594 suppl150
- JuddLLAkiskalHSSchettlerPJThe long-term natural history of the weekly symptomatic status of bipolar I disorderArch Gen Psychiatry200259653053712044195
- JuddLLAkiskalHSSchettlerPJA prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorderArch Gen Psychiatry200360326126912622659
- KuritaMNishinoSNumataYOkuboYSatoTThe noradrenaline metabolite MHPG is a candidate biomarker between the depressive, remission, and manic states in bipolar disorder I: two long-term naturalistic case reportsNeuropsychiatr Dis Treat20151135335825709459
- YoungAHEberhardJEvaluating depressive symptoms in mania: a naturalistic study of patients with bipolar disorderNeuropsychiatr Dis Treat2015111137114325995638
- ValtonenHMSuominenKHaukkaJDifferences in incidence of suicide attempts during phases of bipolar I and II disordersBipolar Disord200810558859618657243
- FountoulakisKNKasperSAndreassenOEfficacy of pharmacotherapy in bipolar disorder: a report by the WPA section on pharmacopsychiatryEur Arch Psychiatry Clin Neurosci2012262suppl 114822622948
- PodawiltzAA review of current bipolar disorder treatment guidelinesJ Clin Psychiatry2012733e1222490265
- CohnJBCollinsGAshbrookEWernickeJFA comparison of fluoxetine imipramine and placebo in patients with bipolar depressive disorderInt Clin Psychopharmacol1989443133222607128
- GijsmanHJGeddesJRRendellJMNolenWAGoodwinGMAntidepressants for bipolar depression: a systematic review of randomized, controlled trialsAm J Psychiatry200416191537154715337640
- YathamLNKennedySHSchafferACanadian network for mood and anxiety treatments (CANMAT) and International Society for bipolar disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2009Bipolar Disord200911322525519419382
- Walpoth-NiederwangerMKemmlerGGrunzeHTreatment patterns in inpatients with bipolar disorder at a psychiatric university hospital over a 9-year period: focus on mood stabilizersInt Clin Psychopharmacol201227525626622842799
- ZhangYYangHYangSAntidepressants for bipolar disorder: a meta-analysis of randomized, double-blind, controlled trialsNeural Regen Res20138312962297425206617
- SidorMMMacqueenGMAntidepressants for the acute treatment of bipolar depression: a systematic review and meta-analysisJ Clin Psychiatry201172215616721034686
- AngstJSwitch from depression to mania, or from mania to depressionJ Psychopharmacol198711131922158748
- SerrettiALilliRSmeraldiEPharmacogenetics in affective disordersEur J Pharmacol2002438311712811909602
- TrumanCJGoldbergJFGhaemiSNSelf-reported history of manic/hypomanic switch associated with antidepressant use: data from the systematic treatment enhancement program for bipolar disorder (STEP-BD)J Clin Psychiatry200768101472147917960960
- PostRMStoddardFJGillinJCAlterations in motor activity, sleep, and biochemistry in a cycling manic-depressive patientArch Gen Psychiatry1977344470477192169
- BunneyWEJrMurphyDLGoodwinFKBorgeGFThe switch process from depression to mania: relationship to drugs which alter brain aminesLancet197017655102210274191630
- JuckelGHegerlUMavrogiorgouPClinical and biological findings in a case with 48-hour bipolar ultrarapid cycling before and during valproate treatmentJ Clin Psychiatry200061858559310982202
- MurphyDLBrodieHKGoodwinFKBunneyWEJrRegular induction of hypomania by L-dopa in “bipolar” manic-depressive patientsNature197122952801351364321339
- FactorSAMolhoESPodskalnyGDBrownDParkinson’s disease: drug-induced psychiatric statesAdv Neurol1995651151387872135
- KuritaMNishinoSNumataYOkuboYSatoTThe noradrenaline metabolite MHPG is a candidate biomarker from the manic to the remission state in bipolar disorder I: a clinical naturalistic studyPLoS One201496e10063424971450
- YoshimuraRNakanoYHoriHIkenouchiAUedaNNakamuraJEffect of risperidone on plasma catecholamine metabolites and brain-derived neurotrophic factor in patients with bipolar disordersHum Psychopharmacol200621743343817029305
- BowersMBJrSwigarMEJatlowPIHoffmanFJPlasma catecholamine metabolites and treatment response at neuroleptic steady stateBiol Psychiatry19892567347382923935
- DrevetsWCGautierCPriceJCAmphetamine-induced dopamine release in human ventral striatum correlates with euphoriaBiol Psychiatry2001492819611164755
- LuYYLinCHLaneHYMania following ketamine abuseNeuropsychiatr Dis Treat20161223723926869791
- LiBLiuMLWuXPEffects of ketamine exposure on dopamine concentrations and dopamine type 2 receptor mRNA expression in rat brain tissueInt J Clin Exp Med201587111811118726379921
- BurrisKDMolskiTFXuCAripiprazole, a novel antipsychotic, is a high-affinity partial agonist at human dopamine D2 receptorsJ Pharmacol Exp Ther2002302138138912065741
- KeckPEJrCalabreseJRMcQuadeRDAripiprazole Study GroupA randomized, double-blind, placebo-controlled 26-week trial of aripiprazole in recently manic patients with bipolar I disorderJ Clin Psychiatry200667462663716669728
- KeckPEJrCalabreseJRMcIntyreRSAripiprazole Study GroupAripiprazole monotherapy for maintenance therapy in bipolar I disorder: a 100-week, double-blind study versus placeboJ Clin Psychiatry200768101480149117960961
- ThaseMEJonasAKhanAAripiprazole monotherapy in nonpsychotic bipolar I depression: results of 2 randomized, placebo-controlled studiesJ Clin Psychopharmacol2008281132018204335
- ZumarragaMDavilaRBasterrecheNCatechol O-methyltransferase and monoamine oxidase A genotypes, and plasma catecholamine metabolites in bipolar and schizophrenic patientsNeurochem Int2010566–777477920206656
- BarbosaIGRochaNPMirandaASIncreased BDNF levels in long-term bipolar disorder patientsRev Bras Psiquiatr2013351676923567603
- BarbosaIGHuguetRBMendoncaVAIncreased plasma levels of brain-derived neurotrophic factor in patients with long-term bipolar disorderNeurosci Lett20104752959820350583
- Machado-VieiraRDietrichMOLekeRDecreased plasma brain derived neurotrophic factor levels in unmedicated bipolar patients during manic episodeBiol Psychiatry200761214214416893527
- ChenBDowlatshahiDMacQueenGMWangJFYoungLTIncreased hippocampal BDNF immunoreactivity in subjects treated with antidepressant medicationBiol Psychiatry200150426026511522260
- BaluDTHoshawBAMalbergJERosenzweig-LipsonSSchechterLELuckiIDifferential regulation of central BDNF protein levels by antidepressant and non-antidepressant drug treatmentsBrain Res20081211374318433734
- MalhiGSTaniousMDasPBerkMThe science and practice of lithium therapyAust N Z J Psychiatry201246319221122391277
- MeyerJHGinovartNBoovariwalaAElevated monoamine oxidase a levels in the brain: an explanation for the monoamine imbalance of major depressionArch Gen Psychiatry200663111209121617088501
- FinbergJPUpdate on the pharmacology of selective inhibitors of MAO-A and MAO-B: focus on modulation of CNS monoamine neurotransmitter releasePharmacol Ther2014143213315224607445
- EdmondsonDEBindaCWangJUpadhyayAKMatteviAMolecular and mechanistic properties of the membrane-bound mitochondrial monoamine oxidasesBiochemistry200948204220423019371079
- BasavrajVNanjundappaGBChandraPSMirtazapine induced mania in a woman with major depression in the absence of features of bipolarityAust N Z J Psychiatry2011451090121692606
- GaoKKempDEGanocySJTreatment-emergent mania/hypomania during antidepressant monotherapy in patients with rapid cycling bipolar disorderBipolar Disord200810890791519594506
- BoerlinHLGitlinMJZoellnerLAHammenCLBipolar depression and antidepressant-induced mania: a naturalistic studyJ Clin Psychiatry19985973743799714266
- BottlenderRRudolfDStraussAMollerHJMood-stabilisers reduce the risk of developing antidepressant-induced maniform states in acute treatment of bipolar I depressed patientsJ Affect Disord2001631–3798311246083
- TatsumiMGroshanKBlakelyRDRichelsonEPharmacological profile of antidepressants and related compounds at human monoamine transportersEur J Pharmacol19973402–32492589537821
- McElroySLWeislerRHChangWEMBOLDEN II (Trial D1447C00134) Investigators. A double-blind, placebo-controlled study of quetiapine and paroxetine as monotherapy in adults with bipolar depression (EMBOLDEN II)J Clin Psychiatry201071216317420122366
