Abstract
Background
Clinical practice guidelines suggest routine screening for distress among cancer patients for immediate early psychiatric care. However, previous studies focusing on routine screening for psychological distress among cancer inpatients in Taiwan are scant. Thus, the aim of this study was to evaluate the prevalence and related factors of psychological distress and mental illness among cancer inpatients in Taiwan.
Patients and methods
This study was conducted as a retrospective chart review in a general hospital in southern Taiwan. Cancer inpatients were regularly screened by nursing staff using the Distress Thermometer and the 12-item Chinese Health Questionnaire. Positive screening results on either instrument were followed by a non-commanded referral to psychiatrists for clinical psychiatric diagnosis and treatment.
Results
Of the 810 participants in this study, 179 (22.1%) were recognized as having psychological distress. Younger age (odds ratio [OR] =1.82), having head and neck cancer (OR =2.43), and having not received chemotherapy (OR =1.58) were significantly related to psychological distress. Among the 56 patients (31.3%) with psychological distress who were referred to psychiatrists, the most common mental illness was adjustment disorder (n=22, 39.2%), followed by major depressive disorder (n=13, 23.2%), depressive disorder not otherwise specified (n=6, 10.7%), and anxiety disorder not otherwise specified (n=4, 7.1%).
Conclusion
Our study indicated that cancer inpatients with psychological distress were more likely to be younger in age, have head and neck cancer, and have not received chemotherapy. The most common psychiatric disorder was adjustment disorder. Early detection of psychological distress and prompt psychiatric consultation and management are very important for cancer inpatients.
Introduction
Cancer-related distress was depicted as a “multifactorial unpleasant emotional experience of a psychological, social, and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms, and its treatment” by the National Comprehensive Cancer Network (NCCN) of the US.Citation1 Distress is related to a lower quality of life,Citation2 treatment compliance and efficacy,Citation3,Citation4 higher mortality,Citation5–Citation7 and a higher risk of suicide.Citation8,Citation9 Therefore, clinicians should make efforts to promote patients’ quality of life and decrease medical costs by alleviating patient distress.Citation10,Citation11
The NCCN clinical practice guidelines (NCCN guidelines) in oncology distress management have, since 1997, advocated routine screening for distress in cancer patients.Citation1 Similar to the model of using pain for the 5th vital sign, the use of distress for the 6th vital sign was recommended in 2005.Citation12
Several medical centers have recommended regular screenings on all cancer patients, as a component of routine cancer management.Citation13 This type of routine cancer care underscores that all patients with distress should receive the appropriate treatment and that top quality psychosocial cancer management involves systematic reevaluation and follow-up. However, challenges to care persist, containing not only the underestimation of the demand for psychosocial care but also the likely related factors. Since a majority of traditional tools designed to screen depression and distress are time-consuming for routine utilization in clinical situations, uncomplicated verbal and visual analog tools, such as the Distress Thermometer (DT),Citation14 the emotions thermometer,Citation15 and the 12-item General Health Questionnaire,Citation16 have been recommended. Of these scales, DT is probably the most widely utilized.Citation17–Citation20
Although several investigations on cancer patients with psychological distress have been published, there are very few investigations on the related factors of distress and its prevalence in Taiwanese patients. The prevalence of psychological distress as screened by the DT was 56.5% and 28.8%, respectively, according to Shim et al and Kim et al.Citation21,Citation22 However, study limitations, including low response rates and scanty sample sizes, rendered generalization of the results to all cancer patients difficult. But with the increasing demands for treating distress in cancer patients, numerous hospitals have developed regular procedures for detecting and managing this condition.
A regular procedure for screening distress has been continually performed at Kaohsiung Chang Gung Memorial Hospital since December 2014. This program has assisted in caring for and approaching distressed patients. In this study, we intended to ascertain the related factors and prevalence of psychological distress among cancer inpatients in a general hospital. We also aimed to evaluate psychiatric disorders among cancer inpatients with psychological distress.
Patients and methods
Participants
This study was conducted as a retrospective chart review in a general hospital in southern Taiwan from December 2014 to May 2015. Our inclusion criteria were as follows: 1) newly hospitalized patients with any confirmed cancer and 2) patients with verbal or written communication ability. Exclusion criteria were as follows: 1) patients with impaired consciousness (Glasgow Coma Scale score below 15 points) and 2) patients who had been readmitted and underwent DT and 12-item Chinese Health Questionnaire (CHQ-12) screening within the past 3 months. However, we could not review the patients who were initially excluded from the program. Therefore, we did not compute the overall response rate for all the procedures.
Measurement of psychological symptoms
Distress Thermometer
The DT is a 1-item self-report screening tool for evaluating psychological distress in patients with cancer.Citation15,Citation23,Citation24 The DT grades distress levels over the prior week based on a visual analog scale with scores from 0 (indicating no distress) to 10 (indicating extreme distress). The DT has been utilized in diverse populations and its performance has been compared with different self-report symptom scales.Citation14,Citation25,Citation26 Scores of 4 or 5 have each been investigated as potential cutoff scores on the DT to show significant distress in different studies.Citation14,Citation24–Citation29 According to the Taiwan Psycho-Oncology Society, a cutoff of 5 on the DT possesses the optimal sensitivity and specificity characteristics among Taiwanese cancer patients.Citation30–Citation32
12-Item Chinese Health Questionnaire
The CHQ-12, with cultural sensitivity, is an excellent tool for researching the potential psychiatric morbidity among ethnic Chinese individuals. The CHQ-12 was developed in Taiwan and derived from the 12-item General Health Questionnaire, which is widely used worldwide.Citation33 The CHQ-12 is a standardized screening tool and has been used previously in surveys of minor psychiatric morbidity in 3 communities in Taiwan.Citation34 It contains a 4-point response scale: 0= “not at all” and “same as usual”; 1= “rather more than usual” and “much more than usual”. It can be used to recognize a patient with a possible minor mental disorder based on a cutoff score above 3. The weighted validity of this instrument was found to be acceptable.Citation34,Citation35
Procedures
Ethical approval was obtained from the Human Research Ethics Committee of Chang Gung Memorial Hospital which waived the requirement to obtain patient’s consent as all the data assessed in this study were collected from our regular clinical care to which the patients have already agreed. A 5-stage procedure was utilized ().
Figure 1 The cancer psychological consultant service implemented in a general hospital.
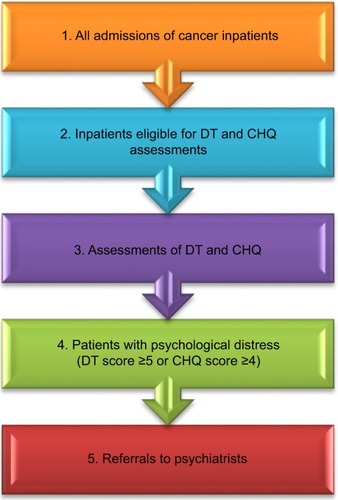
Stage 1
The psycho–oncological consultant service was progressively implemented in our general hospital, from the head and neck cancer ward, urologic cancer ward, colorectal cancer ward to other wards. All the nurses at the oncology wards were required to attend a 120-minute training course given by the program investigators according to the hospital policy. The psychologist taught the nurses how to use the standardized questions in the clinical scenarios. These trained staff would then determine who were eligible for the distress screening program (using the inclusion and exclusion criteria described earlier).
Stage 2
The distress screening tools were assessed before the cancer treatment. Nursing staff at the medical oncology wards routinely provided a distress screening service after explaining the aim and procedure of the program to the eligible patients.
Stage 3
In our study, a patient with distress was defined as having a score of ≥5 on the DT or a score of ≥4 on the CHQ-12.Citation35,Citation36 Similar to the previous DT studies,Citation14,Citation24,Citation26,Citation29 only the visual analog DT itself was evaluated; the companion problem list was skipped.
Stage 4
The nursing staff’s assessment and patient sociodemographic data were entered into the electronic nursing records within 48 hours after admission. Scores ≥5 points on the DT or scores ≥4 points on the CHQ-12, which represent psychological distress, indicated that a psychiatric consultation would be suggested by a pop-up window embedded in the Health Information System of our hospital.
Stage 5
Based on the screening results and pop-up window’s suggestion, the final decision on the referral was made by the in-charge doctor, who evaluated clinical factors, including the patient’s preference for a psychiatric referral and their physical condition. Each referred cancer inpatient was assessed at bedside by senior psychiatrists within 24 hours after referrals. Psychiatric diagnoses were made according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision.Citation37
Sociodemographic data and clinical information based on a medical chart review including the nursing staff’s evaluation and physicians’ assessment were collected. The sociodemographic variables assessed were age, sex, marital status, employment status, education, and current cigarette, alcohol, and betel nut use. We asked whether the patient currently uses these substances habitually or not. The clinical characteristics were comorbid medical diseases, cancer diagnosis, cancer staging, and cancer treatment (surgery, radiotherapy, chemotherapy, and hormonal therapy) in which the patient had received. Since the stage of leukemia could not be defined, patients with leukemia were excluded when cancer staging was investigated. Comorbid medical diseases of patients included hypertension, diabetes mellitus, thyroid disease, heart diseases, respiratory diseases, autoimmune diseases, neurological diseases, etc.
Statistical analysis
Values are shown as mean ± SD. We used SPSS version 12.0 (IBM Corporation, Armonk, NY, USA) to analyze descriptive and inferential statistics. Descriptive statistics (χ2 and Student’s t-tests) were executed first to investigate the difference in demographic data and clinical characteristics among the subjects with and without psychological distress. A stepwise forward model of logistic regression was utilized to examine the possible related factors that reach significant levels in univariate analysis, using clinical and demographic data. The significance level was set at P<0.05.
Results
Sociodemographic and clinical characteristics of the participants
Of the 810 study participants, 32 did not complete the CHQ-12 assessments, and 10 did not complete the DT assessments. The reasons for incomplete data were unknown. The average age of the patients was 59.4±13.2 years. A majority of the participants were male (73.1%), married (88.3%), educated to a high school or higher level (65.3%), and unemployed (64.9%). The predominant clinical diagnosis was head and neck cancer (30.7%), and 44.2% of the participants were in stage 4 (). The other cancer types included breast cancer, liver cancer, lung cancer, connective tissue cancer, pancreas cancer, and esophageal cancer ().
Table 1 Sociodemographic and clinical characteristics of the participants
Prevalence and related factors of psychological distress among cancer patients
Of the 810 inpatients, 179 (22.1%) were designated as having psychological distress. Inpatients with psychological distress were significantly younger compared with elder inpatients (χ2=16.66, P<0.001), had a lower educational level compared with having a higher educational level (χ2=9.06, P=0.011), had head and neck cancer compared with having other cancers (χ2=41.05, P<0.001), and had not received chemotherapy compared with having received chemotherapy (χ2=9.35, P=0.002). No significant correlations were determined in the light of sex, marital status, employment status, comorbid other disease, having received surgery, radiotherapy and hormonal therapy, cancer staging, and current cigarette, alcohol, and betel nut use (). When the significant variables mentioned earlier were investigated with respect to psychological distress utilizing the stepwise forward model of logistic regression, younger age (odds ratio [OR] =1.82; 95% CI, 1.22–2.71; P=0.003), having head and neck cancer (OR =2.43; 95% CI, 1.71–3.46; P<0.001), and having not received chemotherapy (OR =1.58; 95% CI, 1.09–2.29; P=0.015) were ascertained to be 3 significant related factors ().
Table 2 Comparison of sociodemographic and clinical characteristics between patients with and without psychological distress
Table 3 Related factors for psychological distress among cancer inpatients: logistic regression analysis
Categorization of psychiatric disorders among cancer inpatients with significant psychological distress
Of the 179 inpatients with psychological distress, 123 were not referred to psychiatrists; 56 inpatients (31.3%) received a psychiatric assessment and psychiatric diagnosis (). The diagnoses comprised adjustment disorder (n=22, 39.2%), major depressive disorder (n=13, 23.2%), depressive disorder not otherwise specified (n=6, 10.7%), anxiety disorder not otherwise specified (n=4, 7.1%), delirium (n=2, 3.6%), psychotic disorder not otherwise specified (n=1, 1.8%), and insomnia disorder (n=1, 1.8%). Seven patients (12.5%) did not have a psychiatric diagnosis.
Table 4 Psychiatric diagnoses of cancer inpatients
Discussion
The primary result from our report was that 22.1% of the cancer patients suffered from psychological distress. The psychological distress in cancer inpatients was significantly associated with younger age, head and neck cancer, and having not received chemotherapy. The most common psychiatric disorder was adjustment disorder, followed by major depressive disorder, depressive disorder not otherwise specified, and anxiety disorder not otherwise specified. So far as we know, this is the first research to investigate the routine screening for psychological distress among Taiwanese cancer inpatients using DT and CHQ.
Prevalence and related factors of psychological distress among cancer patients
Our finding that 22.1% of the cancer inpatients had psychological distress was concordant with the previous data reporting that nearly 20%–40% of cancer patients suffered from psychological distress.Citation15,Citation38–Citation42 But our result was lower than that in 2 studies on Korean cancer patientsCitation21,Citation22 and other studies,Citation43,Citation44 which found a rate higher than 50%. This variation in prevalence was related mostly to research method (retrospective or prospective study), sample size, ethnicity, diagnostic criteria, and cancer types. In Taiwan, there has been one study on the prevalence of psychological distress among cancer inpatients as recognized by routine screening utilizing the Taiwanese Depression Questionnaire with a cutoff score of ≥13,Citation45 yielding 26.9% positive screens.
We found that younger age significantly correlated with psychological distress, which was consistent with previous studies.Citation42,Citation46–Citation49 The differences based on the life stage revealed that younger patients were inclined to describe psychological distress and need help, nearly 2.1 times more likely than older patients.Citation49 We surmised that the relationship between distress and age is unlikely linear, but is associated with the obligations that emerged in different life phases. It appears that simultaneously working and looking after children dwelling at home when battling cancer in the meantime, as particularly young and middle-aged patients did, raises the demand for additional care.Citation49
Moreover, this study, in line with former reports,Citation39,Citation42 revealed that patients with head and neck cancer were more likely to have psychological distress than did those with leukemia, or colorectal or urologic cancer. Dysfunction of speech and articulation and facial disfigurement were the main reasons for the distress that set head and neck cancer patients apart from other cancer patients.Citation50
We also demonstrated that patients who had not received chemotherapy significantly correlated with psychological distress. The possible explanations are as follows: first, those having received chemotherapy may have benefited more from the inhibition of disease progress, which would result in low levels of psychological distress. Second, there was a decline in depression, anxiety, and the impact of the adverse effects of chemotherapy in patients with the passing of time because of the acceptance of the diagnosis and management.Citation51–Citation53
In a recent study, Kim et alCitation22 examined the prevalence and related factors of psychological distress in recently diagnosed cancer patients at a medical oncology unit in Korea. They demonstrated that a low educational level was related to psychological distress, which supports our finding that lower educational levels were possibly correlated with psychological distress. Possible explanation for the result mentioned earlier is lower educated people might have lower socioeconomic status, and might have more stressful life events and, thus render psychological distress.
Psychiatric disorders among cancer patients with significant psychological distress
We analyzed the psychiatric disorders among cancer inpatients with significant psychological distress. Past reports have indicated that major depressive disorder and adjustment disorder were prevalent in cancer patients.Citation54–Citation57 Approximately 15%–20% of cancer patients with psychiatric disorder were diagnosed with major depressive disorder, 65% with adjustment disorder, and ~10% with delirium.Citation54–Citation56,Citation58 Our results showed nearly equal percentages of patients with adjustment disorder and depressive disorder, at 39% and 34%, respectively. This finding implicated that 10%–30% of cancer inpatients have depressive disorder and need psychotropic and psychological combination treatment.
However, the real prevalence may have exceeded those results. We executed psychiatric assessments for nearly one-third of the inpatients who were recognized as having psychological distress and consequently referred to a psychiatrist. Previous data revealed that the referral percentage of cancer patients from oncologists to consultation-liaison psychiatrists was 4%–45%.Citation22,Citation59–Citation62 The possible reasons for the limited referral rate are a low level of psychological awareness among medical doctors, the stigma attached to psychiatric disease by clinicians, and the traditional idea that a clinician’s main mission is saving life rather than dealing with psychological distress. We could improve the referral rates through promotion in formal hospital meetings and offering website learning to the physicians. Furthermore, many cancer inpatients have severe psychosocial problems (eg, lack of social support). We could consult the social workers to conduct family interviews to overcome the lack of support.
In this study, we effectively overcame several methodological limitations of previous studies on the DT. The strength of this study was that the sample was larger and more varied in terms of cancer treatment and kinds of cancer than former studies. These advantages should allow a generalization of our results to other groups of patients. Nevertheless, several limitations should be kept in mind when interpreting these data. First, we did not analyze the total response rate for our regular procedures for screening distress because we could not ascertain the total number of patients who were initially excluded from the procedures. Second, our participants were from a general hospital in southern Taiwan, which may make generalization of our results difficult. Third, this was a retrospective study, so we were unable to probe into the patients’ psychiatric distress in the course of their cancer disease. Fourth, a number of inpatients with psychological distress were not referred to a psychiatrist, although we attempted to elevate the referral rate many times through promotion in formal hospital meetings and individually encouraging the physicians caring for the patients.
Conclusion
Our study indicated that cancer inpatients with psychological distress were more likely to be younger, have head and neck cancer, and have not received chemotherapy. The most common psychiatric disorder was adjustment disorder, followed by major depressive disorder. Early detection of psychological distress and prompt psychiatric consultation and management are very important for cancer inpatients.
Author contributions
YJC and YL originally conceived the study and drafted its funding application. All the authors planned, wrote, and edited this article and took joint responsibility for its contents. All the authors contributed to and approved the final report, and YL is the study guarantor. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The authors thank the medical staff at Kaohsiung Chang Gung Memorial Hospital for their continued support and services. This work had no specific funding.
Disclosure
The authors report no conflicts of interest in this work.
References
- National Comprehensive Cancer NetworkClinical Practice Guidelines in Oncology, Distress Management, Version 12016 Available from: https://www.nccn.org/professionals/physician_gls/pdf/distress.pdfAccessed June 28, 2016
- SkarsteinJAassNFossaSDSkovlundEDahlAAAnxiety and depression in cancer patients: relation between the Hospital Anxiety and Depression Scale and the European Organization for Research and Treatment of Cancer Core Quality of Life QuestionnaireJ Psychosom Res2000491273411053601
- ColleoniMMandalaMPeruzzottiGRobertsonCBredartAGoldhirschADepression and degree of acceptance of adjuvant cytotoxic drugsLancet200035692381326132711073026
- KissaneDBeyond the psychotherapy and survival debate: the challenge of social disparity, depression and treatment adherence in psychosocial cancer carePsychooncology20091811519097139
- PrietoJMAtalaJBlanchJRole of depression as a predictor of mortality among cancer patients after stem-cell transplantationJ Clin Oncol200523256063607116087949
- OnitiloAANietertPJEgedeLEEffect of depression on all-cause mortality in adults with cancer and differential effects by cancer siteGen Hosp Psychiatry200628539640216950374
- SchneiderSMoyerADepression as a predictor of disease progression and mortality in cancer patients: a meta-analysisCancer2010116133304 author reply 3304–330520564636
- MonahanPOChampionVRawlSWhat contributes more strongly to predicting QOL during 1-year recovery from treatment for clinically localized prostate cancer: 4-weeks-post-treatment depressive symptoms or type of treatment?Qual Life Res200716339941117091363
- ReichMLesurAPerdrizet-ChevallierCDepression, quality of life and breast cancer: a review of the literatureBreast Cancer Res Treat2008110191717674188
- RehseBPukropREffects of psychosocial interventions on quality of life in adult cancer patients: meta analysis of 37 published controlled outcome studiesPatient Educ Couns200350217918612781933
- CarlsonLEBultzBDBenefits of psychosocial oncology care: improved quality of life and medical cost offsetHealth Qual Life Outcomes20031812756059
- BultzBDCarlsonLEEmotional distress: the sixth vital sign in cancer careJ Clin Oncol200523266440644116155033
- National Comprehensive Cancer NetworkDistress management. Clinical practice guidelinesJ Natl Compr Canc Netw20031334437419761069
- MaXZhangJZhongWThe diagnostic role of a short screening tool – the distress thermometer: a meta-analysisSupport Care Cancer20142271741175524510195
- SchubartJREmerichMFarnanMStanley SmithJKauffmanGLKassRBScreening for psychological distress in surgical breast cancer patientsAnn Surg Oncol201421103348335325034820
- GaoWStarkDBennettMISiegertRJMurraySHigginsonIJUsing the 12-item General Health Questionnaire to screen psychological distress from survivorship to end-of-life care: dimensionality and item qualityPsychooncology201221995496121557386
- TraskPCAssessment of depression in cancer patientsJ Natl Cancer Inst Monogr200432809215263046
- VignaroliEPaceEAWilleyJPalmerJLZhangTBrueraEThe Edmonton Symptom Assessment System as a screening tool for depression and anxietyJ Palliat Med20069229630316629559
- MitchellAJKaarSCogganCHerdmanJAcceptability of common screening methods used to detect distress and related mood disorders-preferences of cancer specialists and non-specialistsPsychooncology200817322623617575565
- MitchellAJBaker-GlennEAParkBGrangerLSymondsPCan the distress thermometer be improved by additional mood domains? Part II. What is the optimal combination of Emotion Thermometers?Psychooncology201019213414019296461
- ShimEJShinYWJeonHJHahmBJDistress and its correlates in Korean cancer patients: pilot use of the distress thermometer and the problem listPsychooncology200817654855517957764
- KimSJRhaSYSongSKPrevalence and associated factors of psychological distress among Korean cancer patientsGen Hosp Psychiatry201133324625221601721
- RothAJKornblithABBatel-CopelLPeabodyEScherHIHollandJCRapid screening for psychologic distress in men with prostate carcinoma: a pilot studyCancer19988210190419089587123
- DonovanKAGrassiLMcGintyHLJacobsenPBValidation of the distress thermometer worldwide: state of the sciencePsychooncology201423324125025160838
- JacobsenPBDonovanKATraskPCScreening for psychologic distress in ambulatory cancer patientsCancer200510371494150215726544
- BoyesAD’EsteCCareyMLecathelinaisCGirgisAHow does the distress thermometer compare to the Hospital Anxiety and Depression Scale for detecting possible cases of psychological morbidity among cancer survivors?Support Care Cancer201321111912722618735
- TuinmanMAGazendam-DonofrioSMHoekstra-WeebersJEScreening and referral for psychosocial distress in oncologic practice: use of the distress thermometerCancer2008113487087818618581
- WangGLHsuSHFengACThe HADS and the DT for screening psychosocial distress of cancer patients in TaiwanPsychooncology201120663964621626611
- RecklitisCJBlackmonJEChangGScreening young adult cancer survivors for distress with the distress thermometer: comparisons with a structured clinical diagnostic interviewCancer2016122229630326457669
- Taiwanese Psycho-Oncology SocietyIntroduction of Distress Thermometer – Mandarin Version2016 Available from: http://www.tpos-society.org/Attache/News/1056.pdfAccessed August 26, 2016
- LeeCYChenH-WLiYCTangWRFangCKSuicide prevention in cancer careJ Intern Med Taiwan201122335343
- CYCRelationship among Degree of Psychological Distress, Demoralized Syndrome, Depression and Suicidal Ideation for Patients with Gynecologic Cancer in a Medical Center in Taiwan [MD thesis]TaiwanNational Taipei University of Nursing and Health Sciences2015
- FurukawaTGoldbergDPCultural invariance of likelihood ratios for the General Health QuestionnaireLancet1999353915256156210028994
- ChengTAA community study of minor psychiatric morbidity in TaiwanPsychol Med19881849539683270838
- ChongMYWilkinsonGValidation of 30- and 12-item versions of the Chinese Health Questionnaire (CHQ) in patients admitted for general health screeningPsychol Med19891924955052788292
- GesslerSLowJDaniellsEScreening for distress in cancer patients: is the distress thermometer a valid measure in the UK and does it measure change over time? A prospective validation studyPsychooncology200817653854717973237
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders4th edWashington, DCAmerican Psychiatric Association2000
- StefanekMEDerogatisLPShawAPsychological distress among oncology outpatients. Prevalence and severity as measured with the brief symptom inventoryPsychosomatics198728105305325375393432516
- ZaboraJBrintzenhofeSzocKCurbowBHookerCPiantadosiSThe prevalence of psychological distress by cancer sitePsychooncology2001101192811180574
- CarlsonLEAngenMCullumJHigh levels of untreated distress and fatigue in cancer patientsBr J Cancer200490122297230415162149
- GaoWBennettMIStarkDMurraySHigginsonIJPsychological distress in cancer from survivorship to end of life care: prevalence, associated factors and clinical implicationsEur J Cancer201046112036204420447824
- van ScheppingenCSchroeversMJSminkADoes screening for distress efficiently uncover meetable unmet needs in cancer patients?Psychooncology201120665566321381148
- TraskPCPatersonARibaMAssessment of psychological distress in prospective bone marrow transplant patientsBone Marrow Transplant2002291191792512080358
- OzalpECankurtaranESSoygurHGeyikPOJacobsenPBScreening for psychological distress in Turkish cancer patientsPsychooncology200716430431116909427
- TuCHHsuMCChiSCLinHYYenYCRoutine depression screening and diagnosing strategy for cancer inpatientsPsychooncology20142391057106724798464
- DegnerLFSloanJASymptom distress in newly diagnosed ambulatory cancer patients and as a predictor of survival in lung cancerJ Pain Symptom Manage19951064234317561224
- GilFGrassiLTravadoLTomamichelMGonzalezJRSouthern European Psycho-Oncology Study GroupUse of distress and depression thermometers to measure psychosocial morbidity among southern European cancer patientsSupport Care Cancer200513860060615761700
- GravesKDArnoldSMLoveCLKirshKLMoorePGPassikSDDistress screening in a multidisciplinary lung cancer clinic: prevalence and predictors of clinically significant distressLung Cancer200755221522417084483
- TuinmanMAVan NuenenFMHagedoornMHoekstra-WeebersJEDistress, problems and referral wish of cancer patients: differences according to relationship status and life phasePsychooncology201524669970425345693
- FramptonMPsychological distress in patients with head and neck cancer: reviewBr J Oral Maxillofac Surg2001391677011178847
- DecatCSde AraujoTCStilesJDistress levels in patients undergoing chemotherapy in BrazilPsychooncology201120101130113320740504
- Decat BergerotCCavalcanti Ferreira de AraujoTCAssessment of distress and quality of life of cancer patients over the course of chemotherapyInvest Educ Enferm201432221622425230032
- ZhangMPengLLiuWPhysical and psychological predictors of quality of life in Chinese colorectal cancer patients during chemotherapyCancer Nurs201538431232125159078
- DerogatisLRMorrowGRFettingJThe prevalence of psychiatric disorders among cancer patientsJAMA198324967517576823028
- MassieMJPrevalence of depression in patients with cancerJ Natl Cancer Inst Monogr200432577115263042
- AkechiTOkuyamaTSugawaraYNakanoTShimaYUchitomiYMajor depression, adjustment disorders, and post-traumatic stress disorder in terminally ill cancer patients: associated and predictive factorsJ Clin Oncol200422101957196515143090
- MitchellAJChanMBhattiHPrevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studiesLancet Oncol201112216017421251875
- HotopfMChidgeyJAddington-HallJLyKLDepression in advanced disease: a systematic review Part 1. Prevalence and case findingPalliat Med2002162819711969152
- KissaneDWSmithGCConsultation-liaison psychiatry in an Australian oncology unitAust N Z J Psychiatry19963033974048839952
- McCartneyCFCahillPLarsonDBLyonsJSWadaCYPincusHAEffect of a psychiatric liaison program on consultation rates and on detection of minor psychiatric disorders in cancer patientsAm J Psychiatry198914678989012742016
- GrassiLGrittiPRigatelliMGalaCPsychosocial problems secondary to cancer: an Italian multicentre survey of consultation-liaison psychiatry in oncology. Italian Consultation-Liaison GroupEur J Cancer200036557958510738121
- ShimizuKAkechiTOkamuraMUsefulness of the nurse-assisted screening and psychiatric referral programCancer200510391949195615770689
