Abstract
Background
Various personality traits mediate the association between childhood stress and depressive symptoms in adulthood. The aim of this study was to clarify the indirect effects of the experience of child maltreatment on depressive symptoms and appraisal of life events in adulthood through trait anxiety.
Subjects and methods
A total of 404 participants who were volunteer subjects from the community were studied using the following self-administered questionnaire surveys: Patient Health Questionnaire-9, which measures depressive symptoms; State-Trait Anxiety Inventory Form Y, which measures trait anxiety; the Child Abuse and Trauma Scale, which measures child maltreatment; and Life Experiences Survey, which measures negative and positive appraisal of adulthood life events.
Results
Structural equation modeling demonstrated that the experience of child maltreatment increased depressive symptoms in adulthood as well as the negative appraisal of life events in adulthood through an increase in trait anxiety. Furthermore, trait anxiety affected depressive symptoms in adulthood through its influence on the negative appraisal of adulthood life events. The following indirect effect was also significant: the experience of child maltreatment increased the negative appraisal of adulthood life events via trait anxiety and subsequently influenced adult depressive symptoms.
Limitations
The subjects of this study are volunteer subjects from the community including healthy people, and hence the results may not be generalizable to major depressive patients. Recall bias should be considered when interpreting the results. Because this study is a cross-sectional study, the causality between the experience of child maltreatment and depression is not clear.
Conclusion
This study suggests that trait anxiety may play a mediating role in the influence of the experience of child maltreatment on depressive symptoms in adulthood and negative appraisal of adulthood life events.
Introduction
Major depressive disorder (MDD) is a common psychiatric disorder, with a lifetime prevalence of 5%–17% of the general population.Citation1 The most recent Global Burden of Disease Study reported that MDD is the second leading cause of years lived with disability.Citation2 MDD is caused by the interaction of multiple factors, such as heredity, personality traits, experience of child maltreatment, parenting, and stressful adulthood life events.Citation3–Citation5 Previous studies pointed out that persons who were abused in childhood have a higher incidence of major depressive episodes in adulthood,Citation4 and patients with depression experienced more harmful events in childhood than healthy controls.Citation6 Because there is a long time between the experience of child stress and MDD in adulthood, it is assumed that there are multiple mediators between them.
Previously, we reported that affective temperament, a personality trait associated with depression, plays a major role in the effect of the experience of child maltreatment on adulthood depressive symptoms, as both a moderator and a mediator, in adult volunteer subjects from the community.Citation7,Citation8 In addition, affective temperament plays roles in the effects of the experience of child maltreatment on depressive symptoms and is a mediator of depressive symptoms in MDD patients.Citation9,Citation10 Neuroticism, which is another temperament, has been established as a risk factor for developing depression. High levels of neuroticism tend to induce the development of depressive episodes in response to stressful life events.Citation5 The quality of parenting, mediated by neuroticism, affects the severity of depressive symptoms in patients with MDD.Citation11 Our previous study indicated that neuroticism is also a mediator for the effects of the experience of child maltreatment and quality of parenting on adulthood depressive symptoms, as well as the negative appraisal of life events in volunteer subjects from the community.Citation12,Citation13 Therefore, several personality traits have been proposed as mediators for the effect of childhood stress on depression.
On the other hand, it is known that “trait anxiety” constitutes a public mental health problem.Citation14 A higher therapeutic response in depressive disorders is associated with increased age, longer treatment duration, higher resilience, and lower trait anxiety.Citation15 In addition, trait anxiety has been implicated as a vulnerability characteristic associated with the development of stress-induced depression.Citation16 Furthermore, in cardiac surgery patients, trait anxiety mediates the effect of stress exposure on postoperative posttraumatic stress disorder and depression.Citation17 Although trait anxiety is a personality trait that makes people more vulnerable to depression, it remains unclear whether trait anxiety is involved as a mediator in the effects of the experience of child maltreatment on adulthood depressive symptoms.
Therefore, the aim of this study was to clarify how three factors, namely, trait anxiety, adulthood life events, and the experience of child maltreatment, are associated with adulthood depressive symptoms in adult volunteer subjects from the community and whether the experience of child maltreatment has an indirect effect on depressive symptoms in adulthood and the appraisal of adulthood life events through trait anxiety. Consequently, we analyzed trait anxiety evaluated using the State-Trait Anxiety Inventory Form Y (STAI-Y),Citation18 child maltreatment measured using the Child Abuse and Trauma Scale (CATS),Citation19 adulthood life events assessed using the Life Experiences Survey (LES),Citation20 and demographic characteristics in volunteer subjects from the community, and analyzed the association between the above three causative factors and depressive symptoms by structural equation modeling (SEM).
Subjects and methods
Subjects
This research was part of a larger study, conducted from January to August 2014.Citation12–Citation14 We recruited volunteers by flyers and word of mouth and distributed the self-administered questionnaires to 853 Japanese adult volunteers. Of the 853 volunteers, 404 subjects (47.4%; 220 men, 184 women; age 42.3±11.9 years) agreed to participate in this study and provided complete responses to the questionnaires.
Subjects completed the self-administered questionnaire anonymously. Written informed consent was obtained from all of the subjects after giving the following explanations: 1) participation in this research and replies to the questions can be freely decided by individual judgment; 2) if they do not agree to participate in this research, they will not experience any disadvantages; 3) data of this research will be managed by making all data anonymous in a format which cannot identify individuals; and 4) personal information will not be leaked to the outside. In accordance with the Declaration of Helsinki, this study was conducted with approval from the ethics committee of Tokyo Medical University and Hokkaido University Hospital.
Questionnaires
Patient Health Questionnaire-9 (PHQ-9)
Spitzer et alCitation21 developed the PHQ-9, which is a self-administered questionnaire for the screening of major depressive episodes and the evaluation of the severity of depressive symptoms. The Japanese version was developed and its validity was substantiated by Muramatsu et al.Citation22 Major depressive episodes were diagnosed in two ways, by applying the PHQ-9 diagnostic algorithms and a summary score.Citation23 This study used a summary score for evaluating the severity of depressive symptoms. Specifically, the total score (0–27 points) of nine items of depressive symptoms in the previous 2 weeks using a 4-point Likert scale for each item were calculated (0–3, 0=not at all, 1=several days, 2=more than half the days, and 3=nearly every day).
State-Trait Anxiety Inventory Form Y
The STAI-Y is a 40-item self-reported measure of transient (state) and chronic (trait) anxiety symptoms.Citation18 The STAI-Y state anxiety section consists of 20 statements by which respondents assess how they feel on a 4-point scale (1=not at all, 2=somewhat, 3=moderately so, and 4=very much so) for each statement. The STAI-Y trait anxiety section consists of 20 statements by which respondents evaluate how they feel on a 4-point scale (1=almost never, 2=sometimes, 3=often, and 4=almost always). The STAI-Y state and trait scores range from 20 to 80.
Child Abuse and Trauma Scale
The CATS is a 38-item self-administered questionnaire to retrospectively evaluate adverse childhood experiences.Citation19 Tanabe, an author of the present manuscript, developed and validated the Japanese version of the CATS using the classical translation–back translation technique with the permission and confirmation of Dr Sanders.Citation24 Participants evaluate how frequently they had a particular abusive experience during their childhood and adolescence, using a 5-point scale (0=never, 1=rarely, 2=sometimes, 3=very often, and 4=always). There are three subscales, measuring the subjective reports of the following three aspects of adverse childhood experiences: neglect/negative home atmosphere, punishment, and sexual abuse. In the present study, the average score of 38 items were calculated as the total score, and the average scores of each subscale were also calculated.
Life Experiences Survey
The LES is a 57-item self-administered questionnaire. The respondents state the major events that they experienced in the previous year.Citation20 The Japanese version of the LES was used in this study.Citation7 The respondents evaluated the intensity of the psychological impact of the event using a 7-point scale, ranging from extremely negative (−3) to extremely positive (+3). The positive change score summing the effect of positive events and the negative change score summing the effect of negative events were calculated.
Construction of the structural equation model
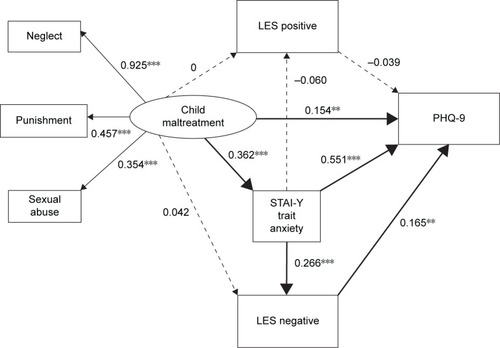
A structural equation model was constructed using the PHQ-9 scores, STAI-Y trait anxiety scores, LES positive change scores, LES negative change scores, and CATS subscale scores (). The average subscale scores of the CATS (sexual abuse, neglect, and punishment) were the observed variables in the CATS, and the latent variable “child maltreatment” was comprised of these subscales. In this model, the experience of child maltreatment, trait anxiety, LES positive and negative change scores (positive and negative appraisal of life events) were considered to directly affect depressive symptoms in adulthood. Furthermore, the experience of child maltreatment was considered to indirectly influence depressive symptoms and the evaluation of life events in adulthood through trait anxiety as a potential mediating factor.
Figure 1 Results of covariance structure analysis in the structural equation model with child maltreatment, trait anxiety (STAI-Y trait anxiety), negative and positive appraisal of life events in adulthood (LES negative and LES positive), and depressive symptoms (PHQ-9) in 404 adult volunteer subjects from the community.
Abbreviations: LES, Life Experiences Survey; STAI-Y, State-Trait Anxiety Inventory Form Y.
The rationale of this structural equation model was based on the temporal characteristics of the questionnaires used in this study, ie, the CATS for child maltreatment evaluates adverse experiences in the childhood and teen years; STAI-Y trait anxiety evaluates the general tendency to feel anxiety as a nonpathological personal trait; the LES evaluates life events during the previous year; and the PHQ-9 evaluates depressive symptoms in the previous 2 weeks. A previous prospective, longitudinal community study showed that the average age of onset of anxiety disorders was earlier than that of depressive disorders and that most anxiety disorders were primary disorders that substantially increase the risk for secondary depression.Citation25
In addition, this study used the latent variable “child maltreatment” instead of the CATS total score because the intention was to clarify the subtypes of child maltreatment that are associated with depressive symptoms. Furthermore, our previous studies showed that neglect, rather than punishment and sexual abuse, is the most influential factor for MDD and depressive symptoms in adult volunteers from the community.Citation7,Citation9,Citation10
Data analysis
The Spearman rank correlation coefficient and the Mann– Whitney U test (SPSS version 24, SPSS Inc., Chicago, IL, USA) were used to calculate correlations between variables and to compare variables between two categories of demographic characteristics (eg, men vs women), respectively. Furthermore, stepwise multiple regression analysis (backward elimination) using PHQ-9 as the dependent variable was performed. Demographic characteristics and scores of the questionnaire data, age, sex, current marital status, presence of offspring, living status, years of education, employment status, comorbidity of physical disease, CATS (neglect, punishment, and sexual abuse), LES change scores (positive and negative) and STAI-Y trait anxiety scores were used as independent variables.
The structural equation model was analyzed by covariance structure analysis robust maximum likelihood estimation using Mplus version 7.3 (Muthén & Muthén, Los Angeles, CA, USA). There is no absolute standard to judge the fitness of the model by covariance structure analysis. For this reason, the model was comprehensively evaluated by combining several indices of goodness-of-fit, such as root mean square error of approximation (RMSEA), Tucker–Lewis index (TLI), and comparative fit index (CFI). A CFI>0.95, a TLI>0.95, and an RMSEA<0.08 indicate an acceptable fit; and a CFI>0.97, a TLI>0.97, and an RMSEA<0.05 indicate a good fit.Citation26 All of the coefficients were standardized and shown (with a maximum of +1 and a minimum of −1) for covariance structure analysis. A P-value of <0.05 was considered to indicate a statistically significant difference between two groups.
Results
Influence of the demographic characteristics of subjects and questionnaire data on total PHQ-9 scores
Demographic and questionnaire data on 404 subjects and their effects on total PHQ-9 scores are shown in . Age, sex, current marital status, and the presence of offspring were significantly associated with total PHQ-9 scores. On the other hand, years of education, employment status, living status, and comorbidity of physical disease were not associated with PHQ-9 summary scores. The total CATS score, average scores of the CATS subscales (neglect, punishment, and sexual abuse), STAI-Y traits and state anxiety scores, and LES negative change score significantly correlated with PHQ-9 summary scores.
Table 1 Background characteristics, PHQ summary, CATS, STAI-Y, and LES scores of the subjects, and their correlation with and effects on PHQ-9 scores
Stepwise multiple regression analysis (backward elimination) of PHQ-9 summary scores
shows the results of stepwise multiple regression analysis (backward elimination) of PHQ-9 summary scores. We chose 14 independent factors with the PHQ-9 summary score as a dependent variable. Ten independent variables were excluded from this model. Four independent variables, namely, STAI-Y trait anxiety, CATS neglect score, LES negative change score, and age significantly predicted PHQ-9 summary scores (adjusted R2=0.466, F=82.892, P<0.001). As variance inflation factors were approximately 1, multi-collinearity was denied in this multiple regression analysis.
Table 2 Results of stepwise multiple regression analysis of PHQ-9
Correlation (ρ) between CATS subscale scores, LES positive and negative change scores, and STAI-Y state and trait anxiety scores
As shown in , the STAI-Y trait anxiety score, total CATS score and subscale scores, and LES negative change score were positively correlated with depressive symptoms. Furthermore, the correlation between total CATS scores and subscale scores, positive and negative change scores of LES, and STAI-Y state and trait anxiety scores were analyzed (). The STAI-Y trait anxiety score significantly correlated with total CATS score and subscale scores, and positive and negative score changes of the LES, and STAI-Y state anxiety scores.
Table 3 Correlation (ρ) between subscale scores of the CATS, the LES positive and negative scores, and the STAI-Y state and trait scores
Analysis of the structural equation model
In our structural equation model, the CATS, LES, and STAI-Y trait anxiety scores affect PHQ-9 summary scores in a complex manner, and this model was analyzed by covariance structure analysis. We treated scores of the three CATS subscales (sexual abuse, neglect, and punishment) as the observed variables, and “child maltreatment” as the latent variable (). The goodness-of-fit of this structural equation model was good (χ2 statistic P=0.445, CFI=1.000, TLI=1.001, and RMSEA=0.000). This model explained 47.8% of the variability in depressive symptoms (R2=0.478).
Direct effects
Child maltreatment had significant positive effects on PHQ-9 scores (severity of depressive symptoms) and STAI-Y trait anxiety scores. However, child maltreatment had no significant effect on LES negative and positive change scores. STAI-Y trait anxiety scores had significant positive effects on LES negative change scores and PHQ-9 scores, but not on LES positive change scores. Negative change scores of LES increased depressive symptoms, but positive change scores of LES did not affect depressive symptoms. Among the subscales of the CATS, the path coefficient from “child maltreatment” to neglect subscale scores was largest.
Indirect effects
Child maltreatment indirectly increased PHQ-9 scores through increasing STAI-Y trait anxiety scores (standardized coefficient 0.199, P<0.001). Child maltreatment indirectly increased negative change scores of the LES through increasing the STAI-Y trait anxiety score (standardized coefficient 0.096, P<0.001). Furthermore, the STAI-Y trait anxiety score indirectly increased PHQ-9 via a positive effect on negative change scores of the LES (standardized coefficient 0.044, P<0.05). Finally, child maltreatment indirectly and significantly increased the PHQ-9 summary score (standardized coefficient 0.016, P<0.05) via a positive effect on the two combined paths of STAI-Y trait anxiety and LES negative change scores. However, no indirect effect via the positive change score of the LES was observed in this model.
Discussion
To our knowledge, this is the first study demonstrating that the experience of child maltreatment indirectly affects depressive symptoms through enhanced trait anxiety, a potential mediator, as well as having a direct effect. In this study, the experience of child maltreatment, trait anxiety, and negative appraisal of life events directly influenced depressive symptoms in 404 volunteer adult subjects from the community. These results suggest that trait anxiety may be a mediator for the effects of child maltreatment on depressive symptoms and the negative appraisal of life events, but not the positive appraisal of life events.
Several studies reported that experiencing child maltreatment, such as physical and sexual abuse, and total adverse childhood experiences increased trait anxiety in university students and patients with anxiety disorder.Citation27,Citation28 Moreover, we reported that childhood parental bonding affected adulthood trait anxiety indirectly through self-esteem; trait anxiety was decreased by high parental care and increased by parental overprotection, respectively.Citation14 The results of earlier studies agree with the results of the present study, indicating a close association between adverse childhood experiences and trait anxiety, which is a characteristic of vulnerability and a risk factor of depression.Citation16,Citation17,Citation29
Neuroticism, which is a personality trait, has been established as a risk factor for developing major depression. High neuroticism tends to induce the development of depressive episodes in response to stressful life events.Citation5 Our previous studies suggested that neuroticism is a mediator for the effects of the experience of child maltreatment and quality of parenting on depressive symptoms in adulthood and the negative appraisal of life events.Citation12,Citation13 Neuroticism shares some characteristics with trait anxietyCitation29 and both are moderately and positively associated.Citation30 As in the case of neuroticism, individuals with a high anxiety trait show hyper responsiveness to threatening stimuli, as well as attentional biases that facilitate the detection of threats and aversiveness.Citation31 Negative life event appraisals were significantly associated with trait anxiety in this study and in the original study that developed the LES, whereas positive life event appraisals were not.Citation20 The SEM results of our present study suggest that trait anxiety increases the vulnerability to stress, leading to more severe depressive symptoms.
In the present study, among the subscales of child maltreatment, a major role of neglect on depressive symptoms in adulthood was found compared with sexual abuse and punishment. In the results of multiple regression analysis of PHQ-9 summary scores in this study, neglect on CATS, but not sexual abuse or punishment, was a significant predictor of depressive symptoms. The coefficient of neglect from the latent variable of “child maltreatment” in the SEM was the largest among the three subscales of the CATS, consistent with our previous studies.Citation7,Citation13 Similarly, a high neglect score on the CATS significantly predicted an MDD diagnosis in the comparison between healthy controls and patients with MDD.Citation9 Because our findings were obtained from studies using the CATS and Japanese subjects, measurement invariance should be confirmed. However, several studies using a different abuse questionnaire (the Childhood Trauma Questionnaire) and subjects of different countries also demonstrated that emotional abuse and neglect have a closer association with depressive symptoms than other types of abuse.Citation32,Citation33 Hence, neglect is considered to be the most influential factor for depressive symptoms among several types of child maltreatment.
Interestingly, trait anxiety, negative life event appraisal, and their combination may play a mediating role in the effects of the experience of child maltreatment on depressive symptoms. In this study, the experience of child maltreatment showed a significant indirect effect on adulthood depressive symptoms through pathways including increased trait anxiety, increased negative life event appraisals, and both, which might reflect vulnerability to stress. A similar phenomenon was reported for neuroticism.Citation13 Consistent with our present and previous studies, other researchers reported that an increased exposure to negative life events in adulthood partly mediates the association between childhood adversities and depression in adulthood.Citation34
The experience of child maltreatment induces long-lived hyperactivity of corticotropin-releasing factor systems or the hypothalamic–pituitary–adrenal (HPA) axis and hypofunction of the hippocampus.Citation35,Citation36 Interestingly, hyperactivity of the HPA axis is also reported in increased trait anxiety and may be a vulnerability factor for stress-induced depression.Citation16,Citation31 Amygdalar activation analyzed by functional MRI is observed in both anxiety disorders and major depressionCitation37,Citation38 and is increased by the experience of child maltreatment and trait anxiety.Citation39,Citation40 These biological changes associated with child maltreatment and increased trait anxiety are suggested to be the neural basis for the onset of depression.
The experience of child maltreatment is an etiological factor for MDD. However, how child maltreatment causes MDD is unknown. Our model suggests that high trait anxiety induced by the experience of child maltreatment may increase sensitivity to stress, leading to the onset of depression. Consistent with this idea, child maltreatment is associated with the comorbidity of anxiety disorders in major depression,Citation41 and most anxiety disorders are primary disorders that substantially increase the risk for secondary depression.Citation25 Clinically, the psychological and social intervention for reducing trait anxiety as well as reducing experiences of child maltreatment may prevent major depression. This study proposes a clinical suggestion that we should positively evaluate the combination of child maltreatment and trait anxiety in depressive patients.
There are some limitations to this study. The first is that the subjects of this study are volunteer subjects from the community including healthy people, and hence the results may not be generalizable to MDD patients. The second limitation is that this study used self-written questionnaires that rely on the subjects’ memories. The CATS used to measure child maltreatment is a questionnaire in which subjects retrospectively recall experiences in childhood, and hence may be affected by recall bias. The third limitation is that because this study is a cross-sectional study, the causality between the experience of child maltreatment and depression is not clear. Santor et alCitation42 showed that a personality trait was relatively stable and largely influenced by the baseline trait, but a small change in a personality trait was caused by depressive symptoms. Therefore, there is the possibility that reverse causality may be established from our data but the reversed effect might be relatively small. The fourth limitation is that 47.4% of volunteers agreed to participate in this study and provided a complete response, which might lead to selection bias. The fifth limitation is that we did not investigate the association of medications or particular comorbidities.
Conclusion
The present study indicates that trait anxiety may play a mediating role in the effects of the experience of child maltreatment on depressive symptoms and the negative appraisal of life events in adulthood. Longitudinal studies are necessary to clarify temporal changes in the associations observed between these variables. These findings suggest the close association between anxiety and depression and suggest that interventions to reduce cases of child maltreatment will decrease the incidence of trait anxiety in adulthood, leading to the prevention of MDD and depressive symptoms.
Author contributions
TI designed the study and wrote the protocol. YU and TI collected and analyzed the data. All authors contributed to data analysis and drafting and critically revising the manuscript. In addition, all authors gave final approval for the present version of the manuscript to be published and agreed to be accountable for all aspects of the work.
Acknowledgments
This work was partly supported by a Grant-in-Aid for Scientific Research (no 16K10194, to T. Inoue) from the Japanese Ministry of Education, Culture, Sports, Science and Technology, the Research and Development Grants for Comprehensive Research for Persons with Disabilities from the Japan Agency for Medical Research and Development under grant no JP18dk0307060 (to T Inoue), and SENSHIN Medical Research Foundation (to T Inoue).
Disclosure
JM has received personal compensation from Otsuka Pharmaceutical, Eli Lilly, Astellas, and Meiji Yasuda Mental Health Foundation and grants from Pfizer. MI has received personal compensation from Otsuka Pharmaceutical, Pfizer, Eli Lilly, Mitsubishi Tanabe Pharma, Mochida Pharmaceutical, Meiji Seika Pharma, Janssen Pharmaceutical, Takeda Pharmaceutical Company, MSD, Dainippon Sumitomo Pharma, and Eisai; grants from Otsuka Pharmaceutical, Eli Lilly, Eisai, Shionogi, Takeda Pharmaceutical, MSD, and Pfizer; and is a member of the advisory board of Meiji Seika Pharma. IK has received personal compensation from Astellas, Chugai Pharmaceutical, Daiichi Sankyo, Dainippon Sumitomo Pharma, Eisai, Eli Lilly, Janssen Pharmaceutical, Kyowa Hakko Kirin, Meiji Seika Pharma, MSD, Nippon Chemiphar, Novartis Pharma, Ono Pharmaceutical, Otsuka Pharmaceutical, Pfizer, Tanabe Mitsubishi Pharma, Shionogi, and Yoshitomiyakuhin; and has received research grants from AbbVie GK, Asahi Kasei Pharma, Astellas, Boehringer Ingelheim, Chugai Pharmaceutical, Daiichi Sankyo, Dainippon Sumitomo Pharma, Eisai, Eli Lilly, GlaxoSmithKline, Kyowa Hakko Kirin, Meiji Seika Pharma, MSD, Novartis Pharma, Ono Pharmaceutical, Otsuka Pharmaceutical, Pfizer, Takeda Pharmaceutical, Tanabe Mitsubishi Pharma, Shionogi, and Yoshitomiyakuhin; and is a member of the advisory board of Dainippon Sumitomo Pharma and Tanabe Mitsubishi Pharma. TI has received personal compensation from GlaxoSmithKline, Mochida Pharmaceutical, Asahi Kasei Pharma, and Shionogi; grants from Astellas; and grants and personal compensation from Otsuka Pharmaceutical, Dainippon Sumitomo Pharma, Eli Lilly, Eisai, Mitsubishi Tanabe Pharma, Pfizer, AbbVie GK, MSD, Yoshitomiyakuhin, Takeda Pharmaceutical, and Meiji Seika Pharma; and is a member of the advisory boards of GlaxoSmithKline, Pfizer, Eli Lilly, Mochida Pharmaceutical, and Mitsubishi Tanabe Pharma. The authors report no other conflicts of interest in this work.
References
- SadockBSadockVKaplanRPKaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry11th edPhiladelphiaLippincott Williams & Wilkins Inc2014
- Global Burden of Disease Study 2013 CollaboratorsGlobal, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013Lancet2015386999574380026063472
- AlloyLBAbramsonLYSmithJMGibbBENeerenAMRole of parenting and maltreatment histories in unipolar and bipolar mood disorders: mediation by cognitive vulnerability to depressionClin Child Fam Psychol Rev200691236416718583
- CaspiASugdenKMoffittTEInfluence of life stress on depression: moderation by a polymorphism in the 5-HTT geneScience2003301563138638912869766
- KendlerKSKuhnJPrescottCAThe interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depressionAm J Psychiatry2004161463163615056508
- KesslerRCMageeWJChildhood adversities and adult depression: basic patterns of association in a US national surveyPsychol Med19932336796908234575
- NakaiYInoueTTodaHThe influence of childhood abuse, adult stressful life events and temperaments on depressive symptoms in the nonclinical general adult populationJ Affect Disord201415810110724655773
- NakaiYInoueTChenCThe moderator effects of affective temperaments, childhood abuse and adult stressful life events on depressive symptoms in the nonclinical general adult populationJ Affect Disord201518720321026342173
- TodaHInoueTTsunodaTThe structural equation analysis of childhood abuse, adult stressful life events, and temperaments in major depressive disorders and their influence on refractorinessNeuropsychiatr Dis Treat2015112079209026316754
- TodaHInoueTTsunodaTAffective temperaments play an important role in the relationship between childhood abuse and depressive symptoms in major depressive disorderPsychiatry Res201623614214726708440
- EnnsMWCoxBJLarsenDKPerceptions of parental bonding and symptom severity in adults with depression: mediation by personality dimensionsCan J Psychiatry200045326326810779883
- OnoYTakaesuYNakaiYThe influence of parental care and overprotection, neuroticism and adult stressful life events on depressive symptoms in the general adult populationJ Affect Disord2017217667228391110
- OnoKTakaesuYNakaiYAssociations among depressive symptoms, childhood abuse, neuroticism, and adult stressful life events in the general adult populationNeuropsychiatr Dis Treat20171347748228243100
- ShimuraATakaesuYNakaiYChildhood parental bonding affects adulthood trait anxiety through self-esteemCompr Psychiatry201774152028086151
- MinJALeeNBLeeCULeeCChaeJHLow trait anxiety, high resilience, and their interaction as possible predictors for treatment response in patients with depressionJ Affect Disord20121371–3616922244377
- SandiCRichter-LevinGFrom high anxiety trait to depression: a neurocognitive hypothesisTrends Neurosci200932631232019409624
- KokLSepMSVeldhuijzenDSTrait anxiety mediates the effect of stress exposure on post-traumatic stress disorder and depression risk in cardiac surgery patientsJ Affect Disord201620621622327479534
- SpielbergerCDManual for the State-Trait Anxiety Inventory STAI (form Y)Palo AltoConsulting Psychologists Press1983
- SandersBBecker-LausenEThe measurement of psychological maltreatment: early data on the child abuse and trauma scaleChild Abuse Negl19951933153239278731
- SarasonIGJohnsonJHSiegelJMAssessing the impact of life changes: development of the life experiences surveyJ Consult Clin Psychol1978465932946701572
- SpitzerRLKroenkeKWilliamsJBValidation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health QuestionnaireJAMA1999282181737174410568646
- MuramatsuKMiyaokaHKamijimaKThe patient health questionnaire, Japanese version: validity according to the mini-international neuropsychiatric interview-plusPsychol Rep20071013 Pt 195296018232454
- InoueTTanakaTNakagawaSUtility and limitations of PHQ-9 in a clinic specializing in psychiatric careBMC Psychiatry2012127322759625
- TanabeHOzawaSGotoKPsychometric properties of the Japanese version of the Child Abuse and Trauma Scale (CATS)The 9th Annual Meeting of the Japanese Society for Traumatic Stress StudiesKobe. JapaneseMarch 6, 2010
- WittchenHUKesslerRCPfisterHLiebMWhy do people with anxiety disorders become depressed? A prospective-longitudinal community studyActa Psychiatr Scand Suppl20004061423
- Schermelleh-EngelKMoosbruggerHMüllerHEvaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measuresMPR online2003822374
- ManciniCvan AmeringenMMacmillanHRelationship of childhood sexual and physical abuse to anxiety disordersJ Nerv Ment Dis199518353093147745385
- ReiserSJMcmillanKAWrightKDAsmundsonGJAdverse childhood experiences and health anxiety in adulthoodChild Abuse Negl201438340741324011493
- BishopSForsterSTrait anxiety, neuroticism, and the brain basis of vulnerability to affective disorderArmonyJVuilleumierPThe Cambridge Handbook of Human Affective NeuroscienceCambridgeCambridge University Press2013553574
- GondaXFountoulakisKNJuhaszGAssociation of the s allele of the 5-HTTLPR with neuroticism-related traits and temperaments in a psychiatrically healthy populationEur Arch Psychiatry Clin Neurosci2009259210611318806915
- WegerMSandiCHigh anxiety trait: a vulnerable phenotype for stress-induced depressionNeurosci Biobehav Rev201887273729407523
- GibbBEChelminskiIZimmermanMChildhood emotional, physical, and sexual abuse, and diagnoses of depressive and anxiety disorders in adult psychiatric outpatientsDepress Anxiety200724425626317041933
- LeeSWBaeGYRimHDMediating effect of resilience on the association between emotional neglect and depressive symptomsPsychiatry Investig20181516269
- KorkeilaJVahteraJNabiHChildhood adversities, adulthood life events and depressionJ Affect Disord20101271–313013820569993
- FrodlTO’KeaneVHow does the brain deal with cumulative stress? A review with focus on developmental stress, HPA axis function and hippocampal structure in humansNeurobiol Dis201352243722426398
- HeimCNemeroffCBThe role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studiesBiol Psychiatry200149121023103911430844
- ShelineYIBarchDMDonnellyJMOllingerJMSnyderAZMintunMAIncreased amygdala response to masked emotional faces in depressed subjects resolves with antidepressant treatment: an fMRI studyBiol Psychiatry200150965165811704071
- GingnellMFrickAEngmanJCombining escitalopram and cognitive-behavioural therapy for social anxiety disorder: randomised controlled fMRI trialBr J Psychiatry2016209322923527340112
- IndovinaIRobbinsTWNúñez-ElizaldeAODunnBDBishopSJFear-conditioning mechanisms associated with trait vulnerability to anxiety in humansNeuron201169356357121315265
- van HarmelenALvan TolMJDemenescuLREnhanced amygdala reactivity to emotional faces in adults reporting childhood emotional maltreatmentSoc Cogn Affect Neurosci20138436236922258799
- CyranowskiJMSchottLLKravitzHMPsychosocial features associated with lifetime comorbidity of major depression and anxiety disorders among a community sample of mid-life women: the SWAN mental health studyDepress Anxiety201229121050105722930404
- SantorDABagbyRMJoffeRTEvaluating stability and change in personality and depressionJ Pers Soc Psychol1997736135413629418283
