Abstract
Moyamoya disease (MMD) is a rare cerebrovascular disorder characterized by the progressive narrowing and occlusion of the intracranial internal carotid arteries, leading to the formation of abnormal collateral vessels. MMD primarily affects the cerebrovascular system, and evidence suggests it is associated with various neuropsychiatric outcomes. This manuscript aims to provide an overview of the current understanding of MMD, including its epidemiology, pathophysiology, clinical manifestations, and diagnosis. Furthermore, it explores the emerging research on the neuropsychiatric sequelae of MMD, such as cognitive impairment, psychiatric disorders, and quality of life. The manuscript concludes with the challenges in managing MMD-related neuropsychiatric outcomes and potential avenues for future research.
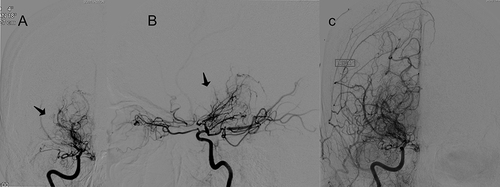
Moyamoya disease (MMD) is a rare cerebrovascular disorder characterized by the progressive narrowing and occlusion of the intracranial internal carotid arteries, leading to the formation of abnormal collateral vessels.Citation1 MMD can progress to the complete occlusion of the intracranial internal carotid arteries (ICA) and/or the proximal portion of the anterior cerebral arteries (ACA) and middle cerebral arteries (MCA), most commonly resulting in ischemic neurovascular events such as arterial ischemic stroke (AIS) and transient ischemic attacks (TIA).Citation1 Posterior cerebral artery (PCA) involvement is less common, but has worse prognosis.Citation2 Hemorrhagic stroke is another less common outcome due to the formation of fragile, dilated collateral vessels. MMD was first characterized by Suzuki and Takaku on digital subtraction angiography in 1969 when they coined the term moyamoya meaning “puff of smoke” in Japanese, to describe the angiographic appearance of vessels.Citation3
MMD has the highest prevalence in East Asia, but some cases are found in North America, especially among individuals of East Asian descent.Citation4 The prevalence rates are highest in Japan and South Korea, 10.9/100,000 and 16.1/100,000, respectively.Citation5,Citation6 Europe had the lowest prevalence of MMD, and the prevalence rates in the United States varied by region.Citation7 Large scale epidemiological analysis of MMD in the United States is quite limited, but one study that analyzed 2280 admissions of moyamoya estimated a prevalence of 0.57/100,000 cases per year.Citation8 The disease affects the population in a bimodal age distribution, impacting individuals ages 10 and 30–40.Citation4 Data suggests a female predominance, but exact ratios varied among countries and regions. The estimated female-to-male disease ratios among Japanese and white European groups are 2:1 and 2.9:1, respectively.Citation7
Evidence suggests the association of MMD with various neuropsychiatric conditions. This is an overview of the current understanding of MMD, including its epidemiology, pathophysiology, clinical manifestations, and diagnosis. It explores the emerging research on the neuropsychiatric sequelae of MMD, such as cognitive impairment, psychiatric disorders, and quality of life. The manuscript concludes by discussing the challenges in managing MMD-related neuropsychiatric outcomes and potential avenues for future research.
Natural History and Neuropsychiatric Manifestations of Moyamoya Disease
Cerebral ischemic events including TIAs and ischemic infarcts are the most common presentation in MMD among pediatric and adult patients. These events are often precipitated by hyperventilation which leads to vasoconstriction and hypoperfusion. In pediatric patients, intellectual disability also occurs due to stroke and chronic hypoxemia.Citation4 Additionally, adults may present with hemorrhagic stroke from the rupture of fragile moyamoya collateral vessels.Citation9
Seizures are common complications of ischemic and hemorrhagic events. Patients also report migraine headaches. Ischemia may also evoke focal neurological impairments including weakness, numbness, difficulty speaking, and visual disturbances.Citation4 Finally, MMD may present with neuropsychiatric symptoms such as mood change, anxiety, and depression.Citation10
Neuropsychiatric Manifestations of Moyamoya Disease
Cognitive impairment is one of the most common MMD-related neuropsychiatric outcomes and occurs in 31% to 79% of adult MMD patients.Citation11 In a comprehensive analysis of 61 adults with MMD, Chan et alCitation11 found that cognitive impairment occurred in 57% of the patients along with non-negligible impacts on performance IQ, executive function, speed of information processing, and visual memory. One prospective studyCitation12 found that MMD patients with a history of stroke only experienced more severe short-term memory decline for words and complex number operations than their “asymptomatic” counterparts.
Neuropsychiatric outcomes vary considerably between patients with adult MMD and pediatric MMD. Psychiatric symptoms in pediatric MMD are infrequent and the current evidence is limited to case reports.Citation13 Those psychiatric encompass conditions like schizophrenia, acute transient psychosis, and mania. Additionally, cognitive impairment, learning disabilities, and attention deficits may be observed in some pediatric MMD patients.Citation13 Children with diminished performance IQ profiles due to MMD who subsequently underwent revascularization surgery experienced significant improvement in their IQ and cognitive function, whereas adults did not.Citation11 The mechanism behind this phenomenon is not fully understood, but it could be due to superior synaptic plasticity in children.Citation14
MMD is associated with psychiatric disorders such as depression, anxiety, and psychoticism, particularly in adult patients.Citation15 A study found anxiety in 32.7% and depression in 29.5% of MMD patients, with higher rates in females. After revascularization surgery, 70% had no change in depression, 19% improved, and 11% worsened.Citation16 Notably, MMD patients often have decreased quality of life due to their neuropsychiatric outcomes. Depression with dysexecutive cognitive syndrome and mental disorders (OCD, psychoticism, and impaired physical and emotional role function) diminish MMD patients’ QoL.Citation15 Clinicians utilize well-known psychiatric assessments and batteries, but there is no established clinical standard for assessing these symptoms.
The literature suggests that many patients experience a neuropsychiatric decline due to chronic cerebral hypoperfusion rather than cerebral infarction or hemorrhage.Citation11 An imaging study even found that the degree of hypoperfusion correlates with the severity of cognitive impairment.Citation15 Chronic hypoperfusion leads to changes in brain chemistry and ischemic changes which result in cognitive impairment. However, after the initial period of cognitive decline, MMD patients’ cognitive function remains relatively stable long-term regardless of their stroke history.Citation11 A cross-sectional studyCitation10 found that Korean MMD patients had higher levels of anxiety and depression than Korean and Dutch patients who previously had strokes and German patients with unruptured aneurysms. MMD patients within one year of diagnosis experience greater depression than patients diagnosed for one year or more. These findings suggest that these psychological phenomena are partially anticipatory due to MMD patients’ fears of hemorrhage or infarction.
Diagnosis of Moyamoya Disease
Upon clinical manifestation of MMD, radiological evaluation is required for a definitive diagnosis. MMD is diagnosed when intracranial arterial stenosis or occlusion is appreciated on imaging along with compensatory moyamoya vessels.Citation7 However, diagnosing MMD can be challenging due to possible confusion with atherosclerotic disease. Distinguishing adult MMD from intracranial atherosclerotic disease is especially challenging in the early stages when the moyamoya vessels are underdeveloped and unidentified radiologically.Citation7 Recently, imaging techniques have improved, allowing for increased recognition of MMD cases. Various imaging modalities can diagnose MMD and MMS; digital subtraction angiography (DSA) remains the gold standard.Citation17 A definitive diagnosis of MMD is typically established based on the two characteristic findings of intracranial arterial stenosis or occlusion and the development of moyamoya vessels. The diagnosis is confirmed using conventional catheter angiography or non-invasive imaging techniques such as MRI and MRA ( and ).Citation17 In cases where various systemic diseases and conditions accompany these two characteristic findings, moyamoya syndrome (MMS) is diagnosed instead of MMD.Citation7 Proper diagnosis also becomes more challenging in later-stage disease as characterized by Suzuki, when the moyamoya vessels begin to disappear.Citation3
Figure 1 A 35-year-old female presented with headaches. Imaging work was done which included T2 MRI (A) and MRA (B) which showed bilateral internal carotid artery tapering (blue arrows) with near-complete occlusion at the carotid termini and presence of skull base collateral vessels, diagnostic of Moyamoya syndrome. On the right, the supraclinoid internal carotid artery shows loss of signal below the posterior communicating artery, with collateral vessels at the skull base. The left displays decreased caliber at the supraclinoid portion with no signal at the carotid terminus. Both sides show collateral vessels at the skull base, indicating a compensatory response to the occlusions.
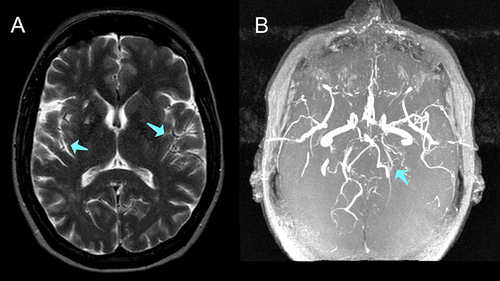
Figure 2 DSA images demonstrates a “puff of smoke” sign (A and B) (black arrows) and reveal unilateral moyamoya syndrome with unilateral disease on the right internal carotid artery which is nearly occluded (C), hypervascularity of the lenticulostriate vessels, and transdural collateral supply, indicative of advanced disease progression.
Kronenburg et alCitation18 presented a comprehensive list of neuropsychological tests used to assess cognitive function in adults and children with Moyamoya disease. They organized the tests by cognitive domains according to Lezak, including general intelligence, memory, working memory, language, attention and executive functioning, processing speed, and visuospatial functioning. For adults, intelligence tests included standardized ones like the National Adult Reading Test and Raven’s Advanced Progressive Matrices, while for children assessments include developmental age, verbal IQ, and performance IQ. Other adult tests include the Rey Auditory Verbal Learning Test for memory, Digit Span for working memory, and the Stroop test for processing speed. Child tests included the Peabody Picture Vocabulary Test for language and the Beery Visual Motor Integration for visuospatial abilities. Notably, when patients exhibited signs of depression in this study, the Beck Depression Inventory was added to the test battery for a more comprehensive evaluation. The wide-ranging list of tests allows for a well-structured approach to evaluating cognitive abilities among Moyamoya patients and enables clinicians to determine cognitive profiles in individuals with Moyamoya disease. Another study recommends the use of two representative concise cognitive assessment batteries: the Neurobehavioral Cognitive Status Examination (Cognistat) and the Frontal Assessment Battery (FAB).Citation19
Pathophysiology of Moyamoya Disease and Its Neuropsychiatric Manifestations
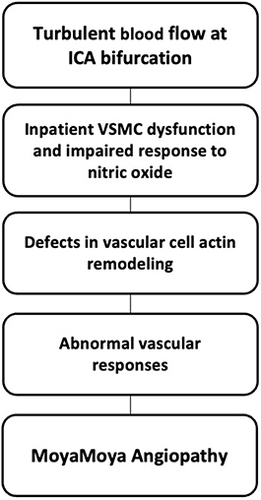
Down syndrome, neurofibromatosis type 1, and several other genetic mutations are associated with the genetic predisposition of MMS.Citation20 Sixteen genes and several pathways, including the Ras and MAPK, Notch, DNA repair, inflammasome, chromatin remodeling, actin remodeling, coagulation, and nitric oxide (NO) pathways, are involved in moyamoya angiopathy ().Citation7 Literature suggests that RNF213 is the primary gene associated with moyamoya angiopathy. RNF213, also known as mysterin, regulates endothelial function and angiogenesis. Specifically, clustering in the E3 domain disrupts the ubiquitination activity of RNF213.Citation7 RNF213 is a susceptibility gene for MMD in East Asian and White populations, but only distinct variants pose a significantly increased risk for moyamoya angiopathy. Furthermore, acquired risk factors such as inflammatory processes and immune dysregulation contribute to the development and progression of the disease. Patients with MMD often have elevated bacterial and viral titers compared with healthy individuals suggesting a potential role in triggering these pathological changes.Citation7 The pathophysiology of RNF213 gene-related moyamoya angiopathy is detailed in .Citation21–24
Table 1 Pathophysiology of RNF213 Gene Related Moyamoya Angiopathy
Neuroimaging Findings and Neuropsychiatric Outcomes in Moyamoya Disease
MMD is classically categorized into six Suzuki stages,Citation2 which are based on the results of the DSA. DSA is considered the gold standard for diagnosing MMD due to its detailed visualization of cerebral vessels.Citation14 Tt provides dynamic imaging of collateral flow and cursory information on perfusion, which can provide valuable insight into ischemic risk. Advancements in imaging techniques integrating DSA, MRI, and cerebrovascular reserve capacity have led to the recently validated Berlin grading system which has proven superior to the traditional Suzuki staging system.Citation20,Citation21 This allows clinicians to evaluate the hemodynamic status while stratifying the individual risks associated with surgery, as opposed to basing clinical decisions strictly on cerebrovascular morphology.Citation20,Citation21 Other researchers have suggested that quantitative MRI-based methods and Doppler may be beneficial in MMD diagnosis and evaluation. Both imaging techniques evaluate cerebral perfusion without requiring contrast media or exposing patients to ionizing radiation.Citation17
Recent studies have compared MMD-related neuropsychiatric outcomes to various cerebral regions and their respective vascular networks. One imaging study revealed that about two-thirds of MMD infarcts occur in the MCAs, approximately one-third occur in the ACAs, and only 3.0% - 4.5% occur in the PCAs, without significant difference in the laterality of the cerebral infarct regions.Citation15 One study found that the degree of cerebral damage in the frontal lobe correlated with paranoia, which is an otherwise rare outcome.Citation16 Another imaging study found that depression in MMD patients is significantly associated with damage to the right non-dominant hemisphere in the middle cerebral artery region.Citation15
A retrospective German study sought to evaluate the relationship between hypoperfusion or cerebral infarction with quality of life, depression, and other neuropsychiatric outcomes in 67 preoperative patients with adult-onset moyamoya angiopathy.Citation15 The findings revealed dysexecutive cognitive syndrome (DCS), defined as two or more abnormal neuropsychiatric tests, in 41.8% of the patients. DCS was significantly more common in patients whose neuroimaging demonstrated hypoperfusion after acetazolamide administration or had evidence of MCA infarction on MRI. The presence of DCS significantly increased the odds of patients having depression. Additionally, patients with signs of hypoperfusion or infarct in either MCA experienced higher rates of psychosis. Neuroimaging is a critical component in evaluating MMD patients for neuropsychiatric outcomes and further studies should be conducted comparing the effect of impaired hemodynamics on the brain.Citation15
Neuropsychiatric Management of Moyamoya Disease
Managing neuropsychiatric outcomes in MMD involves preventing stroke recurrence, improving cognitive function, and providing psychotherapy and psychosocial support. Surgical revascularization is considered the best treatment option for symptomatic patients to prevent cerebral infarction and restore perfusion and reserve capacity.Citation16 Direct artery-to-artery anastomosis and indirect arterio-synangiosis are the two main revascularization techniques, but combination surgical procedures also exist.Citation16 A meta-analysis of 18 studies showed that direct bypass resulted in a greater extent of revascularizations on angiography compared to indirect bypass. Additionally, indirect bypass was associated with a higher incidence of stroke recurrence compared to the direct and combined bypass treatment.Citation7 Traditionally, direct or combined bypass is used in adults, while indirect or combined bypass is applied in children.Citation25 A different study revealed that, in the long term, the outcomes following indirect revascularization are notably superior to direct and combined methods in adults.Citation26 Additionally, it demonstrated that combined and indirect approaches were significantly more effective than direct revascularization in pediatric patients. Indirect revascularization improves blood flow to multiple vascular territories, decreases the risk of hyperperfusion syndrome, and is a less complicated surgical procedure, thereby decreasing risks of complications. Another study demonstrated comparable safety and efficacy of both techniques.Citation27 There is currently no consensus on which method is ideal, and clinical decisions should be made on an individual basis.
In hemodynamically stable, and asymptomatic or mildly symptomatic patients, the optimal treatment strategy remains unclear. One retrospective study found that the use of antiplatelet agents was statistically insignificant in terms of symptomatic cerebral infarction, hemorrhage, and improvement of ischemic symptoms. However, subgroup analyses within the antiplatelet group demonstrated that a longer duration of antiplatelet medication significantly improved ischemic symptoms.Citation28 A retrospective Korean study with 25,978 newly diagnosed MMD patients found that antiplatelet therapy decreased mortality. Cilostazol was the most strongly associated with overall reduced mortality. Cilostazol’s pleiotropic effects of not only preventing platelet aggregation but also inducing vasodilation are thought to contribute to a greater reduction in patient mortality.Citation29 Therefore, specific antiplatelet agents, specifically cilostazol, may be considered for the management of MMD symptoms in candidates ineligible for surgery. In children with poor operative risk or relatively mild disease, The American Heart Association suggests antiplatelet agents such as LMWH, UFH, and Warfarin.Citation30
A third domain of treatment for MMD patients targets their neuropsychiatric symptoms. Psychotherapy, psychosocial support, physical therapy, and psychotropic medications all play a crucial role in helping patients cope with the emotional and psychological impact of the disease.Citation16
Future Directions and Challenges in Moyamoya Disease
Future directions in MMD research include improving the diagnosis, management, and outcomes for patients. Prospective studies addressing long-term neuropsychiatric outcomes and how they relate to disease progression are crucial, especially in asymptomatic patients who remain undiagnosed for too long. This will help identify predictive factors for neuropsychiatric sequelae and track long-term outcomes of the disease and its treatments to guide clinical decision-making. While DSA is the primary imaging technique to diagnose MMD, the optimal system to characterize and identify MMD, especially early, remains unclear. The application of genetic screening and the use of biomarkers such as basic fibroblast growth factor (bFGF) in CSF may provide a predictive role to assist in early diagnosis and characterizing the status of angiogenesis post-revascularization.Citation31,Citation32
Further investigation into the relationship between cognitive status and advanced neuroimaging is critical. Each neuroimaging technique has benefits and limitations and significant progress has been made in improving our characterization of MMD. However, a standardized grading system for MMD is still lacking. One meta-analysis explains the potential impact of multimodal image fusion techniques on characterizing disease status.Citation20 This will also help determine the effects of early revascularization and determine treatment protocols to improve neuropsychiatric outcomes and diminish infarct events.
Conclusion
Neuropsychiatric outcomes of MMD can significantly impact patients’ quality of life, with cognitive impairment being common. Pediatric and adult MMD may differ in cognitive outcomes after revascularization surgery. Genetic factors, including the RNF213 gene variant, and acquired risk factors contribute to the disease’s development. Managing neuropsychiatric outcomes involves preventing stroke recurrence, improving cognitive function, and providing psychotherapy and support.
Disclosure
Dr David Altschul is a consultant for Microvention, Stryker, and Cerenovus. The authors report no other conflicts of interest in this work.
References
- Unda SR, Antoniazzi AM, Fluss R, et al. Ethnic-Associated Phenotype Variations in Moyamoya Cerebrovascular Outcomes. Cerebrovasc Dis. 2022:1–7. doi:10.1159/000528055
- Zhao M, Zhang D, Wang S, et al. Posterior circulation involvement in pediatric and adult patients with moyamoya disease: a single center experience in 574 patients. Acta Neurol Belg. 2018;118(2):227–233. doi:10.1007/s13760-017-0844-1
- Suzuki J, Takaku A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969;20(3):288–299. doi:10.1001/archneur.1969.00480090076012
- Kim JS. Moyamoya Disease: epidemiology, Clinical Features, and Diagnosis. J Stroke. 2016;18(1):2–11. doi:10.5853/jos.2015.01627
- Zhang H, Zheng L, Feng L. Epidemiology, diagnosis and treatment of moyamoya disease. Exp Ther Med. 2019;17(3):1977–1984. doi:10.3892/etm.2019.7198
- Scott RM, Smith ER. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009;360(12):1226–1237. doi:10.1056/NEJMra0804622
- Ihara M, Yamamoto Y, Hattori Y, et al. Moyamoya disease: diagnosis and interventions. Lancet Neurol. 2022;21(8):747–758. doi:10.1016/S1474-4422(22)00165-X
- Starke RM, Crowley RW, Maltenfort M, et al. Moyamoya disorder in the United States. Neurosurgery. 2012;71(1):93–99. doi:10.1227/NEU.0b013e318253ab8e
- Kim JE, Kim KM, Kim JG, et al. Clinical features of adult moyamoya disease with special reference to the diagnosis. Neurol Med Chir. 2012;52(5):311–317. doi:10.2176/nmc.52.311
- Yang YS, Ryu GW, Yeom I, Shim KW, Choi M. Stress and mood of adults with moyamoya disease: a cross-sectional study. Nurs Health Sci. 2020;22(3):795–802. doi:10.1111/nhs.12729
- Chan E, Gal AM, Van Harskamp N, et al. Long-term study of the cognitive profile of Moyamoya Disease in adults. J Stroke Cerebrovasc Dis. 2023;32(6):107064. doi:10.1016/j.jstrokecerebrovasdis.2023.107064
- He S, Duan R, Liu Z, et al. Characteristics of cognitive impairment in adult asymptomatic moyamoya disease. BMC Neurol. 2020;20(1):322. doi:10.1186/s12883-020-01898-8
- Mohapatra S, Sahoo AJ. Neuropsychiatric manifestations in a child with moyamoya disease. J Neurosci Rural Pract. 2016;7(2):331–332. doi:10.4103/0976-3147.176198
- Malone LA, Felling RJ. Pediatric Stroke: unique Implications of the Immature Brain on Injury and Recovery. Pediatr Neurol. 2020;102:3–9. doi:10.1016/j.pediatrneurol.2019.06.016
- Haas P, Fudali M, Wang SS, et al. Quality of life impairment in adult Moyamoya patients-preoperative neuropsychological assessment and correlation to MRI and H215O PET findings. Neurosurg Rev. 2022;45(2):1533–1541. doi:10.1007/s10143-021-01660-9
- Richards M, Grzenda A, Nelson E, Gitlin M. Psychiatric Comorbidity in Moyamoya Disease and Preliminary Guidelines For Treatment. AJP. 2019;176(4):269–274. doi:10.1176/appi.ajp.2018.18040404
- Li J, Jin M, Sun X, et al. Imaging of Moyamoya Disease and Moyamoya Syndrome: current Status. J Comput Assist Tomogr. 2019;43(2):257–263. doi:10.1097/RCT.0000000000000834
- Kronenburg A, Deckers PT, Van Den Berg E, et al. The profile of cognitive impairment and hemodynamic compromise in moyamoya: a single-center prospective cohort study. J Neurosurgery. 2023;138(1):173–184. doi:10.3171/2022.3.JNS212844
- Nakamizo A, Amano T, Michiwaki Y, et al. Long-Term Neurocognitive Outcomes in Patients with Adult Moyamoya Disease. World Neurosurg. 2018;119:e441–e448. doi:10.1016/j.wneu.2018.07.179
- Santoro JD, Lee S, Wang AC, et al. Increased Autoimmunity in Individuals With Down Syndrome and Moyamoya Disease. Front Neurol. 2021;12:724969. doi:10.3389/fneur.2021.724969
- Tanigawara T, Yamada H, Sakai N, Andoh T, Deguchi K, Iwamura M. Studies on cytomegalovirus and Epstein-Barr virus infection in Moyamoya disease. Clin Neurol Neurosurgery. 1997;99:S225–S228. doi:10.1016/S0303-8467(97)00049-8
- Otten EG, Werner E, Crespillo-Casado A, et al. Ubiquitylation of lipopolysaccharide by RNF213 during bacterial infection. Nature. 2021;594(7861):111–116. doi:10.1038/s41586-021-03566-4
- Thery F, Martina L, Asselman C, et al. Ring finger protein 213 assembles into a sensor for ISGylated proteins with antimicrobial activity. Nat Commun. 2021;12(1):5772. doi:10.1038/s41467-021-26061-w
- Miller R, Unda SR, Holland R, Altschul DJ. Western Moyamoya Phenotype: a Scoping Review. Cureus. 2021. doi:10.7759/cureus.19812
- Esposito G, Sebök M, Amin-Hanjani S, Regli L. Cerebral Bypass Surgery: level of Evidence and Grade of Recommendation. Acta Neurochir Suppl. 2018;129:73–77. doi:10.1007/978-3-319-73739-3_10
- Macyszyn L, Attiah M, Ma TS, et al. Direct versus indirect revascularization procedures for moyamoya disease: a comparative effectiveness study. J Neurosurg. 2017;126(5):1523–1529. doi:10.3171/2015.8.JNS15504
- Naamani KE, Chen CJ, Jabre R, et al. Direct Versus Indirect Revascularization for Moyamoya: a Large Multicenter Study. J Neurol Neurosurg Psychiatry. 2023. doi:10.1136/jnnp-2022-329176
- Pang CH, Cho WS, Kang HS, Kim JE. Benefits and risks of antiplatelet medication in hemodynamically stable adult moyamoya disease. Sci Rep. 2021;11(1):19367. doi:10.1038/s41598-021-99009-1
- Seo W, Kim J, Choi E, et al. Association of Antiplatelet Therapy, Including Cilostazol, With Improved Survival in Patients With Moyamoya Disease in a Nationwide Study. JAHA. 2021;10(5):e017701. doi:10.1161/JAHA.120.017701
- Roach ES, Golomb MR, Adams R, et al. Management of stroke in infants and children: a scientific statement from a Special Writing Group of the American Heart Association Stroke Council and the Council on Cardiovascular Disease in the Young. Stroke. 2008;39(9):2644–2691. doi:10.1161/STROKEAHA.108.189696
- Malek AM, Connors S, Robertson RL, Folkman J, Scott M. Elevation of Cerebrospinal Fluid Levels of Basic Fibroblast Growth Factor in Moyamoya and Central Nervous System Disorders. Pediatr Neurosurg. 1997;27(4):182–189. doi:10.1159/000121249
- Fang YC, Wei LF, Hu CJ, Tu YK. Pathological Circulating Factors in Moyamoya Disease. IJMS. 2021;22(4):1696. doi:10.3390/ijms22041696