Abstract
Aripiprazole is widely used in the treatment of schizophrenia and bipolar disorders. Although antipsychotics generally have hypotensive effects, two cases were identified that demonstrated hypertension during the switch from other antipsychotics to aripiprazole. The hypertensive state of these patients recovered after switching back to other antipsychotics, and these cases suggest that aripiprazole may lead to hypertension.
Introduction
Hypotension is a known effect of atypical antipsychotics. In addition, the prevalence of orthostatic hypotension in the elderly is estimated to be between 5% and 33% and increases with age.Citation1 Orthostatic hypotension is a common side effect of a number of medications, including antipsychotic drugs, and a major contributing factor to the occurrence of falls with adverse consequences, such as bone fractures, injuries, functional decline, dependency, and death. Furthermore, the extent to which antipsychotic drugs cause hypotension differs, and low-potency conventional antipsychotics and clozapine are among the more problematic. However, there is little information on acute hypertension resulting from antipsychotic drugs.
Aripiprazole is a potent (high-affinity) partial dopamine D2 agonist, a serotonin 5-HT1A agonist and a 5-HT2A antagonist.Citation2 It acts as a functional antagonist of D2 receptors under hyperdopaminergic conditions but exhibits functional agonistic properties under hypodopaminergic conditions.Citation3 Here, two cases of acute hypertension during the switch from other antipsychotics to aripiprazole are reported.
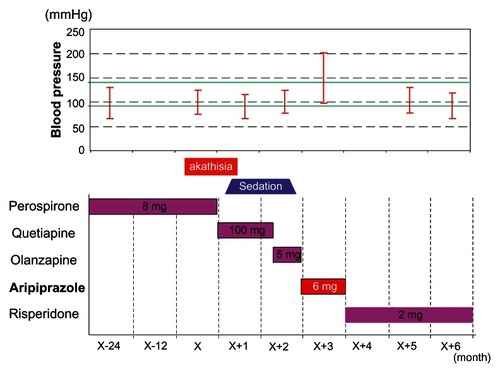
Case one
This patient was a 69-year-old woman with a 35-year history of schizophrenia. Her primary symptoms included auditory hallucinations, persecution mania, and self-talking. Her mental condition had been maintained with 2 mg/day of risperidone or 8–16 mg/day of perospirone for several years. Hypertension (systolic blood pressure > 180 mmHg) had developed 2 years previously and had been treated with a salt reduction policy and amlodipine at 5 mg/day. As a result, her blood pressure was controlled, and amlodipine was discontinued after 1 year. Due to akathisia, perospirone at 8 mg/day was changed to quetiapine at 100 mg/day or olanzapine at 5 mg/day; however, these drugs were withdrawn because of sedation. Thus, aripiprazole was initiated, but she suffered from dizziness, headache, and anacatesthesia as well as hypertension (200/110 mmHg). Thus, aripiprazole was changed to risperidone at 2 mg/day, and her blood pressure immediately dropped to 130/80 mmHg. The clinical course is summarized in .
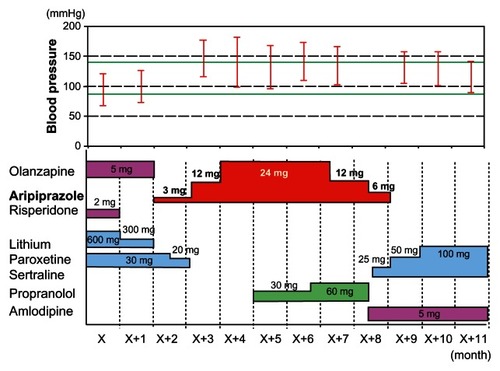
Case two
This patient was a 63-year-old man with a 9-year history of bipolar disorders. His primary symptoms included depressed mood, insomnia, appetite loss, concentration difficulty, and suicidal ideation. Manic episodes were also observed 2 years previously. He was diagnosed with hypertension (systolic blood pressure > 180 mmHg) 1 year previously and treated with a salt reduction policy and nifedipine at 10 mg/day. Consequently, his blood pressure was controlled, and nifedipine was discontinued after 3 months of treatment. His mental status was depressed with lithium treatment at 600 mg/day, paroxetine at 30 mg/day and olanzapine at 5 mg/day. Because of persistent depressive episodes, olanzapine at 5 mg/day was switched to aripiprazole at 3 mg/day. When the dose of aripiprazole escalated to 24 mg/day, his blood pressure increased to 180/90 mmHg with headache, and he was inarticulate. Although his hypertension was treated with amlodipine at 5 mg/day and propranolol at 60 mg/day, his blood pressure did not change. However, after aripiprazole withdrawal, his blood pressure dropped to 147/100 mmHg. The clinical course is summarized in .
Discussion
In the two cases presented here, hypertension after aripiprazole initiation but recovery after aripiprazole discontinuation was observed. Based on these clinical courses, it was concluded that the hypertension worsened due to aripiprazole, although withdrawal effects of previous antipsychotics cannot be ruled out.
Antipsychotics are known to cause the metabolic syndrome of insulin resistance, hyperlipidemia, and hypertension. Thus, addressing blood pressure as well as glycemia and lipid levels is an important step in the management of patients taking aripiprazole. In addition, according to the product information, the most frequently reported adverse reaction in clinical trials was headache (Otsuka Pharmaceutical Co, Ltd, Tokyo, Japan). Headache could have been a symptom of hypertension. In fact, the patients experienced headaches while having hypertension.
The dopamine receptor in vascular smooth muscle participates in vasodilatation, but the possibility that aripiprazole causes vascular smooth muscle to shrink as an antagonist under conditions in which dopamine is superabundant and high blood pressure is induced has been hypothesized. However, there is no D2 receptor in vascular smooth muscle, although there are D1 receptors. Because aripiprazole has extremely low affinity for the D1 receptor, it is unlikely that the high blood pressure observed with aripiprazole was mediated through the D1 receptor.
Although Hirose et al reported that aripiprazole acts as an antagonist for the 5-HT2A receptor,Citation4 Davies et al indicated that aripiprazole is a partial agonist for 5-HT2A.Citation5 Because the 5-HT2A receptor participates in the contraction of vascular smooth muscle, the possibility that vascular smooth muscle shrank as a result of aripiprazole acting as an agonist for 5-HT2A and inducing a rise in blood pressure has been hypothesized. The involvement of α-1A adrenergic receptors cannot be ruled out because aripiprazole has high affinity for α-1A adrenergic receptors,Citation6 which is related to malignant hypertension.Citation7 In addition, nitric oxide is known to suppress blood pressure. An in vitro study using brain macrophages has suggested that aripiprazole inhibits nitric oxide production from microglial cells.Citation8 Therefore, suppression of nitric oxide by aripiprazole may result in the patient’s hypertension.
However, only four reports have demonstrated high blood pressure induced by aripiprazole. Borras et al reported hypertension (220/110 mmHg) and tachycardia during aripiprazole treatment at 30 mg/day in a schizophrenic patient, which disappeared after aripiprazole discontinuation and propranolol administration.Citation9 Pitchot and Ansseau indicated that the addition of 5 mg of aripiprazole to 150 mg of venlafaxine in a patient with major depressive disorder led to hypertension (200/110 mmHg) and that aripiprazole discontinuation led to normalized blood pressure within 48 hours.Citation10 Hsiao et al showed high blood pressure (220/110 mmHg), headache, and dizziness after treatment with 90 mg of duloxetine and 5 mg/day of aripiprazole in a depressed patient.Citation11 Moreover, the administration of nifedipine and ramipril did not have an antihypertensive effect, and blood pressures were normalized with a reduction in aripiprazole from 5 mg/day to 2.5 mg/day. In addition, Bat-Pitault and Delorme reported hypertension (190/110 mmHg) in an adolescent patient, which was most likely induced by aripiprazole.Citation12 Although Pitchot and Ansseau and Hsiao et al discussed the influence of a concomitant drug,Citation10,Citation11 case one in the current report received aripiprazole only, and high blood pressure developed after aripiprazole. Therefore, it is not likely that the influence of the concomitant drug induced hypertension. Pitchot and Ansseau suggested the association with a prior history of cardiovascular disease, including coronary disease,Citation10 and the two cases in the current report also revealed a history of hypertension. Therefore, blood pressure variation must be carefully monitored when administering aripiprazole to patients with a previous history of cardiovascular disease.
Conclusion
This report presented two cases demonstrating high blood pressure after aripiprazole initiation, although blood pressures were normalized following aripiprazole interruption. Although the mechanism underlying the rise in blood pressure remains unclear, careful monitoring of blood pressure variations when administering aripiprazole to patients previously treated for high blood pressure is necessary.
Disclosure
The authors report no conflicts of interest in this work.
References
- VerhaeverbekeIMetsTDrug-induced orthostatic hypotension in the elderly: avoiding its onsetDrug Saf19971721051189285201
- JordanSKoprivicaVChenRTottoriKKikuchiTAltarCAThe antipsychotic aripiprazole is a potent, partial agonist at the human 5-HT1A receptorEur J Pharmacol2002441313714012063084
- FujikawaMNagashimaMInoueTYamadaKFurukawaTPartial agonistic effects of OPC-14597, a potential antipsychotic agent, on yawning behavior in ratsPharmacol Biochem Behav19965349039098801596
- HiroseTUwahodoYYamadaSMechanism of action of aripiprazole predicts clinical efficacy and a favourable side-effect profileJ Psychopharmacol200418337538315358981
- DaviesMAShefflerDJRothBLAripiprazole: a novel atypical antipsychotic drug with a uniquely robust pharmacologyCNS Drug Rev200410431733615592581
- ShapiroDARenockSArringtonEAripiprazole, a novel atypical antipsychotic drug with a unique and robust pharmacologyNeuropsychopharmacology20032881400141112784105
- FuMLHerlitzHWallukatGFunctional autoimmune epitope on α1-adrenergic receptors in patients with malignant hypertensionLancet19943448938166016637527885
- KatoTMizoguchiYMonjiAInhibitory effects of aripiprazole on interferon-γ-induced microglial activation via intracellular Ca2+ regulation in vitroJ Neurochem2008106281582518429930
- BorrasLConstantELEytanAHugueletPHypertension and aripiprazoleAm J Psychiatry200516212239216330611
- PitchotWAnsseauMAripiprazole, hypertension, and confusionJ Neuropsychiatry Clin Neurosci2010221123E3320160240
- HsiaoYLChenSJShenTWChangCHChenSTAripiprazole augmentation induced hypertension in major depressive disorder: a case reportProg Neuropsychopharmacol Biol Psychiatry201135130530621111018
- Bat-PitaultFDelormeRAripiprazole and hypertension in adolescentsJ Child Adolesc Psychopharmacol200919560160219877990