Abstract
Leptin is a hormone with significant effects on the brain, both at the cellular level and cognitive level. This study aimed to establish the association between leptin levels and delirium in a Colombian elderly population. 115 patients older than 60 years were included. Leptin was measured by enzyme-linked immunosorbent assay after overnight fasting and Mini-Mental State Examination and Confusion Assessment Method (CAM) tests were employed. Delirium was diagnosed using CAM in 23.48% of patients, being most frequent in men. There were no significant differences in hematology and renal test values between patients with delirium and those without delirium, but cerebrovascular diagnoses were more frequent in patients with delirium. No correlation with any specific medication was found, but patients with delirium had a higher number of comorbidities and medications. Leptin levels were significantly lower in patients with delirium and correlated negatively with the number of diagnoses and medications, but not with age, gender, body mass index, or hematology and renal test results. Leptin levels may have a role in the pathophysiological process of delirium and low leptin could be a useful clinical biomarker to establish risk in elderly patients given the association with delirium.
Keywords:
Introduction
Elderly patients usually present with comorbidities that frequently include psychiatric disorders, which increase the risk of complications in this population. Delirium is one of the most common disorders that appear to be associated with a number of pathologic conditions in this group of patients.Citation1,Citation2 However, according to different sources, there is a marked variability in the frequency of this disorder (14% to 80% of hospitalized patients).Citation3 This is due to differences in the diagnostic criteria and in the populations evaluated in these studies.Citation4,Citation5
Delirium is characterized by a cognitive dysfunction with an acute onset and a transient and fluctuating course,Citation6 which are the main factors used to differentiate delirium from other causes of dementia.Citation7,Citation8 Other signs that support this diagnosis are lack of attention, disorganized thinking and altered levels of consciousness.Citation9 Delirium is associated with orthopedic, cardiovascular and infectious diseases, cancer, diabetes, trauma, surgeries, anemia, dehydration and use of cholinergic medications, among others.Citation10,Citation11 Elderly patients are the most affected, with a higher rate of morbidity and mortality.Citation2 Delirium is associated with longer hospital stays, increased mortality rates, chronic cognitive compromise and a greater economic burden on the elderly inpatients.Citation12–Citation14 For these reasons, multiple efforts have been undertaken to identify biomarkers that can help elucidate the pathophysiology of delirium and improve the strategies of patient treatment.
Leptin is a hormone with broad effects on several neurotransmitter systems and on a number of neural functions.Citation15,Citation16 This 16 kD protein is produced mainly by white adipose tissueCitation17 and is the key regulator of body weightCitation18 via its effects on the hypothalamic arcuate nucleus. It acts on diverse processes, including immune regulation and energy homeostasis,Citation19 modulation of the reproductive hormone axis, and the growth of several cells and tissues.Citation20 The leptin receptor (LR) belongs to the cytokine receptor family and although it has 6 isoforms, only the b isoform, LRb, has an intracellular domain and therefore the capacity to induce a signaling response.Citation21 LRb is associated with the activation of JAK2, a family of kinases characterized by dual sites of action. JAK2 in turn activates STAT3, a promoter of transcription.Citation22 Leptin receptors are broadly expressed in the brain,Citation23,Citation24 and it has been shown that leptin can affect cognitive performance in both humansCitation25–Citation27 and rodents.Citation28,Citation29 Furthermore, low leptin levels have been associated with certain disorders, including depression,Citation30,Citation31 Alzheimer’s disease,Citation32 borderline personality disorder,Citation33 and obsessive-compulsive disorder,Citation34 all of which are associated with cognitive or/and emotional deficits.
To date, there have been no studies on the relationship between leptin and delirium; therefore, this study explored this association in elderly patients hospitalized in the Hospital Universitario San Jorge in Pereira, Colombia.
Methods
This study included 115 patients acutely hospitalized in the Hospital Universitario San Jorge (Pereira, Colombia) without regard to the reason for hospitalization or the ward in which they were admitted. All the patients were older than 60 years. Informed consent was obtained from the patients or from proxies in case of cognitive impairment, with the approval of the Bioethics Committee of Universidad Tecnológica de Pereira, under and the guidance of the Alzheimer’s Association.Citation35 This study was conducted in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki).Citation36
All of the patients were evaluated using the Mini-Mental State Examination (MMSE), to rule out dementia due to other causes, and the Confusion Assessment Method (CAM), which is the most common and simple scale for delirium diagnoses.Citation37,Citation38 These tests were given within 24 hours of hospitalization by advanced medical students, physicians, or psychiatry residents, who were trained extensively by an experienced psychiatrist. Those patients with scores ≤ 13 in MMSE were excluded from the study; this cut-off was chosen because of previous research results in a Latin American population, which found that it defined dementia prevalence similar to that determined using the 10/66 Dementia Research Group Protocol,Citation39 developed to avoid educational and cultural biases in population-based studies in developing countries.Citation40 Patients with a positive CAM were classified as potential patients with delirium; however the diagnosis only was established if they met the DSM-IV criteria.Citation41 Blood samples were obtained from all of the admitted patients the next morning after admission following overnight fasting, and the serum was stored at −20°C until leptin levels were measured. Leptin was determined by an enzyme-linked immunosorbent assay (ELISA) technique using a commercially available kit (Diasource Immunoassays SA, Leptin-EASIA KAP2281, Nivelles, Belgium). The clinical records of all patients included in this study were revised to include the hematology test data. Each patient’s weight and height was measured to determine the body mass index (BMI).
Statistical analyses were performed using the SPSS version 16.0 (SPSS Inc, Chicago, IL, USA) and GraphPad Prism version 6.0 (GraphPad Software Inc, La Jolla, CA, USA) software. The results are shown as the mean ± standard error of the mean (SEM). Significant differences were determined using an unpaired Student’s t-test, correlation analyses were performed using a non-parametric test and a P-value < 0.05 was considered to be significant. Association between variables was established employing a Chi-squared test. Multivariate logistic regression models were used to adjust for characteristics shown to be associated with leptin and the presence of delirium in bivariate analyses (P < 0.05).
Results
The age range of the patients, who were all mestizo, was between 60 and 91 years, with a mean of 73.2 ± 7.6 years; 42.6% of them were women. Delirium was diagnosed in 23.48% (n = 27) of the patients. There were no differences in the age ranges and means in patients with delirium and those without delirium. With regard to gender, there was a significantly greater (P < 0.0001) proportion of men in the group of patients with delirium (88%) compared to the group of patients without delirium (50%). The two groups of patients did not differ in hemoglobin values, hematocrit, leukocyte count, platelet count, and creatinine and ureic nitrogen values (). BMI was also similar in both groups (25.46 ± 5.45 in patients with delirium and 25.13 ± 6.97 in patients without delirium, no significant differences). shows a summary of clinical diagnoses in patients with delirium and those without delirium. There was a significant difference in the proportion of patients with a cerebrovascular diagnosis in the patients with delirium, but there was no difference in the distribution by other diagnoses or by any medication (data not shown) between the two groups of patients. However, patients with delirium showed an increase in the number of comorbidities as well as in the consumption of medications, and these differences were significant compared to patients without delirium ().
Figure 1 Comparison between number of diagnoses (A) and number of medications (B) in patients without delirium and patients with delirium.
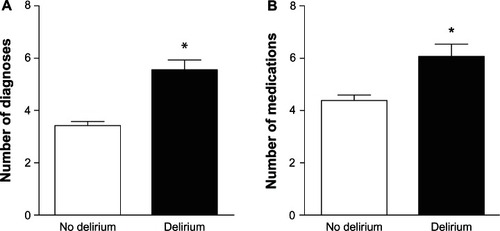
Table 1 Laboratory tests in patients without delirium and patients with delirium
Table 2 Summary of diagnoses in patients without delirium and patients with delirium, grouped according to the type of pathology
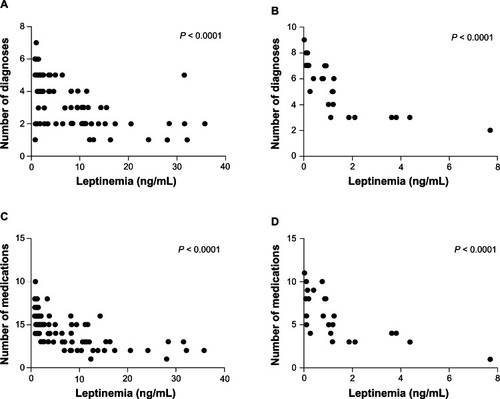
Leptin levels ranged between 0.79 ng/mL and 35.77 ng/mL, with a mean of 6.16 ng/mL. Leptin levels were significantly lower in patients with delirium compared to those without it () and this difference remained after adjustment for number of diagnoses and number of medications. Although leptin levels did not correlate with age, gender, BMI, or laboratory tests in either of the patient groups (data not shown), they correlated negatively with the number of diagnoses and the number of medications in both groups ().
Figure 2 Comparison between leptin levels in patients without delirium and patients with delirium.
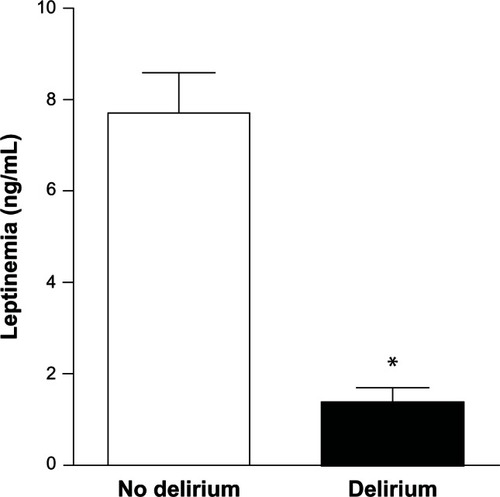
Figure 3 Negative correlation between leptin levels and number of comorbidities and number of medications in patients without delirium (A and C respectively) and in patients with delirium (B and D respectively).
Leptin values were divided into quartiles in order to establish the association between this variable and the presence of delirium, which was positive (P < 0.01). Delirium was more common in quartile 1 patients in comparison with all the other quartiles (P < 0.01) as well as a greater number of diagnoses and number of medications, but no significant differences were found regarding age, gender, BMI or laboratory tests between quartiles (data not shown) as revealed by bivariate analysis. The association between leptin levels and the presence of delirium remained after adjustment for number of diagnoses and number of medications.
Discussion
Delirium is a disorder that increases morbidity and mortality in older patients and its pathophysiology needs to be properly clarified in order to treat patients more effectively through prevention and care.Citation42,Citation43 Biomarkers of delirium can be used to pursue this goal because they may help clarify the course of this condition and aid in early diagnoses, which can result in improved and more appropriate treatments.
This study establishes the association between leptin and delirium in elderly inpatients, a population with an augmented risk of developing delirium and its complications.Citation2 In this study, more men than women developed delirium, which was consistent with other reports.Citation10 The frequency of cerebrovascular diagnoses was higher in the group of patients with delirium, which is consistent with most reports, although this study failed to find any significant difference in the frequency of other types of diagnoses between the two groups of patients. In this study, no correlation was found between delirium and any medication, although other studies have identified associations of delirium and the past consumption of anticholinergic drugs, sedatives and narcotics, among other diverse drugs.Citation44 However, the majority of studies show that delirium has a greater association with the presence of multiple diseases and the consumption of multiple medications than with individual factors,Citation45,Citation46 especially in older people, which is consistent with the findings of the present study.
Leptin levels were significantly lower in patients with delirium compared with those without this disorder and leptin levels are associated with the presence of delirium. This suggests a role for this hormone in the pathophysiological processes that lead to the development of delirium. Additionally, there is a negative correlation between leptin levels and the number of comorbidities and number of medications. This suggests that there is a relationship between this hormone and the severity of the patient’s clinical condition, which is related to these parameters. It is known that the risk of complications or death in older patients is related to the presence of comorbidities, which results in the increased consumption of different medications and increased frequency of adverse reactions. Furthermore, the risk of delirium is greater in older patients with comorbidities; therefore, leptin could be a marker of the severity of clinical features as well as a marker for augmented risk of developing delirium. Leptin is a neural modulator and the association found in this study is not unexpected because low leptin levels have been associated with other neuropsychiatric disorders, such as depression,Citation30,Citation31 which involves emotional discomfort, a symptom shared with delirium. Therefore, leptin has been presented as a possible antidepressant therapy.Citation30,Citation47 In addition, hypoleptinemia increases the risk for Alzheimer’s diseaseCitation48 and vascular dementia.Citation32 Additionally, this hormone decreases the phosphorylation of tau-proteins in neurons, which is associated with the severity of Alzheimer’s disease.Citation49 It is worth noting that aging has been associated with a decrease in the levels of leptin, and a resistance to the actions of leptin.Citation50,Citation51 A greater magnitude of this decline in leptin levels may be associated with a greater risk of cognitive impairment,Citation26 which might explain the augmented risk of developing delirium in this population.
It is not surprising that systemic leptin has effects on the brain, given that leptin, despite being a protein, can enter the central nervous system through the cerebrospinal fluidCitation52 or via a receptor-mediated transport mechanism that allows it to cross the blood-brain barrier.Citation54 Additionally, leptin can be expressed locally in the brain,Citation54 although the regulators of its production remain unclear. In addition LRb is expressed by neurons throughout the brain,Citation23,Citation24 which can explain why leptin may affect a diverse range of neural functions.Citation55,Citation56
More work needs to be done to elucidate the mechanisms by which leptin can intervene during the development of delirium, but a number of studies have shown significant effects of leptin on neurons. Leptin can regulate protein synthesis in neurons and glial cells,Citation57 and it facilitates long-term potentiation in the pyramidal neurons from CA1 hippocampal cortex.Citation58 Mice that are insensitive to leptin have lower synaptic plasticity in the hippocampus, which can affect memory processing.Citation29,Citation59 Leptin may also have neurotrophic actions and increase NMDA receptor activity in the hippocampus,Citation60 the density of dendritic spines, the efficacy of synaptic transmission in pyramidal neurons,Citation60 and the axonal growth cone size in cortical neurons,Citation61 Leptin also induces actin reorganization in the hippocampus, which has an important role in the morphological changes of dendrites in CA1 cells, and in the formation of functional synapses.Citation60,Citation62 It is likely due to these reasons that mice with decreased sensitivity to leptin show cognitive deficits and even Alzheimer’s disease.Citation55,Citation62 Furthermore, leptin could have a role in the treatment of this disorder.Citation63 In aging brains, there is a diminution of dendritic spines in the hippocampal and pyramidal cells,Citation64 and this can be an effect of hypoleptinemia, although further studies must be performed to explore this issue.
Delirium is characterized by compromised cognitive performance, and low leptin levels have been associated with cognitive impairment in humansCitation25–Citation27 and rodents.Citation28,Citation29 Treatment with this hormone improved neurocognitive performance.Citation65–Citation67 Furthermore, it is known that leptin has neuroprotective effectsCitation68,Citation69 as well as antiapoptotic actions on neurons;Citation70 it also stimulates neurogenesis in the hippocampus.Citation71 Low levels of this hormone, as demonstrated by its association with delirium in the elderly patients evaluated in this study, could result in the loss of these beneficial actions, and can be therefore form part of the pathophysiological framework of delirium.
Leptin is also considered to be a modulator of the immune response, and low levels of this hormone are associated with impairment of the immune profile,Citation72 which can result in an increase in the levels of a number of cytokines. Increased cytokine levels have been associated with the development of delirium or cognitive decline in patients after cardiac surgeryCitation73 and secondary to infections.Citation74 This neuroinflammatory response could result in synaptic dysfunction, cognitive impairment and hence delirium.Citation75
In conclusion, leptin levels may have a role in the pathophysiological processes that lead to delirium in older patients, as this hormone is affected by a number of clinical conditions and has profound effects on central nervous system functioning, especially on mechanisms that regulate cognitive performance. According to the results of this study, low leptin is associated with the development of delirium in older people and correlates with the presence of comorbidities or with the consumption of multiple medications, which have been identified as causes of delirium; thus, low leptin could help to predict the risk of developing delirium in the elderly, although a causal relationship cannot be established at this point and further studies need to be conducted to determine its clinical relevance. Moreover, additional research may help clarifying the effects of other neuropsychiatric disorders, such as dementia and depression, on leptin levels, which could not be determined from the present results since these diagnoses were not analyzed. These findings may be useful in pursuing a better understanding of delirium, for developing more effective strategies to prevent this disorder, and for early diagnosis and proper intervention in affected patients.
Acknowledgements
We acknowledge the clinical and the administrative staff of the Hospital Universitario San Jorge for their collaboration in drawing the blood samples and allowing access to patients and their clinical records. We also thank the Universidad Tecnológica de Pereira Research and Innovation Office for their financial and administrative support.
Disclosure
The authors declare no conflicts of interest in this work.
References
- FinucaneTEDelirium at the end of lifeAnn Intern Med2002137429512186524
- MittalVMuraleeSWilliamsonDReview: delirium in the elderly: a comprehensive reviewAm J Alzheimers Dis Other Demen20112629710921285047
- GroverSChakrabartiSControlled trials of deliriumJ Psychosom Res201272186
- InouyeSKRushingJTForemanMDPalmerRMPompeiPDoes delirium contribute to poor hospital outcomes? A three-site epidemiologic studyJ Gen Intern Med19981342342429565386
- LindesayJRockwoodKRolfsonDThe epidemiology of deliriumLindesayJRockwoodKMacdonaldADelirium in old ageOxford (UK)Oxford University Press20022750
- ClaryGLKrishnanKRDelirium: diagnosis, neuropathogenesis, and treatmentJ Psychiatr Pract20017531032315990541
- InselKCBadgerTADeciphering the 4 D’s: cognitive decline, delirium, depression and dementia – a reviewJ Adv Nurs200238436036811985687
- MilisenKBraesTFickDMForemanMDCognitive assessment and differentiating the 3 Ds (dementia, depression, delirium)Nurs Clin North Am200641112216492451
- EdlundALundstromMSandbergOSymptom profile of delirium in older people with and without dementiaJ Geriatr Psychiatry Neurol200720316617117712100
- ArinzonZPeisakhASchrireSBernerYNDelirium in long-term care setting: indicator to severe morbidityArch Gerontol Geriatr201152327027520452686
- GleasonOCDeliriumAm Fam Physician20036751027103412643363
- LeslieDLInouyeSKThe importance of delirium: economic and societal costsJ Am Geriatr Soc201159Suppl 2S241S24322091567
- LinSMLiuCYWangCHThe impact of delirium on the survival of mechanically ventilated patientsCrit Care Med200432112254225915640638
- RockwoodKLindesayJDelirium and dyingInt Psychogeriatr200214323523812475084
- HarveyJLeptin: a diverse regulator of neuronal functionJ Neurochem2007100230731317076761
- ZupancicMLMahajanALeptin as a neuroactive agentPsychosom Med201173540741421597032
- KershawEEFlierJSAdipose tissue as an endocrine organJ Clin Endocrinol Metab20048962548255615181022
- FriedmanJMThe function of leptin in nutrition, weight, and physiologyNutr Rev20026010 Pt 2S1S14 discussion S68–S84, 85–1712403078
- SánchezJPerfil fisiológico de la leptina [Physiological profile of leptin]Colombia Médica20053615059
- AhimaRSFlierJSLeptinAnnu Rev Physiol20006241343710845097
- BjorbaekCUotaniSda SilvaBFlierJSDivergent signaling capacities of the long and short isoforms of the leptin receptorJ Biol Chem19972725132686326959405487
- ChuaSJrSignal transduction pathways for leptin: an embarrassment of richesDiabetes200958351351419246598
- BurgueraBCouceMELongJThe long form of the leptin receptor (OB-Rb) is widely expressed in the human brainNeuroendocrinology200071318719510729790
- CouceMEBurgueraBParisiJEJensenMDLloydRVLocalization of leptin receptor in the human brainNeuroendocrinology19976631451509380271
- GunstadJSpitznagelMBKearyTASerum leptin levels are associated with cognitive function in older adultsBrain Res2008123023323618675793
- HoldenKFLindquistKTylavskyFASerum leptin level and cognition in the elderly: Findings from the Health ABC StudyNeurobiol Aging20093091483148918358569
- HuangJSLetendreSMarquie-BeckJLow CSF leptin levels are associated with worse learning and memory performance in HIV-infected menJ Neuroimmune Pharmacol20072435235818040853
- FarrSABanksWAMorleyJEEffects of leptin on memory processingPeptides20062761420142516293343
- LiXLAouSOomuraYHoriNFukunagaKHoriTImpairment of long-term potentiation and spatial memory in leptin receptor-deficient rodentsNeuroscience2002113360761512150780
- LuXYThe leptin hypothesis of depression: a potential link between mood disorders and obesity?Curr Opin Pharmacol20077664865218032111
- WestlingSAhrenBTraskman-BendzLWestrinALow CSF leptin in female suicide attempters with major depressionJ Affect Disord2004811414815183598
- PowerDANoelJCollinsRO’NeillDCirculating leptin levels and weight loss in Alzheimer’s disease patientsDement Geriatr Cogn Disord200112216717011173891
- AtmacaMKulogluMTezcanEGeciciOUstundagBSerum cholesterol and leptin levels in patients with borderline personality disorderNeuropsychobiology200245416717112097803
- AtmacaMTezcanEKulogluMUstundagBSerum leptin levels in obsessive-compulsive disorderPsychiatry Clin Neurosci200559218919315823166
- Alzheimer’sAResearch consent for cognitively impaired adults: recommendations for institutional review boards and investigatorsAlzheimer Dis Assoc Disord200418317117515494623
- World Medical AssociationDeclaration of Helsinki. Ethical Principles for Medical Research Involving Human SubjectsBulletin of the World Health Organization200179437337411357217
- FolsteinMFFolsteinSEMcHughPR“Mini-mental state”. A practical method for grading the cognitive state of patients for the clinicianJ Psychiatr Res19751231891981202204
- MonetteJGalbaud du FortGFungSHEvaluation of the Confusion Assessment Method (CAM) as a screening tool for delirium in the emergency roomGen Hosp Psychiatry2001231202511226553
- Castro-CostaEFuzikawaCUchoaEFirmoJOLima-CostaMFNorms for the mini-mental state examination: adjustment of the cut-off point in population-based studies (evidences from the Bambui health aging study)Arq Neuropsiquiatr2008663A52452818813712
- PrinceMAcostaDChiuHScazufcaMVargheseMDementia diagnosis in developing countries: a cross-cultural validation studyLancet2003361936190991712648969
- AssociationAPDiagnostic and Statistical Manual of Mental Disorders: DSM-IVWashingtonAmerican Psychiatric Association1994
- InouyeSKBogardusSTJrCharpentierPAA multicomponent intervention to prevent delirium in hospitalized older patientsN Engl J Med1999340966967610053175
- Lampley-DallasVTAnticipating and preventing deliriumJ Okla State Med Assoc2002952717511845674
- CleggAYoungJBWhich medications to avoid in people at risk of delirium: a systematic reviewAge Ageing2011401232921068014
- BergeronNSkrobikYDuboisMJDelirium in critically ill patientsCrit Care20026318118212133171
- FlahertyJHThe evaluation and management of delirium among older personsMed Clin North Am201195355557721549878
- LuXYKimCSFrazerAZhangWLeptin: a potential novel antidepressantProc Natl Acad Sci USA200610351593159816423896
- LiebWBeiserASVasanRSAssociation of plasma leptin levels with incident Alzheimer disease and MRI measures of brain agingJAMA2009302232565257220009056
- GrecoSJSarkarSJohnstonJMLeptin reduces Alzheimer’s disease-related tau phosphorylation in neuronal cellsBiochem Biophys Res Commun2008376353654118801339
- GabrielyIMaXHYangXMRossettiLBarzilaiNLeptin resistance during aging is independent of fat massDiabetes20025141016102111916920
- MaXHMuzumdarRYangXMAging is associated with resistance to effects of leptin on fat distribution and insulin actionJ Gerontol A Biol Sci Med Sci2002576B225B23112023258
- SchwartzMWPeskindERaskindMBoykoEJPorteDJrCerebrospinal fluid leptin levels: relationship to plasma levels and to adiposity in humansNat Med1996255895938616722
- BanksWAKastinAJHuangWJaspanJBManessLMLeptin enters the brain by a saturable system independent of insulinPeptides19961723053118801538
- UrEWilkinsonDAMorashBAWilkinsonMLeptin immunoreactivity is localized to neurons in rat brainNeuroendocrinology200275426427211979057
- HarveyJLeptin regulation of neuronal excitability and cognitive functionCurr Opin Pharmacol20077664364718024215
- MorrisonCDLeptin signaling in brain: A link between nutrition and cognition?Biochim Biophys Acta20091792540140819130879
- AhimaRSBjorbaekCOseiSFlierJSRegulation of neuronal and glial proteins by leptin: implications for brain developmentEndocrinology199914062755276210342866
- WaynerMJArmstrongDLPhelixCFOomuraYOrexin-A (Hypocretin-1) and leptin enhance LTP in the dentate gyrus of rats in vivoPeptides200425699199615203246
- HarveyJSolovyovaNIrvingALeptin and its role in hippocampal synaptic plasticityProg Lipid Res200645536937816678906
- ShanleyLJIrvingAJHarveyJLeptin enhances NMDA receptor function and modulates hippocampal synaptic plasticityJ Neurosci20012124RC18611734601
- ValerioAGhisiVDossenaMLeptin increases axonal growth cone size in developing mouse cortical neurons by convergent signals inactivating glycogen synthase kinase-3betaJ Biol Chem200628118129501295816522636
- O’MalleyDMacDonaldNMizielinskaSConnollyCNIrvingAJHarveyJLeptin promotes rapid dynamic changes in hippocampal dendritic morphologyMol Cell Neurosci200735455957217618127
- JohnstonJMGrecoSJHamzelouAAshfordJWTezapsidisNRepositioning leptin as a therapy for Alzheimer’s diseaseTherapy20118548149022121334
- BishopNALuTYanknerBANeural mechanisms of ageing and cognitive declineNature201046452953520336135
- OomuraYHoriNShiraishiTLeptin facilitates learning and memory performance and enhances hippocampal CA1 long-term potentiation and CaMK II phosphorylation in ratsPeptides200627112738274916914228
- Paz-FilhoGWongMLLicinioJThe procognitive effects of leptin in the brain and their clinical implicationsInt J Clin Pract201064131808181221070531
- Paz-FilhoGJBabikianTAsarnowRLeptin replacement improves cognitive developmentPLoS One200838e309818769731
- TangBLLeptin as a neuroprotective agentBiochem Biophys Res Commun2008368218118518222172
- ZhangFWangSSignoreAPChenJNeuroprotective effects of leptin against ischemic injury induced by oxygen-glucose deprivation and transient cerebral ischemiaStroke20073882329233617600230
- RussoVCMetaxasSKobayashiKHarrisMWertherGAAntiapoptotic effects of leptin in human neuroblastoma cellsEndocrinology200414594103411215166121
- GarzaJCGuoMZhangWLuXYLeptin increases adult hippocampal neurogenesis in vivo and in vitroJ Biol Chem200828326182381824718367451
- QuasimTMcMillanDCWallaceAMKinsellaJThe relationship between leptin concentrations, the systemic inflammatory response and illness severity in surgical patients admitted to ITUClin Nutr200423223323815030963
- RudolphJLRamlawiBKuchelGAChemokines are associated with delirium after cardiac surgeryJ Gerontol A Biol Sci Med Sci200863218418918314455
- van GoolWAvan de BeekDEikelenboomPSystemic infection and delirium: when cytokines and acetylcholine collideLancet2010375971677377520189029
- CerejeiraJFirminoHVaz-SerraAMukaetova-LadinskaEBThe neuroinflammatory hypothesis of deliriumActa Neuropathol2010119673775420309566