Abstract
Objective
We aimed to determine distribution and diversities of psychiatric comorbidities in children and adolescents with attention deficit/hyperactivity disorder (ADHD) in terms of age groups, sex, and ADHD subtype.
Materials and methods
The sample included 6–18 year old children and adolescents from Turkey (N=108; 83 boys, 25 girls) diagnosed with ADHD. All comorbid diagnoses were determined based on the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version assessment.
Results
96.3% of the cases were found to have at least one psychiatric comorbid diagnosis. The most frequent psychiatric comorbid disorder was oppositional defiant disorder (69.4%) followed by anxiety disorders (49%) and elimination disorders (27.8%). Disruptive behavior disorders were more common in ADHD-combined type. Depression and anxiety disorders were more common in girls. Separation anxiety disorder and elimination disorder were more common in children, whereas depression, bipolar disorder, obsessive–compulsive disorder, and social phobia were more common in the adolescents.
Conclusion
According to our results, when a diagnostic tool was used to assess the presence of comorbid psychiatric disorders in children and adolescents diagnosed with ADHD, almost all cases had at least one comorbid diagnosis. Therefore, especially in the clinical sample, ADHD cases should not be solely interpreted with ADHD symptom domains, instead they should be investigated properly in terms of accompanying psychiatric disorders.
Introduction
Attention deficit/hyperactivity disorder (ADHD) is one of the most frequent psychiatric disorders of childhood. ADHD, which is a multifactorial and clinically heterogeneous disease, leads to socioeconomic burden and undesirable academic and occupational results.Citation1,Citation2 Worldwide prevalence of ADHD has been reported to be 4%–7% in children.Citation3 ADHD is most frequent among school-age children and its frequency decreases in further ages.Citation4,Citation5 Furthermore, most of the recent studies assume that ADHD is a lifelong disorder.Citation3,Citation6–Citation10
ADHD is more common in boys as compared to girls. The boy to girl ratio varies from 3:1 to 10:1 depending on the study design; for instance, being a community or a clinical sample.Citation1
Other psychiatric disorders and social problems are likely to accompany a substantial proportion of children admitted to a clinic with a diagnosis of ADHD, and this enhances the severity of the clinical picture.Citation11 The presence of psychiatric comorbidities complicates the diagnosis and treatment procedures, and interferes with the prognostic assumptions of ADHD. Therefore, evaluation and proper diagnosis of comorbid psychiatric disorders are of great importance.Citation12 Psychiatric disorders that accompany ADHD vary widely among different countries and cultures.Citation13,Citation14 There are a limited number of studies that have been performed in Turkey on this issue. A clinical-based study conducted in Turkey evaluated children with ADHD using The Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL) and found that 73.7% of the children had at least one comorbid psychiatric disorder.Citation15
There are numerous population- and clinical-based studies reporting that more than half of ADHD cases have at least one psychiatric comorbidity and that this rate increases with age.Citation16–Citation18 A study conducted in Switzerland reported one comorbidity in 87% of ADHD cases and more than one comorbidity in 67%.Citation18 A study from Iran detected at least one psychiatric comorbidity in 73% of child and adolescent cases of ADHD.Citation19 It has also been reported that the clinical group (cases assessed in psychiatric outpatient clinics) has more comorbid psychiatric disorders compared to the general population.Citation20
Oppositional defiant disorder is characterized by a pattern of hostile, negativistic, defiant, and disobedient attitudes and behaviors, especially toward authority figures, that is associated with less social and academic functioning.Citation21 Oppositional defiant disorder has been reported to be one of the most frequent comorbidities in ADHD with a rate reported between 20% and 80%.Citation18,Citation19,Citation22–Citation24 Conduct disorder is also one of the comorbidities of ADHD.Citation25,Citation26 Wilson and Marcotte divided ADHD cases aged between 14 and 18 years into two groups as having conduct disorder or not and compared them in terms of school success, self-perception, behavior problems, alcohol and substance abuse, and adaptive behaviors.Citation27 They reported that cases with conduct disorder displayed significantly lower school success, higher externalizing behaviors and emotional difficulties, and lower adaptive behaviors as compared to cases without conduct disorder.Citation27 The rate of depression and anxiety disorder concomitant with ADHD has been reported to be 20%–40%.Citation28 Concurrence of ADHD and bipolar disorder or confusing them with each other is an unclear issue. It has also been reported that some of the children receiving ADHD treatment meet the diagnostic criteria of anxiety disorders.Citation29 Family studies have reported that ADHD is widespread among children, adolescents, and adults with bipolar disorder.Citation25,Citation30,Citation31 Tics are sudden, repetitive movements, gestures, or phonic productions that typically mimic some aspect of normal behavior.Citation32 The rate of tic disorder comorbidity has been reported to be between 4% and 18% in patients with ADHD.Citation29,Citation33 The disorders of elimination – enuresis and encopresis – represent an inability to achieve or maintain control of bodily functions.Citation34 Nocturnal enuresis is the intermittent involuntary loss of urine at night, in the absence of physical disease, at an age when a child could reasonably be expected to be dry (chronological age is at least 5 years).Citation34–Citation36 It is known that primary nocturnal enuresis is common in patients with ADHD.Citation37 Although the association between these two conditions has not been clearly defined, they have been considered to share a common genetic mechanism.Citation38 It has been reported that the frequency of primary nocturnal enuresis in patients with ADHD is 21%–32% and it is 1.8–6 times higher as compared to the general population.Citation37,Citation38
In addition, the rate of comorbid diagnoses may vary according to the subtypes of ADHD, age groups, and sex. For instance, it has been reported that conduct disorder and oppositional defiant disorder appear in early childhood in ADHD, whereas depression and anxiety symptoms appear at older ages.Citation11 In another study, Lahey et al found the frequency of anxiety disorder to be higher in children with the ADHD-inattentive subtype as compared to the children with the ADHD-combined subtype.Citation39
In the present study, we aimed to determine frequency of psychiatric comorbidities in children and adolescents diagnosed with ADHD and to assess the association between age groups, sex, and ADHD subtype and the distribution of comorbid psychiatric disorders.
Materials and methods
Participants and process
The present study included children aged between 6 and 18 years, who were admitted to the pediatric psychiatry outpatient clinic of our hospital within a 4-month period and were diagnosed with ADHD according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria. All subjects in this study were treatment-naive. The assessment was done in the first psychiatric admission. The K-SADS-PL was used to assess comorbid psychiatric disorders. Mental retardation was an exclusion criterion in our study.
Scales
The K-SADS-PL is a semi-structured interview scale, which is widely used and enables evaluation in 20 different diagnostic domains. Kaufman et al reported K-SADS-PL as a valid and reliable diagnostic tool.Citation40 Gökler et al adapted K-SADS-PL into Turkish in 2004.Citation41 This scale was applied to all cases and their parents by the physician trained with “Structured Interview Techniques” in the K-SADS-PL.
Statistical analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences (IBM Corporation, Armonk, NY, USA) version 10.0. Descriptive statistics were expressed as mean, standard deviation, and percentage. Proportional comparisons were carried out using Pearson’s chi-square, Yates’ chi-square, and Fisher’s exact tests. For Fisher’s exact tests, as a chi-square value could not be calculated, only P-values are presented. Margin of error (alpha value) was considered 95%; thus, P-values<0.05 were considered to be statistically significant.
Results
The mean age of all participants (n=108; 83 boys, 25 girls) was 10.26±3.3 (range: 6–18) years. Of the children, 64.8% (n=70) were in the 6–11 years age group and 35.2% (n=38) were in 12–18 years age group. Of the children, 86.1% were diagnosed with ADHD-combined type (ADHD-C) and 13.9% were diagnosed with ADHD-predominantly inattentive type (ADHD-PI). None of the children were diagnosed with ADHD-predominantly hyperactive-impulsive type (ADHD-HI). Age and sex distributions with respect to the diagnostic subtypes are summarized in . While the distribution of ADHD subtypes did not differ according to age, ADHD-PI type was found to be more common in the girls.
Table 1 Characteristics of cases according to the diagnosis
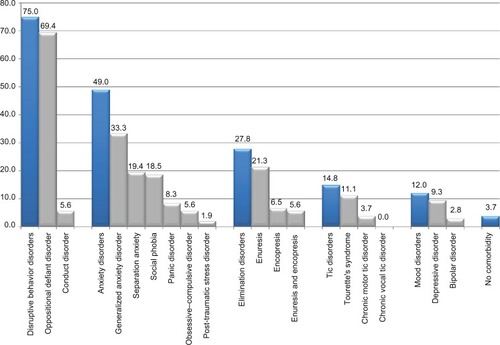
With regard to comorbidities, 104 children (96.3%) had a mental disorder other than ADHD. Of these children, 36 (33.3%) had one, 45 (41.7%) had two, eleven (10.2%) had three, four (3.7%) had four, six (5.6%) had five, and two (1.9%) had six psychiatric comorbidities. The most frequently observed comorbidity was oppositional defiant disorder with a rate of 69.4%. The rates of psychiatric comorbidities are presented in .
Figure 1 Distribution of psychiatric comorbidities in children with attention deficit/hyperactivity disorder.
Psychiatric comorbidities according to ADHD subtypes are demonstrated in . Disruptive behavior disorders were more frequent in children diagnosed with ADHD-C type, whereas anxiety disorders were more frequent in children diagnosed with ADHD-PI type.
Table 2 Psychiatric comorbidities in cases with attention deficit/hyperactivity disorder according to diagnostic subtypes
In general, anxiety disorder was found to be more common in the girls. It was found that depressive disorders were more frequent in the girls as compared to the boys ().
Table 3 Psychiatric comorbidities in cases with attention deficit/hyperactivity disorder according to sex
Based on the assumption that the frequency of comorbidities might be different in children (<12 years) and adolescents (≥12 years), it was investigated with respect to age. Mood disorder was found in 1.4% of the children and 31.6% of the adolescents. Both depression and bipolar disorder were more frequent in the adolescents as compared to the children. Separation anxiety was significantly more common in the children; on the other hand, obsessive–compulsive disorder and social phobia were more common in the adolescents. Elimination disorder was found to be more frequent in the children as compared to the adolescents ().
Table 4 Psychiatric comorbidities in cases with attention deficit/hyperactivity disorder according to the age group
Discussion
In this study, the rates of psychiatric comorbidities in children and adolescents with ADHD were investigated. It has been reported that ADHD is three to ten times higher in males depending on whether the study is population-based or clinical-based.Citation1 In the present clinical-based study, the male:female ratio was 3.3:1.0.
In a recent meta-analysis by Willcut, studies on ADHD diagnosed according to DSM-IV were reviewed and it was revealed that ADHD-PI type was the most frequently observed type in the population; however, ADHD-C type was probably referred to the clinical services more frequently.Citation42 In the present clinical-based study, ADHD-C type (86.1%) was the most common type and 13.9% of the cases were diagnosed with ADHD-PI type; however, none of the cases were diagnosed with ADHD-HI type. Similarly, Byun et al conducted a study using K-SADS-PL and detected ADHD-C type in 66.7%, ADHD-PI type in 21%, ADHD-HI type in 1%, and ADHD not otherwise specified in 11.4% of the patients.Citation43 Differently, Ghanizadeh reported ADHD-C type in 42.7%, ADHD-PI type in 26.3%, and ADHD-HI type in 31% of 171 children with ADHD.Citation19 Another clinical-based study conducted in Turkey reported that the frequency of ADHD-C type was 60.9%, ADHD-PI type was 36.1%, and ADHD-HI type was 3%.Citation15
In population-based samples, in patients with ADHD diagnosed according to DSM-IV, the male:female ratio was reported to be 2.7:1.0 for ADHD-C type, 5.2:1.0 for ADHD-HI type, and 1.8:1.0 for ADHD-PI type.Citation42 In the present study, when investigating the frequency of ADHD subtypes according to sex, ADHD-C type was the most frequently encountered subtype both in boys and girls (92.8% and 64%, respectively). ADHD-PI type was significantly more common in the girls than the boys (36% versus 7.2%, P<0.001). Gaub and Carlson investigated differences between sexes and reported a lower level of attention in girls and more frequent aggressive behaviors in boys.Citation44 Ghanizadeh found no difference between boys and girls in terms of the prevalences of ADHD subtypes.Citation19 Rates may change depending on whether the study is population-based or clinical-based.
In our study, 104 (96.3%) of 108 patients had at least one psychiatric comorbidity. This ratio was similarly high in the results of previous studies conducted using K-SADS-PL (70%–80%); however, in our study the comorbidity rate was unusually higher than those of the studies conducted using different scales.Citation15,Citation17,Citation43,Citation45–Citation47 The high percentage of the presence of comorbid disorders can be associated with the study method. In other words, it can be assumed that various psychiatric disorders can be evaluated with K-SADS-PL in more detail. It has been also reported that the clinical group has more comorbidities as compared to the general population.Citation20 This may result from the fact that patients having more severe symptoms or more functional disorders are admitted to hospitals more frequently. The present study group included the patients admitted to the outpatient polyclinic of a university hospital. Another clinical-based study conducted in Turkey evaluated children with ADHD using K-SADS-PL and found that 73.7% had at least one psychiatric comorbidity.Citation15 Biederman et al reported two or more comorbidities in 20% of ADHD cases admitted to the clinic.Citation28 In the present study, of the ADHD cases, 33.37% had one, 41.7% had two, 10.2% had three, 3.7% had four, 5.6% had five, and 1.9% had six psychiatric comorbidities.
Psychiatric comorbidity may worsen the clinical picture in children and adolescents diagnosed with ADHD. A recently published study reports that psychiatric comorbidity increases social impairment among children with ADHD, but did not worsen academic functioning.Citation48 Likewise, certain comorbidities like oppositional defiant disorder may be particularly problematic for peer functioning, whereas mood/anxiety symptoms may be less impairing.Citation49
Withdrawn was reported to be the most common cause of social problems in ADHD-PI type, whereas it was social exclusion in ADHD-C type.Citation50 In the present study, oppositional defiant disorder was significantly more common in ADHD-C type, whereas anxiety disorders were encountered more frequently in ADHD-PI type. However, another study reported that the frequency of comorbidity showed no difference between ADHD subtypes.Citation19
In this study, oppositional defiant disorder was observed to be the most frequent comorbidity in ADHD with a rate of 69.4%. The comorbidity of oppositional defiant disorder in ADHD has been found to be a risk factor for accompaniment of other disorders, predominantly anxiety symptoms.Citation23 Important family, social, and school-related problems are observed in ADHD cases accompanied by oppositional defiant disorder. These children are more punished and exposed to negative stimulus. The reverse situation is also considered; oppositional defiant disorder more frequently accompanies ADHD in cases having negative family functions.Citation51 Harada et al reported higher frequency of school refusal and friendship problems when ADHD was accompanied by oppositional defiant disorder.Citation52
It has been reported that the presence of conduct disorders in ADHD is associated with more serious symptoms and that the risk for antisocial personality disorder and substance abuse and addiction is increased in these cases.Citation53 In the present study, the rate of conduct disorder was found to be low at 5.6%. Ghanizadeh reported this rate to be 9.9%.Citation19 It has been reported that conduct disorder is more frequently accompanied in those with oppositional defiant disorder symptoms.Citation54 The presence of conduct disorder in ADHD is the most important indicator for the severity of the clinical picture and the rate of hospitalization is greater in this group.Citation26 In the present study, the frequency of conduct disorder was 4% in the girls and 6% in the boys; however, the difference was not significant (Fisher’s exact test P=1.000).
We found that depression and anxiety disorder accompanied ADHD in 9.3% and 49.0% of the cases, respectively. With regard to sex, both comorbidities were more common in girls. It has been reported that conduct disorder and oppositional defiant disorder appear in early childhood in ADHD, whereas depression and anxiety symptoms appear at older ages.Citation11 In the present study, with regard to the age groups, the rate of depression was significantly higher in the adolescents as compared to the children (23.7% versus 1.4%, Fisher’s exact test: P<0.001). Anxiety disorder was present in 60.5% of the adolescents and in 42.9% of the children; however, the difference was not significant (χ2=2.41, standard deviation =1, P=0.121). With respect to the subtypes of ADHD, the frequency of anxiety disorder was higher in ADHD-PI type as compared to ADHD-C type (73% versus 45.2%, P=0.043). Lahey et al found the frequency of anxiety disorder to be higher in children with attention disorder without hyperactivity as compared to the children with ADHD.Citation39 The results of the present study are in accordance with their findings.
Symptoms such as sleep disorders, concentration difficulty, and irritability observed in depression and symptoms such as sustained anxiety and failure of concentration observed in anxiety disorders may be confused with ADHD and may sometimes be misdiagnosed.Citation55–Citation57 Where the depression or anxiety symptoms accompany ADHD, both domains of psychopathology makes the diagnostic procedure complicated and ADHD symptoms may be more severe.Citation58,Citation59 It is debatable how treatment should be planned when these disorders accompany ADHD. In general, the predominant disorder is to be treated as a priority.Citation58 Some psychiatric symptoms observed in family members may inform opinions about additional diagnoses to the cases.Citation60
While it has been reported that ADHD and mood disorders are observed together in 20%–30% of cases, it remains controversial whether mood disorders develop secondary to long-term ADHD symptoms or if they appear independent from ADHD symptoms.Citation55 Recent family, genetic, and long-term follow-up studies have demonstrated that ADHD and major depressive disorder share common familial risk and appear independent from each other.Citation55,Citation61 Compared to high rates (over 30%) in Western countries, the rate of comorbid mood disorder was found to be lower in cases with ADHD in the present study (12%).Citation3,Citation12,Citation47 This finding could be associated with the assumptions that parents in our clinical sample may attend to their children’s extraversive symptoms (eg, inattention, hyperactivity, aggression, and impulsive behavior) rather than their emotional distress. Thus, parents might have reported emotional symptoms of their children to a lesser extent. The children being reluctant to express negative emotions could also be another reason. In brief, low frequency of mood disorders may be a consequence of cultural differences.
According to our results, the most common anxiety disorder was generalized anxiety disorder followed in descending order by separation anxiety disorder, social phobia, panic disorder, obsessive–compulsive disorder, and post-traumatic stress disorder. With respect to the age group, the frequency of separation anxiety disorder was higher in the children than that in the adolescents (25.7% versus 7.9%, P=0.025). However, the frequencies of social phobia and obsessive–compulsive disorder were higher in the adolescents than in the children (34.2% versus 10.0%, P=0.002 for social phobia; 13.2% versus 1.4%, P=0.011 for obsessive–compulsive disorder). Ghanizadeh found the rates of separation anxiety disorder and obsessive–compulsive disorder to be 19.8% and 7.6%, respectively, and reported no difference between sexes.Citation19 Geller et al reported that obsessive–compulsive disorder frequently accompanied ADHD, and in the case of concurrence of both conditions, academic and social skills were affected more, and became more resistant to therapy.Citation62
In this study, in terms of the subtypes of ADHD, the frequency of social phobia was higher in ADHD-PI type; it was present in 60% of the cases diagnosed with ADHD-PI type and in 11.8% of the cases diagnosed with ADHD-C type (P<0.001). Of the patients with anxiety disorder, 47.2% had one, 30.2% had two, 20.7% had three, and 1.9% had four anxiety disorders. The rate of anxiety disorder was similar as compared to that found in previous studies. Since more than 52% of the patients with ADHD have more than two anxiety disorders, the clinician should carefully examine the anxiety symptoms of patients with ADHD.
On the other hand, ADHD was accompanied by bipolar disorder in three cases. All three cases were male adolescents and diagnosed with ADHD-C type. Biederman et al compared 140 children and adolescents with ADHD to 120 healthy children and adolescent controls aged between 6 and 17 years during a 4-year follow-up study.Citation63 They reported the rate of bipolar disorder to be 22% in children and 28% in adolescents with ADHD.Citation63 In the study by Faraone et al investigating ADHD in childhood-onset mania, 68 manic children and 42 manic adolescents were compared with peers with other mental disorders and with healthy controls.Citation64 They found the rate of ADHD to be 93% in manic children, 88% in adolescents with childhood-onset mania, and 59% in adolescents with adolescent-onset mania.Citation64 They suggested that ADHD and bipolar disorder comorbidity did not result from overlapping symptoms.Citation64
In our sample, 14.8% of the cases had tic disorder. With regard to sex, all of the patients diagnosed with tic disorder were male. Evidence concerning the influence of an accompanying tic disorder on the course of ADHD is not as certain the evidence for the accompaniment of conduct disorders; however, it has been reported that the majority of cases with tic disorder accompanying ADHD develop obsessive–compulsive symptoms in the adolescent period.Citation33
In addition, ADHD was accompanied by elimination disorders in 27.8% of the cases. It was more frequent in children than in adolescents (37.1% versus 10.5%, P=0.003).
In conclusion, the present study found a high rate of comorbidity (96.3%) in cases with ADHD. The most common comorbidities were determined to be oppositional defiant disorder and anxiety disorders. Elimination disorders, tic disorders, and mood disorders also accompanied ADHD. Depressive disorders and anxiety disorders were more frequent in girls than in boys. Disruptive behavior disorder and oppositional defiant disorder were more common in ADHD-C type, whereas anxiety disorders and social phobia were more common in ADHD-PI type. Mood disorders, depression, social phobia, and obsessive–compulsive disorder accompanying ADHD were observed more frequently in the adolescents and separation anxiety disorders and elimination disorder accompanying ADHD were observed more frequently in the children.
Limited sample size, and not evaluating other variables including socioeconomic status and good parental care in shared families are some limitations of the present study.
According to our results, when a diagnostic tool was used to assess the presence of comorbid psychiatric disorders in children and adolescents diagnosed with ADHD, almost all cases had at least one comorbid diagnosis. Therefore, especially in the clinical sample, ADHD cases should not be solely interpreted with ADHD symptom domains, instead they should be investigated properly in terms of accompanying psychiatric disorders.
Disclosure
The authors have no conflicts of interest to declare in this work.
References
- BiedermanJAttention-deficit/hyperactivity disorder: a selective overviewBiol Psychiatry200557111215122015949990
- MuellerAKFuermaierABKoertsJTuchaLStigma in attention deficit hyperactivity disorderAtten Defic Hyperact Disord20124310111422773377
- SpencerTJBiedermanJMickEAttention-deficit/hyperactivity disorder: diagnosis, lifespan, comorbidities, and neurobiologyJ Pediatr Psychol200732663164217556405
- BurdLKlugMGCoumbeMJKerbeshianJChildren and adolescents with attention deficit-hyperactivity disorder: 1. Prevalence and cost of careJ Child Neurol200318855556113677583
- VasconcelosMMWernerJJrMalheirosAFLimaDFSantosISBarbosaJBAttention deficit/hyperactivity disorder prevalence in an inner city elementary schoolArq Neuropsiquiatr20036116773 Portugese12715022
- BiedermanJPettyCRO’ConnorKBHyderLLFaraoneSVPredictors of persistence in girls with attention deficit hyperactivity disorder: results from an 11-year controlled follow-up studyActa Psychiatr Scand2012125214715622097933
- ManorIRozenSZemishlaniZWeizmanAZalsmanGWhen does it end? Attention-deficit/hyperactivity disorder in the middle aged and older populationsClin Neuropharmacol201134414815421738027
- MatteBRohdeLAGrevetEHADHD in adults: a concept in evolutionAtten Defic Hyperact Disord201242536222588789
- RöslerMRetzWYaqoobiKBurgERetz-JungingerPAttention deficit/hyperactivity disorder in female offenders: prevalence, psychiatric comorbidity and psychosocial implicationsEur Arch Psychiatry Clin Neurosci200925929810518806916
- SobanskiEBrüggemannDAlmBSubtype differences in adults with attention-deficit/hyperactivity disorder (ADHD) with regard to ADHD-symptoms, psychiatric comorbidity and psychosocial adjustmentEur Psychiatry200823214214918024089
- ConnorDFEdwardsGFletcherKEBairdJBarkleyRASteingardRJCorrelates of comorbid psychopathology in children with ADHDJ Am Acad Child Adolesc Psychiatry200342219320012544179
- WaxmonskyJAssessment and treatment of attention deficit hyperactivity disorder in children with comorbid psychiatric illnessCurr Opin Pediatr200315547648214508296
- BakareMOAttention deficit hyperactivity symptoms and disorder (ADHD) among African children: a review of epidemiology and comorbiditiesAfr J Psychiatry (Johannesbg)201215535836123044891
- SmalleySLMcGoughJJMoilanenIKPrevalence and psychiatric comorbidity of attention-deficit/hyperactivity disorder in an adolescent Finnish populationJ Am Acad Child Adolesc Psychiatry200746121575158318030079
- HergünerSHergünerAPsychiatric comorbidity in children and adolescents with attention deficit hyperactivity disorderArchives of Neuropsychiatry201249114118 Turkish
- GauSSNiHCShangCYPsychiatric comorbidity among children and adolescents with and without persistent attention-deficit hyperactivity disorderAust N Z J Psychiatry201044213514320113302
- HuhYChoiISongMKimSHongSDJoungYA comparison of comorbidity and psychological outcomes in children and adolescents with attention-deficit/hyperactivity disorderPsychiatry Investig20118295101
- JensenPSMartinDCantwellDPComorbidity in ADHD: implications for research, practice, and DSM-VJ Am Acad Child Adolesc Psychiatry1997368106510799256586
- GhanizadehAPsychiatric comorbidity differences in clinic-referred children and adolescents with ADHD according to the subtypes and genderJ Child Neurol200924667968419491114
- HechtmanLAssessment and diagnosis of attention-deficit/hyperactivity disorderChild Adolesc Psychiatr Clin N Am20009348149810944652
- LaheyBBLoeberRQuayHCFrickPJGrimmJOppositional defiant and conduct disorders: Issues to be resolved for DSM-IVJ Am Acad Child Adolesc Psychiatry19923135395461592789
- HareWAInversoMJYoltonRLNeuropathology of the hyperkinetic childJ Am Optom Assoc198051127307410770
- LavigneJVCicchettiCGibbonsRDBinnsHJLarsenLDeVitoCOppositional defiant disorder with onset in preschool years: longitudinal stability and pathways to other disordersJ Am Acad Child Adolesc Psychiatry200140121393140011765284
- MickEBiedermanJFaraoneSVSayerJKleinmanSCase-control study of attention-deficit hyperactivity disorder and maternal smoking, alcohol use, and drug use during pregnancyJ Am Acad Child Adolesc Psychiatry200241437838511931593
- FaraoneSVBiedermanJWozniakJMundyEMenninDO’DonnellDIs comorbidity with ADHD a marker for juvenile-onset mania?J Am Acad Child Adolesc Psychiatry1997368104610559256584
- KadesjöBGillbergCThe comorbidity of ADHD in the general population of Swedish school-age childrenJ Child Psychol Psychiatry200142448749211383964
- WilsonJMMarcotteACPsychosocial adjustment and educational outcome in adolescents with a childhood diagnosis of attention deficit disorderJ Am Acad Child Adolesc Psychiatry19963555795878935204
- BiedermanJNewcornJSprichSComorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disordersAm J Psychiatry199114855645772018156
- IshiiTTakahashiOKawamuraYOhtaTComorbidity in attention deficit-hyperactivity disorderPsychiatry Clin Neurosci200357545746312950698
- FaraoneSVBiedermanJMonuteauxMCAttention deficit hyperactivity disorder with bipolar disorder in girls: further evidence for a familial subtype?J Affect Disord2001641192611292516
- Wilder-WillisKESaxKWRosenbergHLFleckDEShearPKStrakowskiSMPersistent attentional dysfunction in remitted bipolar disorderBipolar Disord200132586211333063
- PetersonBSLeckmanJFThe temporal dynamics of tics in Gilles de la Tourette syndromeBiol Psychiatry19984412133713489861477
- PetersonBSPineDSCohenPBrookJSProspective, longitudinal study of tic, obsessive-compulsive, and attention-deficit/hyperactivity disorders in an epidemiological sampleJ Am Acad Child Adolesc Psychiatry200140668569511392347
- WalshTMenvielleEDisorders of EliminationWienerJMDulcanMKTextbook of Child and Adolescent Psychiatry3rd edWashington, DCAmerican Psychiatric Publishing, Inc2004743750
- EspositoMGallaiBParisiLPrimary nocturnal enuresis as a risk factor for sleep disorders: an observational questionnaire-based multicenter studyNeuropsychiatr Dis Treat2013943744323579788
- EspositoMGallaiBParisiLVisuomotor competencies and primary monosymptomatic nocturnal enuresis in prepubertal aged childrenNeuropsychiatr Dis Treat2013992192623847418
- RobsonWLJacksonHBlackhurstDLeungAKEnuresis in children with attention-deficit hyperactivity disorderSouth Med J19979055035059160067
- BaileyJNOrnitzEMGehrickeJGGabikianPRussellATSmalleySLTransmission of primary nocturnal enuresis and attention deficit hyperactivity disorderActa Paediatr199988121364136810626523
- LaheyBBPelhamWESchaughencyEADimensions and types of attention deficit disorderJ Am Acad Child Adolesc Psychiatry19882733303353379015
- KaufmanJBirmaherBBrentDSchedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity dataJ Am Acad Child Adolesc Psychiatry19973679809889204677
- GöklerBÜnalFPehlivantürkBKültürEÇAkdemirDTanerYReliability and Validity of Schedule for Affective Disorders and Schizophrenia for School Age Children-Present and Lifetime Version-Turkish Version (K-SADS-PL-T)Turk J Child Adolesc Ment Health2004113109116
- WillcuttEGThe prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic reviewNeurotherapeutics20129349049922976615
- ByunHYangJLeeMPsychiatric comorbidity in Korean children and adolescents with attention-deficit hyperactivity disorder: psychopathology according to subtypeYonsei Med J200647111312116502492
- GaubMCarlsonCLGender differences in ADHD: a meta-analysis and critical reviewJ Am Acad Child Adolesc Psychiatry1997368103610459256583
- AugustGJRealmutoGMMacDonaldAWNugentSMCrosbyRPrevalence of ADHD and comorbid disorders among elementary school children screened for disruptive behaviorJ Abnorm Child Psychol19962455715958956085
- The MTA Cooperative GroupA 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorderArch Gen Psychiatry199956121073108610591283
- WilensTEBiedermanJBrownSTanguaySMonuteauxMCBlakeCPsychiatric comorbidity and functioning in clinically referred preschool children an school age youths with ADHDJ Am Acad Child Adolesc Psychiatry200241326226811886020
- BeckerSPLangbergJMVaughnAJEpsteinJNClinical utility of the Vanderbilt ADHD diagnostic parent rating scale comorbidity screening scalesJ Dev Behav Pediatr201233322122822343479
- BeckerSPLuebbeAMLangbergJMCo-occurring mental health problems and peer functioning among youth with attention-deficit/hyperactivity disorder: a review and recommendations for future researchClin Child Fam Psychol Rev201215427930222965872
- HinshawSPPreadolescent girls with attention-deficit/hyperactivity disorder: I. Background characteristics, comorbidity, cognitive and social functioning, and parenting practicesJ Consult Clin Psychol20027051086109812362959
- StrayhornJMBickelDDReduction in children’s symptoms of attention deficit hyperactivity disorder and oppositional defiant disorder during individual tutoring as compared with classroom instructionPsychol Rep2002911698012353805
- HaradaYYamazakiTSaitohKPsychosocial problems in attention-deficit hyperactivity disorder with oppositional defiant disorderPsychiatry Clin Neurosci200256436536912109953
- BiedermanJFaraoneSMilbergerSPredictors of persistence and remission of ADHD into adolescence: results from a four-year prospective follow-up studyJ Am Acad Child Adolesc Psychiatry19963533433518714323
- BurtSAKruegerRFMcGueMIaconoWGSources of covariation among attention-deficit/hyperactivity disorder, oppositional defiant disorder, and conduct disorder: the importance of shared environmentJ Abnorm Child Psychol20011104516525
- BiedermanJMickEFaraoneSVDepression in attention deficit hyperactivity disorder (ADHD) children: “true” depression or demoralization?J Affect Disord1998471–31131229476751
- SchatzDBRostainALADHD with comorbid anxiety: a review of the current literatureJ Atten Disord200610214114917085624
- PlizskaSRAttention Deficit/Hyperactivity DisorderDulcanMKDulcan’s Textbook of Child and Adolescent PsychiatryWashington, DCAmerican Psychiatric Publishing, Inc2010205222
- CohenRLohrIPaulRBolandRImpairments of attention and effort among patients with major affective disordersJ Neuropsychiatry Clin Neurosci200113338539511514646
- PearsonDASantosCWRoacheJDTreatment effects of methylphenidate on behavioral adjustment in children with mental retardation and ADHDJ Am Acad Child Adolesc Psychiatry200342220921612544181
- O’BrienLMIvanenkoACrabtreeVMSleep disturbances in children with attention deficit hyperactivity disorderPediatr Res200354223724312736394
- FaraoneSVBiedermanJDo attention deficit hyperactivity disorder and major depression share familial risk factors?J Nerv Ment Dis199718595335419307614
- GellerDACoffeyBFaraoneSDoes comorbid attention-deficit/hyperactivity disorder impact the clinical expression of pediatric obsessive-compulsive disorder?CNS Spectr20038425926412679741
- BiedermanJRussellRSorianoJWozniakJFaraoneSVClinical features of children with both ADHD and mania: does ascertainment source make a difference?J Affect Disord199851210111210743843
- FaraoneSVBiedermanJMenninDWozniakJSpencerTAttention-deficit hyperactivity disorder with bipolar disorder: a familial subtype?J Am Acad Child Adolesc Psychiatry1997361013781387 discussion 1387–13909334551