Abstract
Fibromyalgia is associated with an increased rate of mortality from suicide. In fact, this disease is associated with several characteristics that are linked to an increased risk of suicidal behaviors, such as being female and experiencing chronic pain, psychological distress, and sleep disturbances. However, the literature concerning suicidal behaviors and their risk factors in fibromyalgia is sparse. The objectives of the present study were to evaluate the prevalence of suicidal ideation and the risk of suicide in a sample of patients with fibromyalgia compared with a sample of healthy subjects and a sample of patients with chronic low-back pain. We also aimed to evaluate the relevance of pain intensity, depression, and sleep quality as variables related to suicidal ideation and risks. Logistic regression was applied to estimate the likelihood of suicidal ideation and the risk of suicide adjusted by age and sex. We also used two logistic regression models using age, sex, pain severity score, depression severity, sleep quality, and disease state as independent variables and using the control group as a reference. Forty-four patients with fibromyalgia, 32 patients with low-back pain, and 50 controls were included. Suicidal ideation, measured with item 9 of the Beck Depression Inventory, was almost absent among the controls and was low among patients with low-back pain; however, suicidal ideation was prominent among patients with fibromyalgia (P<0.0001). The risk of suicide, measured with the Plutchik Suicide Risk Scale, was also higher among patients with fibromyalgia than in patients with low-back pain or in controls (P<0.0001). The likelihood for suicidal ideation and the risk of suicide were higher among patients with fibromyalgia (odds ratios of 26.9 and 48.0, respectively) than in patients with low-back pain (odds ratios 4.6 and 4.7, respectively). Depression was the only factor associated with suicidal ideation or the risk of suicide.
Introduction
Two large population-based studies, one from Denmark and one from the United States, have shown that fibromyalgia is associated with an increased frequency of death from suicide.Citation1–Citation2 A later study, performed in Spain, also showed a high frequency of previous suicide attempts among patients with fibromyalgia.Citation3
Pain is the cardinal symptom of fibromyalgia, and chronic pain has been related to an increased probability of suicidal behaviors (ie, suicidal ideation, suicide attempts, and completed suicide).Citation4,Citation5 It is also important to remember that most patients with fibromyalgia also suffer from sleep disturbancesCitation6 and symptoms of psychological distress, such as anxiety and depression,Citation7 and that both depression and sleep alterations are factors that are strongly associated with the likelihood of suicide.Citation8,Citation9 In addition, female sex is also a predisposing factor to suicide,Citation8 and fibromyalgia is a pathology that is more common in women than in men.Citation10 Thus, many patients with fibromyalgia may present several risk factors for suicide.
Although the literature concerning chronic pain and suicidality is ample, the prevalence of suicidal behaviors among patients with fibromyalgia and the specific relevance of factors predisposing patients to these behaviors have scarcely been investigated, which is in contrast with other types of chronic pain, such as headaches, migraines, arthritis, back pain, bladder pain, or irritable bowel syndrome. Among four recent population-based studies that examined the association between chronic pain and suicidal behaviors,Citation11–Citation14 only two included patients with fibromyalgia.Citation11,Citation14
The main objective of the present study was to evaluate suicidal ideation and the risk of suicide in a sample of patients with fibromyalgia and to compare these patients with a sample of control subjects from the general population as well as with a sample of patients with low-back pain, which represents a condition that involves chronic pain that is frequently found in clinical practice and that has been associated both with depressionCitation15,Citation16 and with sleep disturbances.Citation17,Citation18 A secondary objective was to compare depression, sleep quality, and pain intensity in the three samples as variables that may be relevant to suicidal behaviors.
Patients and methods
Subjects
The inclusion criteria were: age ≥18 years old, an understanding of the requirements of the study, and providing written informed consent. Patients with fibromyalgia were diagnosed according to the American College of Rheumatology 1990 criteria.Citation19 Patients with low-back pain had to have experienced constant or intermittent nonspecific low-back pain for at least the last 3 months. Exclusion criteria for patients included any mental disorder other than the symptoms of depression. Patients were recruited in a primary care center; those patients who had been diagnosed with fibromyalgia or low-back pain were invited to participate in the study. They were informed that the objective of the study was to examine the relationship between suicidal ideation and chronic pain. Those who accepted were examined to evaluate whether they fulfilled the inclusion and exclusion criteria and were then given the questionnaire. Controls were recruited from the friends and colleagues of the investigators; they were included if they did not suffer from a mental disorder or from chronic pain. To preserve the anonymity of the answers, the subjects were instructed to send the completed questionnaires by mail or to deliver them in a sealed envelope.
The recruited participants were given a case report form that included questions concerning sociodemographic data (age, sex, education level, and marital and employment status) and the various outcome measures described below.
The study protocol was approved by the Ethics Committee of the Hospital Universitario Virgen de las Nieves of Granada (Spain).
Methods
Suicidal ideation was evaluated according to the answer given to question 9 of the Beck Depression Inventory (BDI). The BDI is a widely used self-assessment on a 21-item scale that has a maximum total score of 63; higher scores indicate an increased severity of depression. Item 9 can be scored as: 0 (“I don’t have any thoughts of harming myself”), which is considered to be the absence of suicidal ideation; 1 (“I have thoughts of harming myself but I would not carry them out”), which is considered to be passive suicidal ideation; 2 (“I would like to kill myself”); or 3 (“I would kill myself if I had the chance”), which is considered to be active suicidal ideation. Depression severity was measured by the BDI total score after subtracting the value for item 9 to measure the severity of depression independent of suicidal ideation; this approach avoids the artificial inflation of depression scores by this item and has been used in other studies that have evaluated suicidal ideation in patients with chronic pain.Citation20–Citation22 Clinically relevant depression was considered to be present when the total BDI scores were ≥18 points. We used the Spanish validated version of the BDI that was assessed in a sample of 445 Spaniards, which showed good internal consistency (Cronbach’s alpha: 0.83).Citation23
The risk of suicide was measured with the Plutchik Suicide Risk Scale. This scale is a 15-item self-reported measure designed to describe the degree to which an individual reveals characteristics that are similar to those consistent with suicidal behavior; each question is scored as one point, to a maximum of 15. We used the Spanish validated version that was assessed in 672 Spaniards: 35% of the participants had a history of a previous suicide attempt, 17% had been diagnosed with antisocial or borderline personality disorder, and 48% came from the general population. This version showed an internal consistency of 0.9 (Cronbach’s alpha) and a test–retest reliability of 0.89 (Pearson’s correlation); the cutoff point that indicated a substantial suicide risk was established as 6 points.Citation24
Sleep was evaluated with the Pittsburgh Sleep Quality Index (PSQI), which is a self-reported scale that has a maximum value of 21, with high values indicating worse sleep quality; the cutoff point for poor sleep quality is 5. We used the Spanish validated version, which was assessed in two samples: one of 181 students and another of 393 patients. Its internal consistency was 0.81 (Cronbach’s alpha); it showed a sensitivity of 88.63% and a specificity of 74.99%, with a Kappa coefficient of 0.61.Citation25
Pain intensity was measured by the Brief Pain Inventory (BPI), which is a self-reported scale that measures both pain intensity and pain interference with daily activities on a visual analog scale ranging from 0 to 10; high values indicate higher levels of pain severity and interference. We used the Spanish validated version, which was assessed in 126 patients suffering from pain related to cancer; it showed an internal consistency of 0.87 for pain intensity and of 0.98 for pain interference (Cronbach’s alpha). The test–retest reliability was 0.53 and 0.77, respectively (Spearman’s correlation).Citation26
General health status was measured by the Short-Form Health Survey SF-12; this scale provides a physical component summary and a mental component summary, with higher scores indicating a better health status. We used the Spanish validated version, which was assessed in two wide samples of Spaniards (N=1,579 and N=1,798, respectively); it showed an internal consistency of 0.94 for the physical component summary and of 0.9 for the mental component summary (Cronbach’s alpha).Citation27
Data analysis
Raw data from patients with fibromyalgia, patients with low-back pain, and controls were compared with the Kruskal–Wallis test for a global comparison, with the Dunn’s test for multiple comparisons between groups for parametric data, and with a χ2 test for categorical data. We estimated the likelihood of suicidal ideation or the risk of suicide, adjusting for age and sex using logistic regression models. Similarly, to evaluate the predictive factors for the presence of suicidal ideation and the risk of suicide, we also used two logistic regression models, including age, sex, BPI severity score, BDI total score, PSQI total score, and disease state as independent variables, using the control group as a reference. Data were analyzed with SPSS Statistics (IBM Corporation, Armonk, NY, USA) software, version 20.
Results
A total of 126 subjects, 44 patients with fibromyalgia, 50 controls, and 32 patients with low-back pain, were included. All of the participants completed the BDI, the Plutchik scale, the PSQI, and the BPI, but ten (7.9%) had missing responses on the SF-12 questionnaire. Missing data were also found among the sociodemographic data shown in . Clinically relevant depression was found in two (4%) controls, 13 (41%) patients with low-back pain, and 40 (91%) patients with fibromyalgia (χ2: 72.03; P<0.0001). Poor sleep quality, indicated by PSQI scores above the cutoff point, was found in 22 (44%) controls, 26 (81.3%) low-back pain patients, and 38 (86.4%) patients with fibromyalgia (χ2: 22.73; P<0.0001).
Table 1 Sociodemographic data of the participants
shows the evaluated pain, depression, sleep quality, and physical and mental health status in the three studied groups. The mean pain intensity was similar in fibromyalgia and in low-back pain patients, although pain interference with daily activities was higher among patients with fibromyalgia (P<0.05 in relation to low-back pain patients). Total depression scores were highest among patients with fibromyalgia and were significantly different from those of both the controls and of patients with low-back pain (P<0.0001). Sleep quality was poor in fibromyalgia patients and in patients with low-back pain, although sleep quality was worse in fibromyalgia patients (P<0.05). Physical health was also poor in both patient groups (P<0.0001 in relation to controls), whereas the mental health status was similar in the controls and in patients with low-back pain and was significantly lower in patients with fibromyalgia (P<0.0001 in relation to the controls and P<0.01 in relation to patients with low-back pain).
Table 2 Differences between groups in total depression and sleep quality scores, mean pain intensity and severity, and physical and mental health components
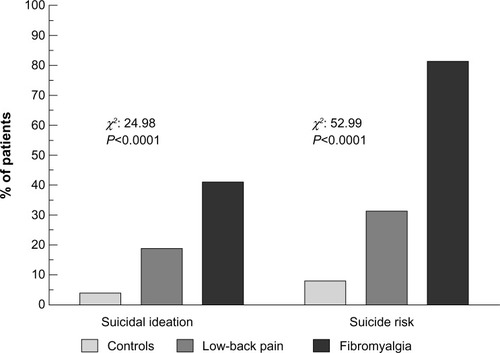
Suicidal ideation was almost completely absent among the controls, with only two (4%) subjects reporting passive suicidal ideation; was low among patients with low-back pain, with six (18.8%) patients reporting passive suicidal ideation; and was prominent among patients with fibromyalgia, with 18 (41%) patients reporting passive suicidal ideation and six (13.6%) patients reporting active suicidal ideation. The difference among the groups was highly significant (χ2: 24.98; P<0.0001) ().
The presence of the risk of suicide, as defined by the cutoff point on the Plutchik scale (6 points), was also higher among patients with fibromyalgia (N=36 [81.8%]), which was in contrast with patients with low-back pain (N=10 [31.3%]) and the controls (N=4 [8%]) (χ2: 52.99, P<0.0001) ().
When the data relative to suicidal ideation and the risk of suicide were adjusted in relation to patient age and sex, the likelihood of suicidal ideation and the risk of suicide in patients with fibromyalgia compared with controls was significantly increased. Among patients with low-back pain, the likelihood of suicidal ideation and the risk of suicide, although statistically significant, was substantially lower. The odds ratios (ORs) for both pathologies are shown in .
Table 3 ORs for suicidal ideation and for risk of suicide in both patient groups as compared with controls
In the predictive models, depression was the only factor associated both with suicidal ideation (OR 1.183, 95% confidence interval [CI] 1.068–1.311, P=0.001) and the risk of suicide (OR 1.159, 95% CI 1.046–1.283, P=0.005).
Discussion
Our data show that both suicidal ideation and the risk of suicide were higher in both patient groups compared with the controls, but they were highest in patients with fibromyalgia. Depression was the factor most strongly associated with both suicidal ideation and the risk of suicide. Examining the characteristics of both patient groups, it was apparent that pain intensity and physical health were similar but that the severity of depression and mental health status were significantly worse among patients with fibromyalgia. Sleep quality was poor in both groups but was worse among patients with fibromyalgia.
From our results, it can be argued that fibromyalgia is not associated with an increased risk of suicidal ideation by itself but is only associated with concomitant depression. This observation agrees with the observations of Ratcliffe et alCitation11 who found that fibromyalgia was positively associated with suicidal ideation and suicide attempts but that this association disappeared after adjusting the data for concomitant psychiatric comorbidity. Similar findings have also been recently reported by Ilgen et al.Citation13 In a previous study, we found that patients with fibromyalgia who had previously attempted suicide had depression scores that were significantly higher than those who did not attempt suicide.Citation3 Additionally, in a cross-sectional study evaluating the relationship between suicidal ideation and the symptoms of fibromyalgia, we found that among the symptoms that were related to suicidal ideation, depression showed the largest effect.Citation28 However, it is important to remember that fibromyalgia and depression are strongly related. Patients with fibromyalgia frequently suffer from a comorbid major depressive disorder, and the relatives of patients with fibromyalgia have been shown to experience depression at a frequency rate that is almost equal to those of relatives that suffer from depression.Citation29,Citation30 The hypothesis that fibromyalgia affects affective spectrum disorders is widely accepted, and both pathologies have been shown to share common pathophysiological mechanisms.Citation30,Citation31 Thus, the risk of suicidal behaviors (either suicidal ideation or suicide attempts) must be seriously considered by the attending physician when dealing with patients diagnosed with fibromyalgia, even if they have not been previously diagnosed with a major depressive disorder by a psychiatrist.
Although the sample of patients with chronic low-back pain in our study was included as a chronic pain group for comparative purposes, interesting considerations can be made from these findings. Depression has been found to be frequent among patients suffering low-back pain.Citation15,Citation32 Ilgen et alCitation14 found that back pain, together with migraines and psychogenic pain, was associated with an increased risk of death from suicide, a risk that persisted after adjusting the data for sociodemographic data and psychiatric comorbidity.
The main limitation of our study is the limited sample size, which was large enough to fulfill the first objective of our study but not large enough to adequately accomplish the second objective. A larger sample size would most likely be able to discriminate the relative weight of sleep disturbances and pain intensity in predicting suicidal ideation and the risk of suicide. An additional limitation is that the control group was significantly different from both patient groups; the controls had better education and employment statuses. Although we do not believe that this fact greatly influenced the results of this study, it is a selection bias that must be acknowledged. Additionally, we did not evaluate other factors that may have influenced our results, such as a family history of suicide, the existence of previous suicide attempts, and the duration of the disease. The first two factors are well known general factors for the predisposition of suicide,Citation8 whereas the last factor is pain-specific and has a relationship with suicidal behaviors that has not been thoroughly investigated. However, there is some evidence that suicidal ideation is more probable among patients with long-lasting pain than among those with recent-onset pain.Citation5 Additionally, this study was an exploratory study that aimed to evaluate suicidal ideation and risk in patients with fibromyalgia compared with healthy subjects and patients with low-back pain. As it was not possible to evaluate every factor that is potentially related to suicidal behaviors because of the limited sample size, we focused our attention on the factors thought to be most relevant to suicidal behaviors in chronic-pain patients, such as pain intensity, sleep disturbances, and mental health status.
Despite these limitations, we believe that our study provides relevant data that can be added to the growing body of evidence that links fibromyalgia with an increased risk of suicidal behaviors. This increased risk is mainly explained by the presence of depressive symptoms, highlighting the importance of adequately evaluating and treating the symptoms of depression.
Disclosure
The authors report no conflicts of interest in this work.
References
- DreyerLKendallSDaneskiøld-SamsoeBBartelsEMBliddalHMortality in a cohort of Danish patients with fibromyalgia: increased frequency of suicideArthritis Rheum201062103101310820583101
- WolfeFHassettALWalittBMichaudKMortality in fibromyalgia: a study of 8,186 patients over thirty five yearsArthritis Care Res201163194101
- CalandreEPVilchezJSMolina-BareaRSuicide attempts and risk of suicide in patients with fibromyalgia: a survey in Spanish patientsRheumatology201150101889189321750003
- FishbainDAThe association between chronic pain and suicideSemin Clin Neuropsychiatry19994322122710498789
- TangNKYCraneCSuicidality in chronic pain: a review of the prevalence, risk factors and psychological linksPsychol Med200636557558616420727
- MoldofskyHThe significance, assessment, and management of nonrestorative sleep in fibromyalgia syndromeCNS Spectrums2008135222618323770
- ArnoldLMClawDJMcCarbergBHImproving the recognition and diagnosis of fibromyalgiaMayo Clin Proc2011865456464
- NockMKBorgesGBrometEJCross-national prevalence and risk factors for suicidal ideation, plans and attemptsBr J Psychiatry200819229810518245022
- PigeonWRPinquartMConnerKMeta-analysis of sleep disturbance and suicidal thoughts and behaviorsJ Clin Psychiatry2012739e1160e116723059158
- QueirozLPWorldwide epidemiology of fibromyalgiaCurr Pain Headache Rep201317835623801009
- RatcliffeGEEnnsMWBelikSLSareenJChronic pain conditions and suicidal ideation and suicidal attempts: an epidemiological perspectiveClin J Pain200824320421018287825
- BradenJBSullivanMDSuicidal thoughts and behavior among adults with self-reported pain conditions in the national comorbidity survey replicationJ Pain20089121106111519038772
- IlgenMAZivinKMcCammonRJValensteinMPain and suicidal thoughts, plans and attempts in the United StatesGen Hosp Psychiatry200830652152719061678
- IlgenMAKleinbergFIgnacioRVNoncancer pain conditions and risk of suicideJAMA Psychiatry201370769269723699975
- SullivanMJLReesorKMikailSFisherRThe treatment of depression in chronic low back pain: review and recommendationsPain19925015131387469
- RushAJPolatinPGatchelRJDepression and chronic low back painSpine200025202566257111034638
- MartyMRozenbergSDuplanBThomasPDuquesnoyBAllaertFQuality of sleep in patients with chronic low back pain: a case-control studyEur Spine J200817683984418389288
- BahouqHAllaliFRkainHHmamouchiIHajjaj-HassouniNPrevalence and severity of insomnia in chronic low back pain patientsRheumatol Int20133351277128123124732
- WolfeFSmytheHAYunusMBThe American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the multicenter criteria committeeArthritis Rheum19903321601722306288
- SmithMTPerlisMLHaythornthwaiteJASuicidal ideation in outpatients with chronic musculoskeletal pain: an exploratory study of the role of sleep onset insomnia and pain intensityClin J Pain200420211111814770051
- SmithMTEdwardsRRRobinsonRCDworkinRHSuicidal ideation, plans, and attempts in chronic pain patients: factors associated with increased riskPain20041111–220120815327824
- KanzlerKEBryanCGMcGearyDDMorrowCESuicidal ideation and perceived burdensomeness in patients with chronic painPain Pract201212860260922429694
- VazquezCSanzJFiabilidad y valores normales de la versión española del inventario para la depresión de Beck de 1978Clín Salud199783403422
- RubioGMonteroIJaúreguiJValidación de la escala de riesgo de suicidio de Plutchik en la población españolaArch Neurobiol1998612143152
- RoyuelaAMacíasJAPropiedades clinimétricas de la versión castellana del cuestionario de PittsburghVigilia-Sueño1998928194
- BadiaXMurielCGraciaAValidación española del cuestionario Brief Pain Inventory en pacientes con dolor de causa neoplásicaMed Clin (Barc)20031202525912570914
- VilagutGValderasJMFerrerMGarinOLópez-GarcíaEAlonsoJInterpretación de los cuestionarios de salud SF-36 y SF-12 en España: componente físico y mentalMed Clin (Barc)2008130272673518570798
- CalandreEPNavajas-RojasMABallesterosJGarcia-CarrilloJGarcia-LeivaJMRico-VillademorosFSuicidal ideation in patients with fibromyalgia: a cross-sectional studyPain Pract Epub1172014
- RaphaelKGJanalMNNayakSSchwartzJEGallagherRMFamilial aggregation of depression in fibromyalgia: a community-based test of alternate hipothesesPain20041101–244946015275798
- PaeCULuytenPMarksDMThe relationship between fibromyalgia and major depressive disorder: a comprehensive reviewCur Med Res Opin200824823592371
- GracelyRHCekoMBushnellMCFibromyalgia and depressionPain Res Treat2012201248659022191023
- BenerAVerjeeMDafeeahEEPsychological factors: anxiety, depression, and somatization symptoms in low back pain patientsJ Pain Res201369510123403693