Abstract
Objective
The purpose of this study was to examine the effectiveness of group psychoeducation to relieve the psychological distress of mothers of children with high-functioning pervasive developmental disorders (HFPDD) and to improve the behaviors of the children.
Methods
Seventy-two mothers of preschool outpatients with HFPDD were randomly assigned to a four-session brief group psychoeducational program (GP). The sessions were held every second week in addition to the usual treatment (GP + treatment as usual [TAU] group), or to a TAU-alone group. The primary outcome was self-reported symptoms of maternal mental health as assessed using the 28-item General Health Questionnaire (GHQ-28) at 21 weeks post-randomization (week 21). The GHQ-28 at the end of the intervention (week 7), Aberrant Behavior Checklist (ABC) for the behavior of the children, the Zarit Burden Interview (ZBI), and the Medical Outcomes Study 36-item Short Form Health Survey (SF-36) were carried out at weeks 7 and 21. We tested the group effects with the interaction between the intervention and the evaluation points.
Results
The GHQ-28 score at week 21 was significantly higher in the GP + TAU group as compared to that in the TAU-alone group, indicating a greater improvement in the TAU-alone group. There was no evidence that GP + TAU led to a greater improvement of maternal mental health than TAU-alone at week 7. Similarly, no evidence was obtained to indicate that GP + TAU led to a reduction in the ABC or ZBI scores by week 7 or 21. The adjusted scores for the RF (role emotional) and MH (mental health) subscales of the SF-36 at week 21 were also significantly lower in the GP + TAU group, indicating a similar tendency to that of the change of the GHQ-28 score at week 21.
Conclusion
The psychoeducational program did not alleviate maternal distress, aberrant behaviors of the children, or caregiver burden.
Introduction
Pervasive developmental disorder (PDD) is defined by its unique symptoms, namely, qualitative impairments in social interaction and communication, and restricted repetitive and stereotyped patterns of behavior and interest.Citation1 The reported prevalence of PDD is <2%.Citation2,Citation3
Recently, research has progressed in the field of high-functioning PDD (HFPDD). Although patients with HFPDD have normal intelligence, their poor communication abilities or repetitiveness often impair their social functioning in school or in society.Citation4 Moreover, they are often stigmatized as ill-disciplined or wayward children by the community because of their normal intelligence and the absence of distinctive physical features.Citation5 Children with PDD are commonly recognized by parents during early childhood,Citation6 although Howlin et al reported that children with Asperger’s disorder were diagnosed at a mean age of 11 years.Citation7 These children are at a higher risk for comorbid psychiatric disorders after puberty.Citation8,Citation9 Therefore, the development of reliable techniques for the diagnosis, training of affected children, and provision of family support is needed.
In addition to the many studies on PDD carried out in the fields of epidemiology and genetics,Citation2,Citation10–Citation12 several studies have focused on the distress of the mothers of children with PDD, who must deal with the atypical development of their children.Citation13–Citation16 Behavioral and emotional problems of children with PDD are associated with parental mental health and family functioning.Citation17 Some of these studies suggest that these stress levels are higher in the mothers than in the fathers.Citation15,Citation18 Daniels et al reported that depression was more common among mothers of children with PDD.Citation19 Existence of an association between maternal depression and a family history of PDD has also been indicated.Citation19,Citation20 Estes et al reported higher levels of parenting stress and psychological distress in mothers of an Autism Spectrum Disorder group when compared to those of a Developmental Delay group.Citation13 Therefore, management of the maternal distress arising from the children’s condition and exploration of methods to cope effectively with such stress are needed.
In several Western and Asian countries, researchers have investigated the effectiveness of various psychotherapeutic techniques, such as childcare counseling and education for mothers about how to treat their children with PDD.Citation21–Citation23 A meta-analysis by Singer et alCitation24 suggested the effects and significance of stress management interventions for the parents of children with developmental disabilities. In this meta-analysis, 17 studies reported that the effect size of behavioral and cognitive behavioral therapy interventions for the parents of children with developmental disabilities was 0.49. This indicates that it is effective in alleviating maternal depressive symptoms and psychological distress. However, in many of the studies included in the analysis, long-term interventions were needed and a considerable number of participants dropped out of the interventions.
Family psychoeducation has become established as an effective intervention in psychiatric patients. Such education was originally developed for patients with psychotic disorders and it successfully reduced the relapse rate of psychotic symptoms.Citation25,Citation26 The meta-analysis by Henken et al reported good effects on decreasing depression and on increasing family functioning.Citation27
Our group reported the effect of brief psychoeducational intervention programs for the relatives of patients with depressive disorder in relieving the caregivers’ expressions of emotion, psychosocial burden, anxiety, and depressive moods.Citation28 The study suggested that family psychoeducation has the potential to maintain the well-being of not only the patients, but also of their families. Recently, psychoeducation has been widely applied to other mental disorders, such as anorexia nervosaCitation29 and dementia.Citation30 However, to the best of our knowledge, few studies have shown the effectiveness of family interventions for PDD in Japan, despite the wide implementation of family psychoeducation using various approaches at medical centers and public health departments. New research may be needed to establish a rigorous evidence base for improving parental mental health and behavior of children with PDD. Although family psychoeducation has not yet been applied to PDD, its use as a therapeutic tool for this disorder is anticipated.
We hypothesized that brief psychoeducation programs for mothers, in addition to the usual treatment for their children, would be more effective for improving parental mental health and behavior of children with PDD than the usual treatment for the children alone. The purpose of this randomized controlled trial (RCT) was to examine the effectiveness of psychoeducation for alleviating the psychological distress of mothers of children with HFPDD and for improving the behavior of children with these traits.
Method
Participants
The trial was conducted from November 10, 2010, to July 31, 2012. At first, the trial was scheduled to be completed on December 31, 2011, but it was prolonged for 7 months more due to a delay in the enrollment of patients meeting the eligibility criteria. The mothers of outpatients at three psychiatric outpatient departments and one pediatric outpatient department in Japan were recruited as participants. The mothers were eligible for inclusion in the study if their child met the following criteria: 1) a diagnosis of autistic disorder, Asperger’s disorder, or pervasive developmental disorder not otherwise specified made by a child psychiatrist or developmental pediatrician according to the Diagnostic and Statistical Manual (DSM-IV-TR); 2) no intellectual disabilities with an intelligence quotient (IQ) or developmental quotient (DQ) of >70; 3) aged 2–6.5 years; 4) diagnosis made more than 3 months previously; 4) entry to an elementary school scheduled more than 6 months later; and 5) a native Japanese speaker. Furthermore, only birth mothers who were actively involved in raising their child were enrolled. The exclusion criteria were: 1) inability to understand the study contents or anticipation of an excessive burden on the potential participant for any reason; or 2) assessed as being an unsuitable candidate for participation in this study for any reason by the doctors of the affected child, who are independent of study intervention. We assumed a case with aggravated harassment, for example, as an unsuitable participant.
Enrollment and baseline characteristics of the patients
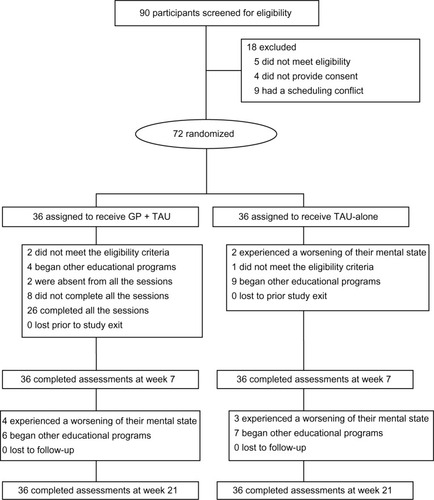
Ninety mothers were screened, and 72 satisfied the eligibility criteria; of the 72, 36 participants were randomly assigned to receive GP + TAU therapy and 36 to receive TAU therapy alone (). There were not any ineligible cases which were deemed as unsuitable candidates for participation due to the exclusion criteria. We found after randomization that three participants had not met inclusion criteria because of their children’s condition. One patient in the GP + TAU group and one in the TAU-alone group had an IQ slightly lower than 70, and another in the GP + TAU was diagnosed within 3 months from randomization. Although these problems were caused by careless checking, we estimated that it would have a small influence on the outcome.
Study design
This was a multicenter, individually randomized, parallel-group study.
Randomization was stratified individually according to the total scores on the 28-item General Health Questionnaire (GHQ; under or over 15) and the Japanese version of the Aberrant Behavior Checklist (ABC; under or over 60). It was expected that the responsiveness of the participants to psychoeducation would differ depending on the baseline mental health of the mother and the degree of severity of the behavioral problems of the child, and stratified randomization was performed so that these factors were equally distributed in both groups. An independent statistician generated the random allocation sequences using a computer and variable blocks. Allocation concealment was maintained by numbering the participants, and only the allocation practitioner was informed of the code numbers. The allocation sequences were kept centrally, and the allocation was manually distributed to each site.
In this parallel-group study, the mothers of the patients were randomly assigned to a brief group psychoeducational program (GP) in addition to the usual treatment for their children (GP + TAU) or a TAU-alone group.
Because of the nature of psychotherapy, neither the patients nor their children’s physicians were blinded to the allocation group.
Assessment measures
Measures of parental mental health, quality of life, burden of providing care, and the behavioral problems of the child were assessed at the baseline, post-treatment (week 7), and at 14 weeks after the completion of treatment (week 21). Participants who dropped out of the intervention were asked to complete the assessments.
The primary efficacy parameters were the total score on the GHQ-28 at week 21 adjusted according to the baseline score.
GHQ-28
The GHQ-28 is a self-reported questionnaire used to detect psychiatric disorders in community settings.Citation31 We used this measure to assess maternal mental health. The 28-item version is composed of four subscales: somatic symptoms, social dysfunction, anxiety and insomnia, and severe depression.Citation32 The scores on the GHQ range from 0 to 28, with higher scores indicating a poorer mental health state.
The Japanese version has shown good reliability and validity in the general population of Japan.Citation33
Japanese version of the ABC
The ABC is an empirically derived psychometric instrument used to rate the inappropriate and maladaptive behaviors of mentally handicapped people.
This scale was originally developed for institutionalized, low-functioning adolescents and adults. Later, it was widely used to evaluate the behavior of autistic children.Citation34,Citation35
The checklist is composed of five factors: 1) irritability, agitation, and crying; 2) lethargy and social withdrawal; 3) stereotypic behavior; 4) hyperactivity and non-compliance; and 5) inappropriate speech.
The items in the ABC are rated on a four-point scale (0= never to 3= very often), and the scores on the ABC range from 0 to 174. The reliability and validity of the Japanese version of the ABC have been reported by Ono et al.Citation36
Japanese version of the Zarit Caregiver Burden Interview (ZBI)
Caregiver burden was assessed using the ZBI, which evaluates the physical, psychological, and social consequences of caring activities and has been widely used to assess the burden of caregivers.Citation37,Citation38 The Japanese version of the ZBI was developed by Arai.Citation33,Citation39 The Japanese ZBI has been demonstrated to have high test–retest reliability (r=0.76) and internal consistency. The Cronbach’s α for the ZBI was 0.93.
The items in the ZBI are rated on a five-point Likert scale (0= best to 4= worst), and the scores on the ZBI range from 0 to 88. Higher scores indicate a heavier caregiver burden.
Medical Outcomes Study 36-item Short-form Health Survey (SF-36; v2)
The SF-36 is a self-reported questionnaire used to assess general quality of life. It contains 36 items that constitute eight measures of physical functioning (PF), role limitations due to physical problems (RP), bodily pain (BP), social functioning (SF), general health perceptions (GH), vitality (VT), role limitations due to emotional problems (RE), and mental health (MH). It also provides two summary measures, the physical component summary (PCS) and the mental component summary (MCS). The PCS is associated with the PF, RP, BP, GH, and VT. The MCS is associated with the MH, RE, SF, VT, and GH. The score of each measure ranges from 0 to 100, and the higher the score, the higher the quality of life. The Japanese version has shown good validity in the general population of Japan.Citation40,Citation41
Sample size
Because this study was the first pilot trial to examine the effect of a brief psychoeducational program for mothers of children with HFPDD, we determined the sample size by referring to our previous researchCitation28 for the relatives of patients with depressive disorder. In this study, we executed brief psychoeducation with four biweekly sessions and its effect size was 1.0. We also referred to earlier researchCitation23,Citation24 with medium effect sizes, which had common factors such as group cognitive behavioral therapy and aimed at alleviating distress of parents of children with developmental disabilities. We then decided the hypothetical effect size was 0.70. We used the statistical software STATA (v12; StataCorp, College Station, TX, USA)Citation45 to calculate the sample size. To obtain a power of 0.8 to detect a significant difference at P=0.05 (two-sided), it was calculated that at least 32 patients were needed for each study arm. Thus, allowing for a 10% dropout or ineligibility rate, 36 participants would need to be recruited per group.
Trial interventions
The treatment regimen for the psychoeducation program used in the present study was developed and structured based on the McFarlane Model,Citation42 the Evidence-Based Practices Toolkit for Family Psycho-Education,Citation43 and the standard model of the Japanese Network of Psychoeducation and Family Support program.Citation44 In our previous study, we reported the effect of brief psychoeducational intervention programs with four biweekly sessions for the relatives of patients with depressive disorder in relieving the caregivers’ expressions of emotion, psychosocial burden, anxiety, and depressive moods.Citation28
We tried to apply this program to families with HFPDD children.
The psychoeducational program consisted of four sessions, each session lasting for 120 minutes and held every second week. In the intervention group, the number of participants in each program ranged from 3–5 and each session was conducted by a multidisciplinary group, consisting of at least three members: 1–2 psychiatrists, 0–2 nurses, 0–1 psychologist, 0–2 speech pathologists, and 0–1 social worker. At least one therapist in the group had participated in intensive training conducted by the Japanese Network of Psychoeducation and Family Support program.
During the first 60 minutes of each session, therapists presented information to the participants on the contents of 1) the characteristics of pervasive developmental disorders; 2) how to treat their children considering the individual characteristics of their children; 3) information about social support resources and preparation for admission into elementary school; 4) the physical and mental health of the mother herself. During the latter 60 minutes, supportive group therapy was provided focusing on problem-solving skills. We conducted these group sessions based on the structures shared by the standard model of the Japanese Network of Psychoeducation and Family Support program. TAU was defined as consultation with a licensed child psychiatrist or developmental pediatrician at least every 6 months. We had two evaluation points, at 7 weeks post-randomization at which the intervention of four sessions had finished (week 7), and at 21 weeks post-randomization (week 21). Participants of both groups made an appointment with evaluators and came to the hospital at week 7 and 21.
Statistical analysis
Descriptive and inferential statistics were computed using SPSS for Windows (v17.0; SPSS, Inc., Chicago, IL, USA).Citation45 We planned to conduct a preplanned analysis by the trial steering committee.
All the analyses were conducted using an intention-to-treat approach. The statistician of this study was blinded to allocations.
1. Analysis of primary efficacy
We conducted unpaired t-tests calculated from the actual measured value of the GHQ-28 score at weeks 7 and 21. We first examined the time by treatment interaction in the linear mixed model. When this interaction was significant, we examined the GHQ28 scores between the intervention and the control groups while controlling for the baseline scores as covariant in analysis of covariance (ANCOVA) at 7 and 21 weeks. A P-value <0.05 was set to test the null hypothesis using a two-sided test.
When missing data were observed, we planned to use multiple imputation to complement the data with SPSS missing values and conducted a completer analysis, evaluating the robustness of the analysis results with regard to the missing data.
2. Analysis of secondary efficacy
The total scores of ABC and ZBI, and each domain of SF-36 were also analyzed using unpaired t-tests and ANCOVA at the same points. The mean and standard deviations of the number of attendants at each session in the intervention group and the proportion of subjects requiring an increased dosage of medication in both groups were also calculated.
Ethical considerations
This study was conducted with the approval of the Ethics Review Committee of Nagoya City University Graduate School of Medicine, Japan, on August 19, 2010, and in accordance with the principles laid down in the Helsinki Declaration. All participants provided written informed consent after the purpose and procedures of the study were explained. The study was registered on ClinicalTrials.gov (NLM identifier: NCT01243905) on November 8, 2010.
Results
summarizes the sociodemographic and clinical parameters at baseline. The randomized groups at trial entry did not exhibit statistical differences except in co-curricular training and therapy (P=0.029) and in the proportion of diagnosis of the children (P=0.026) by chi-square test.
Table 1 Baseline sociodemographic and clinical characteristics of participants
We had no missing data and all participants were included in the intention-to-treat analyses.
Primary outcome
Therapeutic effects with interactions between the intervention and evaluation points were compared between the groups by repeated-measures analysis of variance; an interaction was significant with the GHQ (P=0.01) and the RE subscale of SF-36 (P=0.01).
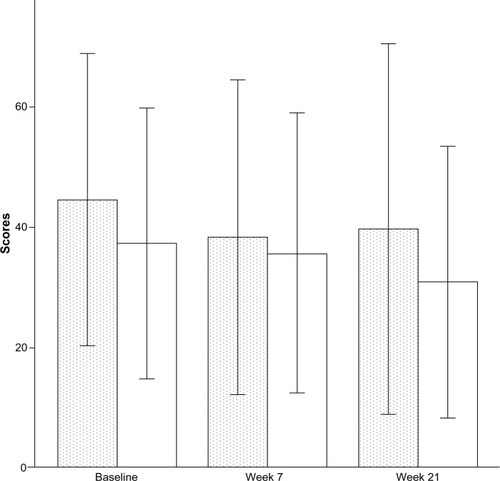
The primary statistical analysis was carried out using an unpaired t-test, then analysis of covariance (ANCOVA) was used according to the study plan (). The intervention group had a higher total GHQ-28 score at week 21, indicating poorer mental health, after adjustments for group differences in the baseline GHQ-28 scores (P=0.046; ). The intervention group reported a slightly lower score at week 7, although there was no evidence that the participants in the intervention group had better outcomes. No evidence was found indicating greater improvement of mental health in the intervention group.
Figure 2 Total scores of the 28-item General Health Questionnaire at baseline, week 7, and week 21.
Abbreviations: GP, group psychoeducational program; TAU, treatment as usual.
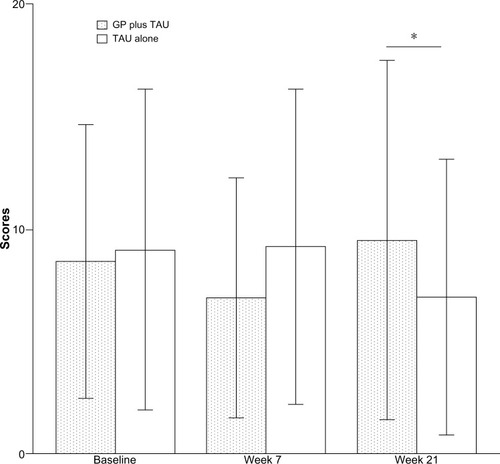
Table 2 Results of primary outcome
Secondary outcome
and present the results of the secondary outcome. The data included two follow-up points. No differences in the ABC () or ZBI scores were seen between the two groups during the period of the study. The intervention group had significantly lower adjusted scores for the RE and MH subscales of SF-36 at week 21.
Table 3 Results for each secondary outcome measure with unpaired t-test
Table 4 Adjusted results for each secondary outcome measure
We conducted post-hoc analyses which compared the completers in the intervention group with those in the control group (). The results did not change and in the MH subscale of SF-36 at week 7, the intervention group had significantly lower adjusted scores, indicating poorer mental health.
Table 5 Completer analysis
Attrition and study integrity
Ten participants in the GP + TAU group did not complete all the sessions because of scheduling conflicts, change of abode, and impact of childbirth, but no participants withdrew their enrollment in this study.
Two of the participants in the intervention group discontinued intervention. They were absent from all interventional programs because they had scheduling conflicts but received evaluation at week 7 and week 21. As shown in , all participants who were randomized were assessed at week 7 and week 21. All the study assessments were completed in the participants. The lecture contents of the group psychoeducational program were manualized, and all the participants in the group psychoeducational program used the same handouts.
Attendance of programs
The mean attendance number (SD) of the programs was 3.3 (1.26).
Proportion of increase in the medication dosage for the mothers
By week 7, the mental state of two of the mothers in the control group had worsened, and these participants were begun on prescription drugs or advised to visit a hospital. By week 21, the mental states of another three mothers in the control group and four mothers in the intervention group had worsened. One participant in the control group had suicidal ideation, but we determined that she would be able to undergo the assessments in this study after receiving adequate treatment from her doctor.
Co-intervention
Four mothers in the GP + TAU group and nine in the TAU-alone group had children who joined another educational program between baseline and week 7; six mothers in the GP + TAU group and seven mothers in the TAU-alone group had children who joined another education program between week 7 and week 21. Only one child in the GP + TAU group began taking medication during the study period. These mothers voluntarily participated in programs at the other facilities, and these co-interventions deviated from the original protocol. However, we included the results of these mothers in the analysis because we gave priority to intention-to-treat analysis.
Discussion
Our results did not provide any evidence to suggest that the brief group psychoeducational program for the mothers of children with HFPDD resulted in any improvement in maternal mental health, caregiver burden, maternal quality of life, or aberrant behavior of the children at the 21-week follow-up point.
In a previous study, Tonge et al conducted an RCT of education and skills training programs and reported the effects of their intervention on the improvement of parental mental health at a 6-month follow-up.Citation46 A recently published meta-analysis of group-based parent-training programs in the Cochrane Database of Systematic ReviewsCitation47 suggested that these programs were statistically effective for improving parental psychosocial factors such as depression, anxiety, and distress post-intervention, but not over the long-term. Contrary to these reports, our results did not reveal any positive effects.
Although it is difficult to identify the exact cause of the worsening mental health in the interventional group, we list several factors that may be responsible for these results: 1) the number of sessions; 2) selection of assessment measures; 3) sample size calculation; 4) the contents and quality of programs; and 5) controlling bias and study conditions.
We additionally discuss below these shortcomings and limitations which might have led to these unexpected results.
First, the number of sessions should be considered. We performed four brief sessions after considering the cost–benefit ratio, although more than twelve sessions were originally recommended by the Family Psychoeducation Program Fidelity Scale.Citation43 The meta-analysis described in the Cochrane Database of Systematic ReviewsCitation47 included ten studies that included six or fewer sessions. Of these brief interventions, only two studies showed statistical improvements of confidence post-intervention and during a short-term follow-up period.Citation48,Citation49 Moreover, we only had four sessions for this intervention, so the absence of participants in one of the sessions could have a significant impact on the assessment of treatment effects.
Next, the optimal assessment measures may also need to be reconsidered. Whether the assessment measures and the timing of the assessments were appropriate has been questioned. We did not assess maternal confidence, which other brief parenting programs had been able to improve. This question may be a common concern for all family programs.
Third, if the sample size was larger and was decided on more rigorously, both groups should be evenly randomized and we might have achieved better results. The study design of RCTs is superior for controlling systematic errors and confounders. The difference of baseline characteristics between the two groups in co-curricular training and therapy might have impact on results.
On the other hand, the difference in the proportion of diagnosis of the children would not be important because in DSM-V, these diagnoses would be integrated into autism spectrum disorder.Citation50
We also complemented our insufficient pilot study data by referring to a previous study. Additionally, it would be better to implement a before–after study for estimating effect and sample sizes. We determined the appropriate sample size by using reference data from studies, and we report our results as pilot data.
Fourth, we might have gained better results if we had measured the fidelity of the contents of our programs more rigorously to improve the quality and reproducibility by randomly checking recorded sessions. We did not use the fidelity checklist (the Family Psychoeducation Program Fidelity Scale);Citation43 therefore, we insured alternative fidelity by the attendance of trained therapists at all the interventional sessions, but there was room for improvement.
Fifth, we should reconsider implementing study protocol more strictly.
The fact that three-quarters of the participants’ children in co-curricular therapy were involved in other parent training programs might have some influence on results. At first, we allowed participants to pursue other treatments outside of the study because we aimed at implementing this study under pragmatic conditions. But the proportion of participants who did this was large and might also have contributed to the increase of joining other co-interventional treatments after randomization. Twenty-seven point seven percent in GP + TAU and 44.4% in TAU-alone participants began other educational programs, deviating from the original protocol. The proportion of these participants was large and could have caused the adverse results in this study.
Moreover, we did not perform a structured interview for the diagnosis of PDD in the children. Previous reports have indicated the difficulty in making a medical diagnosis of PDD,Citation51 but neither the Autism Diagnostic Interview-Revised (ADI-R)Citation52 nor the Autism Diagnostic Observation Schedule-Generic (ADOS-G)Citation53 are available in Japan. Other diagnostic instruments, such as the Childhood Autism Rating Scale (CARS),Citation54 are too lengthy for clinicians to complete because of the limited amount of time available. In the current study, child psychiatrists or developmental pediatricians diagnosed PDD in the children based on the DSM-IV-TR criteria to compensate for any diagnostic difficulties.
Other than these limitations, we attempted to infer meaning from these divergent results.
Our interventional sessions were completed within 7 weeks, and we assessed the participants at 21 weeks hoping to identify the long-term effects of the program. Contrary to our expectations at the follow-up assessment, the control group had a lower GHQ score, indicating that these mothers had greater well-being. A comprehensive overview of disability acceptance in parents reported by Nakata et al suggested that parents often experience confusion, depression, and anxiety.Citation55 The extra education alerted parents to the likely burden of illness on the children and families, a burden which may not have been so clear among the control group.
The family might have different perceptions about the gravity of diagnosis. There is a difference between depressive disorder and pervasive developmental disorder in prognosis. Depressive disorder is a treatable disease,Citation56 and it is reported that the overall cumulative remission rate is 67%. On the other hand, pervasive developmental disorder is a neurodevelopmental condition with early onset symptoms. The mother might feel seriously stressed knowing that the developmental disorder was not completely cured.
We also need to examine the heart of the matter that interventional programs can enhance maternal mental health. In a previous study on attitudes and coping with diseases, it was reported that patients fared better psychologically, behaviorally, and physiologically when the information they received about their medical condition was tailored to their own coping styles: generally those with a monitoring style tended to do better when given more information, and those with a blunting style did better with less information. This study also reported that patients with a monitoring style were more likely to be pessimistic about their future.Citation57 Many mothers of children with HFPDD might have a monitoring style, because completer analysis indicated that mothers with good adherence tended to be poorer in mental health; thus, it was natural for it to affect their mental health. We need to explore the traits of the mothers more closely and consider how to support them by tailoring programs to their own coping styles.
Despite the numerous programs used for mothers in various locations in Japan, this was the first RCT to evaluate structural psychoeducation programs for the mothers of children with HFPDD.
A RCT is an investigation method within a hierarchy of evidence, and we completed our study without any missing values. Although we obtained unexpected results, we completed our preplanned statistical analytical approach.
Despite the unexpected results, most of the participants supported this program and considered it to be helpful. Good adherence to the intervention supported the perceived acceptability of this approach.
In conclusion, this study revealed that adding a brief psychoeducational program for the mothers of children with HFPDD did not alleviate maternal distress or the aberrant behaviors of children with HFPDD. Further continuous and longitudinal attention to mothers, their children, and their families could lead to better interventions and a more complete awareness of their needs.
To develop this psychoeducation research, we should improve the quality and effectiveness of the contents of the intervention. We need to plan a qualitative study reviewing the limitations and agendas. Further research is required to explore what symptoms or psychosocial factors should be targeted in medical services for the mothers of children with HFPDD, the frequency and number of sessions, and what information is needed to make an adequate contribution to maternal well-being and the development of children with HFPDD. We also have to re-plan study conditions such as sampling and bias controlling. We will implement a before–after study next, preparing for a larger, rigorous clinical study.
Acknowledgments/disclosure
The authors are grateful to all the anonymous patients who participated in the trial. We also wish to thank all the therapists (Yuichi Kawamura, MD, PhD; Yuko Goto, MD; Fuminobu Imai, MD; Chie Nakamura, MD; Yuko Ishiguro, MSW; Yukari Shimada, BA; Miho Hagiwara, BA; Hiromi Taguchi, ST; Yasunori Goto, OT; Chikako Otaki, RN; Shoko Yoshimi, RN; and Natsuki Miwa, MAP); the administrative staff (Kaori Kobori and Kozue Maki at Nagoya City University Graduate School of Medical Sciences); the controller for data entry (Ms Kazuyo Mori); the members of the cognitive behavior therapy group and the child psychiatry group at Nagoya City University Graduate School of Medical Sciences (Sei Ogawa, MD, PhD; Masaki Kondo, MD; Akiko Kawaguchi, MD; Nao Shiraishi, MD; Shinkichi Maki, MD; and Mine Hirata, MD) for their valuable support throughout the research; and the supervisor of the additional statistical analysis (Hisashi Noma, MPH, DPH, The Institute of Statistical Mathematics). None of the acknowledged individuals have any financial or other conflicts of interest to report in relation to the subject of this article. The authors report no conflicts of interest in this work.
References
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR®)Washington, DCAmerican Psychiatric Association
- KimYSLeventhalBLKohYJPrevalence of autism spectrum disorders in a total population sampleAm J Psychiatry2011168990491221558103
- Prevalence of autism spectrum disorders – Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008MMWR Surveill Summ2012613119
- CottenceauHRouxSBlancRLenoirPBonnet-BrilhaultFBarthelemyCQuality of life of adolescents with autism spectrum disorders: comparison to adolescents with diabetesEur Child Adolesc Psychiatry201221528929622382494
- GillJLiamputtongPBeing the mother of a child with Asperger’s syndrome: women’s experiences of stigmaHealth Care Women Int201132870872221767096
- De GiacomoAFombonneEParental recognition of developmental abnormalities in autismEur Child Adolesc Psychiatry1998731311369826299
- HowlinPAsgharianAThe diagnosis of autism and Asperger syndrome: findings from a survey of 770 familiesDev Med Child Neurol1999411283483910619282
- SimonoffEPicklesACharmanTChandlerSLoucasTBairdGPsychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sampleJ Am Acad Child Adolesc Psychiatry200847892192918645422
- AbdallahMWGreaves-LordKGroveJNorgaard-PedersenBHougaardDMMortensenELPsychiatric comorbidities in autism spectrum disorders: findings from a Danish Historic Birth CohortEur Child Adolesc Psychiatry20112011–1259960121971944
- MizunoALiuYWilliamsDLKellerTAMinshewNJJustMAThe neural basis of deictic shifting in linguistic perspective-taking in high-functioning autismBrain2011134Pt 82422243521733887
- GomotMBelmonteMKBullmoreETBernardFABaron-CohenSBrain hyper-reactivity to auditory novel targets in children with high-functioning autismBrain2008131Pt 92479248818669482
- NakamuraKSekineYOuchiYBrain serotonin and dopamine transporter bindings in adults with high-functioning autismArch Gen Psychiatry2010671596820048223
- EstesAMunsonJDawsonGKoehlerEZhouXHAbbottRParenting stress and psychological functioning among mothers of preschool children with autism and developmental delayAutism200913437538719535467
- DavisNOCarterASParenting stress in mothers and fathers of toddlers with autism spectrum disorders: associations with child characteristicsJ Autism Dev Disord20083871278129118240012
- YamadaASuzukiMKatoMEmotional distress and its correlates among parents of children with pervasive developmental disordersPsychiatry Clin Neurosci200761665165718081627
- PottieCGIngramKMDaily stress, coping, and well-being in parents of children with autism: a multilevel modeling approachJ Fam Psychol200822685586419102606
- HerringSGrayKTaffeJTongeBSweeneyDEinfeldSBehaviour and emotional problems in toddlers with pervasive developmental disorders and developmental delay: associations with parental mental health and family functioningJ Intellect Disabil Res200650Pt 1287488217100948
- GrayDEGender and coping: the parents of children with high functioning autismSoc Sci Med200356363164212570979
- DanielsJLForssenUHultmanCMParental psychiatric disorders associated with autism spectrum disorders in the offspringPediatrics20081215e1357e136218450879
- GhaziuddinMA family history study of Asperger syndromeJ Autism Dev Disord200535217718215909404
- ShuBCLungFWThe effect of support group on the mental health and quality of life for mothers with autistic childrenJ Intellect Disabil Res200549Pt 1475315634311
- DrewABairdGBaron-CohenSA pilot randomised control trial of a parent training intervention for pre-school children with autism. Preliminary findings and methodological challengesEur Child Adolesc Psychiatry200211626627212541005
- McConachieHRandleVHammalDLe CouteurAA controlled trial of a training course for parents of children with suspected autism spectrum disorderJ Pediatr2005147333534016182672
- SingerGHEthridgeBLAldanaSIPrimary and secondary effects of parenting and stress management interventions for parents of children with developmental disabilities: a meta-analysisMent Retard Dev Disabil Res Rev200713435736917979202
- PharoahFMariJRathboneJWongWFamily intervention for schizophreniaCochrane Database Syst Rev201012CD00008821154340
- XiaJMerinderLBBelgamwarMRPsychoeducation for schizophreniaCochrane Database Syst Rev20116CD00283121678337
- HenkenHTHuibersMJChurchillRRestifoKRoelofsJFamily therapy for depressionCochrane Database Syst Rev20073CD00672817636850
- KatsukiFTakeuchiHKonishiMPre-post changes in psychosocial functioning among relatives of patients with depressive disorders after Brief Multifamily Psychoeducation: a pilot studyBMC Psychiatry2011115621477384
- FisherCAHetrickSERushfordNFamily therapy for anorexia nervosaCochrane Database Syst Rev20104CD00478020393940
- PerryMDraskovicILucassenPVernooij-DassenMvan AchterbergTRikkertMOEffects of educational interventions on primary dementia care: a systematic reviewInt J Geriatr Psychiatry201126111121157845
- GoldbergDPBlackwellBPsychiatric illness in general practice. A detailed study using a new method of case identificationBr Med J1970157074394435420206
- GoldbergDPHillierVFA scaled version of the General Health QuestionnairePsychol Med197991139145424481
- NaritaKThe factor structure of a General Health Questionnaire in a Japanese community sample-Using a 28-item versionJap J Gerontol19941622936
- MiralSGencerOInal-EmirogluFNBaykaraBBaykaraADirikERisperidone versus haloperidol in children and adolescents with AD: a randomized, controlled, double-blind trialEur Child Adolesc Psychiatry20081711818080171
- StiglerKADienerJTKohnAEAripiprazole in pervasive developmental disorder not otherwise specified and Asperger’s disorder: a 14-week, prospective, open-label studyJ Child Adolesc Psychopharmacol200919326527419519261
- OnoYFactor validity and reliability for the Aberrant Behavior Checklist-Community in a Japanese population with mental retardationRes Dev Disabil19961743033098827840
- MoriEIkedaMKosakaKDonepezil for dementia with Lewy bodies: a randomized, placebo-controlled trialAnn Neurol2012721415222829268
- LuchsingerJMittelmanMMejiaMThe Northern Manhattan Caregiver Intervention Project: a randomised trial testing the effectiveness of a dementia caregiver intervention in Hispanics in New York CityBMJ Open201225pii: e001941
- AraiYKudoKHosokawaTWashioMMiuraHHisamichiSReliability and validity of the Japanese version of the Zarit Caregiver Burden interviewPsychiatry Clin Neurosci19975152812879413874
- FukuharaSBitoSGreenJHsiaoAKurokawaKTranslation, adaptation, and validation of the SF-36 Health Survey for use in JapanJ Clin Epidemiol19985111103710449817121
- FukuharaSWareJEJrKosinskiMWadaSGandekBPsychometric and clinical tests of validity of the Japanese SF-36 Health SurveyJ Clin Epidemiol19985111104510539817122
- McFarlaneWRMultifamily Groups in the Treatment of Severe Psychiatric DisordersNew YorkThe Guilford Press2002
- US Department of Health and Human ServicesSubstance Abuse and Mental Health ServicesFamily Psychoeducation Evidence-Based Practices (EBP) KIT32010 Available at: http://store.samhsa.gov/product/Family-Psychoeducation-Evidence-Based-Practices-EBP-KIT/SMA09-4423Accessed March 20, 2014
- The standard model of the Japanese Network of Psychoeducation and Family Support Program Available at: http://jnpf.net/Accessed March 20, 2014 [Japanese]
- STATA 12 [computer program] Version 12TX, USAStata Corp2011
- TongeBBreretonAKiomallMMackinnonAKingNRinehartNEffects on parental mental health of an education and skills training program for parents of young children with autism: a randomized controlled trialJ Am Acad Child Adolesc Psychiatry200645556156916670650
- BarlowJSmailagicNHubandNRoloffVBennettCGroup-based parent training programmes for improving parental psychosocial healthCochrane Database Syst Rev20126CD00202022696327
- JoachimSSandersMRTurnerKMReducing preschoolers’ disruptive behavior in public with a brief parent discussion groupChild Psychiatry Hum Dev2010411476019633952
- WolfsonALacksPFuttermanAEffects of parent training on infant sleeping patterns, parents’ stress, and perceived parental competenceJ Consult Clin Psychol199260141481556284
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders, Fifth Edition, DSM-52013Washington, DCAmerican Psychiatric Association
- VentolaPEKleinmanJPandeyJAgreement among four diagnostic instruments for autism spectrum disorders in toddlersJ Autism Dev Disord200636783984716897398
- LordCRutterMLe CouteurAAutism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disordersJ Autism Dev Disord19942456596857814313
- LordCRisiSLambrechtLThe autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autismJ Autism Dev Disord200030320522311055457
- KuritaHMiyakeYKatsunoKReliability and validity of the Childhood Autism Rating Scale – Tokyo version (CARS-TV)J Autism Dev Disord19891933893962793784
- NakataYA parental response to having a child with developmental disorders: a stage model or chronic sorrow?Waseda Psychol Rep1995278392
- RushAJTrivediMHWisniewskiSRAcute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D reportAm J Psychiatry2006163111905191717074942
- MillerSMMonitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease. Implications for cancer screening and managementCancer19957621671778625088