Abstract
A 49-year-old man with mitochondrial disease presented with visual allesthesia, a rare and puzzling phenomenon. He was admitted for treatment because of convulsions. After the convulsions ceased, he exhibited left homonymous hemianopsia. Brain diffusion-weighted magnetic resonance imaging (MRI) showed a high-intensity area in the right occipital lobe. Both the hemianopsia and the MRI activation in this area disappeared by day 36 of hospitalization. On the morning of day 57, right homonymous hemianopsia emerged in a singular manner. The patient perceived an illusory object (a bottle placed by the bedside) in his left visual field, while the real object was in his blind right field. This case of visual allesthesia was accompanied by palinopsia, ie, perseveration of the image of the bottle. Diffusion-weighted MRI showed a new, high-intensity area in the left occipital lobe. We believe the visual allesthesia resulted from transfer of cortical information obtained by blindsight between hemispheres as a result of epileptic excitation.
Introduction
Allesthesia is a condition in which a stimulus is perceived at a location remote from its application. It is usually reported in association with somatic stimuli.Citation1 There is an early report of visual allesthesia by Beyer in 1895Citation2 and this case was introduced by Herrmann and Pötzl in 1928.Citation3 Following this early observation, we believe there have been at least seven other cases.Citation4–Citation10 The etiology is unknown, but possible links have been established with migraine,Citation2 arteriovenous malformation,Citation4–Citation6 meningioma,Citation7 metastatic brain tumor,Citation8 gunshot injury,Citation9 and neurocysticerosis.Citation10 Previously, no patient with both mitochondrial disease and visual allesthesia has been reported. Our patient who had mitochondrial disease, accompanied by hemianopsia, showed episodic visual allesthesia in which objects on his blind side were perceived contralaterally. Furthermore these contralateral, “ghost” perceptions were followed by palinopsia, or visual perseveration. We considered the possible pathophysiology of visual allesthesia in this patient.
Case report
A 49-year-old man was admitted to our hospital because of convulsions. At age 35, he had been diagnosed with diabetes mellitus and began to take oral anti-diabetic drugs. He also received surgical replacement of the intraocular lenses due to bilateral juvenile cataracts. At age 46, his first generalized convulsion occurred, and he was diagnosed with cerebellar ataxia with arteriovenous malformation in the cerebellar vermis. Following this, he took phenobarbital and zonisamide, but experienced generalized convulsions five to ten times a year. The arteriovenous malformation was treated with gamma knife within 6 months of diagnosis, and gradually reduced in size.
Furthermore, on the morning of admission the patient developed general tonic-clonic convulsions. The left homonymous hemianopsia revealed itself about 2 hours after the convulsions stopped. Cerebellar ataxia in limbs and trunk, and ataxic dysarthria were also observed. Other physiological and neurological findings were normal. Brain computed tomography (CT) on admission showed a mild low-density area in the right occipital lobe, and brain magnetic resonance imaging (MRI) (T2-weighted and diffusion-weighted images [ and ]) showed a high-intensity area in the right occipital lobe. Eventually, he was diagnosed with mitochondrial disease with cerebellar ataxia because of repeated convulsions, stroke-like episodes with characteristic radiological findings, and intrathecal high concentrations of lactic acid and pyruvic acid. The patient refused muscle biopsy and the pathological findings are unknown. Genetic analysis revealed no mitochondrial DNA mutation at nucleotide positions 3,243 and 8,344. Thus the type of mitochondrial disease is unknown. With continuing use of phenytoin and zonisamide, the left homonymous hemianopsia gradually resolved itself by hospital day 36. The high-intensity lesion on diffusion-weighted MRI had extended to the right parietal and temporal lobes by hospital day 22 ( and ), then, in parallel with the clinical symptoms, it disappeared by hospital day 36 ( and ).
Figure 1 Brain magnetic resonance imaging (MRI) findings.
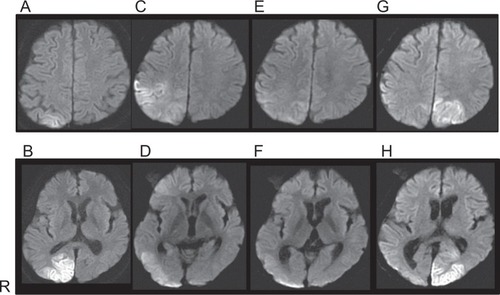
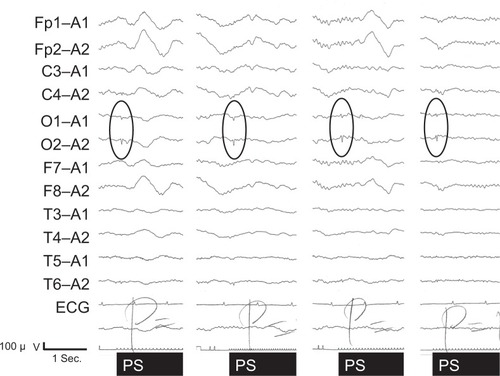
However, on the morning of hospital day 57, he suddenly complained that his right visual field was blind. Confrontation visual field examination revealed right homonymous hemianopsia. In the afternoon he suddenly saw a bottle in his left visual field, and tried to grasp it but failed. He then realized it was an illusion produced by a bottle placed on a bedside table in his blind, right visual field. He noticed the illusory image without turning to the right. Thus there is no possibility that he saw the bottle in the intact left visual field. The illusory image had the same shape, size, color, and even letters on the label as the real bottle. He also saw a nurse appear in his left intact visual field, but then noticed she was really on his right. Because the entrance to the room was in his right blind visual field and the wall was in his intact visual field, there was no possibility that the nurse had already been seen on the intact visual side and then reappeared. These illusory images were palinoptic and tended to persist a few minutes after the objects were no longer in view. His visual field was re-examined several times by confrontation perimetry using different observers and we confirmed that the right homonymous visual site was still blind. Our diagnosis was visual allesthesia with palinopsia. Furthermore, the visual allesthesia shifted from the blind homonymous site to the contralateral site and was accompanied by palinopsia. Episodes of this unusual visual phenomenon occurred intermittently for a few weeks, while T2-weighted and diffusion-weighted brain MRI showed a high-intensity area in the left parieto-occipital lobes ( and ). Electroencephalogram showed positive sharp waves evoked by photic stimulation in bilateral occipital leads ().
Discussion
After the first report in Germany of visual allesthesia in 1895,Citation2 this interesting phenomenon has rarely been reported. In the later reports,Citation4–Citation10 only one case, reported by Ardila et alCitation10 had the direction of shift from blind to the intact visual site. Therefore the shift observed in our case is very rare. A possible explanation, discussed by Ardila et al is that cortical blindness in the hemianopsia field is incomplete.Citation10 This was supported by another reportCitation11 in which a patient with right occipital infarction had an “island” of preserved vision detected only by detailed perimetry, although the patient reported seeing nothing in the area. Thus, partially preserved primary visual cortex may play a role in blindsight.Citation12 Since stroke-like lesions in mitochondrial disease are often reversible, incomplete damage of the primary visual cortex may be related to the blindsight of our patient. Meanwhile, alternative mechanisms of blindsight have also been suggested.Citation13 The colliculiCitation14 and direct projections from the lateral geniculate body to extrastriate visual cortexCitation15 are also thought to be involved in blindsight. The involvement of such subcortical structures may be agreeable since the radiologically-proven lesions in our case study were located bilaterally in the occipito-parieto-temporal lobes, but not in the thalamus and brainstem.
The next problem is how vision transferred from the blind to the intact visual field. Ardila et alCitation10 hypothesized that information perceived in the damaged visual cortex (with its island of preserved activity) was transferred to the intact side by epilepsy-linked cortical excitation, and that the “ghost” image was subsequently perceived contralateral to the real image. Furthermore, other case reports of visual allesthesiaCitation4–Citation10 noted palinopsia, as with our case. In these reports, the pathophysiology of both visual allesthesia and palinopsia is thought to be epileptic in origin. Our patient’s condition was also accompanied by seizure and epileptic electroencephalogram findings. We believe epileptic excitation may link the two hemispheres transferring information from the intact island on the blind side to the intact visual area of the contralateral hemisphere.
Conclusion
This is the first case of mitochondrial disease with visual allesthesia which shifted from blind to intact visual site. Although the etiology of visual allesthesia is unknown, its manifestation in our patient suggests blindsight mediated by incomplete cortical impairment and epileptic excitation of cerebral cortex.
Author contributions
HM, HI, AS, AF, YS, MS and MK clinically assessed the case and performed a literature search. HM, AS, AF, YS and MS drafted the manuscript. HI, MWM and MK revised critically for important intellectual content. All authors agree to the present manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
This study was supported by Grant-in-aids for Scientific Research on Innovative Areas, “Face Perception and Recognition” (MEXT, 23119720) and “The Science of Mental Time” (MEXT, 25119006); and a Grant-in-Aid for Scientific Research (MEXT, 23591283). This study was also supported in part by the Showa University Medical Foundation and the Research Funding for Longevity Sciences (25–13) from the National Centre for Geriatrics and Gerontology (NCGG), Japan.
Disclosure
The authors report no conflicts of interest in this work.
References
- KawamuraMHirayamaKShinoharaYWatanabeYSugishitaMAllesthesiaBrain198711012252363801852
- BeyerEUber verlagerungen im gesichtsfeld bei flimmerskotom [About displacement in visual field at the time of scintillating scotoma]Neurol Centralbl1895141015 German
- HerrmannGPötzlODie Optische Allaesthesie: studien zur psychopathologie der raumbildung [The visual allesthesia: studies of pyschopathology of the space forming]BerlinKarger192816 German
- JacobsLVisual allesthesiaNeurology19803010105910637191497
- ErettoPASchoenFSKrohelGBPEchetteDPalinoptic visual allesthesiaAm J Opthalmol1982936801803
- NakajimaMYasueMKaitoNKamikuboTSakaiHA case of visual allesthesiaNo To Shinkei1991431110811085 Japanese1799515
- AraiTIrieKAkiyamaMA case of falcotentorial meningioma with visual allesthesiaNo To Shinkei2002543255259 Japanese11968817
- CritchleyMTypes of visual preservation: “Palinopsia” and “Illusory visual spread”Brain195174326729914869536
- MendezMFChenJWEpilepsy partialis continua with visual allesthesiaJ Neurol200925661009101119240953
- ArdilaABoteroMGomezJPalinopsia and visual allesthesiaIntern J Neurosci1987323–4775782
- FendrichRWessingerCMGazzanigaMSResidual vision in a scotoma: Implications for blindsightScience19922585087148914911439839
- KastenEWuestSSabelBAResidual vision in transition zones in patients with cerebral blindnessJ Clin Exp Neuropsycho1998205581598
- BartonJJDisorders of higher visual processingHandb Clin Neurol201110222326121601069
- PtitoALeporeFPtitoMLassondeMTarget detection and movement discrimination in the blind field of hemispherectomized patientsBrain19911141B4975122004253
- CoweyAStoerigPThe neurobiology of blindsightTrends Neurosci1991141B1401451710851