Abstract
Purpose
The purpose of this study was to develop and validate a tool called the Pictorial Cognitive Screening Inventory (PCSI), which consists of pictorial memory and attention tests that are not influenced by literacy level.
Patients and methods
PCSI, Mini Mental State Examination (MMSE), and Clinical Dementia Rating (CDR) questionnaires were administered to 80 elderly participants (20 illiterate normal, 20 illiterate with dementia, 20 literate normal, and 20 literate with dementia).
Results
PCSI scores were highly correlated with those of the MMSE (r 0.51) and the CDR (r −0.71). In addition, the PCSI scores differed significantly between the normal group and the dementia group (mean difference 1.71, standard error [SE] 0.14, P<0.001), while no such difference was observed between the illiterate group and the literate group (mean difference 0.00, SE 0.24, P=0.997). Diagnostic validity of the PCSI is excellent, with a sensitivity of 90% and a specificity of 98% for screening dementia, whereas the MMSE has a sensitivity of 85% and a specificity of 60%.
Conclusion
These results indicate that the PCSI is a sensitive and reliable test for screening dementia, regardless of an individual’s literacy skills. The PCSI meets the increasing needs for screening of dementia in illiterate elderly populations in developing countries.
Introduction
Dementia is an acquired syndrome that gradually impairs cognitive functions such as memory, language, visuospatial processing, conceptualization, and judgment. The incidence of dementia has risen alongside the increase in the aging population. Consequently, screening for dementia has become necessary to reduce the potential burden it incurs for the public.Citation1 The purpose of this study was to develop a test to screen for dementia in elderly populations, regardless of their education and literacy level.
Development of an accurate dementia screening tool that is independent of literacy level is crucial, especially for use in elderly populations who tend to have a high rate of illiteracy. Many elders in Asia have not received a formal education due to poverty, resulting in higher incidence rates of dementia. In fact, illiterate elders have four times the risk of dementia. Thus, the detection of dementia in illiterate elders is critical;Citation2 however, in reality, they remain largely unacknowledged. The Mini Mental State Examination (MMSE) is one of the most widely used dementia screening instruments in the world.Citation3 It has been shown to have good reliability and validity in detecting dementia; however, this instrument is limited because its results are strongly influenced by education.Citation4,Citation5 Other dementia screening instruments also consistently bear these problems (eg, the 7-minute screening, Consortium to Establish a Registry for Alzheimer’s Disease [CERAD], and the Hasegawa dementia rating scale). Therefore, it is crucial to develop a sensitive dementia screening tool that is not influenced by education and literacy levels.
To overcome these difficulties, researchers have adopted age and educational norms of the elderlyCitation6 or used caregiver interviews to screen for dementia. However, the tools that are administered to assess dementia in illiterate elders still need to be developed further. First, administering different norms depending on the patient’s educational level hinders and undermines the efficiency of screening and dementia assessment in clinics. Second, the use of second-hand information, such as gathered in a caregiver’s interview, to examine a patient’s performance can be less accurate. Therefore, an accurate and brief screening tool that directly measures performance of a participant should be developed.
This study developed the Pictorial Cognitive Screening Inventory (PCSI) to screen for dementia regardless of education and literacy level. The PCSI comprises a ‘pictorial’ memory test and a selective attention test with color perception.Citation7 The pictorial memory test was modified from a delayed ‘word’ recall test that shows high predictive accuracy (95.2%) for screening of dementia in Alzheimer’s disease.Citation8 In addition, the selective attention impairment test is sensitive enough to detect subcortical dementia such as subcortical ischemic vascular dementia, a dementia with Lewy bodies.Citation9 Verbal series attention tests using numbers and letters have been shown to have a high correct group classification of 89%Citation10 in the assessment of dementia.
The goals of the current study are to test the validity of the PCSI to screen dementia, to verify its accuracy in dementia screening regardless of literacy, and to find its optimal cut-off point to differentiate the normal population from the dementia population.
Materials and methods
Scale development of the PCSI
The PCSI consists of two subtests: a pictorial memory test and a selective attention test. In the pictorial memory test, 20 pictorial stimuli were created to replace the 20 word stimuli from the previous screening instrument.Citation11,Citation12 These new pictorial stimuli afford the test the advantage of also being usable with illiterate people ().
When selecting pictorial stimuli, each picture representing a word is within the 90th percentile for frequency in the corpus of the Korean language and has a concrete meaning. The 20 stimuli were drawn by a professional illustrator, ensuring that they were generally easy for participants to recognize.
The initial pictorial memory test used ten of the 20 pictorial stimuli (flower, umbrella, chair, hand, key, house, phone, hat, turtle, and hanger). The other ten stimuli (tree, mushroom, ship, cherry, sun, star, faucet, necklace, cat, and envelope) were used as distracters in the delayed recognition test, which was administered toward the end of the pictorial memory test. Researchers used computers to create circles of about 5 cm diameter, in yellow, red or black, to measure the selective attention of participants.
Participants
The 80 participants were at least 65 years old and were recruited from the SMG-SNU Boramae Medical Center of South Korea during the period December 2008 to March 2009. The participants could be classified into four distinct groups: 20 illiterate normal, 20 illiterate with dementia, 20 literate normal, and 20 literate with dementia.
Exclusion criteria
The exclusion criteria for participating in this study included a known history of neurological disease, head trauma, stroke, or any other physical illness affecting cognitive functions; visual or hearing difficulties that would interfere with the testing procedure; and motor impairment that could affect test scores. This research was completed in accordance with the guidelines of the Helsinki Declaration.
Dementia diagnosis
Dementia was diagnosed based on the criteria of the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)Citation13 by a trained psychiatrist and a neurologist. All dementia subjects underwent neurological examinations and brain magnetic resonance imaging to exclude other brain diseases. The MMSE and the Clinical Dementia Rating (CDR) instruments were administered by a psychologist.
The diagnosis results revealed that, within the dementia group, 27 (70%) subjects were diagnosed with Alzheimer’s dementia, eight (20%) subjects were diagnosed with subcortical vascular dementia, and five (10%) subjects were diagnosed with other dementia such as frontotemporal dementia and Lewy body disease. The CDR score was 0 for all participants in the normal group, while, in the dementia group, 16 (40%) received a score of 0.5 (questionable dementia), 16 (40%) received a 1 (mild dementia), five (12.5%) received a 2 (moderate dementia), and three (7.6%) received a 3 (severe dementia).
PCSI administration procedures
The review board of our institution, Boramae Medical Center of South Korea, approved the study protocol. The psychologist independently administered the PCSI, the MMSE, and the CDR to all participants, and made a valid diagnosis of dementia. All stimuli were presented on a computer. The basic order when administering the PCSI is to first present ten initial pictorial stimuli. A participant will then undergo the selective attention test. The participant is then asked to recall the initial pictorial stimuli. Finally, the psychologist presents a set of stimuli that is a mix of both the initial pictorial stimuli and the new pictorial stimuli. Each pictorial stimulus was presented one at a time with an inter-stimulus interval of 2 seconds. During the presentation, the participant ‘read’ the stimuli out loud to commit it to memory. During this phase, if the subject was unable to correctly ‘read’ the first pictorial stimuli, the administrator could read the stimuli with the participant. After the first set of pictorial stimuli was presented, the selective attention test was administered. In order to measure an individual’s selective attention, yellow, red, or black circles were presented on the center of the computer screen one at a time for 3 seconds each. This test presented 50 colored (black, yellow, and red) circles. Half of the circles, a mixture of yellow and red, were presented randomly, and the other half was solely black and were also randomly distributed. Participants were asked to respond only to the black circles by pressing the space bar on the keyboard. The number of correct responses (out of 50 trials) was calculated by summing the number of correct inhibitions to yellow and red stimuli (out of 25 trials) and the number of correct responses to black stimuli (out of 25 trials).
Once the selective attention test was finished, a recall test from the initial pictorial memory test of ten stimuli was administered. The number of correctly recalled pictorial stimuli was the score (out of ten trials) for the delayed recall test. Then, in a delayed recognition test, the ten previously presented pictorial stimuli along with ten novel stimuli (we previously called these optional pictorial stimuli) were presented one by one in random order with a 2-second inter-stimulus interval. The delayed recognition score (out of ten) was calculated by subtracting ten from the sum of correct ‘yes’ or ‘no’ responses (20 trials in total) to the question of whether the picture had been previously presented. Consequently, the PCSI scores consisted of a delayed recall score (out of ten), a delayed recognition score (out of ten), and a selective attention score (out of 50). The total administration took about 6–8 minutes for each test subject. To assess the test–retest reliability of PCSI, 25 participants (nine illiterate normal, one illiterate with dementia, ten literate normal, and five literate with dementia) were gathered after 2 weeks and re-tested with the PCSI with the same procedures and materials.
Assessment
Literacy questionnaire
A literacy questionnaire developed by Moon and CheyCitation14 was used to assess the literacy level of the subjects. This questionnaire categorizes literacy into four levels: level 1 is for those who are unable to read or write Korean at all; level 2 is for those who have difficulty with both reading and writing Korean; level 3 is for those who only have difficulty with writing in Korean; and level 4 is for those who have no difficulty with writing and reading in Korean. Levels 1 and 2 are categorized as illiterate, and levels 3 and 4 are categorized as literate. For a more detailed description of this instrument, see Youn et al.Citation15
Clinical Dementia Rating
The CDR is a representative measurement for assessing dementia severity that was developed by Hughes et alCitation16 and partially revised by Morris.Citation17 It is designed to produce a global composite CDR score for dementia severity, combining the clinical evaluation by a clinician on impairment in six areas: memory, orientation, judgment and problem solving, community affairs, home and hobbies, and personal care. The composite rating consists of five levels: 0 (none), 0.5 (questionable), 1 (mild), 2 (moderate), and 3 (severe).
Mini Mental State Examination
The MMSE is a neurocognitive test designed to screen cognitive impairment.Citation3 Its scores range from 0 to 30, where higher scores indicate better cognition and scores below 25 indicate cognitive impairment. It can be administered in 5–10 minutes. The Korean version of the MMSE consists of orientation (10 points), short-term memory registration and recall (6 points), attention (5 points), naming (2 points), following verbal commands (4 points), judgment (2 points), and copying a double pentagon (1 point). The MMSE was validated for use with an elderly Korean population by Lee et al.Citation6
Data analysis
SPSS for Windows 18.0 (SPSS Inc., Chicago, IL, USA) was used to analyze the data. Between-group differences were verified by running analysis of variance (ANOVA) and chi-square tests across the demographic variables (age, education, and sex) and the test scores with Bonferroni adjustment for multiple testing. Pearson’s correlation analysis was conducted to assess the relationship between age and PCSI, MMSE, and CDR scores. To examine the concurrent validity, partial correlation analyses were conducted between the PCSI scores and the MMSE and the CDR scores while controlling for the effect of age on test scores. Two-way ANOVAs were conducted to test for any significant main and interaction effects of dementia status and literacy status in the scores of the PCSI and the MMSE. To assess the ability of the PCSI subtests and the MMSE to screen dementia, separate receiver operating characteristics (ROC) curves were plotted for the illiterate group, the literate group, and the whole group. To measure the test–retest reliability, intra-class correlation coefficients (ICCs) for the baseline and 2-week follow-up PCSI scores were assessed.
A composite score for the PCSI was calculated by combining the scores of the three subtests using discriminant analysis to simplify its use in real clinical settings. To allow for comparison of the three subtests that employ different scales of measurement, they were first converted to Z scores, and the discriminant function coefficient for each score was calculated. The products of the Z scores of each subtest and their coefficients were summed to produce the composite scores. Correlation analyses were conducted between these composite PCSI scores and the other test scores (MMSE and CDR) and demographic variables. Two-way ANOVAs were conducted to test the between-group difference based on dementia status and literacy status, and ROC curves of the PCSI and MMSE were plotted to examine how well they discriminated dementia in the illiterate group, the literate group, and the whole group. Comparison of ROC curves was performed with MedCalc software (MedCalc Software bvba, Ostend, Belgium). The significance level for all statistical tests was set to a two-tailed P-value of 0.05.
Results
Demographics
The information about age, education, and sex for each group (illiterate-normal, illiterate-dementia, literate-normal, and literate-dementia) is presented in . The average age of the total group of 80 participants was 74.60 years (standard deviation [SD] 6.61), the average years of education was 3.94 years (SD 4.93), and there were 13 males and 67 females. The mean age and years of education was significantly different between the four groups, (Fage(3, 76)=24.56, P<0.001; Feducation(3, 76)=29.09, P<0.001), as was sex ratio (P<0.001).
Table 1 Demographic variables for each group
Each demographic variable showed significant correlations with PCSI subtest, MMSE, and CDR scores. Age was significantly correlated with delayed recall score (r −0.339, P<0.01), delayed recognition score (r −0.323, P<0.01), selective attention score (r −0.269, P<0.05), MMSE score (r −0.629, P<0.01), and CDR score (r 0.513, P<0.01). Education level showed significant correlation only with the MMSE score (r 0.351, P<0.01).
Concurrent validity
In order to assess the concurrent validity of the PCSI subtest scores, partial correlation analyses between the PCSI subtest scores and the MMSE and the CDR scores were conducted while controlling for age, because age showed a significant correlation with all PCSI subtest scores among the demographic variables. Since education level was highly correlated with illiteracy (r 0.802, P<0.01) and was not correlated with the PCSI subtest scores, we did not control for education level.
The delayed recall score from the PCSI showed significant correlation with both the MMSE score (r 0.50, P<0.01) and the CDR score (r −0.69, P<0.01). The delayed recognition score also showed significant correlation with both the MMSE score (r 0.33, P<0.01) and the CDR score (r −0.56, P<0.01). The number of correct responses in the selective attention test showed significant correlation with both the MMSE score (r 0.38, P<0.01) and the CDR score (r −0.54, P<0.01). According to all of the significant correlations with the measurements, these indicate good performance on the PCSI, which can predict good cognition and low clinical severity.
Diagnostic validity and literacy level
presents the means of the PCSI and the MMSE scores based on dementia status (normal vs dementia) and literacy level (illiterate vs literate). In order to examine the main and interaction effects of the groups on the PCSI and the MMSE scores, two-way ANOVAs were conducted.
Table 2 Means and standard deviations for the PCSI and the MMSE scores by dementia status and literacy status
Dementia status had a significant effect on all subtest scores of PCSI (delayed recall F(1, 79)=162.79, P<0.001; delayed recognition F(1, 79)=49.53, P<0.001; selective attention F(1, 79)=12.74, P<0.01). However, literacy level did not have a significant effect on these scores (delayed recall F(1, 79)=0.09, P>0.05; delayed recognition F(1, 79)=1.47, P>0.05; selective attention F(1, 79)=0.02, P>0.05). In contrast, the MMSE showed significant differences according to the literacy level of the participant (F(1, 79)=23.43, P<0.001) as well as dementia status (F(1, 79)=67.50, P<0.001). These results indicate that PCSI is valid for the screening of dementia regardless of participants’ literacy level, unlike the MMSE.
ROC curves for PCSI subtest and MMSE scores
ROC curves were plotted to indicate how well the PCSI subtest scores and the MMSE scores discriminate between the normal group and the dementia group. shows the cut-off scores, sensitivity, specificity, false-negative rate, false-positive rate, and correct classification rate (CCR) for the whole group, the illiterate group, and the literate group.
Table 3 Cut-off points, sensitivity, specificity, and correct classification rate for PCSI subtest scores and MMSE score
The PCSI subtest scores had high accuracy for discriminating dementia status using the same cut-off points for both illiterate and literate groups. Moreover, recall score of the pictorial stimuli in particular showed higher discrimination accuracy than did other test scores. In contrast, the MMSE scores had low specificity: 0.6 for the whole group, 0.8 for the literate group, and 0.4 for the illiterate group.
Test–retest reliability
Test–retest reliability data were collected from 25 participants at 2-week intervals. Score difference in the selective attention test from the first to second evaluation was between −4 and 2, and the ICC between the baseline scores and the follow-up was 0.98 (P<0.001). The score difference in the delayed recall test was between −3 and 2, with an ICC of 0.89 (P<0.001), and the score difference in the delayed recognition test was between −6 and 6, with an ICC of 0.83 (P<0.001).
The composite score of the PCSI
To make the usage in clinical settings simpler and more convenient, a composite score was calculated using discriminant analysis on the three subtest scores of the PCSI. The discriminant analysis strongly predicted dementia (Wilks’ Lambda 0.33, P<0.001) and correctly classified 93.75% of the cases. The discriminant function coefficient was 0.905 for delayed recall, 0.162 for delayed recognition, and 0.059 for selective attention. The resulting composite scores had a mean of 0 and an SD of 1.00, with values ranging between −1.75 and 2.01. These PCSI composite scores showed significant correlation with the MMSE scores (r 0.51, P<0.001) and the CDR scores (r −0.71, P<0.001) as well as PCSI subtest scores (delayed recall r 0.99, P<0.001; delayed recognition r 0.78, P<0.001; selective attention r 0.48, P<0.001). Age variable showed a significant correlation with PCSI composite score (r −0.36, P<0.001). The PCSI composite score also showed a significant effect of dementia status consistent with the results of each subtest score (F(1, 79)=165.81, P<0.001) while not showing an effect of literacy level between groups.
ROC curves were plotted to demonstrate how well the PCSI composite scores and the MMSE scores discriminated dementia status in the whole group (). The area under the ROC curve was 0.98 for PCSI and 0.87 for MMSE. shows the ROC curve for the illiterate group, with the area under the ROC curve being 0.95 for PCSI and 0.90 for MMSE. shows the ROC curve for the literate group, with the area under the ROC curve being 0.99 for PCSI and 0.90 for MMSE.
Figure 1 Receiver operating characteristic curve analysis of the PCSI and MMSE scores for detecting dementia.
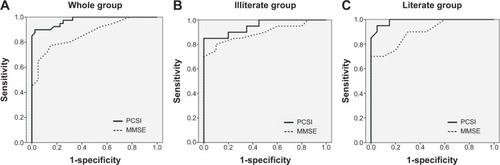
When compared against the sensitivity, specificity, and CCR of the PCSI, the MMSE scores showed lower figures. In a statistical evaluation with MedCalc ROC curve comparison, the PCSI was found to be statistically better than the MMSE (P=0.01). Furthermore, using the same cut-off value for both illiterate and literate groups for diagnosis resulted in a significant drop in sensitivity, specificity, and CCR for the MMSE but not for the PCSI ().
Table 4 Cut-off points, sensitivity, specificity, and correct classification rate for PCSI composite score and MMSE score
Discussion
The MMSE, a widely used dementia screening instrument, is strongly affected by literacy level and education. Researchers suggest that countries with low education levels need cognitive ability testing instruments tailored to their own environment.Citation18,Citation19 This study developed the PCSI, a dementia screening tool that consists of a memory test using pictorial stimuli. Its most significant finding is considered to be that it is an efficient way to diagnose Alzheimer’s dementia among illiterate subjects.Citation20,Citation21 Moreover, the selective attention test in the PCSI has shown the acceptable diagnosis for subcortical ischemic vascular dementia, a Lewy Body dementia.Citation22,Citation23 The administration results for the PCSI in this study show strong concurrent validity, diagnostic validity, and test–retest reliability.
The correlation between the PCSI composite score and its subtest scores and the MMSE and CDR scores were all significant, indicating that the PCSI has adequate concurrent validity as a testing instrument for measuring dementia. Both the subtest scores and the composite scores of the PCSI showed a high sensitivity to screening dementia while not being affected by literacy status. Unlike the PCSI, the MMSE had difficulty discriminating between the normal-illiterate group and the dementia-literate group. These results indicate that the PCSI is a test that overcomes the challenge of distinguishing the normal-illiterate group from the dementia group of the existing test.
The ROC curve also demonstrates the effectiveness of the PCSI. Regardless of literacy status, the PCSI score was able to detect dementia using an identical cut-off value. However, for the MMSE score, specificity and CCR were decreased within the illiterate group when an identical cut-off value (22/23) was used for diagnosis. Unlike the MMSE, the PCSI is not affected by literacy status; thus, it certainly reflects the fact that, in countries with a low education rate, the PCSI has more validity as a testing instrument than the MMSE. Furthermore, the PCSI showed high test–retest reliability, demonstrating its reliability as a testing instrument with minimal measurement error.
The PCSI focused on attention and memory performance; it does not cover other cognitive functions such as executive functions, abstract thinking, visuospatial skills, and social cognitive skills that can be affected in dementia patients. The screening tool should take less than 10 minutes to administer in clinic. Therefore, we only focused on the two functions (attention and memory) that are most impaired in dementias such as Alzheimer’s disease, subcortical ischemic vascular dementia, and Lewy Body dementias. However, even though these two performances showed high sensitivity in the screening of dementia, further studies should examine the possibility of other cognitive functions that can more efficiently distinguish dementia.
The current study has a few limitations. First, the group assignment of the participant sample did not consider demographic variables such as age, education, and sex. In particular, in terms of sex, the number of female participants was significantly higher in the illiterate group, reflecting the traditional situation in Korea, whereby the female population had scarce opportunity to receive a proper education. Nevertheless, the PCSI subtest scores and composite score showed no significant correlation with education level, whereas the MMSE score showed a significant correlation. To reduce the perceived bias, this study controlled for age during the statistical analysis, but future studies should conduct research on age- and sex-matched groups. Second, the current study had a small sample size, which may limit the generalizability of the results; thus, cross-validation studies with larger samples are needed.
Conclusion
The PCSI developed in the current research is a reliable instrument for detecting dementia effectively, regardless of participant’s education history or literacy status. The PCSI addresses the limitations of existing tests and is appropriate for use in countries with a high illiteracy rate. Furthermore, this tool takes less than 8 minutes to administer, which suggests that it can be a valuable and efficient tool, satisfying the rapidly increasing needs for the screening of dementia in the rising elderly population in Asian countries.
Acknowledgments
This study was conducted in Seoul, South Korea. This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry for Health and Welfare, Republic of Korea (A070001).
Supplementary materials
Disclosure
The authors report no conflicts of interest in this work.
References
- YusufAJBaiyewuOSheikhTLShehuAUPrevalence of dementia and dementia subtypes among community-dwelling elderly people in northern NigeriaInt Psychogeriatr201123337938620716387
- LeeJYChangSMJangHSIlliteracy and the incidence of Alzheimer’s disease in the Yonchon County survey, KoreaInt Psychogeriatr200820597698518452643
- FolsteinMFFolsteinSEMcHughPR“Mini-mental state”. A practical method for grading the cognitive state of patients for the clinicianJ Psychiatr Res19751231891981202204
- AnthonyJCLeRescheLNiazUvon KorffMRFolsteinMFLimits of the ‘Mini-Mental State’ as a screening test for dementia and delirium among hospital patientsPsychol Med19821223974087100362
- Le CarretNAuriacombeSLetenneurLBerguaVDartiguesJFFabrigouleCInfluence of education on the pattern of cognitive deterioration in AD patients: the cognitive reserve hypothesisBrain Cogn200557212012615708201
- LeeDYLeeKULeeJHA normative study of Mini-Mental State Examination in the Korean elderlyJ Korean Neuropsychiatr Assoc2002413508525 Korean [with English abstract]
- ReisAFaíscaLIngvarMPeterssonKMColor makes a difference: Two-dimensional object naming in literate and illiterate subjectsBrain Cogn2006601495416271820
- KnopmanDRybergSA verbal memory test with high predictive accuracy for dementia of the Alzheimer typeArch Neurol19894621411452916953
- CalderonJPerryRJErzincliogluSWBerriosGEDeningTHodgesJRPerception, attention, and working memory are disproportionately impaired in dementia with Lewy bodies compared with Alzheimer’s diseaseJ Neurol Neurosurg Psychiatry200170215716411160462
- MahurinRKCookeNVerbal series attention test: Clinical utility in the assessment of dementiaClin Neuropsychol19961014353
- ReyAL’Examen clinique en psychologie [Clinical Psychology Review]ParisPresses Universitaires de France1970 French
- ReyALe troubles de la memoire et leur examen psychometrique [Memory disorders and psychological examination]DessartBruxelles1966 French
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text RevisionWashington DCAmerican Psychiatric Press2000943
- MoonHSCheyJYLiteracy and neuropsychological functions in the older Korean adultsJ Korean Geriatr psychiatry200482113120
- YounJHSiksouMMackinRSChoiJSCheyJLeeJYDifferentiating illiteracy from Alzheimer’s disease by using neuropsychological assessmentsInt Psychogeriatr201123101560156821777502
- HughesCPBergLDanzigerWLCobenLAMartinRLA new clinical scale for the staging of dementiaBr J Psychiatry198214065665727104545
- MorrisJCThe Clinical Dementia Rating (CDR): current version and scoring rulesNeurology19934311241224148232972
- MarcopulosBAMcLainCAGiulianoAJCognitive impairment or inadequate norms? A study of healthy, rural, older adults with limited educationClin Neuropsychol1997112111131
- OlinJTZelinskiEMThe 12-month Reliability of the Mini-Mental State ExaminationPsychol Assess199133427432
- SilveriMCLeggioMGInfluence of disorders of visual perception in word-to-picture matching tasks in patients with Alzheimer’s diseaseBrain Lang19965423263348811963
- WelshKAButtersNHughesJPMohsRCHeymanADetection and staging of dementia in Alzheimer’s disease. Use of the neuropsychological measures developed for the Consortium to Establish a Registry for Alzheimer’s DiseaseArch Neurol19924954484521580805
- McGuinnessBBarrettSLCraigDLawsonJPassmoreAPAttention deficits in Alzheimer’s disease and vascular dementiaJ Neurol Neurosurg Psychiatry201081215715920145028
- RöslerABillinoJMüllerNGWeidauerSSteinmetzHKleinschmidtAVisual search in patients with subcortical vascular dementia: short fixations but long reaction timesDement Geriatr Cogn Disord200520637538016244479