Abstract
Meningiomas are the most common benign brain tumors, and are characterized by slow growth and a long asymptomatic period. Once the tumor becomes symptomatic, the various presentations may be related to the location and compression of adjacent structures. Meningioma is primarily treated through surgical intervention, and thus earlier diagnosis is likely to result in better prognosis. The symptoms of the meningioma may mimic other diseases, making precise diagnosis difficult, which will then delay treatment. We report a case of brain meningioma that showed initial signs and symptoms similar to cervical radiculopathy. The symptoms extended gradually, and the ultimate diagnosis of meningioma was confirmed based on brain-image studies. After brain-tumor excision, postoperation radiotherapy, and aggressive rehabilitation, the patient was able to perform better in daily activities.
Introduction
Muscle weakness is a common and nonspecific complaint that encompasses a broad range of differential diagnosis. Progressive monolimb weakness is a very common symptom that occurs in any age range and in various situations, thus needing further differential diagnoses. To approach the lesions of the neuromuscular system, a careful evaluation of the motor cortex through the corticospinal tracts, anterior horn cells, spinal nerve roots, peripheral nerves, neuromuscular junction, and finally the muscle should be conducted. Detailed neurologic examination should be able to identify lesions of the central and peripheral nervous systems. Pure motor hemiparesis is a syndrome that is occasionally mimicked by central or peripheral pathologies,Citation1 along with the etiology of cortical lesions, lacunar syndromes and basal ganglia lesions, brain-stem processes, radiculopathies, plexopathies, peripheral nerve injuries, disuse atrophy, and myasthenia gravis, among others. Cervical radicular symptoms tend to follow a dermatomal pattern, depending upon which cervical nerve root is compressed, thus producing upper-extremity radicular symptoms, such as pain, numbness, weakness, and paresthesia.Citation2 Given the compression or inflammation of the nerve root, radiculopathy is commonly associated with a radiating pain experienced in the dermatome, myotome, or sclerotome.Citation3 In a review of cervical radiculopathy, the clinical consequence of radiculopathy is arm pain or paresthesias in the dermatomal distribution of the affected nerve, and may or may not be associated with neck pain and motor weakness.Citation4 The weakness attributed to central nervous systems includes common acute stroke syndromes, space-occupying lesions (such as tumors), and lesions of the spinal cord.
Meningioma accounted for more than a third of all primary central nervous system tumors reported in the US between 2006 and 2010, where the highest incidence rate (7.44 per 100,000) of the disease has been recorded.Citation5 Meningiomas usually grow slowly, with a long initial asymptomatic phase, and may remain silent until the patient’s sudden death.Citation6 Only 3%–6% of clinically detected asymptomatic meningiomas later become symptomatic.Citation7 When symptomatic, intracranial meningiomas present a wide variety of symptoms arising from the compression of adjacent structures, direct invasion of or reactive changes in the adjacent brain tissue, and obstruction of cerebrospinal fluid pathways, cortical veins, or major venous sinuses.Citation8 Symptoms and signs may include seizure disorders, raised intracranial pressure sign, classic early morning headaches, focal neurological deficits, such as motor and sensory disorders, ataxia, language dysfunction, cranial neuropathies, psychomotor symptoms, and behavioral disturbances.Citation8 We report a case that presented initial signs and symptoms of numbness that started from the fingers, extending to the forearm, but the symptoms became atypical, resulting in an ultimate diagnosis of meningioma.
Case report
A 54-year-old man reported experiencing a gradual onset of numbness, which started from his left thumb and extended to his fingers, approximately 6 months before he was admitted. The numbness gradually progressed to his left forearm, and cervical traction was conducted at the local medical department, based on the assumption of cervical radiculopathy. The symptoms did not disappear. Three months later, intermittent headaches occurred following the numbness of the left hand, especially during defecation and coughing. At the same time, weakness in the upper-left proximal extremity, especially at the shoulder and elbow, were noted. As time progressed, he was no longer able to dress himself, because he was unable to lift his arm and forearm. However, flexion of the fingers was preserved: he could still grasp things and grip the handlebars while riding his motorcycle. Eventually, he found it difficult to carry on with his job and daily activities.
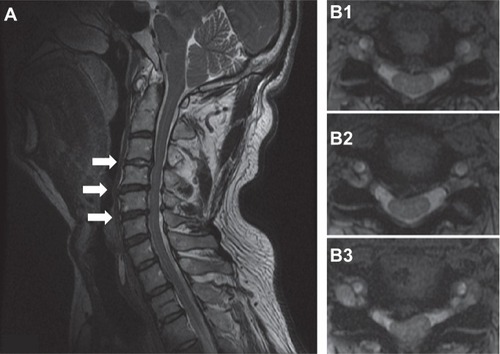
He visited our neurosurgery outpatient department 1 month prior to admission. During the initial evaluation, numbness of the left thumb, fingers, and forearm was noted. Physical examination for muscle power revealed grade IV in the left wrist joint and grade II in the left elbow and shoulder. Increasing deep-tendon reflex in bilateral lower extremities was also noted, with a positive Spurling sign at the left side and a negative Hoffmann sign. Based on an assumption of cervical radiculopathy, an X-ray of the cervical spine was performed, which showed evidence of reduced normal lordosis with a mild narrowing of the intervertebral disk spaces at almost all levels of the cervical spine, with osteoarthrosis of several apophyseal joints (). Magnetic resonance imaging (MRI) of the cervical spine revealed a minor disk bulge at C3–C4, C4–C5, and C5–C6, with posterocentral and right paramedian compression of the ventral surface of the spinal cord (). An electrodiagnostic test revealed normal nerve-conduction velocity in bilateral median and ulnar nerves, and normal findings in the needle-electromyography study of bilateral abductor pollicis brevis and digiti minimi muscles. After treatment using oral nonsteroidal anti-inflammatory drugs, the numbness of the upper-left limb was relieved for several days, but the weakness persisted.
Figure 1 X-ray of the cervical spine anterior–posterior (A) and lateral (B) views showed a mild narrowing of intervertebral disk spaces at almost every level of the cervical spine and osteoarthrosis of several apophyseal joints.
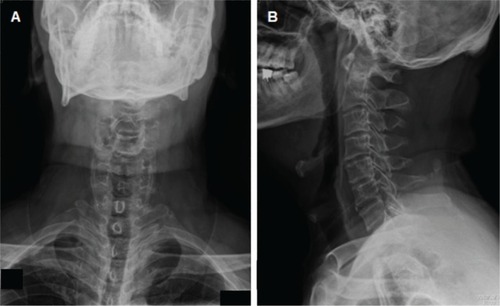
Figure 2 Cervical spine magnetic resonance imaging sagittal (A) and axial views showed herniation of the intervertebral disk in C3/4 (B1), C4/5 (B2), and C5/6 (B3) shown by arrows in (A), with a compression of the ventral surface of the spinal cord.
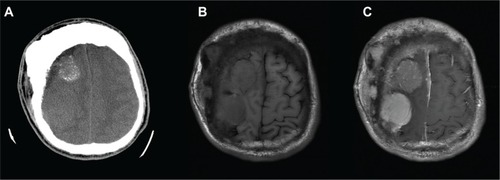
Two weeks before admission, he suffered from an unsteady gait caused by lower-limb weakness, and returned to our neurosurgery outpatient department for further evaluation. He mentioned a deformity in his skull at the right parietal bone, which he had had for years, and that he had experienced intermittent headaches while under the Valsalva maneuver within the last 3 months. Brain computed tomography was performed, revealing two large lobulated masses, with some calcifications in the right high-frontal region and another in the right frontal–parietal region and with severe adjacent frontal bone hyperostosis (). Brain MRI () with gadolinium showed two lobulated and well-defined brain tumors, one of which was in the right high-frontal area and the other in the right frontal–parietal area.
Figure 3 Axial view of brain computed tomography without contrast.
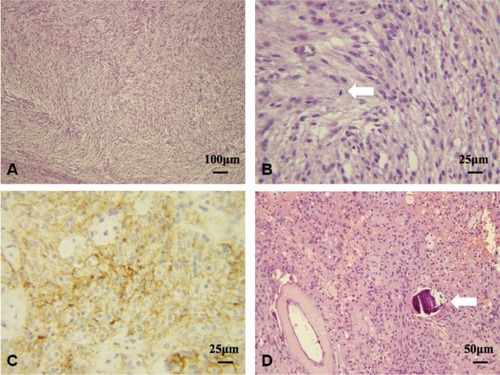
Craniectomy was performed to remove the tumors. The immunohistochemical stain and the pathology report were consistent with atypical meningioma, World Health Organization (WHO) grade II (). After radiotherapy and 1.5 months of aggressive rehabilitation programs, muscle power in the left proximal upper limb improved from grade II to grade IV, and from grade I to grade III in the distal upper limb. The spasticity of the upper-left limb decreased from 2 to 1 in the elbow under the modified Ashworth scale. His functional status, such as his standing balance, improved from fair to good, and he could walk without the help of any device. Performance of daily activities also improved from moderate assistance to near-complete independence. The functional independence measure score improved from 71 to 106, and the Barthel index increased from 35 to 80 as the rehabilitation program ended.
Figure 4 A–D Histologic findings of atypical meningiomas (World Health Organization) grade II.
Abbreviations: HPF, high power fields; EMA, epithelial membrane antigen.
Discussion
Brain-tumor symptoms can vary widely depending on the location of the mass. Possible clinical presentations may be generalized or focal signs, such as headaches, seizures, nausea, vomiting, cognitive dysfunction, extremity weakness, sensory loss, disorder of language function, and visual and hearing loss.Citation9 A great heterogeneity in histology, recurrence rates, aggressiveness, symptoms, and survival outcomesCitation10 exists, despite a large majority of meningioma being classified as benign lesions. Meningiomas are primarily treated through surgery, and no major changes in treatment have been achieved since the publication of the monograph by Cushing and Eisenhardt in 1938,Citation11 except for meningiomas arising in the central skull base. Total resection for intracranial meningiomas is performed in cases of convexity, parasagittal, or falcine meningiomas.Citation12 Therefore, early and accurate diagnosis of the symptoms and treatment of the underlying disease are important.
Based on the literature, a patient being diagnosed with intracranial meningioma with only an initial presentation of numbness in one hand and forearm is very rare. Khalatbari et alCitation13 reported on a 56-year-old woman with brain meningioma who presented pain and paresthesia originating from the anterior upper arm and extending to her radial forearm and right thumb and index finger (corresponding to C6 radicular pain). Meningioma was finally diagnosed by brain computed tomography, which was arranged before the patient received cervical spinal surgery because of persistent headache. Our patient also developed a headache while under the Valsalva maneuver. Compared with the tumor location of our patient, the woman’s tumor growth was more central, which may have resulted in paresthesia starting from the proximal area. Vigilance should be emphasized when facing a similar case, because distinguishing between a brain tumor and radiculopathy is very difficult, and even impossible in these cases. A discussion on the distribution and pattern of the numbness and weakness may aid in arriving at a correct diagnosis in the earlier stages.
Tracing back the history of this case, our patient told of a history of cervical spondylotic radiculopathy that was not fully treated after previous cervical traction. The most common symptom of cervical radiculopathy is radiating pain in the arm due to nerve compression.Citation14 Our patient’s symptoms appeared 6 months prior to the final diagnosis of meningioma. Initially, our patient complained about the numbness, which started from his left thumb and extended to his other fingers, and then progressed and gradually extended to his left forearm. At the same time, our patient denied any neck pain or soreness. Although cervical radiculopathy was originally suspected because of a positive Spurling sign, the distribution of the regions of numbness did not follow a dermatomal pattern, and the radiation pattern was from the distal to proximal area, which was different from the pattern in radiculopathy. Depending on the location of the patient’s meningioma (), the numbness and paresthesia in the left hand was comparable to Penfield and Rasmussen’s first map of cortical homunculus, which compressed the primary somatosensory area in the parietal lobe of the cerebral cortex.Citation15 However, we failed to identify this important point in the beginning. The diagnosis of cervical radiculopathy could later be ruled out based on image findings and the electrodiagnostic study.
Figure 5 Depending on the location of the patient’s meningioma (arrows), the weakness, numbness, and paresthesia of the upper-left limb were compatible with the cortical homunculus, which compressed to the primary somatosensory area (A) and the primary motor cortex (B).
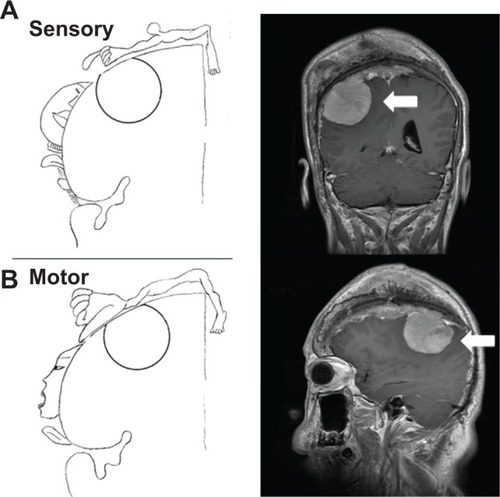
The clinical presentations of cervical radiculopathy can range from pain, numbness, and/or tingling in the upper extremity to electrical-type pains or even weakness.Citation4 Our patient developed weakness in his upper-left proximal extremity, especially in his shoulder and elbow, but exhibited fine motor skills of his wrist and fingers, allowing him to grasp things without difficulty. At the same time, his weakness progressed severely from the proximal limbs to the distal limbs, which is unusual in radiculopathic patients. Additionally, the deep tendon reflex in the bilateral lower extremities of our patient increased, indicating an upper motor-neuron sign, and thus cervical spondylotic myelopathy (CSM) was diagnosed initially. CSM is defined clinically as a symptomatic dysfunction of the cervical spinal cord, and is the most common cause of myelopathy in adults over 55 years old, causing progressive disabilities and impairing quality of life. Cervical myelopathy must be distinguished from the less serious syndromes of cervical radiculopathy and the simple neck pains, which may also result from spondylosis.Citation16 Some studies have concluded that a subtle gait disturbance is the most common presentation of CSM,Citation17,Citation18 and that a spastic gait occurs first, temporally followed by upper-extremity numbness and sensory loss, which may follow a dermatomal pattern, and often underlies complaints of loss of fine-motor control of the hands. The weakness in the proximal limb of our patient was much more severe than that in the distal area, which is a different symptom from myelopathy. In retrospect, the distribution of the weakness could be attributed to Penfield and Rasmussen’s first map of cortical homunculus, where compression of the primary motor cortex happens ().Citation15,Citation19
Cervical spondylosis is the main cause of CSM. However, age-related cervical spondylosis does not always result in CSM. The radiographic incidence of cervical spondylosis in an asymptomatic population in their 70s was reported as 95% in men and 70% in women, and in patients older than 40 years old, nearly 60% had disk degeneration and 20% had foraminal stenosis.Citation20 MRI has become the most important method in diagnosing a significant pathology in the cervical spine. However, an MRI may produce a substantial amount of false-positive findings, because asymptomatic radiological abnormalities are common in radiological imaging of the cervical spine.Citation21 MRI findings are only part of the investigation, and one should always consider a thorough neurological examination.Citation22 Jensen et alCitation23 reported that 36% of 98 asymptomatic subjects had normal disks at all levels. The results of the two readings were averaged, and showed that 52% of the subjects had a bulge on at least one level, 27% had a protrusion, and 1% had an extrusion. The weak correlation between the MRI and clinical findings, such as false-positive and false-negative findings, could be influenced by both the radiologist’s and the clinician’s experience.Citation24 In fact, the morphological findings are difficult to compare with functional results.
The WHO morphologically classifies meningiomas into three categories using a grading scheme.Citation25 Patients harboring either grade II or III meningiomas have higher recurrence rates, varying between 29%–52% and 50%–94%, respectively. After gross total resection without postoperative radiation, grade II meningiomas are shown to have a high recurrence rate, with most recurrences occurring within 5 years after the resection.Citation26 A retrospective case series supports the observation that postoperative radiotherapy may result in lower rates of recurrence of atypical meningiomas that have undergone initial gross total resection: actuarial recurrence rates within 5 years were close to 42% without radiotherapy and 20% with radiotherapy.Citation27 In the current study, age and radiotherapy dosage were associated with longer 5- and 10-year actuarial overall survival rates, while size and grading of the tumor influenced the 5- and 10-year disease-free survival rates.Citation28 In the present case, after the patient was diagnosed with meningioma, he received surgical intervention and participated in radiotherapy for the residual tumor. After aggressive rehabilitation, the muscle power in his upper-left limb increased, and the patient exhibited improved walking abilities, with near-complete independence of performing daily activities. Follow-up conducted 1.5 years later showed that the patient had no evidence of recurrence.
Conclusion
In this case report, we demonstrated a patient with brain meningioma with initial clinical symptoms similar to cervical radiculopathy. With the progression of the clinical symptoms, the diagnosis of brain meningioma was finally confirmed, and the patient was treated accordingly. Upon review of the progression of the clinical symptoms, the possibility of a brain lesion could have been identified earlier if the neurological examination was executed carefully. This examination encompasses the patient’s mental status, cranial nerve examination, motor system (muscle strength, upper or lower motor-neuron sign, and muscle tone), deep-tendon reflexes, sensation system, abnormal gaits, and coordination, and also the pattern and distribution of neurologic defects.
Acknowledgments
This study is supported in part by Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (DOH102-TD-B-111-004).
Disclosure
The authors report no conflicts of interest in this work.
Reference
- LuYTLanMYLiuJSChenWHAn unusual presentation of hypokalemic paralysis with evolving pure motor hemiparesisJ Clin Neurosci201118571671921349722
- WaldropMADiagnosis and treatment of cervical radiculopathy using a clinical prediction rule and a multimodal intervention approach: a case seriesJ Othop Sports Phys Ther2006363152159
- Apelby-AlbrechtMAnderssonLKleivaIWKvåleKSkillgateEJosephsonAConcordance of upper limb neurodynamic tests with medical examination and magnetic resonance imaging in patients with cervical radiculopathy: a diagnostic cohort studyJ Manipulative Physiol Ther201336962663224161389
- CaridiJMPumbergerMHughesAPCervical radiculopathy: a reviewHSS J20117326527223024624
- OstromQTGittlemanHFarahPCBTRUS statistical report: Primary brain and central nervous system tumors diagnosed in the United States in 2006–2010Neuro Oncol201315Suppl 2ii1ii5624137015
- NakasuSNakasuYFukamiTJitoJNozakiKGrowth curve analysis of asymptomatic and symptomatic meningiomasJ Neurooncol2011102230331020686821
- YoneokaYFujiiYTanakaRGrowth of incidental meningiomasActa Neurochir (Wien)2000142550751110898357
- WhittleIRSmithCNavooPCollieDMeningiomasLancet200436394201535154315135603
- LiuZWangCWangHWangYLiJYLiuYClinical characteristics and treatment of angiomatous meningiomas: a report of 27 casesInt J Clin Exp Pathol20136469570223573316
- SarafSMcCarthyBJVillanoJLUpdate on meningiomasOncologist201116111604161322028341
- CushingHEisenhardtLMeningiomas. Their classification, regional behaviour, life history and surgical end resultsBull Med Libr Assoc1938272185
- AdegbiteABKhanMIPaineKWTanLKThe recurrence of intracranial meningiomas after surgical treatmentJ Neurosurg198358151566847909
- KhalatbariMGhalenouiHYahyaviSTBorghei-RazaviHLeft somatosensory cortex tumor presented with radicular hand pain and paresthesiaArch Iran Med200811110710918154431
- JelladABen SalahZBoudokhaneSMigaouHBahriIRejebNThe value of intermittent cervical traction in recent cervical radiculopathyAnn Phys Rehabil Med200952963865219846359
- SchottGPenfield’s homunculus: a note on cerebral cartographyJ Neurol Neurosurg Psychiatry1993563293338482950
- DillinWBoothRCucklerJBalderstonRSimeoneFRothmanRCervical radiculopathy: a reviewSpine (Phila Pa 1976)198611109889913576348
- GorterKInfluence of laminectomy on the course of cervical myelopathyActa Neurochir (Wien)1976333–4265281941717
- LunsfordLDBissonetteDJJannettaPJSheptakPEZorubDSAnterior surgery for cervical disc disease. Part 1: Treatment of lateral cervical disc herniation in 253 casesJ Neurosurg19805311117411195
- WalterCAHistological studies on the localisation of cerebral functionBr J Psychiatry190450211651662
- GoreDRSepicSBGardnerGMRoentgenographic findings of the cervical spine in asymptomatic peopleSpine (Phila Pa 1976)19861165215243787320
- MatsumotoMFujimuraYSuzukiNMRI of cervical inter-vertebral discs in asymptomatic subjectsJ Bone Joint Surg Br199880119249460946
- Kalsi-RyanSKaradimasSKFehlingsMGCervical spondylotic myelopathy: the clinical phenomenon and the current pathobiology of an increasingly prevalent and devastating disorderNeuroscientist201319440942123204243
- JensenMCBrant-ZawadzkiMNObuchowskiNModicMTMalkasianDRossJSMagnetic resonance imaging of the lumbar spine in people without back painN Engl J Med1994331269738208267
- WainnerRSGillHDiagnosis and nonoperative management of cervical radiculopathyJ Orthop Sports Phys Ther2000301272874411153552
- LouisDNOhgakiHWiestlerODThe 2007 WHO classification of tumours of the central nervous systemActa Neuropathol200711429710917618441
- AghiMKCarterBSCosgroveGRLong-term recurrence rates of atypical meningiomas after gross total resection with or without postoperative adjuvant radiationNeurosurgery20096415660 discussion 6019145156
- KomotarRJIorgulescuJBRaperDMThe role of radiotherapy following gross-total resection of atypical meningiomasJ Neurosurg2012117467968622920955
- DettiBScocciantiSDi CataldoVAtypical and malignant meningioma: outcome and prognostic factors in 68 irradiated patientsJ Neurooncol2013115342142724045968
