Abstract
Objective
Recent studies have shown that sleep problems occur in migraineurs and poor sleep causes chronification, but the mechanisms by which chronic migraine affects sleep quality are still unknown. This review aims to analyze commonly reported sleep disturbances in chronic migraine (CM) and determine the effect of CM on sleep quality.
Materials and Methods
We conducted a comprehensive review of all published articles on CM and sleep quality from inception to March 2022 in the literature. Clinical trials, observational studies, and case series (≥20 cases) were included. Two reviewers and a supervisor reviewed the titles and abstracts of all search results with predefined inclusion and exclusion criteria. PubMed search for randomized controlled trials and open studies on CM and sleep quality reported in English between 1983 and 2022 was conducted using the keywords including chronic migraine, sleep, insomnia, sleep quality, polysomnography, and Pittsburgh Sleep Quality Index.
Results
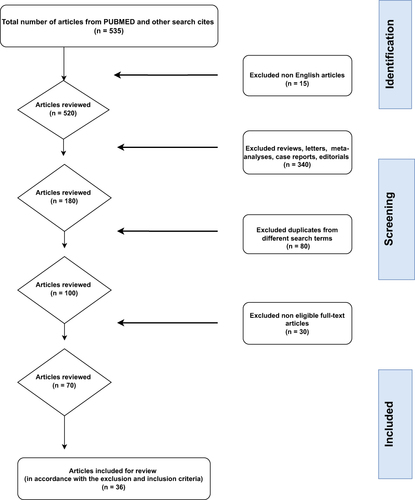
A total of 535 potentially relevant articles were found. A total of 455 articles and reviews, meta-analyses published in any language other than English, with other exclusion criteria, were excluded from the review. In the remaining articles, 36 clinical studies, reviewing sleep quality and its association with migraine, were identified and reviewed. Evidence from this review shows that poor sleep and migraine chronicity are intertwined with other accompanying comorbidities and dysregulation of circadian rhythm that innovative treatments promise to bring relief to both poor sleep as well as migraine.
Conclusion
Sleep disorders are common in CM and the association between migraine chronification and sleep quality is bidirectional. Comorbid conditions with accompanying frequent attacks in migraine may impair sleep quality. While the maladaptive pain process worsens sleep, poor sleep quality also negatively affects migraine pain. Sleep disturbance, which is affected by worsening migraine attacks, causes deterioration in the quality of life, loss of workforce, and economic burden.
Introduction
Chronic migraine (CM) is a headache emerging 15 days or more per month for more than three months, which is migraine-like for at least eight days or more per month. It could lead to complications such as work disability, loss of workforce, and deteriorating quality of life.Citation1 Global studies show that ∼1.4–2.2% of the world’s population is diagnosed with CM.Citation2 Clinical studies involving the diagnosis and management of chronic pain are important because of various symptomatology, comorbidities, and risk of disability.Citation3
Sleep is one of the most important physiological processes and it is considered a period of rest and recovery for the body.Citation4,Citation5 Sleep supports cognitive functions, mood, and memory, and ensures the proper functioning of the endocrine and immune systems.Citation5,Citation6 In addition, sleep is a sensitive regulator of the circadian rhythm, in which biological, environmental (eg exposure to natural light), and behavioral factors are regulated.Citation7 The association between sleep and migraine is complex and bidirectional, as changes in sleep may trigger migraine and be important in its symptom and treatment.Citation8
There is a relationship between migraine and sleep, which has not been fully understood yet in terms of pathogenesis.Citation9 Insomnia can trigger migraine attacks, and sleep is disrupted during attacks.Citation10–12 Sleep disorders and headaches overlap clinically and have pathophysiological, anatomical, and physiological similarities.Citation13 The increasing number of evidence suggests that there may also be a common underlying etiology. Sleep deprivation, which is associated with migraine pathology,Citation11 results in decreased pain inhibition and dysfunction of the pathway, leading to the development of central sensitization and pain amplification.Citation14,Citation15
Certain lifestyle factors and comorbidities have also been confirmed as risk factors for the development of CMCitation16 and sleep disturbances are well-known risk factors for migraine chronification.Citation6,Citation17 Changes in sleep-wakefulness patterns, such as sleep deprivation, and disorders such as insomnia, restless leg syndrome, sleep apnea, and poor sleep quality-duration are also common migraine triggers.Citation11,Citation18–20 Conditions that disrupt the cycle, such as shift work, may also contribute to the exacerbation of migraine attacks.Citation21
Patients with CM have reported shorter nighttime sleep duration compared to those with episodic migraine (EM) and have been more likely to initiate sleep, maintain sleep, and show sleep-inducing headaches. Also, complaints of insomnia symptoms were at least three times more common than in the general population.Citation22 In contrast, targeted behavioral sleep intervention can provide improvement in headache frequency and conversion from CM to EM.Citation23
Poor sleep is often found during the premonitory or postdrome migraine stages.Citation24,Citation25 Poor sleep quality is associated with the developmental process of CM.Citation26 Sleep disturbance impairs endogenous pain-relieving function and increases spontaneous pain, especially headache.Citation27 Studies reported in the literature have tried to explain possible associations between chronic pain and sleep by common biochemical mediators such as serotonin, melatonin, orexins, dopamine, and adenosine, which play a role in both migraines and sleep disorders.Citation6,Citation28
Neuroimaging studies on CM have found functional and microstructural changes in the brainstem, hypothalamus, basal ganglia, and cortex, which are involved in pain processing. Changes may be associated with headache frequency and/or duration, insomnia, and other comorbidities such as depression and anxiety.Citation29–32
The purpose of this review is to review the effect of CM on sleep quality in light of current scientific literature. Studies will be generally presented in the form of the relationship between CM and sleep, the relationship between etiological causes, and the analysis of sleep quality after migraine treatment. In the literature, there is an increasing number of studies on the relationship between migraine and sleep disorders in contrast to fewer studies discussing the subject of chronic migraine and sleep quality, with most focusing on how poor quality sleep leads to migraine being transformed into its chronic form. In our review, we investigated how sleep-related diagnostic scales or methods can affect sleep as well as treatment interventions.
Materials and Methods
To study the interaction between CM and sleep quality, sleep studies conducted with CM patients older than 18 years of age with no structural lesions in the brain and pregnancy excluded were reviewed. The search was conducted on PubMed and Google Scholar for research articles with ≥20 cases, and relevant observational studies published between 1983 and 2022 using the keywords chronic migraine, sleep, sleep quality, insomnia, insufficient sleep, insomnia, sleep disorders, polysomnography, actigraphy. The last search date used was March 2022. Articles were selected through an independent, unbiased selection of articles using appropriate keywords. Studies were also distinguished for the initial evaluation by examining the references of the articles. Unpublished studies the full versions of which were unavailable, those that did not diagnose CM according to the “International Classification of Headache Disorders” for the diagnosis of migraine and did not meet the criteria for sleep disorders according to the “International Classification of Sleep Disorders” were excluded.
All abstracts of the articles in English meeting search criteria were reviewed. shows the progress of article selection and the number of articles in each step. The review was conducted with a focus on CM and sleep quality and sleep disorders.
Our article exclusion criteria consisted of review articles, meta-analyses, letters, editorials, case reports or studies with <20 patients, opinion articles, and abstracts with no full articles published.
Questionnaires, Scales Used in Studies
In this review, the studies that used the following scales, the validity, and reliability of which was ensured for the respective studies, were analyzed: “Pittsburgh Sleep Quality Index (PSQI), Insomnia Severity Index (ISI), International Restless Legs Syndrome study group consensus criteria (IRLSSG), Epworth Sleepiness Scale (ESS), Somatic symptom qualitative and quantitative questioning, Medical Outcomes Study (MOS) Sleep scale, tests six dimensions of sleep, including initiation, maintenance (eg staying asleep), quantity, adequacy, somnolence (eg drowsiness), and respiratory impaired breaths (eg shortness of sleep problems), Sleep quantity score, Sleep Condition Indicator (SCI), Stanford Sleepiness Scale (SSS), SLP6 index, which is a summary of sleep problems based on adequacy, shortness of breath, and somnolence, Dysfunctional Beliefs, and Attitudes about Sleep (DBAS), Pre-sleep arousal scale, Berlin Questionnaire”.
Results
As a result of the search conducted on electronic databases, 535 articles published between 1983 and 2022 were found for review of titles and abstracts ().
The search was completed with a total of 36 articles meeting the search and inclusion criteria for full-text review. These eligible articles were reviewed by two reviewers for eligibility based on the relationship of title, abstract, and statistical results review. Thirty articles could not be accessed even through the library of our university.
The studies reviewed were performed in multiple geographic regions and included case-control, prevalence study, prospective cohort study, and sleep assessment after intervention with interventional-behavioral-digital or drug therapy. The review was carried out by focusing on the studies conducted in the field of CM and sleep and the studies in which we obtained significant statistical results from the relevant research. Studies that did not provide specialized statistics for CM patients among general migraine patients were excluded from the review. In the study, studies in which the relationship between scales and sleep quality was evaluated in general are presented in , while studies in which sleep was evaluated by applying migraine treatment with medication or other treatments are summarized in .
Table 1 Summary of Results from Published Studies of CM and Sleep Without Treatment Intervention
Table 2 Summary of Findings from Studies Evaluating the Effect of Various Treatments for CM on Sleep Quality
The Role of Sleep in the Chronicity Process and Accompanying Comorbidities
Headache, a progressive form characterized by increases in frequency, severity, duration, and resistance of migrainous attacks may evolve into CMCitation33 and chronicity occurs in about 3% of EM patients.Citation34,Citation35 The coexistence of neural pathways involved in pain processing and genetic factors is responsible for this course.Citation36
Various comorbidities and risk factors associated with migraine chronification are well defined.Citation16,Citation35 Identified triggers and aggravating factors appear as emotional and physical stress, nutrition, and sleep disturbances.Citation37,Citation38 Poor sleep plays an important role in the chronicity process.Citation39 Lifestyle and behavioral changes, and acute and prophylactic treatments should be planned together to reduce the frequency, severity, and duration of migraine attacks.Citation40
Understanding specific comorbidities in migraine is important for several reasons. First, recognition of migraine comorbidities may help understand the genetic or biological mechanisms that support the development of new treatments and facilitate disease management, and may also improve prognosis.Citation41 The identification of migraine comorbidities can also help in the development of new treatments for subgroups and the recognition of underlying biological diseases.Citation42
Sleep Disorders and the Importance of Circadian Rhythm in Chronic Migraine
Previous studies evaluated a wide spectrum of sleep disorders commonly seen in migraine patients, including insomnia, increased daytime sleepiness, poor sleep quality, prolonged sleep latency, sleep apnea, restless legs syndrome, and parasomnia.Citation6,Citation43 In patients with CM, headache is highly accompanied by insomnia, poorer sleep, sleep disturbances, and sleep insufficiency.Citation44
It has been suggested that excessive sleep and sleep deprivation are the most common causes of morning migraine attacks.Citation45 Problems such as sleep deprivation, excessive sleeping, or inability to sleep regularly may be an important factor in the transition from the episodic to the chronic form of migraine.Citation9 Most of the available data in the literature comes from self-administered self-report scales. In our review, by PSQI, ISS, IRLSSG, ESS, qualitative and quantitative questioning of somatic symptoms, we observed a high rate of concomitant sleep disorders, insomnia, RLS, and increased daytime sleepiness, impaired sleep quality, and snoring in CM patients.Citation41,Citation46–53 However, it is noteworthy that there are differences in the studies conducted. Rothrock et al’s study of a quantitative investigation of migraine triggers showed that too much or little sleep was not a trigger with increased risk for chronic migraineurs, contrary to expectations. They identified a correlation between having more frequent migraine headaches or longer exposure to the disease and improved ability to identify and compensate for triggers.Citation54 Viana et al found insomnia comorbidity severe enough to require hypnosis in the CM-drug overuse headache (MOH) group. They also found the rate of snoring to be higher in the chronic group than in the EM group.Citation49
Insomnia, RLS in Chronic Migraine
Insomnia-related mechanisms emphasize hyperalgesic state resulting from reduced inhibition of the pain pathway, caused by sleep deprivation and fragmented sleep, as well as the importance of desensitization of nociceptors by increased proinflammatory cytokine cascade.Citation49 Again, in the CaMEO study, the study in which extensive web-based analysis was performed, the rates of both snoring and insomnia were high in CM, compared to EM, according to the MOS sleep scale and Berlin questionnaire.Citation18 Similarly, Lucchesi et al and Ceylan et al reported a higher PSQI score in CM compared to EM, but Lucchesi et al found similar levels of daytime sleepiness in the EM and CM groups.Citation50,Citation51
In another study investigating RLS and sleep quality in CM and EM, the rate of RLS was high in CM patients, and sleep quality worsened in patients with RLS.Citation52 For this study, CM patients were overweight, which is a risk factor for apnea. Shortness of breath as poor sleep quality with a high risk of chronification (17.0 vs 9.5), and daytime somnolence (33.2 vs 21.9), sleep adequacy (38.7 vs 60.5) were less in these patients compared to those with episodic migraine.
Central Sensitization, Circadian Rhythm, Melatonin in Chronic Migraine
Tommaso et al investigated central sensitization in the form of detailed interviews in all primary headache groups (including CM) with MOS, the Sleep Problems Index (SLP6), sleep quantity (SLPQRAW) scales and found that sleep duration was decreased in the CM group about short sleep duration, central sensitivity symptoms, and chronicity in CM patients. However, MOS scores did not correlate with central sensitization symptoms between the different groups.Citation53 The study also emphasized that the relationship between allodynia, pericranial sensitivity, and short sleep characterizes chronic migraine more than other primary headaches. Increased frequency of headaches and unexpected nocturnal or early morning awakenings may cause sleep fragmentation; difficulty falling asleep and lack of sleep are triggers for the majority of patients with migraine.Citation55 Cutaneous allodynia, which is a prominent symptom during migraine attacks, has been shown to worsen in response to REM sleep deprivation,Citation56 which may indicate the importance of allodynia in the wakefulness-REM-NREM transitions in migraine. They discussed that the triggering mechanism between chronic pain attack and sleep may be due to the interaction between the circadian rhythm influence and the inhibition of the nociceptive pathway as a result of increased expression in orexin receptors.Citation53
In their study investigating the circadian rhythm difference in attacks using MOS, and sleep quantity score, the authors did not find a rhythm difference in the time of onset of headache in CM patients compared with EM.Citation57 In another study evaluating the circadian periodicity of migraine patients, migraine attacks were frequently in the early morning hours, and the study characterized patients with an early chronotype.Citation58 However, Tommaso et alCitation57 discussed the inadequacy of the consistency of headache diaries and the inclusion of only chronically followed patients as limitations in their study.
In the majority of studies, circadian differences found in patients with headache showed the greatest pain sensitivity at night and in the early morning,Citation59,Citation60 and CM patients who received botox as their headache treatment also found that morning therapy was more painful.Citation61 Among the studies conducted to show the place and importance of the circadian rhythm in CM, in a pilot study comparing EM and CM patients, Ong et al conducted wrist actigraphy and Dim light melatonin onset (DLMO) measurements. In CM, the number of headache days per month was significantly associated with DLMO and later sleep episodes.Citation62 There was no evidence that individuals with CM would have a delayed circadian phase compared to healthy subjects. They pointed out that circadian dysregulation may be an explanatory bridging mechanism between CM and insomnia and other comorbidities. Melatonin to be used in the treatment of migraine may improve the circadian phase and provide positive bidirectional interaction for both headaches and sleep.Citation62
Peres et al collected serum for hourly hormone determination for 17 hours and 12 hours in CM and the control group to monitor hypothalamic and pineal functions. As for one of the hormones tested, melatonin, they found a delayed nocturnal melatonin peak in patients with CM and lower concentrations of melatonin in patients with CM accompanied by insomnia.Citation63 Apart from the small sample size of the study, the fact that drug detoxification was provided and that patients with accompanying insomnia provided a clear diagnosis also provide valuable data. The circadian rhythm of melatonin secretion is regulated by the suprachiasmatic nucleus in the hypothalamus.Citation64 The results of the study supported the theory that hypothalamic involvement in CM causes a chronobiological dysfunction. While the interpretation of migraine as a cause or a result cannot be made, it has also been discussed that it may be related to sleep disorders. This study emphasized that melatonin is an endogenous scavenger and may be an alternative in treatment.
For circadian periodicity of pain, ion channels involved in pain responses are thought to be managed by circadian variations in the expression and activity levels. Pro-inflammatory cytokines, chemokines secreted by control genes of non-clock gene expressions and hormone concentrations as well as glial activity levels regulate the circadian rhythm.Citation65 In addition, prodromal insomnia with an increase in the number of nighttime awakenings before the migraine attack has been reported. Disruption of REM sleep is among the findings discussed as an underlying mechanism of untimely awakening and nocturnal migraine attacks.Citation12
Predictors of Sleep Disturbance in Chronic Migraine Chronic Migraine
Sleep disturbance, increased headache frequency, analgesic overuse, and depression are the strongest risk factors for the new onset of CM.Citation44,Citation66 In a recent study investigating the predictors of sleep quality, Pedrón et al showed that depressive symptoms, pain, and headache-related disability had a 33% role in affecting sleep quality.Citation67
Another study investigating the effect of isolation of the COVID process on insomnia recently demonstrated that there was an increase in monthly headache frequency and ISI score with isolation in migraine groups, most of which comprised CM patients.Citation68 Currò et al showed that in CM sufferers during the COVID quarantine period, decreased sleep duration and quality, prolonged sleep latency, and ultimately higher PSQI values were associated with worsening depression/anxiety and increased migraine attack frequency. This study showed that reduced sleep duration is associated with an increase in migraine attack duration and pain.Citation69
Stress is the trigger for poor sleep and migraine chronification.Citation21,Citation70 Quarantine is a lifestyle that increases stress.Citation71 Ultimately, different circadian habits and decreased physical activity associated with stress, anxiety, or depression may affect patients’ sleep disturbances, leading to a potential increase in migraine attack frequency.Citation72 A previous review suggested that conditions such as stress levels increasing with disruption of the sleep-wakefulness cycle, and shift work may also contribute to an exacerbation of migraine attacks.Citation21
High attack frequency in CM was associated with poor and weak sleep; sleep with incomplete restoration is seen as poor sleep habits, short sleep time, and longer sleep latency.Citation44 Fragmented sleep is generally not restorative and negatively affects daytime performance; moreover, reduced sleep efficiency and increased waking up after sleep onset have recently been identified as a trigger for migraine.Citation73
Regarding the effects of migraine on sleep quality, we examined the vulnerabilities that should be emphasized because both of them create a negative interaction with each other. Anxiety, stress, depression, pain and sleep problems negatively affect the daily living activities and lives of individuals and become a great burden on both sleep and CM in terms of providing treatment modalities always in cooperation with different disciplines.
Common Pathophysiological Mechanisms in Migraine and Sleep
Insomnia is the most common sleep disorder among migraine sufferers and the relationship appears to be bidirectional.Citation74 Many studies in the literature discussed that insomnia triggers migraine. However, it has also been noted that migraine is a precursor to insomnia.Citation75 Fragmented sleep caused by migraine headaches can lower the pain threshold, as well as increase the risk of migraine attacks due to their role in the pathophysiology of monoaminergic disorders such as serotonin and dopamine that occur in sleep disorders. As a result, migraine and sleep disorders have been hypothesized to have a possible similar pathogenetic role.Citation11
In addition, adenosine levels rise during migraine attacks and induce sensitivity to pain.Citation76 In the case of sleep deprivation, overstimulation of A1 receptors and adenosine overload is a possible mechanism that modulates neuronal activity and CSD because adenosine A1 receptor activation contributes to the persistent secondary phase of Leão’s cortical spreading depression developing in the attack.Citation77,Citation78
Despite the emphasis on the effectiveness of orexinergic pathways and the importance of melatonin treatment in migraine patients, it is obvious that there is still a lack of sleep quality in migraine. This leads researchers to conduct further studies on sleep in migraine.Citation79 The hypothalamic orexinergic system plays a critical role in sleep/wakefulness transitions and stabilizing REM sleep and has been linked to migraine.Citation80
Calcitonin gene-related peptide (CGRP), a neuropeptide known to be a major player in migraine, may play a role in regulating nighttime sleep maintenance.Citation81,Citation82 A clear understanding of the etiological disorders can reduce the risk of chronicity with the identification and treatment of both sleep disorders and migraine.Citation83
The varying volume of various regions of the prefrontal cortex, occipital lobe, right putamen, 4th ventricle, optic chiasm, and thalamus in migraine patients may indicate central plasticity in the pathogenesis and chronification of migraine.Citation84 Chen et al’s study reported that basal forebrain volume was negatively associated with the sleep disturbance scale, supporting that altered basal forebrain may be associated with poorer sleep in migraine patients.Citation84 It should also be noted that the deep gray matter structure and the thalamus, which is responsible for the modulation of visual information in migraine, have a role in regulating the sleep-wakefulness cycle.Citation85
During sleep, the glymphatic system, which functions as a CNS waste clearance system and helps clear abnormal proteins, is responsible for a wide variety of homeostatic functions. Since glymphatic activity is primarily a sleep-related activity, dysregulation of sleep processes can result in the accumulation of CNS wastes with nociceptive properties; this supports the view that how sleep triggers migraine, how it relieves migraine, and how it contributes to migraine chronification.Citation11
Evaluation of Sleep Quality After Treatment of Chronic Migraine
Comorbid conditions complicate the treatment of migraine. Current migraine treatments either reduce pain or prevent the occurrence of migraine.Citation86 The treatment algorithm was arranged based on the relationships between migraine, sleep disorders, triggers, and psychiatric conditions. The sleep diary is the gold standard in headache management to identify triggers, confirm the diagnosis, guide behavioral therapy, and evaluate outcomes.Citation74 If there is accompanying insomnia, hypnotics, and cognitive behavioral treatment may be beneficial, if there is insomnia with accompanying anxiety -depression, migraine prophylaxis with sedative antidepressants or anticonvulsants may provide relief, while hypersomnia requires neutral or more stimulant drugs.
In studies investigating the role and place of treatments applied in CM in regulating sleep quality, transcranial direct stimulation, GON-B, monthly erenumab therapy, digital cognitive behavioral therapy, botulinum toxin, occipital nerve stimulation, cognitive-behavioral therapy, behavioral insomnia treatment, non-invasive vagus nerve stimulation (nVNS), effective dose topiramate therapy and nefazodone treatment as 5HT2 antagonist have been examined in comparison with many other scales, especially PSQI, and actigraphy, and the quality of sleep was evaluated after the treatments applied. Groups have sometimes been studied in groups with medication overuse headache patients or chronic tension headache patients.
Starting with the most recent, Icco et al demonstrated that in the study of patients receiving double-blind controlled treatment, after transcranial direct stimulation procedure was evaluated with SCI, PSQI, and SSS scales, sleep quality improved with treatment.Citation87 In the studies of Saçmacı and Ulusoy, in which the effects of GON-B treatment in CM were evaluated, after 3 months of migraine treatment, sleep quality and insomnia improved with PSQI and other scales, and even according to Saçmacı et al’s study, daytime sleepiness level decreased, pre-arousal states before sleep and even dysfunctional behaviors and attitudes towards sleep improved.Citation88,Citation89 GONB treatment may be initially considered if comorbidities such as stress, depression and sleep disturbance are high in CM patients with few treatment options.Citation88
Behavioral insomnia therapy accompanied by actigraphy was found to result in significant improvements in total sleep duration and sleep efficiency according to both actigraphy and PSQI in patients with CM accompanied by insomnia.Citation90 In the general migraine patient group with CM at a rate of 9.5%, the PSQI score was the highest in the group with CM. In addition, increased migraine frequency and RLS are independent risk factors for poor sleep.Citation12 Digital cognitive therapy was applied for 12 weeks to patients with insomnia and CM significantly improved insomnia.Citation91
In a study of patients with large CM series,Citation92 Blumenfeld et al showed that sleep quality reported by PSQI improved after botox treatment, whereas Aydınlar et al’s study with prospective series demonstrated that sleep quality did not significantly improve compared to PSQI in patients with initially intense depressive features.Citation93 Other comorbidities, such as accompanying depression, are obstacles to treatment success. Loeb et al found the therapeutic effect of Laser therapy and botox therapy on sleep in favor of LBBT in their group comprising patients with CM.Citation94 In a study, however, the successful ameliorative effects of botox treatment on pain frequency and severity and depression in the CM group with high comorbidities could not be demonstrated objectively on sleep, and the need for multidisciplinary treatment was emphasized.Citation95 Onabotulinumtoxin A treatment may help improve sleep in migraine patients by reducing the amount of activated CGRP.Citation96
Rodrigo et al proved the success of occipital nerve stimulation therapy in improving sleep quality, finding that it resulted in improvement in 91% of 37 patients with refractory CM.Citation97 They showed that there was an overall improvement in the PSQI score in the “sleep delay and daytime dysfunction” subgroups in EM and CM patients treated with non-invasive vagus nerve stimulation (nVNS).Citation98
In a study conducted to elucidate the possible side effects of topiramate therapy, used in the treatment of migraine, on sleep, they showed that only two (4%) of 50 patients who tried topiramate therapy had a side effect of insomnia.Citation99 In the evaluation of the 5HT2 antagonist Nefazodone treatment in patients mostly with CM, post-treatment sleep score as a visual analog scale improved significantly.Citation100 Russo et al proved that after a 6-month monthly erenumab treatment, there was a significant improvement in sleep quality according to MOS Sleep Scale.Citation101 In conclusion, studies, consistent with the literature, show that preventive chronic migraine treatments, behavioral interventions such as BDT, and relaxation training also improve sleep in migraine patients.Citation102
Summary of a Sleep Disorder in CM
First of all, it is necessary to recognize the comorbidities associated with chronic migraine and to understand the importance of sleep and the way it interacts with other risk factors. Each of these diseases is intertwined. In our review, sleep was mainly analyzed using scale approaches, and it is noteworthy that especially there are a limited number of studies utilizing polysomnographic and biochemical methods. In addition, there are fewer studies investigating the effect of pure chronic migraine on sleep, with existing studies more commonly focused on treating chronic headaches or the episodic group. Some studies have mentioned a pathway that can adapt to the chronic process, while others have discussed the transformation of the chronic process into a maladaptive process. Also, more elaborative studies have not addressed all sleep disorders. Again, a more comprehensive evaluation has not been made for chronicity, whether it is poor sleep or frequent attacks. Although there are several experimental studies on pain pathways and sleep mediators for chronic migraine, there is no clear consensus on the importance of circadian rhythm and neurohypophyseal pathway studies. Many studies have emphasized how individual therapeutic methods for migraine headaches can improve sleep, ie, the importance of killing two birds with one stone.
Limitations
There are inevitably limitations that need to be addressed in addition to the above-mentioned summary of findings. The studies included in this review had a small number of patients and different study designs. In addition, self-report scales were used to evaluate sleep quality in studies. The lack of PSG studies that objectively evaluate sleep architecture is an important shortcoming. This will be important in terms of fully understanding the sleep profile in CM and providing effective sleep interventions. In addition, more emphasis placed on functional and longitudinal studies investigating common neuroanatomical pathways for migraine and sleep will enrich the literature. Since sleep quality assessment appears as a side (sub) data in many studies, the effects of this on migraine frequency, severity, and duration have not been evaluated. Another limitation of the literature is that patients with CM were evaluated under treatment. Ultimately, it will be very important to evaluate the patients who receive and those who do not receive treatment together.
Conclusion
This review aimed to analyze the association between migraine chronicity and sleep quality and the mutual effects of sleep and migraine on one another. The findings show that adults with CM achieve significantly higher scores on the PSQI than healthy controls or episodic patients and that treatments primarily intended for pain relief in CM also have a positive effect on sleep. However, there is a lack of more elaborate studies on sleep disorders. For example, a comprehensive analysis of all sub-titles such as parasomnias or the relationship of restless legs syndrome should have been conducted. Large biochemical studies and sleep analysis studies in larger populations have not addressed circadian rhythm disturbances also.
CM, as a disease, disrupts sleep quality with many triggering factors. It provokes the pain process again in disturbed sleep. Therefore, if this interaction chain is not broken in itself, the pathophysiology can continue in two directions. In general, although current studies provide guidance, further studies on sleep in migraine should be undertaken. Because there is no consensus on whether patients show objective changes in sleep architecture. We are likely to detect significant differences with further studies. Based on all the studies, a better insight into the relationship between migraine as a common and chronic disease, first of all, enables the provision of treatments before the conditions become more complicated and achievement of significant developments in the field of individual, mental, public health, and well-being.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Author Contributions
All authors made a significant contribution to the work reported, either in all or part of the conception, study design, execution, acquisition of data, analysis, and interpretation phases, took part in drafting, revising, or critically reviewing the article, and gave final approval of the version to be published, agreed on the journal to which the article will be submitted and agreed to be accountable for all aspects of the work.
Disclosure
The authors declare no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Additional information
Funding
References
- Pescador Ruschel MA, De Jesus O. Migraine headache. In: StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC; 2022.
- Stovner LJ, Nichols E, Steiner TJet al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:954–976. doi:10.1016/S1474-4422(18)30322-3
- Huntsman DD, Bulaj G. Healthy dwelling: design of biophilic interior environments fostering self-care practices for people living with migraines, chronic pain, and depression. Int J Environ Res Public Health. 2022;19(4):2248. doi:10.3390/ijerph19042248
- Hutka P, Krivosova M, Muchova Z, et al. Association of sleep architecture and physiology with depressive disorder and antidepressants treatment. Int J Mol Sci. 2021;22:1333. doi:10.3390/ijms22031333
- Maurovich-Horvat E, Pollmacher T, Sonka K. The effects of sleep and sleep deprivation on metabolic, endocrine and immune parameters. Prague Med Rep. 2008;109:275–285.
- Waliszewska-Prosół M, Nowakowska-Kotas M, Chojdak-łukasiewicz J, Budrewicz S. Migraine and sleep—an unexplained association? Int J Mol Sci. 2021;22:5539. doi:10.3390/ijms22115539
- Potter GD, Skene DJ, Arendt J, Cade JE, Grant PJ, Hardie LJ. Circadian rhythm and sleep disruption: causes, metabolic consequences, and countermeasures. Endocr Rev. 2016;37:584–608. doi:10.1210/er.2016-1083
- Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27:394–402. doi:10.1111/j.1468-2982.2007.01303.x
- Goadsby PJ, Holland PR, Martins-Oliveira M, Hoffmann J, Schankin C, Akerman S. Pathophysiology of migraine: a disorder of sensory processing. Physiol Rev. 2017;97(2):553–622. doi:10.1152/physrev.00034.2015
- Rains JC, Poceta JS, Penzien DB. Sleep and headaches. Curr Neurol Neurosci Rep. 2008;8(2):167–175. doi:10.1007/s11910-008-0027-9
- Vgontzas A, Pavlović JM. Sleep disorders and migraine: review of literature and potential pathophysiology mechanisms. Headache. 2018;58:1030–1039. doi:10.1111/head.13358
- Lin YK, Lin GY, Lee JT, et al. Associations between sleep quality and migraine frequency: a cross-sectional case-control study. Medicine. 2016;95:e3554. doi:10.1097/MD.0000000000003554
- Altamura C, Corbelli I, de Tommaso M, et al. Pathophysiological bases of comorbidity in migraine. Front Hum Neurosci. 2021;15:640574. doi:10.3389/fnhum.2021.640574
- Arendt‐Nielsen L, Morlion B, Perrot S, et al. Assessment and manifestation of central sensitisation across different chronic pain conditions. Eur J Pain. 2018;22:216–241. doi:10.1002/ejp.1140
- Krause AJ, Prather AA, Wager TD, Lindquist MA, Walker MP. The pain of sleep loss: a brain characterization in humans. J Neurosci. 2019;39:2291–2300. doi:10.1523/JNEUROSCI.2408-18.2018
- Buse DC, Greisman JD, Baigi K, Lipton RB. Migraine progression: a systematic review. Headache. 2019;59:306–338. doi:10.1111/head.13459
- Duman T, Dede Ö, Uluduz H, Seydaoğlu D, Okuyucu G, Melek İ. Sleep changes during prophylactic treatment of migraine. Ann Indian Acad Neurol. 2015;18:298–302. doi:10.4103/0972-2327.160084
- Buse DC, Rains JC, Pavlovic JM, et al. Sleep disorders among people with migraine: results from the chronic migraine epidemiology and outcomes (CaMEO) study. Headache. 2019;59:32–45. doi:10.1111/head.13435
- Kim J, Cho SJ, Kim WJ, Yang KI, Yun CH, Chu MK. Insufficient sleep is prevalent among migraineurs: a population-based study. J Headache Pain. 2017;18:50. doi:10.1186/s10194-017-0756-8
- Wöber C, Wöber-Bingöl C. Triggers of migraine and tension-type headache. Handb Clin Neurol. 2010;97:161–172.
- Sandoe CH, Sasikumar S, Lay C, Lawler V. The impact of shift work on migraine: a case series and narrative review. Headache. 2019;59(9):1631–1640. doi:10.1111/head.13622
- Kelman L, Rains JC. Headache and sleep: examination of sleep patterns and complaints in a large clinical sample of migraineurs. Headache. 2005;45:904–910. doi:10.1111/j.1526-4610.2005.05159.x
- Sullivan DP, Martin PR, Boschen MJ. Psychological sleep interventions for migraine and tension-type headache: a systematic review and meta-analysis. Sci Rep. 2019;9:6411. doi:10.1038/s41598-019-42785-8
- Giffin N, Ruggiero L, Lipton RB, et al. Premonitory symptoms in migraine: an electronic diary study. Neurology. 2003;60:935–940. doi:10.1212/01.WNL.0000052998.58526.A9
- Giffin NJ, Lipton RB, Silberstein SD, Olesen J, Goadsby PJ. The migraine postdrome: an electronic diary study. Neurology. 2016;87:309–313. doi:10.1212/WNL.0000000000002789
- Adams AM, Serrano D, Buse DC, et al. The impact of chronic migraine: the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study methods and baseline results. Cephalalgia. 2015;35:563–578. doi:10.1177/0333102414552532
- Smith MT, Edwards RR, McCann UD, Haythornthwaite JA. The effects of sleep deprivation on pain inhibition and spontaneous pain in women. Sleep. 2007;30:494–505. doi:10.1093/sleep/30.4.494
- Moreno-Ajona D, Villar-Martínez MD, Goadsby PJ. Emerging targets for migraine treatment. Neurol India. 2021;69(7):S98–s104. doi:10.4103/0028-3886.315989
- Androulakis XM, Krebs KA, Jenkins C, et al. Central executive and default mode network intranet work functional connectivity patterns in chronic migraine. J Neurol Disord. 2018;6. doi:10.4172/2329-6895.1000393
- Woldeamanuel YW, DeSouza DD, Sanjanwala BM, Cowan RP. Clinical features contributing to cortical thickness changes in chronic migraine–a pilot study. Headache. 2019;59:180–191. doi:10.1111/head.13452
- Neeb L, Bastian K, Villringer K, Israel H, Reuter U, Fiebach JB. Structural gray matter alterations in chronic migraine: implications for a progressive disease? Headache. 2017;57(3):400–416. doi:10.1111/head.13012
- Schulte LH, Allers A, May A. Hypothalamus as a mediator of chronic migraine: evidence from high-resolution fMRI. Neurology. 2017;88(21):2011–2016. doi:10.1212/WNL.0000000000003963
- Utiumi MAT, Küster JGB, Godk KS, et al. Prevalence of trigeminocervical convergence mechanisms in episodic and chronic migraine. Arq Neuropsiquiatr. 2022;80(5):482–489. doi:10.1590/0004-282x-anp-2021-0095
- Tsai C-K, Tsai C-L, Lin G-Y, Yang F-C, Wang S-J. Sex differences in chronic migraine: focusing on clinical features, pathophysiology, and treatments. Curr Pain Headache Rep. 2022;26:1–9.
- Filipchuk M, Gassmann J, Castro Zamparella T, et al. High rates of (treated) hypothyroidism among chronic migraine patients consulting a specialized headache clinic: are we missing something? Neurol Sci. 2022;43(2):1249–1254. doi:10.1007/s10072-021-05424-7
- Andreou AP, Edvinsson L. Mechanisms of migraine as a chronic evolutive condition. J Headache Pain. 2019;20:117. doi:10.1186/s10194-019-1066-0
- Mollaoğlu M. Trigger factors in migraine patients. J Health Psychol. 2013;18:984–994. doi:10.1177/1359105312446773
- Grozeva V, Mínguez-Olaondo A, Vila-Pueyo M. Experiment in vivo: how COVID-19 lifestyle modifications affect migraine. Front Neurol. 2021;12:744796. doi:10.3389/fneur.2021.744796
- Bigal ME, Lipton RB. What predicts the change from episodic to chronic migraine? Curr Opin Neurol. 2009;22:269–276. doi:10.1097/WCO.0b013e32832b2387
- Frampton JE, Silberstein S. OnabotulinumtoxinA: a review in the prevention of chronic migraine. Drugs. 2018;78:589–600. doi:10.1007/s40265-018-0894-6
- Yin JH, Lin YK. Prevalence and association of lifestyle and medical-, psychiatric-, and pain-related comorbidities in patients with migraineA Cross-Sectional Study. Headache. 2021;61:715–726.
- Scher AI, Bigal ME, Lipton RB. Comorbidity of migraine. Curr Opin Neurol. 2005;18:305–310. doi:10.1097/01.wco.0000169750.52406.a2
- Lin Y-K, Lin G-Y, Lee J-T, et al. Associations between sleep quality and migraine frequency: a cross-sectional case-control study. Medicine. 2016;95:e3554.
- Yang CP, Wang SJ. Sleep in patients with chronic migraine. Curr Pain Headache Rep. 2017;21:39. doi:10.1007/s11916-017-0641-9
- Ong JC, Park M. Chronic headaches and insomnia: working toward a biobehavioral model. Cephalalgia. 2012;32(14):1059–1070. doi:10.1177/0333102412455709
- Lin GY, Lin YK, Lee JT, et al. Prevalence of restless legs syndrome in migraine patients with and without aura: a cross-sectional, case-controlled study. J Headache Pain. 2016;17:97. doi:10.1186/s10194-016-0691-0
- Barbanti P, Aurilia C, Egeo G, Fofi L, Vanacore N. A case-control study on excessive daytime sleepiness in chronic migraine. Sleep Med. 2013;14:278–281. doi:10.1016/j.sleep.2012.10.022
- Maizels M, Burchette R. Somatic symptoms in headache patients: the influence of headache diagnosis, frequency, and comorbidity. Headache. 2004;44(10):983–993. doi:10.1111/j.1526-4610.2004.04192.x
- Viana M, Bottiroli S, Sances G, et al. Factors associated to chronic migraine with medication overuse: a cross-sectional study. Cephalalgia. 2018;38:2045–2057. doi:10.1177/0333102418761047
- Lucchesi C, Baldacci F, Cafalli M, et al. Fatigue, sleep-wake pattern, depressive and anxiety symptoms and body-mass index: analysis in a sample of episodic and chronic migraine patients. Neurol Sci. 2016;37:987–989. doi:10.1007/s10072-016-2505-1
- Ceylan M, Yalcin A. Coexistence of symptoms associated with trigeminal pathways in chronic and episodic migraine and the effects on quality of life. Pain Med. 2019;20:172–179. doi:10.1093/pm/pny118
- Lucchesi C, Bonanni E, Maestri M, Siciliano G, Murri L, Gori S. Evidence of increased restless legs syndrome occurrence in chronic and highly disabling migraine. Funct Neurol. 2012;27:91–94.
- de Tommaso M, Delussi M, Vecchio E, Sciruicchio V, Invitto S, Livrea P. Sleep features and central sensitization symptoms in primary headache patients. J Headache Pain. 2014;15:64. doi:10.1186/1129-2377-15-64
- Andress-Rothrock D, King W, Rothrock J. An analysis of migraine triggers in a clinic-based population. Headache. 2010;50:1366–1370. doi:10.1111/j.1526-4610.2010.01753.x
- Calhoun AH, Ford S, Finkel AG, Kahn KA, Mann JD. The prevalence and spectrum of sleep problems in women with transformed migraine. Headache. 2006;46:604–610. doi:10.1111/j.1526-4610.2006.00410.x
- Kim SH, Park JY, Shin HE, Ryu DW, Kim TW, Park JW. The influence of rapid eye movement sleep deprivation on nociceptive transmission and the duration of facial allodynia in rats: a behavioral and Fos immunohistochemical study. J Headache Pain. 2019;20:1–9. doi:10.1186/s10194-019-0977-0
- de Tommaso M, Delussi M. Circadian rhythms of migraine attacks in episodic and chronic patients: a cross sectional study in a headache center population. BMC Neurol. 2018;18:94. doi:10.1186/s12883-018-1098-0
- van Oosterhout W, van Someren E, Schoonman GG, et al. Chronotypes and circadian timing in migraine. Cephalalgia. 2018;38:617–625. doi:10.1177/0333102417698953
- Burish MJ, Chen Z. Emerging relevance of circadian rhythms in headaches and neuropathic pain. Acta Physiologica. 2019;225:e13161. doi:10.1111/apha.13161
- Junker U, Wirz S. Review article: chronobiology: influence of circadian rhythms on the therapy of severe pain. J Oncol Pharm Pract. 2010;16(2):81–87. doi:10.1177/1078155209337665
- Packard A, Smotherman C. Effect of circadian rhythm on the pain associated with preventive onabotulinumtoxinA injections for migraines. Chronobiol Int. 2020;37:1766–1771. doi:10.1080/07420528.2020.1802290
- Ong JC, Taylor HL, Park M, et al. Can circadian dysregulation exacerbate migraines? Headache. 2018;58:1040–1051. doi:10.1111/head.13310
- Peres MF, Sanchez Del Rio M, Seabra ML, et al. Hypothalamic involvement in chronic migraine. J Neurol Neurosurg Psychiatry. 2001;71:747–751. doi:10.1136/jnnp.71.6.747
- Pandi-Perumal SR, Cardinali DP, Zaki NF, et al. Timing is everything: circadian rhythms and their role in the control of sleep. Front Neuroendocrinol. 2022;100978. doi:10.1016/j.yfrne.2022.100978
- Fonken LK, Frank MG, Kitt MM, Barrientos RM, Watkins LR, Maier SF. Microglia inflammatory responses are controlled by an intrinsic circadian clock. Brain Behav Immun. 2015;45:171–179. doi:10.1016/j.bbi.2014.11.009
- Buse DC, Fanning KM, Reed ML, et al. Life with migraine: effects on relationships, career, and finances from the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study. Headache. 2019;59:1286–1299. doi:10.1111/head.13613
- Garrigós-Pedrón M, Segura-Ortí E, Gracia-Naya M, La Touche R. Predictive factors of sleep quality in patients with chronic migraine. Neurologia. 2022;37:101–109. doi:10.1016/j.nrl.2018.11.004
- Di Stefano V, Ornello R. Social distancing in chronic migraine during the COVID-19 Outbreak: results from a multicenter observational study. Nutrients. 2021;13:1361. doi:10.3390/nu13041361
- Currò CT, Ciacciarelli A, Vitale C, et al. Chronic migraine in the first COVID-19 lockdown: the impact of sleep, remote working, and other life/psychological changes. Neurol Sci. 2021;42:4403–4418. doi:10.1007/s10072-021-05521-7
- Gardani M, Bradford DRR, Russell K, et al. A systematic review and meta-analysis of poor sleep, insomnia symptoms and stress in undergraduate students. Sleep Med Rev. 2022;61:101565. doi:10.1016/j.smrv.2021.101565
- Scher AI, Midgette LA, Lipton RB. Risk factors for headache chronification. Headache. 2008;48:16–25. doi:10.1111/j.1526-4610.2007.00970.x
- Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi:10.1016/j.psychres.2020.112954
- Bertisch SM, Li W. Nightly sleep duration, fragmentation, and quality and daily risk of migraine. Neurology. 2020;94:e489–e496. doi:10.1212/WNL.0000000000008740
- Rains JC. Sleep and migraine: assessment and treatment of comorbid sleep disorders. Headache. 2018;58:1074–1091. doi:10.1111/head.13357
- Ødegård SS, Sand T, Engstrøm M, Zwart JA, Hagen K. The impact of headache and chronic musculoskeletal complaints on the risk of insomnia: longitudinal data from the Nord-Trøndelag health study. J Headache Pain. 2013;14:24. doi:10.1186/1129-2377-14-24
- Guieu R, Devaux C, Henry H, et al. Adenosine and migraine. Can J Neurol Sci. 1998;25:55–58.
- Lindquist BE, Shuttleworth CW. Adenosine receptor activation is responsible for prolonged depression of synaptic transmission after spreading depolarization in brain slices. Neuroscience. 2012;223:365–376. doi:10.1016/j.neuroscience.2012.07.053
- Lindquist BE, Shuttleworth CW. Evidence that adenosine contributes to Leao’s spreading depression in vivo. J Cereb Blood Flow Metab. 2017;37:1656–1669. doi:10.1177/0271678X16650696
- Stanyer EC, Creeney H, Nesbitt AD, Holland PR. Subjective sleep quality and sleep architecture in patients with migraine. A Meta-Analysis. 2021;97:e1620–e1631.
- Feng H, Wen SY, Qiao QC, et al. Orexin signaling modulates synchronized excitation in the sublaterodorsal tegmental nucleus to stabilize REM sleep. Nat Commun. 2020;11:3661. doi:10.1038/s41467-020-17401-3
- Villalón CM, Olesen J. The role of CGRP in the pathophysiology of migraine and efficacy of CGRP receptor antagonists as acute antimigraine drugs. Pharmacol Ther. 2009;124:309–323. doi:10.1016/j.pharmthera.2009.09.003
- Kunst M, Hughes ME, Raccuglia D, et al. Calcitonin gene-related peptide neurons mediate sleep-specific circadian output in Drosophila. Curr Biol. 2014;24:2652–2664. doi:10.1016/j.cub.2014.09.077
- Lőrincz ML, Adamantidis AR. Monoaminergic control of brain states and sensory processing: existing knowledge and recent insights obtained with optogenetics. Prog Neurobiol. 2017;151:237–253. doi:10.1016/j.pneurobio.2016.09.003
- Chen XY, Chen ZY, Dong Z, Liu MQ, Yu SY. Regional volume changes of the brain in migraine chronification. Neural Regenera Res. 2020;15:1701–1708. doi:10.4103/1673-5374.276360
- Younis S, Hougaard A, Noseda R, Ashina M. Current understanding of thalamic structure and function in migraine. Cephalalgia. 2019;39(13):1675–1682. doi:10.1177/0333102418791595
- Smelt AF, Louter MA, Kies DA, et al. What do patients consider to be the most important outcomes for effectiveness studies on migraine treatment? Results of a Delphi study. PLoS One. 2014;9:e98933. doi:10.1371/journal.pone.0098933
- De Icco R, Putortì A, De Paoli I, et al. Anodal transcranial direct current stimulation in chronic migraine and medication overuse headache: a pilot double-blind randomized sham-controlled trial. Clin Neurophysiol. 2021;132:126–136. doi:10.1016/j.clinph.2020.10.014
- Ulusoy EK, Bolattürk ÖF. The effect of greater occipital nerve blockade on the quality of life, disability and comorbid depression, anxiety, and sleep disturbance in patients with chronic migraine. Neurol Sci. 2020;41:1829–1835. doi:10.1007/s10072-020-04286-9
- Saçmacı H, Aktürk T, Tanık N, İnan LE. Clinical success of greater occipital nerve blockade in improving sleep quality of chronic migraineurs: a prospective observational study. Sleep Breath Schlaf Atmung. 2021;25:1003–1010. doi:10.1007/s11325-021-02309-z
- Smitherman TA, Walters AB, Davis RE, et al. Randomized controlled pilot trial of behavioral insomnia treatment for chronic migraine with comorbid insomnia. Headache. 2016;56:276–291. doi:10.1111/head.12760
- Crawford MR, Luik AI, Espie CA, et al. Digital cognitive behavioral therapy for insomnia in women with chronic migraines. J Headache Pain. 2020;60:902–915. doi:10.1111/head.13777
- Blumenfeld AM, Tepper SJ, Robbins LD, Manack Adams A, Buse DC, Orejudos A. Effects of onabotulinumtoxinA treatment for chronic migraine on common comorbidities including depression and anxiety. J Neurol Neurosurg Psychiatry. 2019;90:353–360. doi:10.1136/jnnp-2018-319290
- Aydinlar EI, Dikmen PY, Kosak S, Kocaman AS. OnabotulinumtoxinA effectiveness on chronic migraine, negative emotional states and sleep quality: a single-center prospective cohort study. J Headache Pain. 2017;18:23. doi:10.1186/s10194-017-0723-4
- Loeb LM, Amorim RP, Mazzacoratti M, Scorza FA, Peres MFP. Botulinum toxin A (BT-A) versus low-level laser therapy (LLLT) in chronic migraine treatment: a comparison. Arq Neuropsiquiatr. 2018;76:663–667. doi:10.1590/0004-282x20180109
- Barad M, Sturgeon JA, Fish S, Dexter F, Mackey S, Flood PD. Response to BotulinumtoxinA in a migraine cohort with multiple comorbidities and widespread pain. Reg Anesth Pain Med. 2019;44:660–668. doi:10.1136/rapm-2018-100196
- Cernuda-Morollón E, Ramón C, Martínez-Camblor P, Serrano-Pertierra E, Larrosa D, Pascual J. OnabotulinumtoxinA decreases interictal CGRP plasma levels in patients with chronic migraine. Pain. 2015;156:820–824. doi:10.1097/j.pain.0000000000000119
- Rodrigo D, Acin P, Bermejo P. Occipital nerve stimulation for refractory chronic migraine: results of a long-term prospective study. Pain Physician. 2017;20:E151–E159. doi:10.36076/2017.1.E151
- Kinfe TM, Pintea B, Muhammad S, et al. Cervical non-invasive vagus nerve stimulation (nVNS) for preventive and acute treatment of episodic and chronic migraine and migraine-associated sleep disturbance: a prospective observational cohort study. J Headache Pain. 2015;16:101. doi:10.1186/s10194-015-0582-9
- Peres MF, Mercante JP, Tanuri FC, Nunes M, Zukerman E. Chronic migraine prevention with topiramate. J Headache Pain. 2006;7:185–187. doi:10.1007/s10194-006-0339-6
- Saper JR, Lake AE, Tepper SJ. Nefazodone for chronic daily headache prophylaxis: an open-label study. Headache. 2001;41:465–474. doi:10.1046/j.1526-4610.2001.01084.x
- Russo A, Silvestro M, Scotto Di Clemente F, et al. Multidimensional assessment of the effects of erenumab in chronic migraine patients with previous unsuccessful preventive treatments: a comprehensive real-world experience. J Headache Pain. 2020;21:69. doi:10.1186/s10194-020-01143-0
- Tiseo C, Vacca A, Felbush A, et al. Migraine and sleep disorders: a systematic review. J Headache Pain. 2020;21:126. doi:10.1186/s10194-020-01192-5