Abstract
Women in developing countries are at high risk of HIV, sexually transmitted infections, and unplanned pregnancy. The female condom (FC) is an effective dual protective method regarded as a tool for woman’s empowerment, yet supply and uptake are limited. Numerous individual, socioeconomic, and cultural factors influence uptake of new contraceptive methods. We reviewed studies of FC knowledge, attitudes, practices, and behaviors across developing countries, as well as available country-level survey data, in order to identify overarching trends and themes. High acceptability was documented in studies conducted in diverse settings among male and female FC users, with FCs frequently compared favorably to male condoms. Furthermore, FC introduction has been shown to increase the proportion of “protected” sex acts in study populations, by offering couples additional choice. However, available national survey data showed low uptake with no strong association with method awareness, as well as inconsistent patterns of use between countries. We identified a large number of method attributes and contextual factors influencing FC use/nonuse, most of which were perceived both positively and negatively by different groups and between settings. Male partner objection was the most pervasive factor preventing initial and continued use. Importantly, most problems could be overcome with practice and adequate support. These findings demonstrate the importance of accounting for contextual factors impacting demand in FC programming at a local level. Ongoing access to counseling for initial FC users and adopters is likely to play a critical role in successful introduction.
Introduction
Women carry a disproportionate burden of HIVCitation1 resulting from numerous physiological, socioeconomic, cultural, and political factors, including unbalanced gender norms impacting sexual negotiation.Citation2–Citation7 Furthermore, over one-third of pregnancies in developing countries is unplanned,Citation8 making unmet need for contraception a priority policy area.Citation9
The female condom (FC) is the only available woman-initiated method for preventing HIV/sexually transmitted infections (STIs) and unintended pregnancy.Citation10 It has comparable dual protective efficacy to male condoms (MCs)Citation11 and is frequently cited as a tool for women’s empowerment.Citation12–Citation14 There are several FC models including FC2, The Woman’s Condom, The Phoenurse, Cupid, Panty (Condon Femenino), Velvet, and VA w.o.w (Condom Feminine); all have common components with unique design features.Citation15 Although the Female Health Company’s FC2 (Chicago, IL, USA) is the only current model approved by the United States Food and Drug Administration (USFDA), Cupid has been prequalified for distribution by United Nations (UN) agenciesCitation16 and others have commenced or are planning UN and USFDA applications.Citation15
Over 20 years since its first USFDA approval, FC supply and uptake remains inadequate.Citation17 Few established national programs exist,Citation18–Citation20 with low distributionCitation21 often attributed to a lack of policy and donor supportCitation11,Citation17,Citation22 and relatively high procurement costs compared to MCs,Citation11,Citation23 despite long-term cost effectiveness.Citation14,Citation24,Citation25 As FC options increase, the method may become more affordable, encouraging greater distribution and use.Citation15
Increasing availability of new contraceptive methods does not automatically broaden choice. Uptake depends on the perceptions and experiences of potential users and the socioeconomic context,Citation23,Citation26 with culture and gender relations often having greater impact on acceptability than actual attributes of the method.Citation13,Citation27 Health system capacity and acceptance of new methods by service providers additionally influence uptake and sustained use.Citation26,Citation28 Any FC program evaluation must therefore consider acceptability in context, by exploring knowledge, attitudes, practices, and behaviors (KAPB) in a wide range of stakeholders. We conducted a scoping reviewCitation29 of FC KAPB across developing countries to identify overarching themes linking contextual variables with these outcomes.
Methods
The format of our review was a scoping study. The purpose of a scoping review is to map a wide range of literature and to identify the nature, range, and extent of the evidence.Citation29,Citation30 Scoping reviews differ from systematic reviews in their broad approach to a topic, purposive sampling frame, and identification of gaps in the literature. We searched MEDLINE without date restrictions for material available through January 2015, using the terms “female condom” or “female-initiated”, to identify KAPB studies for male and female users and nonusers. We also searched for studies exploring perspectives of other stakeholders such as health care providers, although this information falls beyond the scope of this article. Countries in which research was identified are listed in . Titles or abstracts (where a decision could not be made on title alone) were screened for studies that discussed FC KAPB in developing nations. We included English-, French-, and Spanish-language articles. We also searched the Websites of major international organizations involved in FC programming and the survey database of the Reproductive Health Supplies CoalitionCitation31 using the same inclusion criteria. We reviewed a compiled list of research studies at the Female Health Company Website (http://www.femalecondom.org/).Citation32 All reference lists were reviewed; where potentially relevant additional material was unavailable online, we contacted authors or publishers to obtain a copy where possible. All sources were organized by country, and data were extracted onto standardized data abstraction forms that stratified KAPB variables by distinct user subpopulations. Data were then examined across countries to identify emerging themes and trends. The purpose of a scoping review is to map a wide range of literature and to identify the nature and extent of the evidence;Citation29 thus, for each country, research articles for which there were available data on potential or actual users or providers were then selected for inclusion in this review.
Table 1 Availability of female condom research by participant type and country
Results
We identified 56 countries with national survey data (usually as Demographic and Health Surveys [DHS])Citation33–Citation41 and 34 countries with other types of material (peer-reviewed articles, governmental or nongovernmental organizational reports, or other gray literature). The frequency of articles and the depth of information varied considerably across countries. shows the type of participants included in the FC studies, by country. Most research focused on women, particularly female sex workers (FSWs). Notably, only three studiesCitation42–Citation44 included men who have sex with men (MSM) (none addressed FC use by women for anal sex); we therefore include these data alongside those for female users, while perspectives of heterosexual male partners are considered separately. Sample sizes for quantitative reports ranged to 2,700, although most contained a few hundred participants. Qualitative reports tended to be smaller, though most sample sizes exceeded 100. “maps” the number and variety of peer-reviewed research compared with coverage by national survey data, organized by country and continent. Most countries listed provided DHS or other country-level survey data, but peer-reviewed data were considerably less frequent. The majority of peer-reviewed research emanated from Africa, where both qualitative and quantitative studies were available for several countries. By contrast, countries in the Americas were less well represented by quantitative studies. Single countries having the greatest number of peer-reviewed articles were South Africa (18 articles), the People’s Republic of China (nine articles), and Zimbabwe (eight articles) (data not shown). Although most studies were conducted with the discontinued FC1, several demonstrated comparable acceptability between various brands.Citation45–Citation50 Reports on provider attitudes were limited; our search turned up only six peer-reviewed articles. We made reference to these findings where relevant and integrated with data from users.
Table 2 Comparison of national survey data and peer-reviewed research by type, country, and continent
Knowledge and awareness
National data on FC knowledge, primarily from DHS, were available for 56 countries. These demonstrated widely varying between-country awareness (). The prevalence of FC awareness within countries was consistently lower than that of MCs; for example in the Democratic Republic of the Congo, 43% and 82% of women had knowledge of FCs and MCs, respectively.Citation51 The proportion of women across all countries having heard of FC (FC knowledge) was also generally lower (47%) than for the oral contraceptive (OC) (85%), injectables (80%), and the intrauterine device (IUD) (55%) (data not shown).Citation33 In general, men demonstrated slightly higher FC awareness (54%) than women (47%), but they exhibited lower levels of knowledge on other methods, as compared with that of women: OC (76%); injectables (67%); or the IUD (38%) (data not shown).Citation33 FC knowledge also varied within countries (where available);Citation52 for example, in India, 13% of urban women reported awareness compared to 6% of rural women.Citation41 Some studies supported the contention that greater awareness of and counseling on FC would increase interest and possible use;Citation53,Citation54 nevertheless, it is clear that FC awareness alone appears to be insufficient to stimulate uptake.Citation55 For example 91.4% of women interviewed in the most recent Swaziland DHS had heard of FCs, yet only 46% knew where to source one.Citation56
Table 3 Prevalence of female condom awareness and useTable Footnotea by country (listed by prevalence of awareness) from national survey data
General perceptions and attitudes
High acceptability was documented across numerous and varied settings where studies were undertaken among women, men, and couples who tried the device.Citation45,Citation57–Citation59 For example, studies introducing FCs in South Africa and Kenya reported that over 85% of male and female participants expressed an intention to use FCs in the future, and even more would recommend them to friends.Citation60,Citation61 A large number of studies among FSWs suggest that FCs are consistently acceptable to this population;Citation62,Citation63 for example, in Papua New Guinea, 90% of female participants engaging in transactional sex reported “liking” the FC.Citation64 In India, 83% of MSM FC users said they would continue to use the device.Citation42
Numerous studies reported that FCs compared favorably with MCs. For example, 80% of women in a South African short-term crossover trial favored the FC1 and FC2 over MCs;Citation50 in a Nigerian study, many more participants accepted and paid for FCs than MCs (8% versus 1%, respectively) following a provider training intervention.Citation65 Women and MSM also gauged FC acceptability against the MC, based on previous negative experiences or perceived superior safety, strength, or effectiveness.Citation42,Citation43,Citation66 Advantages over the MC were frequently highlighted, such as comfort, lack of male responsibility, enhanced sexual pleasure, and potential use during menstruation.Citation67–Citation71 Contraceptive properties were highlighted in El Salvador, Swaziland, and Zimbabwe.Citation68–Citation70
Several studies did not distinguish between factors influencing initial uptake or continued use, but they reported overall responses. The same method attributes of FCs were perceived both positively and negatively by different groups and between settings (). Similarly, environmental/contextual factors both positively and negatively influenced uptake in different settings (). Although few studies commented on patterns of acceptability, several contradictory trends existed between countries based on marital status, education, and occupation,Citation55,Citation58,Citation72–Citation76 thus supporting the conclusion of a 2006 systematic review that predictors of acceptability are not generalizable across cultural contexts.Citation77
Table 4 Method attributes (actual and perceived) of FCs influencing acceptability, uptake and/or continued use
Table 5 Contextual/environmental factors influencing FC acceptability, uptake, and/or continued use (excluding availability)
Some studies reported that stigmatized notions of the FC impeded initial use and were widely expressed by men, women, and health care providers,Citation52,Citation54,Citation73,Citation78,Citation79 linking the device with infidelity and commercial sex work, even when marketed as a contraceptive for stable couples.Citation54,Citation61,Citation66,Citation68,Citation78–Citation81 For example, a quarter of female participants in a Kenyan study felt that using or carrying an FC was synonymous with unfaithfulness.Citation61 Researchers in Zimbabwe commented that “just like the male condom, the [FC] was seen as a threat to intimacy and commitment, in that requesting them would introduce an element of distrust and suspicion of infidelity and promiscuity”.Citation82
Cost was a frequently cited acceptability barrier. Although both clients and providers often indicated that the FC should be freely available,Citation83–Citation86 most conceded that they would be willing to pay a highly subsidized price,Citation67,Citation87–Citation90 usually equal to that of MCs.Citation66,Citation91,Citation92 FSWs in Malawi noted that free FCs were only available in hospitals.Citation84 By contrast, in Cameroon, where intensive FC availability campaigns and a massive decrease in price has recently occurred, a relatively high ever-use rate among female high school students (8%) suggests that price significantly influences acceptability.Citation93
Lack of availability and access were the most frequently cited contributing factors to FC non-use, discontinuation and reuse, across diverse subpopulations, including students, FSWs and women in the general population. For example, 43% of Rwandan undergraduates agreed that they would use FC if available;Citation54 and only one-quarter of Chinese family planning clients thought that FC was easy to obtain.Citation95 Furthermore, lack of access or availability were frequently cited by healthcare providers as a reason not to counsel clients on FC use. 22% of Zimbabwean health care workers indicated they would offer FCs more frequently if availability was improved (note that the terms availability and access were used variously by different authors with a great degree of overlap in meaning; we have adhered to the original study terms where possible).Citation94
Initial use
FC acceptance in a trial setting varied. In a large Brazilian study, 90% of participants initially introduced to the device had used the FC at least once at the 90-day follow-up visit (hereafter, referred to as follow-up);Citation58 whereas in a Kenyan study, less than half of the participants recruited through HIV counseling and testing centers were willing to use the FC.Citation61 The most common reason for never-use was the fear of partner reaction or partner refusal.Citation60,Citation61,Citation78,Citation96 AppearanceCitation59,Citation61,Citation81,Citation92 and lack of perceived needCitation61 were also cited as initial barriers.
Triggers for initial FC use included novelty,Citation43,Citation61,Citation67,Citation71,Citation96 dual protective properties, partners’ or clients’ unwillingness to use MCs,Citation42,Citation67,Citation92 and the feeling that it was woman-initiated.Citation43,Citation61,Citation67,Citation97 Promotion and support were frequently-reported facilitators of initial use.Citation22,Citation53,Citation71,Citation81,Citation88,Citation98–Citation100 For example, counselor training and peer support groups in Kenya helped women introduce the FC into sexual relationships.Citation98,Citation101 In Zimbabwe, having observed an FC demonstration in a hair salon more than doubled a woman’s likelihood of having tried the device.Citation22 In Tanzania, a mass media campaign, which triggered communication about the FC between partners, increased women’s intention to use the device.Citation99
Continued use
A large number of studies reported that continued use was strongly influenced by experiences during the adoption phase. These included reservations regarding appearance, insertion or removal difficulties, discomfort caused by the inner or outer ring, noise, technical difficulties during sex, and partner resistance.Citation60,Citation66,Citation71,Citation92,Citation96,Citation102–Citation106 However, study data indicated that most users overcome initial difficulties with practice, resulting in high acceptabilityCitation62,Citation70,Citation81,Citation102,Citation107,Citation108 and few clinical failures.Citation63,Citation90,Citation95,Citation107,Citation109 For example, FSWs in El Salvador reported using FCs independently in up to ten sexual acts before they formed an opinion of the device and felt skilled enough to use it with a partner. Consequently, these women recommended that providers offer in-depth training to potential users who are new to the FCs.Citation92
Continued use was commonly associated with adequate support during the adoption phase, through counseling or peer education, in studies following women and couples for 2–20 months.Citation62,Citation88,Citation102,Citation107,Citation110 For example, in the People’s Republic of China, education and demonstration sessions significantly increased FSWs’ knowledge and acceptance of FCs, and confidence that clients would accept its use.Citation62,Citation75 Brazilian women reported benefiting from FC demonstration, negotiation tips, hearing testimonials from others, and discussing initial difficulties:
The meetings were good because she explained many things, I could rehearse again how to insert it correctly in a model resembling the vagina, I also talked about how to introduce it to the partner.Citation102
In the same Brazilian study, other important factors influencing continued use were perceived safety (compared with MCs), pleasure (stimulation from external ring), and increased sense of power for safer sex negotiation.Citation102
Conversely, some studies found that women were more likely to report inconsistent use or discontinuation when their initial difficulties were not overcome. Inconsistent use was most commonly attributed to partner objection – as cited by 30% of Kenyan women at 12-month follow-upCitation111 and by FSWs in Zimbabwe, who reported that their clients distrusted unfamiliar methods.Citation63 Other common reasons for discontinuation were lack of perceived need for a barrier method, often due to belief in a mutually faithful partnership,Citation111 or desire for unprotected sex with a loved one.Citation48
Several studies found that discontinuation was frequently attributed to partner resistance, objection, or dislike of the device.Citation60,Citation66,Citation112,Citation113 Method attributes influencing discontinuation included unattractive appearance, noise, reduced sensation, size, overlubrication, difficulty inserting, and discomfort from the internal ring.Citation58,Citation60,Citation66,Citation84,Citation105,Citation113,Citation114
Patterns of use
National survey data () supported a handful of cross-sectional studiesCitation52,Citation54,Citation66,Citation115 that demonstrated low ever or current use in the general population. FC use among FSWs was more common,Citation64,Citation67,Citation85,Citation116,Citation117 with ever-use prevalence ranging from 5% in MalawiCitation104 to 33% in Swaziland.Citation117
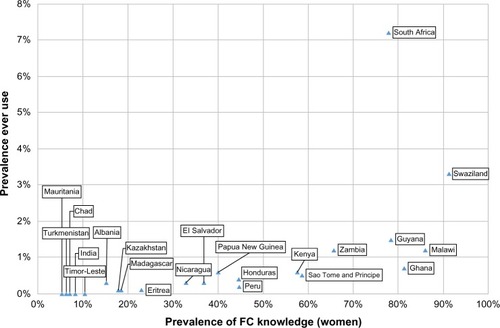
Notably, trends in uptake based on demographic variables were inconsistent between countries, and no strong association was apparent between awareness and ever use for 22 countries where both national datasets were available (), although no formal statistical tests of associations were undertaken. An analysis of South African national survey data identified significant associations only with older age and living in a particular province. Interestingly, many variables were associated with high knowledge prevalence but low use, or vice versa.Citation55
Figure 1 Scatterplot showing the prevalence of FC knowledge in women and ever use for countries where national survey data were available.
Dual protection was a commonly cited advantage in a number of settings. For example, general population women in South Africa and Ghana usually cited STI/HIV prevention;Citation66,Citation88 Ugandan HIV-positive women cited prevention of partner transmission;Citation118 and Swazi FSWs cited prevention of STIs, unintended pregnancy, and HIV reinfection.Citation70 However, the most common partner type with whom FC use was reported varied between settings. For example, in Kenya, South Africa, and Zimbabwe, use was more common with a spouse/regular partner than a casual/commercial partner,Citation61,Citation69,Citation88 whereas in Uganda, use was more common in high-risk sexual relationships.Citation48 FSWs in Brazil and El Salvador reported using FCs more often with regular clients than with new/occasional clients or boyfriends.Citation67,Citation68 Conversely, despite both sexes generally perceiving dual protection as an advantage, women in Swaziland, Zimbabwe, Cote d’Ivoire, and India reported discomfort discussing disease prevention with long-term partners.Citation69,Citation70,Citation119,Citation120
Consistency of use and impact on protected sex
The prevalence of consistent FC use varied between studies, but it was often low. For instance, in Kenya, 11% of women enrolled in an FC acceptability trial reported consistent use at 6-month follow-up.Citation111 Conversely, consistent use in a general population sample ranged as high as 25%, as shown in a recent cross-sectional study in a Zimbabwean hospital.Citation121 Most evidence, however, suggested that couples interchange MC and FC use to maintain or increase the proportion of protected sex acts.Citation69,Citation70,Citation88,Citation122 In Zimbabwe, factors influencing method choice included availability, partner preference, and the woman’s menstrual cycle. Women were more likely to use FCs consistently if they did not experience technical difficulties or partner opposition, did not rely on other contraceptive methods, and used FCs for contraception.Citation69 Another Zimbabwean study showed that factors influencing consistent use depended on partner type: consistent use between spouses was negatively associated with multiple partner behaviors, but for regular nonmarital partners, it was positively associated with perceived ease of use and effectiveness for STI prevention.Citation123
A 2006 systematic reviewCitation77 and three further studies in Mexico, Kenya, and MadagascarCitation85,Citation122,Citation124 concluded that FC provision can increase consistent condom use in a population, supporting other evidence that expanded choice improves contraceptive uptake and health outcomes.Citation18,Citation19 The addition of free FC provision into an existing peer education program among FSWs in Kenya increased consistent MC or FC use from 60% to 67%.Citation124
Covert use
Despite being a commonly perceived advantage, studies that investigated actual covert FC use suggest that this practice is not widespread. Evidence from Brazil, South Africa, India, and Uganda suggested that only a minority of women practice covert use,Citation43,Citation60,Citation67,Citation125 although this may be higher for FSWs.Citation126,Citation127 In South Africa, reduced partner awareness, often when partners were drunk or high, was more important to women than absolute covert use.Citation80 Covert use may facilitate higher sex work earnings from clients willing to pay more for sex without a condom,Citation68 whilst increasing a woman’s chance of protection:
[I]f you have the female condom, you can go to the bath-room and put it in and the client thinks they are not using a condom. But because you are wearing it, there is no risk that he can give you an infection (FSW, El Salvador).Citation68
Reuse
Research in Zimbabwe, Uganda, Zambia, Mexico, Bangladesh, and Swaziland suggested that a minority of women reuse FCs.Citation48,Citation70,Citation85,Citation86,Citation89,Citation128 In India, 11% of MSM users reported reuse of a single FC with multiple clients.Citation42 In South Africa, among 150 family planning clients and women at high risk for STIs, 83% reported willingness to reuse the FC, and those who trialed reuse up to seven times reported that the recommended steps involved were easy to perform and acceptable.Citation91 In Swaziland, FSWs reported reuse without removal or washing, citing reasons of limited availability and lack of privacy needed for disposal and reinsertion.Citation70
Heterosexual male partners
Studies involving heterosexual men were identified in 15 countries (); participants included single men, FSW clients, regular or cohabiting partners, and husbands. Men in several countries in Africa, Asia, and South America welcomed the device.Citation45,Citation59,Citation87,Citation102,Citation115,Citation129 For example, over 80% of men participating in an acceptability trial in India reported willingness to buy both the FC2 and Reddy FC in the future.Citation45 Men frequently perceived superior effectiveness of the FC over the MC for HIV/STIs/pregnancy prevention and valued its dual protective properties.Citation45,Citation89,Citation115,Citation118,Citation130 High levels of comfort and sensation were also reported, especially with practice, resulting from loose fit and lubrication.Citation48,Citation89,Citation131 Men in Nigeria and Uganda liked the potential to insert before sex, and not having to remove the FC immediately after sex.Citation48,Citation89 Men in Brazil, South Africa, and China recognized the advantages of a female-initiated method,Citation59,Citation87,Citation102,Citation115 namely because it reduced male responsibility and increased female sexual agency: “Women can decide independently whether they would choose contraception or not. This is its greatest strength” (College educated young man, Shanghai).Citation87
Conversely, several studies identified major concerns from men.Citation48,Citation59,Citation79,Citation82,Citation130,Citation132,Citation133 Ugandan men complained that the FC was more difficult to use than the MC,Citation48 while South African male students cited appearance, unfamiliarity, and concerns about pleasure as barriers to initial use, but felt that these might improve with experience.Citation115 In another South African study, male students with prior use of the FC reported discomfort with their partners’ suggestion of FC use, as well as female partners’ insertion prior to negotiation.Citation59 Other studies found that men felt threatened by a woman taking control of her own sexuality and were concerned that the FC might encourage promiscuity if women no longer feel at risk.Citation82,Citation130,Citation132,Citation133 Ugandan and Indian men feared that women would reuse FC without adequate cleaning.Citation45,Citation118
Negative attitudes were sometimes fuelled by misconceptions: men in Cameroon, Nigeria, and Zimbabwe reported a refusal to use FCs with FSWs for fear of multiple use or “sperm harvesting” for black magic.Citation133 Some men in South Africa believed that they might not be protected by a device that is not worn by a man.Citation115
Some studies found that women often reported positive responses from male partners, despite initial objection.Citation63,Citation88,Citation102,Citation134 For example, while some women in Zimbabwe reported partner refusal for fear of women becoming “casual about sex”, most said they were encouraged to get more FCs.Citation108 In South Africa, over 80% of women reported partner approval, based on natural feel, sexual pleasure, size, and strength. Conversely, attributes perceived as “disliked” were overlubrication and large size.Citation50 Notably, these responses were mainly reported by women who had successfully negotiated FC use.
Women’s empowerment and negotiating use
The relationship between FC and women’s empowerment was frequently commented on, yet inconsistently interpreted by study authors. A few studies noted that by catalyzing processes that challenge established gender norms, FCs had the potential to transform gender relations. For example, university students in Nigeria reported that a key reason for FC use was the sense of empowerment that the method afforded.Citation97 FC provision in Cambodia reinforced FSWs’ intentions to share experiences and support each other to adopt new methods.Citation127 In Mozambique, nearly 5,000 women have met in FC “empowerment groups” to discuss negotiation tactics with partners and the correct use of FCs, including basic education about women’s bodies.Citation135 Conversely, most authors characterized the FC as a protective tool for use within the existing constraints of gendered power imbalances, usually whereby women were empowered to protect themselves with the FC when their partner refused MC use.Citation43,Citation50,Citation67,Citation68,Citation105,Citation112,Citation126,Citation128 Commentaries were similarly mixed on the question of whether the FC truly “empowers”, or whether it can only be used by already “empowered” women.Citation12–Citation14,Citation125 In Tunisia, the authors of a study on FSWs commented that FC acceptance would be slow due to women’s highly proscribed gender roles and the fact that “customs imposed a real obstacle to social innovations”.Citation103 A number of other studies found that FCs were of limited value to women, who were only able to use them with full partner awareness and agreement.Citation82,Citation125,Citation136 Indeed, in one Zimbabwean study, two-thirds of women said that FC use depended on partner permission.Citation82 Nonetheless, studies conducted in over half the countries found that the FC’s female-initiated nature was perceived as a major advantage. In Zimbabwe, 35.6% of female inconsistent condom users said they could use FCs more consistently than MCs, simply because they did not have to rely on the man to wear it.Citation79,Citation137 In Vietnam, women said that the FC offered more control over unwanted pregnancy, even if desired by their husbands, and it provided sexual security if they doubted their husbands’ fidelity.Citation81 Women in several settings preferred the FC to the MC because they could guarantee that it had not been deliberately damaged by men.Citation70,Citation126 FSWs often valued the potential for FC use with drunk clients,Citation43,Citation68,Citation127,Citation138 and some women saw benefit in inserting the FC before drinking themselves: “When I am going to date, and know I am going to drink, then I put the female condom before, because I think it is more safe, because I know that if I drink I can forget to put it on” (28-year-old drug user, Brazil).Citation102
The FC is also used as a bargaining tool to negotiate either MC or FC use.Citation127,Citation128,Citation138 For example, following an FC intervention in Thailand, 60% of FSWs reported that more clients agreed to use an MC after learning that the only alternative was the FC.Citation138 Other gender dynamics reported include men’s involvement in FC use; for example, one South African study found that 45% of women reported partner assistance with FC insertion, stabilizing the device, or removal. In this study, male involvement was most commonly reported by students and least commonly by FSWs.Citation139
Discussion and conclusion
FCs can be highly acceptable to women and men with diverse risk profiles across a variety of settings, and as a female-initiated method, the device can be used as an additional tool to protect women within the context of gendered power imbalances. Furthermore, FCs are often used interchangeably with MCs, and thus their provision can positively impact the proportion of protected sex acts in a population, through uptake by women or couples for whom other methods of contraception or HIV prevention are inaccessible. The fact that most FC users employ the method interchangeably with the MC means that consistent FC use is less important than its role in increasing consistent condom use overall. Despite clear advantages at both an individual and population level, the national prevalence of FC use remains extremely low, even in the context of high awareness; these data suggest that models of successful programming are still not being implemented on a sufficiently wide scale. Current FC use was less than 1% (average: 0.04%) for all countries, compared with current use of the IUD, pill, and injectables, which averaged between 2%–6%, ranging up to 30% for the IUD (data not shown).Citation33,Citation35,Citation36,Citation41 Ever use of FC was also less than 1% for most countries – notable exceptions were South Africa (7.2%), Swaziland (3.3%), Guyana (1.5%), Malawi (1.2%), and Zambia (1.2%) – compared with ever use of the IUD, pill, and injectables, which averaged between 9%–21%, ranging up to nearly 50% for the IUD (data not shown) ().Citation33,Citation36,Citation41
Several important conclusions can be drawn from our data. Since the same method attributes are perceived positively and negatively within and between localities, contextual and environmental factors arguably play a greater role in determining overall FC acceptability and uptake. This is evidenced by the pervasive influence of stigma and male partner responses in determining initial and continued use of FCs. Indeed, even its female-initiated nature may limit acceptability if men fear loss of control. The fact that most of the physical and contextual factors negatively influencing use can be overcome with practice and adequate support suggests that demand creation is at least as important a component of programming as adequate supply.
Currently, since most research has focused on FC acceptability in trial settings, little is known about the profile of FC users and nonusers within the general population, and systems and market research to identify effective promotion and distribution mechanisms at a local level (ie, lower than national) is lacking. The scarcity of studies addressing FC use for anal sex by heterosexual couples and MSM in developing countries is an additional research gap, which perhaps reflects sociocultural taboo, as well as a general lack of attention to male perspectives on FC use. Policymakers, international donors, civil society groups, and programmers therefore have a responsibility not only to increase FC availability and advocate the sexual rights of women, but also to identify and implement local evidence-based strategies for effective FC programming.
There was near-universal endorsement, across the studies and population groups reviewed here, that increasing availability and access will contribute to increased FC use and limit reuse, although reuse levels were found to be low (current World Health Organization guidelines advise that a new FC should be used with every sexual act; Family Planning Global Handbook, 2011).Citation141 Integrating FCs into a wide variety of services, programs, and nontraditional settings will inevitably improve access, but it may also increase exposure and normalize the device, thus contributing to the narrowing of the observed gap between awareness and use. Adequate programmatic support must also be available to ensure implementation of strategies with proven efficacy, such as FC demonstration, negotiation skills counseling, and user support. Greater efforts are also required to target men in FC programming and advocacy, by using male-specific branding and addressing potential anxieties related to female-initiated methods. One example is the recent branding as “inner condoms” by the South Africa-based Population Services International affiliateCitation140 (see ). Promotional messaging should draw on local evidence to increase FC acceptability in the general population, by promoting commonly cited advantages such as sexual pleasure, while combating stigma and taboo.
Limitations
This review used peer-reviewed literature, country surveys, and other sources available via the Internet, and is thus subject to these limitations. Papers and reports outside our language scope would not be represented here. The fact that most research to date has been conducted with the discontinued FC1 suggests that some results may lack relevance to current programming. Our study was not intended to be a systematic review, and therefore did not include a complete count of articles retrieved and rejected. Scoping studies represent a broad approach to a topic, where the aim is to map a wide range of literature and identify the nature, range, and extent of the evidence. Some qualitative reports reviewed here were based on small sample sizes, although most were based on greater than 100 participants. Finally, the fact that our paper selected developing countries as a focus should not be construed to mean that the FC is not appropriate or acceptable for women in developed countries, as considerable literature has already shown.
Disclosure
The authors report no conflicts of interest in this work.
References
- Joint United Nations Programme on HIV/AIDS (UNAIDS)UNAIDS Report on the Global AIDS Epidemic 2013Geneva, SwitzerlandJoint United Nations Programme on HIV/AIDS (UNAIDS)2013
- DunkleKLJewkesRKBrownHCGrayGEMcIntyreJAHarlowSDGender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South AfricaLancet200436394191415142115121402
- JewkesRMorrellRGender and sexuality: emerging perspectives from the heterosexual epidemic in South Africa and implications for HIV risk and preventionJ Int AIDS Soc201013620181124
- AnderssonNCockcroftASheaBGender-based violence and HIV: relevance for HIV prevention in hyperendemic countries of southern AfricaAIDS200822Suppl 4S73S8619033757
- DunkleKLStephensonRKaritaENew heterosexually transmitted HIV infections in married or cohabiting couples in urban Zambia and Rwanda: an analysis of survey and clinical dataLancet200837196312183219118586173
- HirschJSMenesesSThompsonBNegroniMPelcastreBdel RioCThe inevitability of infidelity: sexual reputation, social geographies, and marital HIV risk in rural MexicoAm J Public Health200797698699617463368
- ClarkEarly marriage and HIV risks in sub-Saharan AfricaStudy Fam Plann2004353149160
- SedghGHussainRBankoleASinghSWomen with an Unmet Need for Contraception in Developing Countries and Their Reasons for Not Using a Method, Occasional Report No 37New York, NYGuttmacher Institute2007
- AlkemaLKantorovaVMenozziCBiddlecomANational, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: a systematic and comprehensive analysisLancet201338198781642165223489750
- GollubESteinZLiving with uncertainty: acting in the best interests of womenAIDS Res Treat2012201252493623193463
- GalloMFKilbourne-BrookMCoffeyPSA review of the effectiveness and acceptability of the female condom for dual protectionSex Health201291182622348629
- GollubELThe female condom: tool for women’s empowermentAm J Public Health20009091377138110983187
- MantellJESteinZASusserIWomen in the time of AIDS: barriers, bargains, and benefitsAIDS Educ Prev20082029110618433316
- PATH;UNFPAFemale Condo: A Powerful Tool for ProtectionSeattle, WAUNFPA and PATH2006
- BeksinskaMSmitJJoanisCPotterWNew female condoms in the pipelineReprod Health Matters2012204018819623245425
- United Nations Population FundUNFPA Prequalified Female Condom Manufacturing SitesNew York, NYUnited Nations Population Fund2013
- PetersAJansenWvan DrielFThe female condom: the international denial of a strong potentialReprod Health Matters2010183511912820541090
- WarrenMPhilpottAExpanding safer sex options: introducing the female condom into national programmesReprod Health Matters2003112113013912800710
- MarseilleEKahnJGSmarter Programming of the Female Condom: Increasing Its Impact on HIV Prevention in the Developing WorldSan Francisco, CAFSG Social Impact Advisors2008
- United Nations Population FundDonor Support for Contraceptives and Condoms for Family Planning and STI/HIV Prevention 2010New York, NYUNFPA2010
- United States Agency for International DevelopmentIs There a Condom Gap In 2010?Washington, DCUSAID2010
- Center for Health and Gender EquitySaving Lives Now: Female Condoms and the Role of US Foreign AidTakoma Park, MDCenter for Health and Gender Equity2008
- HoffmanSMantellJExnerTSteinZThe future of the female condomInt Fam Plan Perspect200430313914515381469
- DowdyDWSweatMDHoltgraveDRCountry-wide distribution of the nitrile female condom (FC2) in Brazil and South Africa: a cost-effectiveness analysisAIDS200620162091209817053355
- MarseilleEKahnJGBillinghurstKSabaJCost-effectiveness of the female condom in preventing HIV and STDs in commercial sex workers in rural South AfricaSoc Sci Med200152113514811144911
- World Health OrganizationMaking Decisions about Contraceptive Introduction: A Guide for Conducting Assessments to Broaden Contraceptive Choice and Improve Quality of CareGeneva, SwitzerlandWorld Health Organization2002
- MinnisAMShiboskiSCPadianNSBarrier contraceptive method acceptability and choice are not reliable indicators of useSex Transm Dis200330755656112838083
- MantellJEScheepersEKarimQAIntroducing the female condom through the public health sector: experiences from South AfricaAIDS Care200012558960111218545
- LevacDColquhounHO’BrienKKScoping studies: advancing the methodologyImplement Sci201056920854677
- ArskeyHO’MalleyLScoping studies: towards a methodological frameworkInt J Soc Res Methodol2005811932
- Reproductive Health Supplies CoalitionSupplies Information DatabaseBrussels, BelgiumReproductive Health Supplies Coalition2014
- The Female Health CompanyFemale Condom Bibliography – Sorted by DateChicago, ILThe Female Health Company2013 Available from: http://www.femalecondom.org/wp-content/uploads/2013/07/Female_condom_bibliography_march_2013_date.pdfAccessed May 11, 2015
- InternationalICFThe DHS Program STATcompilerRockville, MDICF International2012
- Ministry of Health and Social ServicesNamibia Demographic and Health SurveyWindhoek, NamibiaMinistry of Health and Social Services2014
- Central Statistical Office; UNICEFSwaziland Multiple Indicator Cluster Survey 2010Mbabane, SwazilandCentral Statistical Office and UNICEF2011
- ShisanaORehleTSimbayiLCSouth African National HIV Prevalence, Incidence, Behaviour and Communication Survey 2008: A Turning Tide among Teenagers?Cape Town, South AfricaHSRC Press2008
- National Department of HealthSouth Africa Demographic and Health Survey 2003Pretoria, South AfricaNational Department of Health2003
- Centro de Estudios Sociales Y DemograficosRepública Dominicana Encuesta Demografica Y de Salud 2007Calverton, MDMacro International Inc.2008 Spanish
- National Statistical OfficePapua New Guinea Demographic and Health Survey 2006Port Moresby, Papua New GuineaNational Statistical Office2009
- National Population CommissionNigeria Demographic and Health Survey 2008Calverton, MDICF Macro2008
- Ministry of Health and Family WelfareIndia National Family Health Survey (NFHS-3) 2005–6Mumbai, IndiaInternational Institute for Population Sciences2007
- KokkuSBTuckerSPunyamSExploring dynamics around female condom use for anal sex among MSMSex Transm Infect201187A250
- Hindustan Latex Family Planning Promotion TrustFemale Condom: The Indian ExperienceLondon, UKThe Female Health Company2004
- ChenBZhangMYangDWangXZhengYAcceptability of female condom use in money boys compared with other men who have sex with men in Chengdu, China: a comparative studySex Health20118226226321592446
- SmitaJNeelamJRochelleDYComparative acceptability study of the Reality female condom and the version 4 of modified Reddy female condom in IndiaContraception200572536637116246664
- JoanisCBeksinskaMHartCTweedyKLindaJSmitJThree new female condoms: which do South-African women prefer?Contraception201183324825421310287
- BeksinskaMEPiaggioGSmitJAPerformance and safety of the second-generation female condom (FC2) versus the Woman’s, the VA worn-of-women, and the Cupid female condoms: a randomised controlled non-inferiority crossover trialLancet Glob Health201313e146e15225104263
- WanyenzeRKAtuyambeLKibirigeVThe new female condom (FC2) in Uganda: perceptions and experiences of users and their sexual partnersAfr J AIDS Res201110321922425859790
- HouLYQiuHYZhaoYZZengXSChengYMA crossover comparison of two types of female condomInt J Gynaecol Obstet2010108321421819939380
- SmitJBeksinskaMVijayakumarGMabudeZShort-term acceptability of the reality polyurethane female condom and a synthetic latex prototype: a randomized crossover trial among South African womenContraception200673439439816531174
- Ministère du Plan et Suivi de la Mise en oeuvre de la Révolution de la Modernité/Ministère de la Santé PubliqueEnquête Démographique et de Santé En République Démocratique Du Congo 2013–2014Rockville, MDICF International2014 French
- OladeindeBHOmoregieROnifadeAAOlleyMAnunibeJAOladeindeOBAwareness and use of female condoms among young Nigerian womenCentrepoint Journal2011172157163
- ÇalışkanDSakızlıgilBHOcaktanMEThe awareness and use of the female condom among women at low and high risk for sexually transmitted infections in Ankara, TurkeyDicle Medical Journal/Dicle Tip Dergisi20123919
- MbarushimanaVNtaganiraJKnowledge and attitude to female condom use among undergraduates of Kigali Health InstituteRwanda Journal of Health Sciences2013211625
- GuerraFMSimbayiLCPrevalence of knowledge and use of the female condom in South AfricaAIDS Behav201418114615823934341
- Central Statistical OfficeSwaziland Demographic and Health SurveyCalverton, MDMacro International Inc.2008
- XuJXLeeperMAWuYUser acceptability of a female condom (Reality) in ShanghaiAdv Contracept199814419319910075288
- BarbosaRMKalckmannSBerquóESteinZNotes on the female condom: experiences in BrazilInt J STD AIDS200718426126617517999
- MasvawureTBMantellJEMabudeZ“It’s a different condom, let’s see how it works”: young men’s reactions to and experiences of female condom use during an intervention trial in South AfricaJ Sex Res201451884185124053638
- BeksinskaMEReesVHMcIntyreJAWilkinsonDAcceptability of the female condom in different groups of women in South Africa – a multicentred study to inform the national female condom introductory strategyS Afr Med J200191867267811584783
- Liverpool VCT, Care, and Treatment, Population CouncilFemale-Initiated Prevention: Integrating Female Condoms into HIV Risk-Reduction Activities in KenyaNairobi, KenyaPopulation Council2009
- YiminCZhaohuiLXianmiWIntroductory study on female condom use among sex workers in ChinaContraception200266317918512384207
- RaySvan De WijgertJMasonPNdowaFMaposhereCConstraints faced by sex workers in use of female and male condoms for safer sex in urban ZimbabweJ Urban Health200178458159211796805
- United States Agency for International Development/Family Health InternationalBehaviors, Knowledge, Exposure to InterventionsPort Moresby, Papua New GuineaFHI Papua New Guinea2011
- AdeokunLMantellJEWeissEPromoting dual protection in family planning clinics in Ibadan NigeriaInt Fam Plan Perspect20022828795
- SkaerMEbinVIn Our Own Hands: SWAA-Ghana Champions the Female CondomNew York, NYPopulation Council2006
- GalvãoLWDiazJMobleySCabralFMarchiNFruetSAcceptability of the Female Condom After a Social Marketing Campaign in Campinas, BrazilWashington, DCPopulation Council2002
- MackNGreyTGAmsterdamAMattaCIWilliamsonNCentral American sex workers’ introduction of the female condom to different types of sexual partnersAIDS Educ Prev201022546648120973666
- KerriganDMobleySRutenbergNFisherAWeissEThe Female Condom: Dynamics of Use in Urban ZimbabweWashington, DCPopulation Council2000
- MathenjwaTMaharajP‘Female condoms give women greater control’: a qualitative assessment of the experiences of commercial sex workers in SwazilandEur J Contracept Reprod Health Care201217538339222839696
- EzireOOluigboOArchibongVIfeanyiOAnyantiJBarriers to repeated use of female condom among women and men of reproductive age in NigeriaJournal of AIDS and HIV Research201356206213
- RaschVYambesiFKipingiliRAcceptance and use of the female condom among women with incomplete abortion in rural TanzaniaContraception2007751667017161127
- AraZBegumNNwenekaCVAcceptability of female-controlled HIV/STI prevention options among professionals in Dhaka, BangladeshSouth East Asia Journal of Public Health2012214653
- AghaSIntention to use the female condom following a mass-marketing campaign in Lusaka, ZambiaAm J Public Health200191230731011211646
- LiaoSWeeksMRWangYInclusion of the female condom in a male condom-only intervention in the sex industry in China: a cross-sectional analysis of pre- and post-intervention surveys in three study sitesPublic Health2011125528329221513961
- WangYLiaoSJiangJWho are the preferential targets for intervention programs related to the female condom among sex workers in southern China?AIDS Educ Prev201325434936123837812
- VijayakumarGMabudeZSmitJBeksinskaMLurieMA review of female-condom effectiveness: patterns of use and impact on protected sex acts and STI incidenceInt J STD AIDS2006171065265917059633
- MunyanaMPromoting the female condom in BurundiExchange on HIV/AIDS, Sexuality and Gender200621213
- BuckJKangMSvan der StratenAKhumalo-SakutukwaGPosnerSPadianNBarrier method preferences and perceptions among Zimbabwean women and their partnersAIDS Behav20059441542216254738
- MacPhailCTerris-PrestholtFKumaranayakeLNgoakoPWattsCReesHManaging men: women’s dilemmas about overt and covert use of barrier methods for HIV preventionCult Health Sex200911548549719479490
- United Nations Population FundThe Acceptability of Female Condoms among Migrant Workers in Industrial Zones in Viet NamHa Noi, Viet NamUnited Nations Population Fund2012
- Francis-ChizororoMNatshalagaNRThe female condom: acceptability and perception among rural women in ZimbabweAfr J Reprod Health20037310111615055153
- SusserISteinZCulture, sexuality, and women’s agency in the prevention of HIV/AIDS in southern AfricaAm J Public Health20009071042104810897180
- UNAIDSSTI/HIV/AIDS Prevention CenterWorld Health OrganizationNeeds and Acceptability of Female Condoms among Women in Thanh Xuan Commune and Dong Da District, HanoiHanoi, VietnamUNAIDS, STI/HIV/AIDS Prevention Center, and WHO2000
- StockmanJKMorrisMDMartinezGPrevalence and correlates of female condom use and interest among injection drug-using female sex workers in two Mexico-US border citiesAIDS Behav20121671877188622711225
- SmithJBNkhamaGTrottierDAFemale condom reuse in Lusaka, Zambia: evidence from 12 casesJ Urban Health200178463864611796810
- CoffeyPSKilbourne-BrookMJunqingWInitial reactions to the Woman’s Condom by potential user groups in Shanghai, ChinaJ Fam Plann Reprod Health Care201339211112022906855
- Reproductive Health Research Unit, Family Health International and the Department of Health of South AfricaIntroduction of the female condom in South Africa: programme activities and performance 1998–2000 Draft report in preparation
- National AIDS Coordination ProgrammePiloting the Female Condom in Zimbabwe: A National SurveyHarare, ZimbabweMinistry of Health and Child Welfare1998
- ZachariahRHarriesADBuhendwaLSpielmanMPChantuloABakaliEAcceptability and technical problems of the female condom amongst commercial sex workers in a rural district of MalawiTrop Doct200333422022414620427
- PettiforAEBeksinskaMEReesHVMqoqiNDickson-TettehKEThe acceptability of reuse of the female condom among urban South African womenJ Urban Health200178464765711796811
- MackNGreyTGAmsterdamAWilliamsonNMattaCIIntroducing female condoms to female sex workers in Central AmericaInt Perspect Sex Reprod Health201036314915520880800
- TarkangEEBainLEFactors that influence utilization of the female condom among senior secondary school female students in urban CameroonAmerican Journal of Health Research201424125133
- HoltKBlanchardKChipatoTA nationally representative survey of healthcare provider counselling and provision of the female condom in South Africa and ZimbabweBMJ Open201333 pii: e002208
- WangXXiMZhangLJiaLWangYChengYAwareness of female condoms and failures reported with two different types in ChinaInt J Gynaecol Obstet2015128215215625458411
- SéhonouJGrésenguetGTokunagaMMbopi KéouFXFavierCBélecLAcceptability of the female condom in Bangui, Central African Republic: results from a prospective studyInt J STD AIDS200213964965112243136
- Tobin-WestCIMadukaOOnyekwereVNTellaAOAwareness, acceptability, and use of female condoms among university students in Nigeria: implications for STI/HIV preventionInt J Adolesc Med Health201426225926524114893
- AnkrahEMAttikaSAAdopting the Female Condom in Kenya and Brazil: Perspectives of Women and Men. A SynthesisArlington, VAFamily Health International (FHI) and AIDS Control and Prevention Project (AIDSCAP)1997
- AghaSVan RossemRImpact of mass media campaigns on the intentions to use the female condom in TanzaniaInt Fam Plan Perspect2002283151158
- MantellJESmitJAExnerTMPromoting female condom use among female university students in KwaZulu-Natal, South Africa: results of a randomized behavioral trialAIDS Behav Epub852014
- Mung’alaLKilonzoNAngalaPTheobaldSTaegtmeyerMPromoting female condoms in HIV voluntary counselling and testing centres in KenyaReprod Health Matters200614289910317101427
- Telles DiasPRSoutoKPage-ShaferKLong-term female condom use among vulnerable populations in BrazilAIDS Behav2006104 SupplS67S7516799843
- BoudayaSMasmoudiAMeziouTJAcceptability of the female condom among prostitutes in TunisiaAnn Dermatol Venereol20061332185187 French16508611
- Family Planning Association in MalawiCounting the Uncatchables: A Report of the Situation Analysis of the M. Lagnitude, Behavioural Patterns, Contributing Factors, current Interventions and Impact of Sex Work in HIV Prevention in MalawiLilongwe, MalawiFamily Planning Association in Malawi and UNFPA2011
- NaiduMPerceptions around second generation female condoms reporting on women’s experiencesAnthropological Notebooks20131912534
- OkunlolaMAMorhason-BelloIOOwonikokoKMAdekunleAOFemale condom awareness, use and concerns among Nigerian female undergraduatesJ Obstet Gynaecol200626435335616753690
- GalvãoLWOliveiraLCDíazJEffectiveness of female and male condoms in preventing exposure to semen during vaginal intercourse: a randomized trialContraception200571213013615707563
- RaySBassettMMaposhereCAcceptability of the female condom in Zimbabwe: positive but male-centred responsesReprod Health Matters1995356879
- BeksinskaMSmitJGreenerRPiaggioGJoanisCThe female condom learning curve: patterns of female condom failure over 20 usesContraception2015911859025444717
- HokeTHFeldblumPJDammeKVRandomised controlled trial of alternative male and female condom promotion strategies targeting sex workers in MadagascarSex Transm Infect200783644845317591662
- FeldblumPJKuyohMABwayoJJFemale condom introduction and sexually transmitted infection prevalence: results of a community intervention trial in KenyaAIDS20011581037104411399986
- SakondhavatCWeeravatrakulYBenetteTConsumer preference study of the female condom in a sexually active population at risk of contracting AIDSJ Med Assoc Thai200184797398111759978
- IsahYOgunbowaleDAlagbileMAcceptability of female condom as a family planning method among women of reproductive ages in Adamawa State, North Eastern NigeriaInternational Conference on Family PlanningNovember 12–15, 2013Addis Ababa, Ethiopia
- SinpisutPChandeyingVSkovSUahgowitchaiCPerceptions and acceptability of the female condom [Femidom] amongst commercial sex workers in the Songkla province, ThailandInt J STD AIDS1998931681729530904
- MantellJESmitJABeksinskaMEverywhere you go, everyone is saying condom, condom. But are they being used consistently? Reflections of South African male students about male and female condom useHealth Educ Res201126585987121693684
- United States Agency for International Development/NamibiaHIV and AIDS and Treatment Literacy Namibia Survey 2008: Main ReportWindhoek, NamibiaUSAID/Namibia2009
- National Emergency Response Council on HIV and AIDS and United Nations Programme on HIV/AIDSSituation Analysis on Commercial Sex Work in SwazilandMbabane, SwazilandNERCHA and UNAIDS2007
- WanyenzeRKTumwesigyeNMKindyomundaRUptake of family planning methods and unplanned pregnancies among HIV-infected individuals: a cross-sectional survey among clients at HIV clinics in UgandaJ Int AIDS Soc2011143521718524
- UsmaniFThe Female Condom: Opportunities and Challenges in South AsiaKathmandu, NepalUNFPA Country Technical Services Team for South and West Asia2002
- DeniaudFDynamics of female condom acceptability among prostitutes and young women in Abidjan, Ivory CoastContracept Fertil Sex19972512921932 French9497605
- ChipfuwaTManwereAKuchengaMMLevel of awareness and uptake of the female condom in women aged 18 to 49 years in Bindura district, Mashonaland Central province, ZimbabweAfr J AIDS Res2014131758025174518
- HokeTHFeldblumPJVan DammeKTemporal trends in sexually transmitted infection prevalence and condom use following introduction of the female condom to Madagascar sex workersInt J STD AIDS200718746146617623503
- MeekersDRichterKFactors associated with use of the female condom in ZimbabweInt Fam Plan Perspect2005311303715888407
- ThomsenSCOmbidiWToroitich-RutoCA prospective study assessing the effects of introducing the female condom in a sex worker population in Mombasa, KenyaSex Transm Infect200682539740216854997
- GreenGPoolRHarrisonSFemale control of sexuality: illusion or reality? Use of vaginal products in south west UgandaSoc Sci Med200152458559811206655
- van DijkMGPinedaDLGrossmanDSorhaindoAGarcíaSGThe female condom: a promising but unavailable method for Dominican sex workers, their clients, and their partnersJ Assoc Nurses AIDS Care201324652152923465398
- BuszaJBakerSProtection and participation: an interactive programme introducing the female condom to migrant sex workers in CambodiaAIDS Care200416450751815203418
- SharifuzzamanMJanaSGomesJMEnamul HoqueASMMahmudKFFemale condom (FC) can lead safer sex when clients do not agree to use condomThe XIV International AIDS Conference2002 Abstract MoPeF4025
- BloggJBloggSAcceptability of the Female Condom (Femidom) Within a Population of Commercial Sex Workers and Couples in Salima Nkhotakota, MalawiLondon, UKThe Female Health Company1994
- PoolRHartGGreenGHarrisonSNyanziSWhitworthJMen’s attitudes to condoms and female controlled means to protect against HIV and STDs in south-western UgandaCult Health Sex20002219721112295882
- CoffeyPSKilbourne-BrookMAustinGSeamansYCohenJShort-term acceptability of the PATH Woman’s Condom among couples at three sitesContraception200673658859316730489
- MantellJEAdeokunLWeissEThe impact of male gender roles on HIV risk in southwest NigeriaThe 129th Annual Meeting of APHAAtlanta, GAAmerican Public Health Association2001
- KosterWBruinderinkMGKuijperCSiemerinkMCMale views on acceptability and use of female condoms with sex workers: findings from a qualitative study in Nigeria, Cameroon and ZimbabweThe 19th International AIDS ConferenceWashington, DCInternational AIDS Society2012 Abstract no THPE203
- SusserIAIDS, Sex and Culture: Global Politics and Survival in Southern AfricaChichester, UKWiley-Blackwell2009
- SimoneOVespiaM webpage on the InternetThe power of female condoms in MozambiqueWatertown, MAPathfinder International2013 Available from: http://www.pathfinder.org/blog/to-young-women-in-mozambique.html. Accessed
- HartGJPoolRGreenGHarrisonSNyanziSWhitworthJAWomen’s attitudes to condoms and female-controlled means of protection against HIV and STDs in south-western UgandaAIDS Care199911668769810716009
- NapieralaSKangMSChipatoTPadianNvan der StratenAFemale condom uptake and acceptability in ZimbabweAIDS Educ Prev200820212113418433318
- Jivasak-ApimasSSabaJChandeyingVAcceptability of the female condom among sex workers in Thailand: results from a prospective studySex Transm Dis2001281164865411677387
- BeksinskaMEReesHVKleinschmidtIMcIntyreJThe practice and prevalence of dry sex among men and women in South Africa: a risk factor for sexually transmitted infections?Sex Transm Infect199975317818010448396
- Population Services International (PSI) South AfricaLovers+ It’s PlaytimePSI
- World Health Organization Department of Reproductive Health and Research (WHO/RHR)Johns Hopkins Bloomberg School of Public Health/Center for Communication Programs (CCP) Knowledge for Health ProjectFamily Planning: A Global Handbook for Providers (2011 Update)Baltimore, MD and Geneva, SwitzerlandCCP and WHO2011