Abstract
Background
Even after achieving tremendous advances in diagnosis and treatment of rheumatoid arthritis (RA), many of the patients undergo delays in diagnosis and initiation of treatment, which leads to worsening of the condition and poor prognosis.
Objective
The objective of this study was to perform a literature review to quantify the lag times in diagnosis and treatment of RA and study the reported factors associated with it.
Methods
The authors searched literature published until September 2016 in electronic full-text and abstract databases and hand-searched the suitable articles.
Results
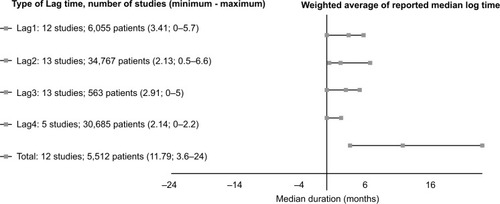
The weighted average of median lag time from symptom onset to therapy was 11.79 months (12 studies, 5,512 patients, range 3.6–24.0 months). Lag1 was 3.14 months (onset of symptoms to first physician consultant; 12 studies, 6,055 patients, range 0–5.7 months); lag2 was 2.13 months (physician visit to RA specialist referral; 13 studies, 34,767 patients, range 0.5–6.6 months); lag3 was 2.91 months (consultation with rheumatologist to diagnosis; 3 studies, 563 patients, range 0–5 months), lag4 was 2.14 months (diagnosis to initiation of disease-modifying antirheumatic drug therapy; 5 studies, 30,685 patients, range 0–2.2 months). Numerous patient-and physician-related factors like gender, ethnicity, primary care physician knowledge of the condition, availability of diagnostics, and so on were responsible for the delays.
Conclusion
This review estimated the delay times and identified the main factors for delay in RA patients in diagnosis and initiation of treatment. A most plausible solution to this is coordinated effort by the rheumatology and primary care physicians.
Introduction
Rheumatoid arthritis (RA) follows a chronic course and invariably involves significant long-term disability and morbidity.Citation1,Citation2 A diverse group of agents called disease-modifying antirheumatic drugs (DMARDs) and potent anti-inflammatory antibodies that block tumor necrosis factor are widely accepted, respectively, for slowing the progression of RA and alleviating the painful symptoms.Citation3,Citation4 Though clinically effective, these drugs become less effective in halting the long-term progression of RA if initiation of therapy is delayed.Citation5,Citation6 After onset of the symptoms, the disease progresses quickly leading to irreversible cartilage damage in <2 months.Citation7 This damage can only be prevented by the initiation of therapy within 2 months from the onset of symptoms.Citation7 Initial studies reported no such benefit;Citation8 however, carefully designed subsequent studies have established that patients in the earliest stages respond better to treatment compared to patients with long-established disease.Citation8,Citation9
With empirical evidence supporting early initiation of therapy in RA patients, it becomes necessary to minimize the lag time between the initiation of symptoms and therapy.Citation10 Unfortunately, the early stages of RA are characterized by nonspecific clinical signs that have been a frequent hurdle in timely initiation of the therapy.Citation11 A large study of 488 patients during 1950–1974 had shown that there was a median lag of 6 months between the onset of symptoms and diagnosis.Citation12 This has not improved even during the 1990s as 5 months lag between the onset of symptoms and diagnosis was very common.Citation13 Furthermore, some of the patients remain untreated for up to 10 years after the symptoms appear.Citation13
A recent study performed in Saudi Arabia found that patients consulted an average of 4 physicians between their first symptom of RA and final diagnosis, with a mean time from the first physician visit to final RA diagnosis of ~30 months.Citation14 Although patients consulted with physicians at a mean of 7 months after the onset of RA symptoms, very few subjects initially sought a consultation with rheumatologists, who were ultimately responsible for diagnosing most RA patients.
Like any other disease, the RA patient’s journey involves 3 distinct stages: onset of symptoms to consultation (lag1), consultation to rheumatology referral or definite RA diagnosis (lag2), and diagnosis to proper treatment (lag3). These lag times have been of interest to rheumatologists and have been reported by numerous studiesCitation15,Citation16 with some studies focusing specifically on the factors that contribute to these delays and measures undertaken to overcome these.
In this review, we examined the literature to study the lag times in RA patients with an aim to summarize the findings for future reference. Further analysis of factors was also undertaken to understand the reasons for these lags.
Methods
The primary objective of this study was to review the reported delay in the duration (lag time) between symptom onset and initial physician visit, an initial visit to rheumatology referral, referral to diagnosis and diagnosis to proper treatment.
Secondary objectives are to review the significance of reported factors that may have contributed to delayed RA diagnosis, and the possible measures that could be taken to accelerate RA diagnosis and early initiation of treatment.
A systematic search of OVID and PubMed databases was conducted in March 2016 to identify all the data related to the journey of RA patients. In addition, Annals of Rheumatic Diseases, American College of Rheumatology Conference Index, and European League Against Rheumatism Conference Index were searched for relevant abstracts that are not published elsewhere.
The following keywords were used in the search for literature: [time lag, delay, duration] between [onset of symptoms of rheumatoid arthritis] and [presentation to/encounter/consult] of [a physician/rheumatologist]. In addition, we searched: [time lag, delay, duration] between [onset of symptoms of rheumatoid arthritis] and [initiation antirheumatic drugs]. All the search terms were “exploded” in conjunction with using a keyword search. The search was conducted on March 31, 2016, and was limited to English language papers.
Included databases were distributed among authors and were searched independently using the above keywords. In each database, all the search results were reviewed and papers were checked for their relevance to our primary and secondary objectives based on their title, abstract, and manuscript. Papers that were not related to our objectives were excluded primarily. After the first round of work, databases were switched among authors to ensure accuracy of literature search and selection. Disagreements were settled through discussion between the authors. The studies were subjected to 3-phase selection. Titles were screened in the first round, abstracts in the second round, and full-texts in the third round. The most recent study was considered in the case of duplicate or overlapping population studies.
Studies were eligible for inclusion if they contained original data on number of patients, lag between the onset of symptoms and first physician visit or lag between initial visit and rheumatology referral, or lag from referral to diagnosis and/or lag from diagnosis to the initiation of DMARDs. Papers analyzing the significance of factors contributing to these lags in RA patients were selected toward the secondary objective of this review. Studies satisfying the above criteria were eligible for inclusion, irrespective of demographic, geographic, or design variations.
Lag times were not reported uniformly among papers. For example, some considered lag1 as the time from onset to first medical encounter while others considered it as the time from first medical encounter until referral to rheumatologist, and so on. Many studies reported a single time lag (eg, from onset to diagnosis) and provided no further details. Some studies reported lag time in weeks and others in months. Some articles compared the results of 2 or more studies that were performed under similar settings but in 2 different time periods followed by comparison of lag times. Descriptive presentation also varied as some studies reported lag time as averages while others reported the median values. Except for the mean and median issue, we resolved other issues by setting our own definitions of lag times, namely lag1 as the time from onset of symptoms to seeking first medical consultation; lag2 as time from seeking medical consultation until referral to rheumatologist; lag3 as the time from referral to definite RA diagnosis, and lag4 as the time from diagnosis to the initiation of DMARDs.
If detailed lag times were not reported in any study, but only a single lag time with a specific start and end points, cells in the corresponding row on the table were merged according to the start and end points specified in that study. We used months as time unit uniformly. Whenever the lag times were reported in weeks and days, we converted them into months. In the case of comparative studies, we only reported data from the latest studies.
For the mean and median issue, when calculating the total lag time, we included only studies that had reported the delay in mean and SD value in the calculation of the total lag times.
Results and discussion
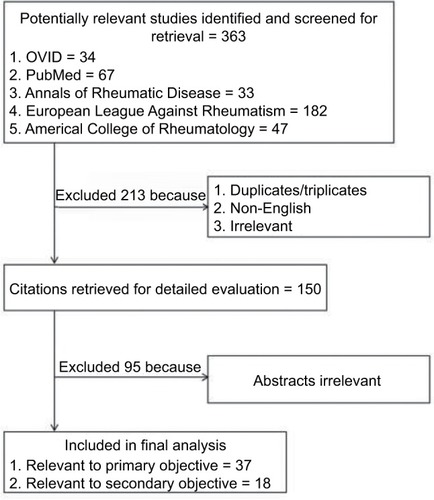
The initial literature search returned 363 titles. After screening of titles for eliminating duplicates and irrelevant studies, we were left with 150 studies. Ninety-five studies were eliminated in the next stage after abstract and full-text screening (). Out of these, 37 studies were relevant to 1 or multiple variables of our primary objective, and 18 studies were relevant to our secondary objective. Data from these papers were extracted and reviewed.
The full-text papers from the first and second category were reviewed. Studies that were only available as informative abstracts were included if complete data on the number of subjects and lag time were provided, even if published in non-English languages.
outlines the main data from the eligible studies. Twelve studies reported the total lag time from the onset of symptoms to the initiation of DMARD therapy. The weighted average of median lag time of 5,512 patients from the onset of symptoms to therapy was 11.79 months with a range of 3.6–24.0 months ().Citation16–Citation26
Table 1 Characteristics of the studies providing data relevant to our analysis
Lag1 data were also available from 12 studies on a total of 6,055 RA patients. The weighted average of median lag time from the onset of symptoms to the first physician consultation was 3.41 months with a range of 0–5.7 months.Citation17,Citation20,Citation22,Citation26–Citation34
Lag2 data were available from 13 studies on a total of 34,767 RA patients. The weighted average of median lag time for RA specialist referral after consulting a physician was 2.13 months with a range of 0.5–6.6 months.Citation17,Citation20,Citation22,Citation25,Citation26,Citation29–Citation31,Citation33–Citation37
Lag3 data were available from 3 studies on a total of 563 RA patients. The weighted average of median lag time for the diagnosis of RA after consulting a rheumatologist was 2.91 months with a range of 0–5 months.Citation16,Citation17,Citation21
Lag4 data were available from 5 studies on a total of 30,685 RA patients. The weighted average of median lag time for initiation of DMARD therapy after definite diagnosis of RA was 2.14 months with a range of 0–2.2 months.Citation16,Citation17,Citation20,Citation24,Citation37
Early RA diagnosis and gaps in care
The understanding of “early” RA is heterogeneous. Two of 3 rheumatologists use the term “early” for symptoms shorter than 3 months. The vast majority of the rheumatologists surveyed regard symptom duration of <3 months as early.Citation38
Evidence is accumulating that very early RA (within the first 12 weeks) may be an immunopathologically distinct phase of disease. Thus, a “window of opportunity” may exist during which introducing DMARDs may have different effects than treatment at a later date, including prevention of erosions and possibly complete switching off of the disease.Citation39
It was found that the strongest predictor of improvements in disease activity (according to the American College of Rheumatology definition) was shorter disease duration at the start of treatment.Citation39
Gaps in care begin with the person’s recognition of the symptoms and the action of visiting a family physician (FP). If RA is suspected, the FP refers the person to a rheumatologist who provides diagnosis and prescribes appropriate medications. Next, the person will be periodically assessed by a rheumatologist.
Studies performed in the past 2 decades which evaluate the onset of DMARDs treatment in patients with early RA, performed in the USA, Spain, Canada, the UK, the Middle East, and in European countries, show that the mean time since the onset of disease and the onset of disease-modifying antirheumatic treatment ranges from 6 to 18 months.Citation22 This indicates that the diagnosis of RA after the onset of symptoms is delayed, and therefore, the objective of starting treatment early is not achieved in most of the cases.
Causes of delay
Delay is probably due to a combination of patient-related and physician-related factors. We reviewed 17 papers and analyzed factors contributing to the delay in care for RA patients ().
Table 2 Factors associated with delays in the diagnosis and treatment of rheumatoid arthritis
The results of a recent study published in 2014 evaluating the time since the beginning of disease and the visit to the FP, the time since this and the referral to the rheumatologist, and the time to onset of DMARD treatment,Citation22 showed that only in 19% of patients, DMARDs were started in the first 3 months after disease onset and that the delay in the prescription of DMARDs was mainly due to the delay in referral from family medicine to the rheumatologist.
In addition to the assumption of incompetency and poor knowledge, a qualitative research among osteoarthritis (OA) and RA patients in Germany, France, Spain, UK, and Italy revealed that for the majority of interviewed patients, their general practitioner visit is rated as disappointing due to poor communication and a focus merely on pain control. The journey that a patient undergoes before seeking medical advice is frequently long and emotionally exhausting.Citation40
Delay in the diagnosis and management of RA may stem from slow diagnosis by physicians rather than postponed medical consultation by patients. This may be because patients with RA often do not seek the advice of rheumatologists at the onset of their symptoms and non-rheumatologists fail to refer RA patients to rheumatologists soon enough. In Saudi Arabia, although patients consulted with physicians at a mean of 7 months after the onset of RA symptoms, very few subjects initially sought a consultation with rheumatologists, who were ultimately responsible for diagnosing most RA patients.Citation14 It is thus believed that delayed specialist referrals constitute a principal reason for late diagnosis and subsequent treatment.
Possible interventions
It is necessary to implement measures that act on early diagnosis and treatment of RA, through the diffusion of knowledge relating to the disease in the general population, advertising campaigns as well as an increase in the level of knowledge regarding RA in primary care physicians.
Successful intervention is largely dependent on the availability of local programs and the coordination among the rheumatologist, the FP, and other health professionals. Moving from one level of care to the next involves a potential wait period.Citation41
A 2013 systematic literature review addressed and identified 3 main areas of delay to care for patients with inflammatory arthritis (IA) and potential solutions.Citation42 From the onset of symptoms to primary care, several websites provided information but were of varying quality and insufficient to aid early referral. At a primary care level, many guidelines emphasized the need for early referral with providing specific referral criteria.Citation39,Citation43 Once referred, early arthritis clinics provided a point of early access to rheumatology assessment. Triage systems, including triage clinics, helped prioritizing clinic appointments for patients with IA. Use of referral forms standardized the information required, further optimizing the triage process.
Guidelines for early referral are needed.Citation38 Clinical criteria would facilitate early referral of the patient with suspected RA to a rheumatologist for definitive diagnosis and initiation of DMARD treatment. In a recently published study by Almoallim et al,Citation44 we have validated the variables that may aid in the design of referral criteria. These are based on musculoskeletal examination techniques to assess the presence of arthritis by primary care physicians in “target” joints; wrists, second and third metacarpophalangeals, and third proximal interphalangeal joints.Citation45 This is in addition to positive rheumatoid factor and anti-citrullinated protein antibody (anti-cyclic citrullinated peptide).
Key points of the referral criteria were formed based on literature review. Clinical evidence strongly supports the observations that rapid referral to a rheumatologist is advised when RA is suspected, which may be supported by the presence of any of the following: persistent joint swelling in more than 1 joint, early morning stiffness ≥30 minutes, or involvement of metacarpophalangeal or metatarsophalangeal joints.Citation39,Citation43 These criteria were mainly based on experts’ opinion not on validated measures as in our unpublished work. Urgent referral (ideally within 6 weeks of symptom onset) to rheumatology should then be made with a clear indication that IA (or RA) is suspected. This should be done without waiting for the results of tests such as rheumatoid factor and plain radiographs, which are often normal in the early phase of disease.Citation39,Citation43
All rheumatologists should make it a priority to see patients with suspected IA on an urgent basis. Triage is important to facilitate early treatment; however, rheumatologists in this service are not currently triaging suspected RA referrals with reference to known poor prognostic indicators.Citation46 However, several interventions could improve both informative referrals and triaging of referrals to decrease time to diagnosis and treatment including public education, general practitioner education sessions with associated distribution of referral guidelines, and reminding triaging rheumatology clinicians about the available prognostic factors often present in general practitioner referrals that assist with correct triage.Citation46
Acknowledgments
This work was supervised and funded by Alzaidi Chair of Research in Rheumatic Diseases, Umm Alqura University. The authors are grateful to Dr Soha Elmorsy, MD, PhD, Research Consultant, King Abdullah Medical City, Makkah, KSA, for statistical advice.
Disclosure
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or nonfinancial interest in the subject matter or materials discussed in this manuscript. The authors report no conflicts of interest in this work.
References
- PincusTCallahanLFReassessment of twelve traditional paradigms concerning the diagnosis, prevalence, morbidity and mortality of rheumatoid arthritisScand J Rheumatol198918Suppl796796
- SherrerYSBlochDAMitchellDMYoungDYFriesJFThe development of disability in rheumatoid arthritisArthritis Rheum19862944945003707627
- SteimanAJPopeJEThiessen-PhilbrookHNon-biologic disease-modifying antirheumatic drugs (DMARDs) improve pain in inflammatory arthritis (IA): a systematic literature review of randomized controlled trialsRheumatol Int20133351105112023292213
- AaltonenKJVirkkiLMMalmivaaraAKonttinenYTNordströmDCBlomMSystematic review and meta-analysis of the efficacy and safety of existing TNF blocking agents in treatment of rheumatoid arthritisPLoS One201271e3027522272322
- PincusTRheumatoid arthritis: disappointing long-term outcomes despite successful short-term clinical trialsJ Clin Epidemiol19884111103710413060568
- KushnerIDoes aggressive therapy of rheumatoid arthritis affect outcome?J Rheumatol198916112497254
- HarrisEDJrRheumatoid arthritis: pathophysiology and implications for therapyN Engl J Med199032218127712892271017
- AndersonJJWellsGVerhoevenACFelsonDTFactors predicting response to treatment in rheumatoid arthritis: the importance of disease durationArthritis Rheum2000431222910643696
- BorgGAllanderELundBAuranofin improves outcome in early rheumatoid arthritis. Results from a 2-year, double blind placebo controlled studyJ Rheumatol198815121747175414552308
- SinghJASaagKGBridgesSLJr2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid ArthritisArthritis Rheumatol2016681126
- JacobyRJaysonMCoshJOnset, early stages, and prognosis of rheumatoid arthritis: a clinical study of 100 patients with 11-year follow-upBr Med J197325858964700332
- LinosAWorthingtonJWO’FallonMKurlandLTThe epidemiology of rheumatoid arthritis in Rochester Minnesota: a study of incidence, prevalence, and mortalityAm J Epidemiol1980111187987352462
- ChanKWAFelsonDTYoodRAWalkerAMThe lag time between onset of symptoms and diagnosis of rheumatoid arthritisArthritis Rheum19943768148208003053
- HussainWNoorwaliAJanoudiNFrom symptoms to diagnosis: an observational study of the journey of rheumatoid arthritis patients in Saudi ArabiaOman Med J20163112926816566
- Hernández-GarcíaCVargasEAbásoloLLag time between onset of symptoms and access to rheumatology care and DMARD therapy in a cohort of patients with rheumatoid arthritisJ Rheumatol200027102323232811036824
- Rodríguez-PolancoEAl SnihSKuoY-FMillánARodríguezMALag time between onset of symptoms and diagnosis in Venezuelan patients with rheumatoid arthritisRheumatol Int201131565766520066425
- JamalSAlibhaiSMBadleyEMBombardierCTime to treatment for new patients with rheumatoid arthritis in a major metropolitan cityJ Rheumatol20113871282128821572157
- ZafarSBadshaHMoftiAEfforts to increase public awareness may result in more timely diagnosis of rheumatoid arthritisJ Clin Rheumatol201218627928222955475
- ClementeDHernández-GarcíaCAbásoloLReduction in time until first treatment with disease modifying treatment in patients with rheumatoid arthritisReumatol Clín (English Edition)200736245250
- WiddifieldJBernatskySThorneJCWait times to rheumatology care for patients with rheumatic diseases: a data linkage study of primary care electronic medical records and administrative dataCMAJ Open201642E205E212
- AmbrožičAGaspersicNHocevarATime to disease-modifying anti-rheumatic drug treatment for new patients with rheumatoid arthritis-single center experienceArthritis Rheumatol201567694695
- Zonana NacachACampaña-ParraASantana-SahagúnJEThe lag time between onset of symptoms, medical encounter, and initiation of disease modifying antirheumatic drugs in patients with rheumatoid arthritisReumatol Clín (English Edition)2014102131132
- De CockDMeyfroidtSJolyJVan der ElstKWesthovensRVerschuerenPA detailed analysis of treatment delay from the onset of symptoms in early rheumatoid arthritis patientsScand J Rheumatol20144311824050519
- De CockDMeyfroidtSJolyJVan der ElstKWesthovensRVerschuerenPAB0169 Type of rheumatology practice is an important determinant of treatment delay in flandersAnn Rheum Dis201372Suppl 3A837
- Van DoornumSTropeaJTaceyMLiewDTime To Institution Of Disease Modifying Anti-rheumatic Drugs In Australian Patients With Early Rheumatoid ArthritisArthritis & Rheumatism201365S565
- KielyPWilliamsRWalshDYoungAEarly Rheumatoid Arthritis NetworkContemporary patterns of care and disease activity outcome in early rheumatoid arthritis: the ERAN cohortRheumatology (Oxford)2009481576018984608
- ChoKJJangSHLeeSKDohWSUtilization characteristics of health care service for rheumatoid arthritis patients in KoreaYonsei Med J19983932472519664830
- IrvineSMunroRPorterDEarly referral, diagnosis, and treatment of rheumatoid arthritis: evidence for changing medical practiceAnn Rheum Dis199958851051310419871
- KumarKDaleyECarruthersDDelay in presentation to primary care physicians is the main reason why patients with rheumatoid arthritis are seen late by rheumatologistsRheumatology20074691438144017578850
- van der LindenMPLe CessieSRazaKLong-term impact of delay in assessment of patients with early arthritisArthritis Rheum201062123537354620722031
- KimuraMYoshidaKOshikawaHAB0308 Delay in referral and diagnosis of rheumatoid arthritis in a community medical center in japanAnn Rheum Dis201371Suppl 3655
- NataliaZChristianAWMariaFMDelay in consultation and starting disease modifying anti-rheumatic drugs in patients with rheumatoid arthritis in ArgentinaHow early arthritis clinics impact on health barriers?Paper presented at: 2013 ACR/ARHP Annual MeetingOctober 25–30; 2013San Diego, CA
- FautrelBJoubertJ-MCukiermanGLaurendeauCGourmelenJFagnaniFTHU0512 Rheumatoid arthritis (RA), comorbidities and biological agents uptake in France: analysis of a national claims databaseAnn Rheum Dis201372Suppl 3A337
- NanjiJAChoiMFerrariRLyddellCRussellASTime to consultation and disease-modifying antirheumatic drug treatment of patients with rheumatoid arthritis – Northern Alberta PerspectiveJ Rheumatol201239470771122337235
- WiddifieldJBombardierCThorneJCA novel approach to assess wait-times to rheumatologistsPaper presented at: Arthritis and Rheumatology2014Hoboken, NJ
- AyasSNurMDiagnosis, referral pattern and course of early arthritis: results of a special early arthritis clinicAnn Intern Med19961246997078633829
- LacailleDAnisAHGuhDPEsdaileJMGaps in care for rheumatoid arthritis: a population studyArthritis Care Res2005532241248
- AletahaDEberlGNellVMacholdKSmolenJPractical progress in realisation of early diagnosis and treatment of patients with suspected rheumatoid arthritis: results from two matched questionnaires within three yearsAnn Rheum Dis200261763063412079906
- HyrichKLPatients with suspected rheumatoid arthritis should be referred early to rheumatologyBMJ2008336763721521618219044
- DiazaraqueRScottC[SAT0503] From me to you (without love): the arthritis patient journey from symptom onset to medical diagnosisAnn Rheum Dis200968Suppl3705
- LiLC[SP0106] Gaps in care and research in health service delivery: using rheumatoid arthritis as a sample caseAnn Rheum Dis200968Suppl33318230627
- VilleneuveENamJLBellMJA systematic literature review of strategies promoting early referral and reducing delays in the diagnosis and management of inflammatory arthritisAnn Rheum Dis2013721132222532640
- EmeryPBreedveldFDougadosMKaldenJSchiffMSmolenJEarly referral recommendation for newly diagnosed rheumatoid arthritis: evidence based development of a clinical guideAnn Rheum Dis200261429029711874828
- AlmoallimHJanoudiNAttarSMDetermining early referral criteria for patients with suspected inflammatory arthritis presenting to primary care physicians: a cross-sectional studyOpen Access Rheumatology: Research and Reviews201798128490909
- AlmoallimHAttarSJannoudiNSensitivity of standardised musculoskeletal examination of the hand and wrist joints in detecting arthritis in comparison to ultrasound findings in patients attending rheumatology clinicsClin Rheumatol20123191309131722673791
- RobinsonPCTaylorWJTime to treatment in rheumatoid arthritis: factors associated with time to treatment initiation and urgent triage assessment of general practitioner referralsJ Clin Rheumatol201016626727320689443
- SokkaTPincusTContemporary disease modifying antirheumatic drugs (DMARD) in patients with recent onset rheumatoid arthritis in a US private practice: methotrexate as the anchor drug in 90% and new DMARD in 30% of patientsJ Rheumatol200229122521252412465145
- FeldmanDEBernatskySHaggertyJDelay in consultation with specialists for persons with suspected new-onset rheumatoid arthritis: a population-based studyArthritis Care Res200757814191425
- BadshaHKongKOTakPPRheumatoid arthritis in the United Arab EmiratesClin Rheumatol200827673974217973153
- Ankjær-JensenAHospital waiting time for patients with rheumatic diseases in DenmarkAnn Rheum Dis200968Suppl3799
- KohETThongBTehCLDifferences in patients with rheumatoid arthritis presenting over time from 1960 to 2005Ann Rheum Dis200968Suppl 3415
- FathiNAbdaEAMSalimZAKongKBadshaHRheumatoid arthritis in a cross section of Egyptian patientsAnn Rheum Dis200968Suppl3422
- BlancoFJBallinaJCarbonellJDescriptive study of the use of DMARD in patients with rheumatoid arthritis or persistent arthritis who start drug treatment in Spain (FIRST)Reumatol Clín2011728893 Spanish21794790
- RazaKStackRKumarKDelays in assessment of patients with rheumatoid arthritis: variations across EuropeAnn Rheum Dis201170101822182521821867
- VerschuerenPJolyJLangenakenCPatient and disease related determinanats of the delay between symptom onset and the diagnosis of RA in a Flemish populationAnn Rheum Dis201170Suppl359021372193
- ZafarSBadshaHMoftiAEfforts to increase public awareness may result in more timely diagnosis of rheumatoid arthritisJ Clin Rheumatol201218627928222955475
- Gόmez CaballeroMECorominasHNarváezJAB1361 Diagnostic and therapeutic delay of rheumathoid artritis patients in catalonia (Spain) and their relationship with specialized healthcare units. The audit studyAnn Rheum Dis201371Suppl 3715
- De CockDWesthovensRJolyJVerschuerenPSAT0454 Determinants of delay between onset of symptoms and initiation of treatment in a belgian RA populationAnn Rheum Dis201371Suppl 3626
- GibsonKALutaGPincusTAB0255 Delay in diagnosis from onset of symptoms by more than one year in 48% of 177 patients with rheumatic diseases, including 36% in patients with rheumatoid arthritis in AustraliaAnn Rheum Dis201473Suppl 2888
- SørensenJHetlandMLDiagnostic delay in patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis: results from the Danish nationwide DANBIO registryAnn Rheum Dis2015743e1224534758
- BenaglioFBalduzziSBugattiSSakellariouGMontecuccoCCaporaliRDiagnostic Delay in Early Arthritis: Ten Years-experience of a Single CenterArthritis & Rheumatology201567712714
- LardLRHuizingaTWHazesJVlielandTDelayed referral of female patients with rheumatoid arthritisJ Rheumatol200128102190219211669154
- Xibillé-FriedmannDMondragón-FloresVde la RosaCHCriteria used by primary care physicians for the diagnosis and referral to a rheumatologist of patients with rheumatoid arthritisReumatol Clín20062523523821794335
- NeillLOKitchenJCoughlanRJ[FRI0238] Impediments to early referral and assessment of patients with early inflammatory arthritis – a primary care perspectiveAnn Rheum Dis201170Suppl 342321109518
- WiddifieldJPatersonMJBernatskySPotential Barriers That Limit Access to Rheumatologists Among Patients with Early Rheumatoid Arthritis in a Universal Access Health Care SystemArthritis & Rheumatism201264S1060
- PanchalSSamantaAMoorthyAHayatSPandeIAdebajoAOChakravartyKA British survey of time to presentation and treatment of rheumatoid arthritis in subjects of black and minority ethnic originACR Meeting Abstracts2012
- DelaurierABernatskySBaronMLégaréJFeldmanDEWait times for rheumatology consultation: is rheumatoid arthritis prioritized?J Clin Rheumatol201218734134423013849
- GrygielskaJOP0241-PARE Time to diagnosis and quality of life people with diagnosed rheumatoid arthritis in polandAnn Rheum Dis201371Suppl 3137
- MolinaERestrepoJFdel RinconIBattafaranoDEscalanteATreatment Delays and Worse Outcomes Associated with Lower Socioeconomic Status in Rheumatoid ArthritisArthritis & Rheumatology201466S889S890
- BarnabeCXiongJPopeJEFactors associated with time to diagnosis in early rheumatoid arthritisRheumatol Int2014341859223989941
- SungYKChoSKKimDFactors Associated with Time to Diagnosis from Symptom Onset in Early Rheumatoid Arthritis PatientsArthritis & Rheumatology201466S889
- WiddifieldJThorneCJTuKPrimary Care Management of Patients with Rheumatic Diseases Prior to Rheumatologist ConsultationArthritis & Rheumatology20156730393041
- SimonsGMallenCDKumarKStackRJRazaKA qualitative investigation of the barriers to help-seeking among members of the public presented with symptoms of new-onset rheumatoid arthritisJ Rheumatol201542458559225641894
- MolinaEDel RinconIRestrepoJFBattafaranoDFEscalanteAAssociation of socioeconomic status with treatment delays, disease activity, joint damage, and disability in rheumatoid arthritisArthritis Care Res2015677940946
- PeerboomDVan der ElstKDe CockDThe patient trajectory from symptom onset until referral to a rheumatologistPaper presented at: European Congress of RheumatologyJune 10–13; 20152015Rome
- MølbækKHørslevPetersenKPrimdahlJDiagnostic delay in rheumatoid arthritis: a qualitative study of symptom interpretation before the first visit to the doctorMusculoskeletal care2016141263626052985
- PrattAGLendremDHargreavesBAslamOGallowayJBIsaacsJDComponents of treatment delay in rheumatoid arthritis differ according to autoantibody status: validation of a single-centre observation using national audit dataRheumatology201655101843184827373893