Abstract
We present an 18-year-old female from South Sudan presented with right fingertips ulceration and black discolouration associated with bilateral wrist/metacarpophalangeal joints pain for five months. The ulceration began at the tip of the right middle finger and gradually progressed to involve the rest of the hand and was associated with agonizing pain. A Doppler study of the right upper limb revealed thrombosis of the antecubital portion of the basilar, ulnar, and part of the distal radial arteries. Blood investigations showed high anti-CCP, doubtful rheumatoid factor titre and ANA titre of 1:320 with coarse and nucleated cells; however, all ANA parameters were negative. A definitive diagnosis of rheumatoid arthritis complicated by rheumatoid vasculitis was made. Unfortunately, the middle finger could not be preserved and ended up amputated, and the patient was commenced on steroids, DMARDs and warfarin. The patient responded very well to the management plan with pain alleviation, ulcers healing and clot resolution.
Introduction
Rheumatoid Vasculitis (RV) is a rare, catastrophic complication of longstanding deforming Rheumatoid Arthritis (RA).Citation1 It is an autoimmune vasculitis characterized by a necrotizing or leukocytoclastic process that mainly affects small to medium-sized blood vessels and is associated with significant mortality rates, making it one of the most serious extra-articular manifestations of rheumatoid arthritis, necessitating prompt recognition and intervention.Citation1,Citation2
Rheumatoid Vasculitis preceding or following a recent diagnosis of rheumatoid arthritis rather than a longstanding disease is a distinct uncommon entity; however, if diagnosed and treated promptly, it can prevent the development of severe comorbidities.Citation3 RA diagnosis is made using EULAR criteria, with the presence of all the following: Inflammatory arthritis involving three or more joints, positive rheumatoid factor (RF) and/or anti-citrullinated peptide antibodies (anti-CCP), elevated levels of CRP and/or ESR and duration of symptoms is more than six weeks.Citation4 Although no current criterion is available to diagnose RV, it should be expected in patients with longstanding rheumatoid arthritis and raised anti-CCP/RF presenting with vasculitis lesions (commonly Digital Ischemia), imaging studies showing ischemia and/or tissue biopsy showing vasculitis, and exclusion of other causes of vasculitis (ANCA related vasculitides, polyarteritis nodosa, etc.).Citation5
The incidence of RV has reduced to a less than 1% among RA patients, given the introduction of methotrexate and other biologic disease-modifying antirheumatic drugs in the recent era.Citation6,Citation7 Nevertheless, autopsy results show a significantly higher percentage of prevalence reaching 30%.Citation8 Males are 2.3 times more prone to developing RV than females.Citation9 Furthermore, the 5-year mortality of RV reaches to almost 40%.Citation10
We present a rare case of RV demonstrated in a non-deforming RA female patient, causing upper limb arterial thrombosis, and warranting middle finger amputation.
Case Report
An 18 years old female nonsmoker from South Sudan presented to the medical casualty with unilateral painful fingertip ulceration and black discolouration for five months. The ulceration began at the tip of the right middle finger and gradually progressed to involve the rest of the hand and was associated with agonizing pain; nevertheless, no involvement of the other hand (no ulcers, discolouration or deformity). The patient sought advice, and a Doppler U/S of the right upper limb revealed arterial thrombosis of the antecubital portion of basilar, ulnar, and part of the distal radial arteries with normal proximal basilar, axillary and subclavian artery. The patient underwent a partial amputation of the right middle finger and was referred for our consultation afterwards as no final diagnosis was reached and no thorough workup was done at the time. On assessing the patient, she reported a seven-month history of high-grade remittent fevers associated with weight loss and fatigue. She also described bilateral wrists and metacarpophalangeal joints pain, not associated with morning stiffness, sicca symptoms (dry skin, dry eyes, etc.), or genital ulceration. A further systematic review was unremarkable, apart from bilateral frontal headache and amenorrhea for five months.
On physical examination, the patient was in pain, not pale or jaundiced, with a weak radial pulse bilaterally, an amputated middle finger and extensive digital ulceration. No ulcers were present elsewhere, and the rest of the examination did not show signs of any inflammatory process, skin lesions or joint deformities ().
Figure 1 Right hand of the patient post middle finger amputation, demonstrating extensive digital ulceration.

Routine lab tests, hands X-ray and an immunological workup were requested, revealing normocytic normochromic anaemia, elevated Anti-CCP levels with rheumatoid factor level was doubtful. Nonetheless, the ANA Global titre was 1:320 with coarse and nucleated cells with all ANA parameters being negative, thus suggestive of exclusively active rheumatoid arthritis ().
Table 1 Complete Blood Picture
Table 2 Immunology Workup
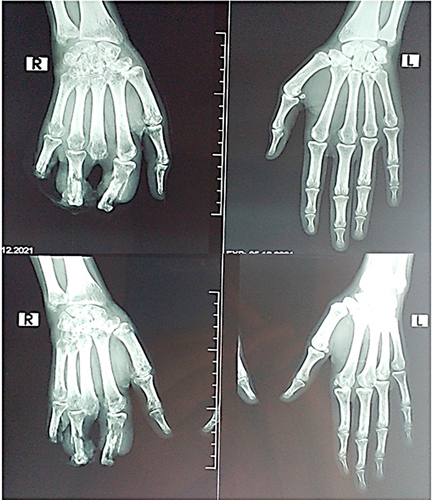
Hand x-ray shows reduced bone density at the distal end of the radius and ulna, carpal bone, and metacarpophalangeal joint with a fracture in the index and ring fingers and an amputated middle finger ().
Figure 2 Bilateral hands x-ray demonstrating right hand reduced bone density in the distal end of radius and ulna, carpal bone, and metacarpophalangeal joint with a fracture in the index and ring fingers and amputated middle finger. Normal left hand.
A definitive diagnosis of rheumatoid arthritis (EULAR 7 and DAS 28-ESR 5.8) complicated with rheumatoid vasculitis was made. The patient was commenced on low-dose prednisolone, hydroxychloroquine, methotrexate, and warfarin. The patient responded very well to the management plan with pain alleviation, ulcers healing, clot resolution and normalization of his inflammatory markers. All medications were continued except for warfarin, which was stopped after six months.
Discussion
Rheumatic vasculitis is an infrequent complication of longstanding severe rheumatoid arthritis. It is one of the most alarming extra-articular manifestations of rheumatoid arthritis and is associated with high morbidity and mortality; however, it manifests in only 1–5% of the patients.Citation11 Deposition of the immune complexes may be a major contributor to vascular inflammation in patients with rheumatoid arthritis. The most common manifestation of rheumatoid vasculitis is cutaneous vasculitis like palpable purpura, nail bed infarcts and digital gangrene,Citation3 which was the presenting complaint in our patient with elevated ESR; consistent with the fact that vasculitis is associated with systemic inflammatory response and the majority of the patients with rheumatoid vasculitis present with very high ESR.Citation2 Furthermore, higher levels of anti-CCP appear to be associated with progressive and severe extra-articular manifestation like vasculitis,Citation3 being 137 in our patient.
The literature reports that vasculitis mainly occurs in patients with a longstanding disease with severe joint deformity.Citation11 Major risk factors for developing vasculitis include male gender, smoking and longstanding disease.Citation3
Our patient, an 18-year-old female nonsmoker, presented with vasculitis that predates the diagnosis of rheumatoid arthritis, which is a very rare and unique presentation.
To the best of our knowledge, only four patients presented with vasculitis preceding or following a recent diagnosis of rheumatoid arthritis. These cases included 61 years male presenting with pulmonary vasculitis with subsequent development of anti-CCP positive symmetric polyarthritis;Citation12 secondly, a 63-year-old man who developed bilateral carpal tunnel syndrome, mononeuritis of both sciatic nerve and inflammatory myositis six months after being diagnosed with rheumatoid arthritis.Citation13 The third was a 38-year-old man presenting with polyarteritis nodosa-like symptoms; however, on stopping treatment after six years, he developed RA; thus, misdiagnosed as at the beginning as PAN rather than rheumatoid vasculitis.Citation14 Lastly, a 74-year-old man presented with acute cholecystitis within a week of diagnosis with rheumatoid arthritis and, nonetheless, histopathologic evidence of small vessel vasculitis and rheumatoid nodules.Citation15
Rheumatoid vasculitis is actively managed with corticosteroids and cyclophosphamide.Citation11 Furthermore, cutaneous vasculitis commonly responds to lower doses of immunosuppression than systemic vasculitis, which mandates higher doses of immunosuppression and has an overall poor prognosis.Citation14
Conclusion
Rheumatoid vasculitis preceding non-deforming RA is a very rare entity causing devastating outcomes. Prompt recognition and management are crucial given their wide range of involvements and complications. Therefore, a multidisciplinary approach is required, together with further studies to be performed to construct an explicit criterion for diagnosis and management.
Consent
Written informed consent was obtained from the patient for publication of her case details with images of her hand lesions.
Disclosure
All authors report no conflicts of interest in this work.
Acknowledgments
Medical staff at Haj El-Safi Teaching Hospital.
References
- Kishore S, Maher L, Majithia V. Rheumatoid vasculitis: a diminishing yet devastating menace. Curr Rheumatol Rep. 2017;19(7):39. doi:10.1007/s11926-017-0667-3
- Makol A, Matteson EL, Warrington KJ. Rheumatoid vasculitis: an update. Curr Opin Rheumatol. 2015;27(1):63–70. doi:10.1097/BOR.0000000000000126
- Makol A, Crowson CS, Wetter DA, Sokumbi O, Matteson EL, Warrington KJ. Vasculitis associated with rheumatoid arthritis: a case-control study. Rheumatology. 2014;53(5):890–899. doi:10.1093/rheumatology/ket475
- Aletaha D, Neogi T, Silman AJ, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62(9):2569–2581. doi:10.1002/art.27584
- Whelan P. Clinical Manifestations and Diagnosis of Rheumatoid Vasculitis. Matteson EL, Romain PL, Eds. Uptodate; 2022. Available from: https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-rheumatoid-vasculitis?search=rheumatoid%20vasculitis&source=search_result&selectedTitle=1~72&usage_type=default&display_rank=1#H19127931.
- Watts RA, Mooney J, Lane SE, Scott DG. Rheumatoid vasculitis: becoming extinct? Rheumatology. 2004;43:920. doi:10.1093/rheumatology/keh210
- Stone J. Massachusetts general hospital department of pathology, 2015, personal communication.
- Voskuyl AE, Zwinderman AH, Westedt ML, Vandenbroucke JP, Breedveld FC, Hazes JM. Factors associated with the development of vasculitis in rheumatoid arthritis: results of a case-control study. Ann Rheum Dis. 1996;55(3):190–192. doi:10.1136/ard.55.3.190
- Turesson C, O’Fallon WM, Crowson CS, Gabriel SE, Matteson EL. Occurrence of extra-articular disease manifestations is associated with excess mortality in a community based cohort of patients with rheumatoid arthritis. J Rheumatol. 2002;29(1):62–67.
- Suzuki A, Ohosone Y, Obana M, et al. Cause of death in 81 autopsied patients with rheumatoid arthritis.. J Rheumatol. 1994;21(1):33–36.
- Anwar MM, Tariq EF, Khan U, Zaheer M, Ijaz SH. Rheumatoid vasculitis: is it always a late manifestation of rheumatoid arthritis? Cureus. 2019;11(9):e5790. doi:10.7759/cureus.5790
- Tourin O, de la Torre Carazo S, Smith DR, Fischer A. Pulmonary vasculitis as the first manifestation of rheumatoid arthritis. Respir Med Case Rep. 2013;8:40–42. doi:10.1016/j.rmcr.2013.01.003
- Parker B, Chattopadhyay C. A case of rheumatoid vasculitis involving the gastrointestinal tract in early disease. Rheumatology. 2007;46(11):1737–1738. doi:10.1093/rheumatology/kem237
- Sacks S, Steuer A. Can rheumatoid vasculitis predate a diagnosis of rheumatoid arthritis? Eur J Rheumatol. 2017;4(1):57–58. doi:10.5152/eurjrheum.2017.160058
- Sandhu SK, Choy G. Vasculitis of the gallbladder in early rheumatoid arthritis. BMJ Case Rep. 2013;2013:bcr2012008228. doi:10.1136/bcr-2012-008228
