Abstract
We report a 38-year-old man with a complaint of blurred vision in his right eye for the previous 5 days. He had bilateral optic disc drusen. Fluorescein angiography revealed multiple hyperfluorescent foci within temporal optic discs and temporal inferior arcade in late phase. Optical coherence tomography showed bilateral peripapillary serous detachment as well as right macular detachment. This is the first reported case of a concurrent peripapillary and macular detachment in a patient with central serous papillopathy by optic disc drusen. Central serous papillopathy is an atypical form of central serous chorioretinopathy that should be considered as a potential cause of acute loss of vision in patients with optic nerve head drusen.
Introduction
Optic nerve head drusen (ONHD) are hyaline material calcificated deposits due to an axoplasmic transport alteration in the presence of a small scleral canal.Citation1,Citation2 They are a casual fundus finding but are rarely complicated with a peripapillary choroidal neovascularization, an anterior ischemic optic neuropathy, or a central serous papillopathy (CSP).Citation3 Herein, we report a patient with bilateral peripapillary and right macular serous detachment as first manifestation of ONHD.
Case report
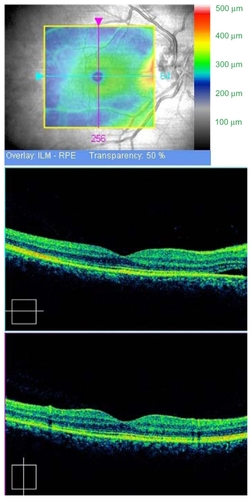
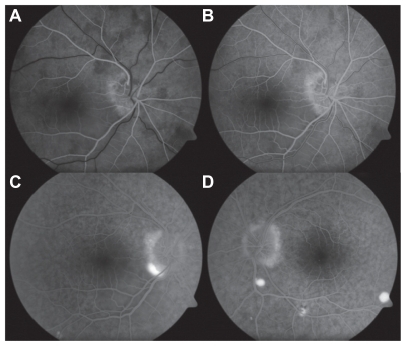
A 38-year-old man presented with complaint of progressive loss of vision for five days in his right eye. Past systemic and ocular history was unremarkable, but flu was reported three weeks before. The diagnosis given by another physician was bilateral viral papillitis. He denied pain on eye movements, discromatopsy, and took no prescription medications. Visual acuity was 20/30 in the right eye and 20/20 in the left eye. Pupils were of equal size and constricted briskly without a relative afferent pupil defect when exposed to direct light. Extraocular movements and biomicroscopic examination of the anterior ocular segment were normal. Fundus examination revealed bilateral ONHD ( and ). The right eye showed a serous detachment extending from optic nerve to macula ( and ). Fluorescein angiography showed autofluorescence of the disk drusen () and abnormal hyperfluorescence from temporal optic discs in early phases (). Our patient also presented one hyperfluorescent focus in lower part of right optic nerve head () and multiple pinpoint foci of hyperfluorescence within temporal inferior veins in late frames (). A cranial tomography scan showed calcium density bodies at both head optic nerves (). Automated static perimetry demonstrated a bilateral enlargement of the blind spot. After two months most of subretinal fluid disappeared () with no treatment and visual acuity improved to 20/20 in both eyes. No relapses occurred during one-year follow-up.
Figure 1 A, B) Fundus photograph shows with a bilateral peripapillary and a macular detachment extending from the right optic disc to the macula. B) In left eye, two anular images correspond to pigment epithelium detachments within inferior temporal vein.
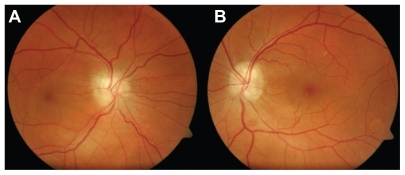
Figure 2 Stratus OCT 3 (Stratus Optical Coherence Tomography 3; Carl Zeiss Meditec, Dublin, CA, USA). The Stratus OCT shows an elevated optic nerve head with a signal-poor region below the surface and a peripapillary serous detachment (white arrows) in both eyes.
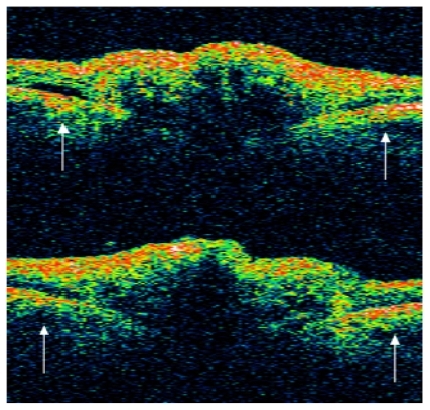
Figure 3 Optical Coherence Tomography Cirrus (Carl Zeiss Meditec, Dublin, CA, USA), macular thickness. It shows a huge neurosensory detachment from disc to macula in right eye.
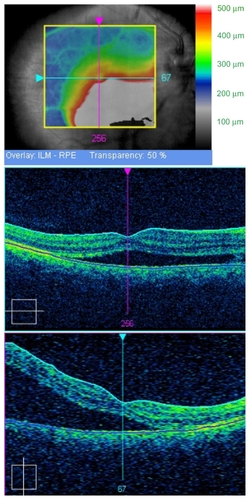
Figure 5 (A, B) Early phase fluorescein angiogram demonstrates hyperfluorescence within temporal disc optic, with appearance in mid-phase and late phase of multiple pinpoint foci of hyperfluorescence (C, D).
Discussion
ONHD are an uncommon congenital entity. Evidence suggests that axoplasmic transport alteration and axonal degeneration are involved in disc drusen formation. Most patients are asymptomaticCitation4 and visual acuity is normally well preserved.Citation5 When a rapid decrease of visual acuity appear in these patients, the differential diagnosis should include anterior ischemic optic neuropathy, central retinal artery or vein occlusion, peripapillary choroidal neovascularization,Citation6,Citation7 and CSP.Citation8,Citation9
Central serous chorioretinopathy (CSC) is a condition characterized by accumulation of transparent fluid under the neurosensory retina, retinal pigment epithelium (RPE), or both, causing a circumscribed macular detachment or RPE detachments. The pathophysiology of CSC remains poorly understood, but focal choroidal hyperpermeability has been recently implicated.Citation10 An exceptional form of CSC is CSP that may occur in normal optic disc or in those with a pit or coloboma.
In our patient, spontaneous reabsorption of fluid and “benign” evolution ruled out a peripapillary choroidal neovascularization, suggesting CSP as a final diagnosis. Moisseiev et al described a case of optic disc drusen and CSP.Citation11 We report the second case in literature describing simultaneous occurrence of optic nerve drusen and CSP, but the first one in which both bilateral peripapillary and macular detachment are observed. Optic nerve drusen seems to alter the normal barrier between the prelaminar optic nerve and the peripapillary retina. This anomalous peripapillary area joined to focal hyperpermeability seen in CSC may act together in the subretinal fluid production in patients with ONHD. It is critical to correctly diagnose patients with CSP to avoid unnecessary work-up and overlooking potential serious conditions such as true papilledema. CSP should be considered as a potential cause for acute loss of vision in patients with optic nerve head drusen.
Disclosure
The authors of this article have no proprietary or commercial interest in any materials or method discussed in this article.
References
- Auw-HaedrichCStaubachFWitschelHOptic disk drusenSurv Ophthalmol20024751553212504737
- TsoMOMPathology and pathogenesis of drusen of the optic nerve headOphthalmol19818810661080
- LeeAGZimmermanMBThe rate of visual field loss in optic nerve head drusenAm J Ophthalmol20051391062106615953437
- WilkinsJMPomeranzHDVisual manifestations of visible and buried optic disc drusenJ Neuroophthalmol20042412512915179065
- LeeAGZimmermanMBThe rate of visual field loss in optic nerve head drusenAm J Ophthalmol20051391062106615953437
- BrownSMdel MonteMAChoroidal neovascular membrane associated with optic head nerve drusen in a childAm J Ophthalmol19961212152178623896
- KiesJCBirdACJuxtapapillary choroidal neovascularization in older patientsAm J Ophthalmol1988105911
- BrodskyMCCentral serous papillopathyBr J Opthalmol199983878884
- JohnsonDAtypical central serous chorioretinopathy with peripapillary subretinal fluid suggesting an optic neuropathyJ Neuro-Ophtalmol200929155156
- PrydsASanderBLarsenMCharacterization of subretinal fluid leakage in central serous chorioretinopathyInvest Ophthalmol Vis Sci201026
- MoisseievJCahaneMTreisterGOptic nerve head drusen and peripapillary central serous chorioretinopathyAm J Ophthalmol1989152022032757107