Abstract
Purpose
To evaluate the optic disc characteristics of eyes with superior segmental optic hypoplasia (SSOH) using the Heidelberg retina tomograph (HRT).
Patients and methods
Thirteen eyes of 13 Japanese patients with SSOH were studied with the HRT (software version: 3.0). The group included six males and seven females, with a mean age of 34.7 years. Six optic disc parameters in the six sectors derived from the patients with SSOH were compared with those of 13 eyes of 13 normal controls. In addition, the diagnostic classification performance of the Frederick S Mikelberg (FSM) discriminant function, glaucoma probability score (GPS), and Moorfields regression analysis (MRA) were assessed.
Results
When compared with normal subjects, many of the optic disc parameters were significantly altered in SSOH in the superior sectors. The area under the curve (AUC) for the receiver operating characteristic was 0.932 for the rim area, 0.926 for the cup-to-disc area ratio, and 0.882 for the cup shape measure. Among the HRT parameters, the largest AUC (0.988) was found for the cup shape measure in the nasal superior segment. The proportion classified as outside normal limits by the FSM discriminant function was 92.3% (12 eyes). For GPS, six eyes (46.2%) were classified as outside normal limits. For MRA, when borderline cases were considered test-negative or test-positive, 10 eyes (76.9%) or 11 eyes (84.6%) were classified as outside normal limits, respectively. The AUCs were 0.976 for the FSM discriminant function, 0.914 for the MRA overall classification, and 0.710 for the GPS overall classification.
Conclusions
In eyes with SSOH, there is a significant thinning of the rim, especially in the nasal superior sector. Approximately half of the eyes with SSOH were classified as abnormal using indices developed for detecting glaucoma, but the sectorial analysis revealed that the affected sectors were different from those of glaucoma. Optic nerve head measurements using the HRT may be useful in evaluating the optic disc characteristics in eyes with SSOH.
Introduction
Superior segmental optic hypoplasia (SSOH) is a congenital optic nerve anomaly characterized by localized inferior visual field defects, superior nerve fiber layer defects, and good visual acuity.Citation1–Citation13 The term “superior segmental optic nerve hypoplasia” (SSONH), which is preferred by some investigators, has also sometimes been used instead of SSOH, because the clinical features of this entity include not only a morphologic optic disc anomaly, but also optic nerve fiber defects.Citation10,Citation12 SSOH is considered to be a type of optic nerve hypoplasia, but is unusual in that the central visual acuity is spared. Kim et al have shown four characteristic findings concerning the optic disc, ie, a relative superior entrance of the central retinal artery, a superior peripapillary scleral halo, pallor of the superior disc, and a thinning of the superior peripapillary nerve fiber layer.Citation4 However, not all of these features could be consistently found in other reports.Citation6,Citation8–Citation10 Instead, a double-ring sign, which is a hallmark of optic hypoplasia, has been found.Citation10 Also, while previous reports from Western countries have demonstrated that SSOH is frequently associated with maternal type 1 diabetes mellitus, reports from Japan and Korea have not supported this association.Citation10,Citation12 Thus, the definition of SSOH remains obscure, and it may possibly consist of multiple optic nerve anomalies.
The Heidelberg retina tomograph (HRT), a confocal scanning laser ophthalmoscopy device, has been used to evaluate quantitatively the three-dimensional surface topography of the optic nerve head and the surrounding nerve fiber layer.Citation14–Citation26 HRT can provide objective measurements of the optic nerve head, such as the cup-to-disc ratio, cup volume, rim area, and thickness of the nerve fiber layer. It is well known that glaucomatous visual field defects appear only after a substantial number of nerve fibers have been lost.Citation27,Citation28 Therefore, HRT is considered to be a promising tool for the early detection of glaucoma. A thinning of the nerve fiber layer often suggests glaucoma, but SSOH is similar to glaucoma in that nerve fiber layer defects and corresponding visual field losses are observed.Citation8 In this study, we investigated the topography of the optic nerve head in SSOH using HRT. This technique includes statistical analyses, Frederick S Mikelberg (FSM) discriminant function,Citation14 Moorfields regression analysis (MRA),Citation16 and the glaucoma probability score (GPS) classification,Citation18 for discriminating glaucomatous and normal optic discs. We also used HRT to evaluate the diagnostic ability of these tests in patients with SSOH.
Subjects and methods
We examined 13 eyes of 13 patients with SSOH. The mean age ± standard deviation of the patients was 34.7 ± 12.9 (range 15–53) years. There were six males and seven females. Seven had bilateral and six had monocular SSOH. Only one eye was randomly selected and examined for bilateral cases. Each eye had a best-corrected visual acuity ≥20/20 and a normal intraocular pressure (IOP) ≤21 mmHg, with no history of elevated IOP, a normal open angle, and an inferior wedge-shaped visual field defect (oriented to the blind spot) with a corresponding retinal nerve fiber layer defect. The retinal nerve fiber layer defects were detected with ophthalmoscopy and documented by fundus photographs. None of the patients was born of a mother with diabetes mellitus. The average mean deviation of the Humphrey full-threshold 30-2 program was −4.35 ± 4.37 (ranging from −11.96 to +1.76) dB. Thirteen eyes of 13 subjects with normal vision were also studied and served as controls. Only one eye was examined for each normal subject. The normal subjects were recruited from the hospital staff or their friends. Ophthalmic examination of these subjects did not reveal any ocular abnormalities.
In each patient, optic disc topography was examined using HRT II (version 3.0; Heidelberg Engineering, GmbH, Heidelberg, Germany). Informed consent was obtained from each subject. HRT II uses a diode laser (670 nm wavelength) to scan the retinal surface sequentially in the horizontal and vertical directions on multiple focal planes. By using confocal scanning principles, a three-dimensional topographic image is constructed from a series of optical image sections at consecutive focal planes. The topographic image determined from the acquired three-dimensional image consists of 384 × 384 (147,456) pixels, each of which is a measurement of the surface height of retina and optic nerve head at its corresponding location. For every subject in this study, images were obtained through undilated pupils, with a 15° field of view. Three topographic images were obtained, combined, and automatically aligned to make a single mean topographic image for analysis. A contour line of the optic disc margin was drawn around the inner margin of the peripapillary scleral ring by an experienced examiner, who had been kept uninformed of the other clinical information. Six HRT parameters obtained with routine analysis were analyzed in terms of the disc area, cup area, cup-to-disc area ratio, rim area, cup shape measure, and height variation contour. Magnification errors were corrected using the subjects’ refractive status and corneal-curvature measurements.
Six sectoral (temporal, nasal, superotemporal, superonasal, inferotemporal, and inferonasal) and global optic nerve head parameters were compared between those of the control subjects and those of patients with SSOH, thus producing P values and the area under the curve (AUC for the receiver operating characteristic) for each comparison.
For the FSM discriminant function, the discriminant analysis formula described by Mikelberg et al was used.Citation14 We chose the FSM discriminant function because it was thought to be the most representative among such discriminant functions. In the MRA, a measured rim area was compared with the predicted rim area adjusted for disc size and age. The normative database was compared in six regions (superior temporal, inferior temporal, temporal, superior nasal, inferior nasal, and nasal) and as an overall global classification. The eyes were classified into three categories: within normal limits (WNL) 95% confidence intervals (CI); borderline (BL), 95%–99.9% CI; and outside normal limits (ONL), 99.9% CI. In the GPS calculation, parameters describing the shape of the optic nerve head and retinal nerve fiber layer were calculated based on the mathematical model derived from normal and glaucomatous eyes in HRT. The parameters thus obtained were used to compute the GPS numeric scores. Then, the final GPS was used for the classification was WNL (0%–27%), BL (28%–64%), and ONL (65%–100%). The AUC curves were plotted between the normal and SSOH eyes for the FSM discriminant function, MRA, and GPS. The categoric variable was computed where “normal” = 0, “borderline” = 1, and “outside normal limits” = 2.
We used Mann–Whitney’s U test for each comparison. Because of the large number of tests, the Bonferroni correction for multiple comparisons was also applied. SPSS (17.0 J; SPSS Japan, Inc., Tokyo, Japan) and MedCalc (version 10.1; MedCalc Software bvba, Mariakerke, Belgium) were used to perform the statistical analysis.
Results
shows the demographic and clinical characteristics of the subjects included in the study. Gender, age, and refraction did not differ significantly between the patients with SSOH and normal subjects. None of the patients with SSOH showed a progression of the visual field defects in the subsequent follow-up. The follow-up period was 74.4 ± 27.2 (range 48–133) months.
Table 1 Demographic and clinical characteristics of the subjects included in the study
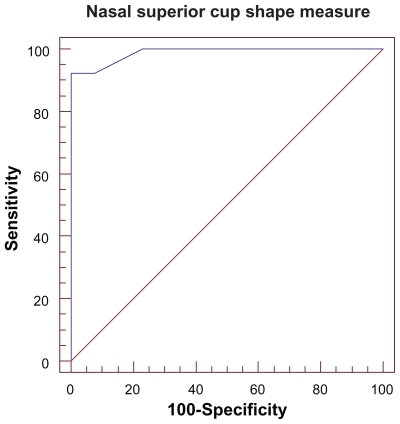
shows various HRT parameters of the patients with SSOH and the healthy control subjects. There was no statistically significant difference between the disc area of patients with SSOH and normal subjects. The cup area and cup-to-disc area ratio were larger, while the rim area was reduced, in patients with SSOH, especially in the superonasal area. The parameters with the largest AUCs were the nasal superior cup shape measure (0.988), the nasal superior cup-to-disc area ratio (0.970), and the nasal superior rim area (0.959). shows the AUC for the nasal superior cup shape measure.
Table 2 Global and segmental optic disc parameters and areas under the receiver operating characteristic curve for each parameter
The results of the diagnostic classification tests are shown in . Using the FSM discriminant function, 92.3% of the eyes were classified as outside the normal limits. By the MRA and GPS, 84.6 (*76.9)% and 46.2% of the eyes were classified as abnormal, respectively (when the borderline was classified as normal). The MRA in each sector revealed that the superonasal rim area was most frequently abnormal (). The AUC was 0.976 for the FSM discriminant function, 0.914 for the MRA, and 0.710 for the GPS. The sectoral analysis of MRA revealed the largest AUC (0.956) in the nasal superior sector. The FSM discriminant function showed a sensitivity of 92.3% and a specificity of 92.3%. The MRA overall classification had a sensitivity of 84.6 (76.9)% and a specificity of 92.3 (100)%. The GPS overall classification had a sensitivity of 46.2 (46.2)% and a specificity of 92.3 (100)%.
Figure 2 A receiver operating characteristic curve for the nasal superior Moorfields regression analysis (MRA).
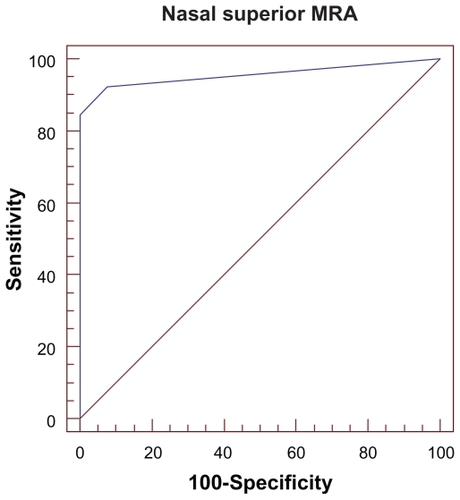
Table 3 ROC, sensitivity, and specificity for the FSM discriminant function, MRA, and GPS used to discriminate between normal eyes and eyes with SSOH
Discussion
Our sectorial analysis of the optic nerve head has shown that many of the parameters differed significantly between normal subjects and patients with SSOH. Also, a large proportion of the eyes with SSOH were determined to be abnormal using the FSM discriminant function and MRA. It is important to distinguish this condition from glaucoma, because costly antiglaucoma medication is not warranted in the presence of SSOH, assuming that SSOH is a nonprogressive disease. Whereas a notch in the inferotemporal or superotemporal rim is commonly found in glaucoma, the rim area in the superonasal segment was found by this study to be most decreased in cases of SSOH. Our results may be generalized to cases of SSOH in general, because it is thought to be a nonprogressive disease and the degree of disease severity is not so variable as in glaucoma.Citation21,Citation24 There may be “subclinical” SSOH in which visual field testing does not detect any abnormality, while, in fact, nerve fibers are already reduced. HRT could be helpful in such cases.
The definition of SSOH remains to be determined. So far, different studies have used different criteria to define SOOH. We used diagnostic criteria based on a previous report.Citation10 However, the appearances of the optic discs of SSOH in this study appear to be somewhat different from those reported in Western countries. In general, the optic discs of SSOH in Japan often have a glaucoma-like cupping.Citation7,Citation8,Citation10 Although glaucoma has to be excluded in the initial diagnosis of SSOH, because the former is an acquired optic nerve disorder, the association between SSOH and glaucoma remains unclear. It is sometimes difficult to differentiate SSOH from glaucoma (especially from normal- tension glaucoma, in which the IOP is within normal limits) because the two share similar optic disc appearance features, such as a large cupping and a rim thinning.Citation10 Furthermore, glaucoma and SSOH do coexist in some cases. However, optic discs in the case reports from Western countries do not seem to show any general glaucoma-like cupping.Citation11 Additionally, SSOH is almost never associated with maternal diabetes mellitus in Japan. Thus, SSOH may be heterogeneous, and our conclusion may apply only to the specific type of SSOH that is typically found in Japan or Korea. However, superior nerve fiber layer defects and corresponding inferior visual field defects (either inferior altitudinal defects or inferior sector defects connected to the blind spot) are always observed in SSOH.
The visual fields in SSOH are shown to be stable over a 10-year periodCitation9 or an eight-year period,Citation10 but the long-term prognosis is not known, because no longer follow-ups have yet been reported. SSOH has been found in young patients, in whom glaucoma is less likely than in aged patients.Citation10 These findings seem to support the notion that SSOH is a congenital anomaly and does not progress. HRT could be used for the patients with SSOH over time to make sure that there is no progression of the disease.
Subjective qualitative techniques, such as ophthalmoscopy, are dependent on the examiner’s experience. However, only a few previous reports investigating SSOH have utilized objective quantitative imaging technologies of the optic disc.Citation7,Citation10,Citation11 Unoki et al used OCT to investigate the tomography of the optic disc and peripapillary retina in patients with SSOH.Citation7 Using OCT, obviously abnormal findings may be observed in patients in whom the optic disc shows only minimal changes, even in the fundus photograph.Citation7 Although both OCT and HRT can provide objective quantitative measurements of optic disc topography, the fundamental measurement principles of these two instruments are different. HRT is thought to be specifically useful for accurate structural assessments of the optic nerve head.Citation16,Citation19 A recent study utilizing OCT and HRT in SSOH generally supports our findings.Citation13
In this study, most eyes with SSOH were classified as abnormal, with a high specificity, using the FSM discriminant function and MRA. HRT generally requires a manual drawing of the contour line of the edge of the optic disc,Citation16,Citation19 and this process introduces an element of uncontrolled variability into the analysis because such contour lines, drawn by different observers, may vary considerably. The outlining of the disc margin is not necessary for GPS, and thus GPS is considered to be a more objective method than MRA.Citation18 While sensitivity and specificity values were found to be comparable between MRA and GPS in some reports,Citation20 the agreement between MRA and GPS is not necessarily high in defining glaucoma in other reports.Citation22 This study also shows that such an agreement is not high in SSOH either, probably reflecting the differences in the analysis algorithm. It is not surprising to find a rather low sensitivity for the GPS, because this is a diagnostic test designed specifically for glaucoma,Citation18 but not for SSOH. Alternatively, the GPS results in this study may have revealed that the GPS is not sensitive to the local rim-volume losses, which are shown by MRA, because of the influence of neighboring normal sectors.Citation20 Therefore, sectorial HRT-GPS analysis appears to have some limitations, although it has the clear merit that it is independent of the contour line traced manually by an examiner. Although it has been reported that both GPS and MRA are likely to produce many false-positive classifications in glaucoma,Citation20 high specificity values were obtained in SSOH. It has been reported that optic disc size influences the diagnostic accuracy of HRT in glaucoma, with small optic discs showing a lower sensitivity and a higher specificity compared with larger discs.Citation24 In this study, the disc area in SSOH was not statistically significantly different from that of the controls.
Since diagnostic tests for glaucoma using HRT frequently determine the SSOH to be abnormal, it will be necessary in a future study to develop a test which can reliably differentiate SSOH from glaucoma. From our results, it seems that HRT can discern the pattern of the area of rim losses between SSOH and glaucoma. Our results also indicate that HRT can be useful in identifying a reduction of the rim area, especially in the superonasal region, in patients with SSOH.
Disclosure
This research was presented at the World Glaucoma Congress in Boston, USA, July 8–11, 2009. The authors report no conflicts of interest in this work.
References
- GardnerHBIrvineAROptic nerve hypoplasia with good visual acuityArch Ophthalmol1972882552584340828
- PetersenRAWaltonDSOptic nerve hypoplasia with good visual acuity and visual field defects: A study of children of diabetic mothersArch Ophthalmol197795254258836211
- BjörkALaurellCGLaurellUBilateral optic nerve hypoplasia with normal visual acuityAm J Ophthalmol197886524529707598
- KimRYHoytWFLessellSSuperior segmental optic hypoplasia. A sign of maternal diabetesArch Ophthalmol1989107131213152783063
- LandauKBajkaJDKirchschlägerBMTopless optic disks in children of mothers with Type I diabetes mellitusAm J Ophthalmol19981256056119625543
- HashimotoMOhtsukaKNakagawaTTopless optic disk syndrome without maternal diabetes mellitusAm J Ophthalmol199912811111210482109
- UnokiKOhbaNHoytWFOptical coherence tomography of superior segmental optic hypoplasiaBr J Ophthalmol20028691091412140214
- YamamotoTSatoMIwaseASuperior segmental optic hypoplasia found in Tajimi Eye Health Care Project participantsJpn J Ophthalmol20044857858315592784
- HayashiKTomidokoroAAiharaMLong-term follow-up of superior segmental optic hypoplasiaJpn J Ophthalmol20085241241418991047
- TakagiMAbeHHataseTSuperior segmental optic nerve hypoplasia in youthJpn J Ophthalmol20085246847419089568
- AthappillyGPelakVSTeaching neuroimages: Superior segmental optic nerve hypoplasia confirmed by optical coherence tomographyNeurology200972e91e9219414718
- HanSBParkKHKimDMPrevalence of superior segmental optic nerve hypoplasia in KoreaJpn J Ophthalmol20095322522819484440
- LeeHJKeeCOptical coherence tomography and Heidelberg retina tomography for superior segmental optic hypoplasiaBr J Ophthalmol2009931468147319628499
- MikelbergFSParfittCMSwindaleNVAbility of the Heidelberg retina tomograph to detect early glaucomatous visual field lossJ Glaucoma1995424224719920681
- IesterMMikelbergFSDranceSMThe effect of optic disc size on diagnostic precision with the Heidelberg retina tomographOphthalmology19971045455489082287
- WollsteinGGarway-HeathDFHitchingsRAIdentification of early glaucoma cases with the scanning laser ophthalmoscopeOphthalmology1998105155715639709774
- Garway-HeathDFPoinoosawmyDWollsteinGInter- and intraobserver variation in the analysis of optic disc images: Comparison of the Heidelberg retina tomograph and computer assisted planimetryBr J Ophthalmol19998366466910340972
- SwindaleNVStjepanovicGChinAAutomated analysis of normal and glaucomatous optic nerve head topography imagesInvest Ophthalmol Vis Sci2000411730174210845593
- MigliorSGuareschiMAlbeEDetection of glaucomatous visual field changes using the Moorfields regression analysis of the Heidelberg retina tomographAm J Ophthalmol2003136263312834666
- CoopsAHensonDBKwartzAJAutomated analysis of Heidelberg retina tomograph optic disc images by glaucoma probability scoreInvest Ophthalmol Vis Sci2006475348535517122123
- MedeirosFAZangwillLMBowdCInfluence of disease severity and optic disc size on the diagnostic performance of imaging instruments in glaucomaInvest Ophthalmol Vis Sci2006471008101516505035
- Burgansky-EliashZWollsteinGBilonickRAGlaucoma detection with the Heidelberg retina tomograph 3Ophthalmology200711446647117141321
- ZangwillLMJainSRacetteLThe effect of disc size and severity of disease on the diagnostic accuracy of the Heidelberg retina tomograph glaucoma probability scoreInvest Ophthalmol Vis Sci2007482653266017525196
- FerrerasAPajarínAPoloVDiagnostic ability of Heidelberg retina tomograph 3 classifications. Glaucoma probability score versus Moorfields regression analysisOphthalmology20071141981198717445899
- FerrerasAPabloLEPajarínABDiagnostic ability of the Heidelberg retina tomograph 3 for glaucomaAm J Ophthalmol200814535435918078851
- FerrerasAPabloLELarrosaJMDiscriminating between normal and glaucoma-damaged eyes with the Heidelberg retina tomograph 3Ophthalmology200811577578117870171
- KassMAHeuerDKHigginbothamEJThe Ocular Hypertension Treatment Study: A randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open- angle glaucomaArch Ophthalmol200212070171312049574
- JohnsonCASamplePAZangwillLMStructure and function evaluation (SAFE): II. Comparison of optic disk and visual field characteristicsAm J Ophthalmol200313514815412566017