Abstract
Purpose:
To investigate the relationship between spectral domain optical coherence tomography (SD-OCT) findings and visual outcomes following resolution of macular edema in central retinal vein occlusion (CRVO).
Methods:
Patients with recent onset CRVO who had undergone SD-OCT and fluorescein angiography (FA) exams on the day of initial presentation were included. All patients had resolution of macular edema in SD-OCT images at the end of follow-up, and they were separated into two groups according to final visual acuity: group 1 (≤20/200) and group 2 (>20/200). SD-OCT scans and FA studies were analyzed in a masked fashion. Macular perfusion status by FA was categorized according to presence or absence of macular ischemia.
Results:
A total of 22 eyes from 22 patients [mean age 53.0 ± 15.0 (standard deviation)] were included. Mean follow up period was 14.6 ± 8.1 (standard deviation) months. Group 1 (10 eyes) had significantly higher rates of residual intraretinal fluid, loss of foveal inner segment/outer segment (IS/OS) junction line and loss of inner retinal layers in late stage SD-OCT images (P = 0.027) when compared with group 2 (12 eyes). Loss of foveal IS/OS junction line (odds ratio [OR] = 13.826; P = 0.098) and loss of inner retinal layers (OR = 38.908; P = 0.013) in late stage SD-OCT images were correlated with poorer final visual outcomes. Macular ischemia by FA correlated with thinner central subfield thickness (r = −0.54, P = 0.021) and loss of inner retinal layers (r = 0.47, P = 0.031) in early stage SD-OCT images; and presence of residual intraretinal fluid (r = 0.61, P = 0.003) and loss of inner retinal layers (r = 0.71, P < 0.001) in late stage SD-OCT images.
Conclusion:
Loss of foveal IS/OS junction line and inner retinal layers on SD-OCT significantly correlated with poorer visual outcomes in CRVO patients.
Introduction
Central retinal vein occlusion (CRVO) is a frequent retinal vascular disorder, often associated with severe visual loss.Citation1,Citation2 Macular edema is the most common vision-threatening complication associated with CRVO. Various options for treatment of macular edema secondary to CRVO have been studied, such as laser photocoagulation,Citation3 radial optic neurotomy,Citation4 and intravitreal injection of various agents including tissue plasminogen activator,Citation5 triamcinolone acetonide,Citation6 or anti-vascular endothelial growth factor agents.Citation7,Citation8 However, there is no proven remedy for visual loss due to CRVO.Citation9 Despite the observation that resolution of macular edema often leads to visual improvement, some patients suffer persistent poor vision following complete resolution of the macular edema.Citation10
Optical coherence tomography (OCT) is a noncontact, noninvasive method that allows quantitative determination of retinal thickness and volume. It provides cross-sectional slice images of the retina and useful information on vitreoretinal interface changes associated with various posterior segment disorders.Citation11–Citation13 Spectral domain OCT (SD-OCT) is the latest generation of the technology which provides images of higher axial resolution and reduced motion artifacts.Citation14–Citation16 It permits accurate identification of individual retinal layers with near-histological detail and provides significant clinicopathological information in many retinal conditions.Citation17,Citation18 A number of recent OCT studies have identified that continuity of the photoreceptor inner segment/outer segment (IS/OS) junction line in the fovea is a hallmark of foveal photoreceptor integrity, which is critical to visual outcome in eyes with disorders such as branch retinal vein occlusion (BRVO)Citation19–Citation21 and CRVO.Citation10 However, there is scant information in the literature unraveling the relationship between specific retinal structural changes recorded in SD-OCT images and visual outcomes in eyes with CRVO.
In the current study, we investigated whether early and late SD-OCT findings, such as loss of inner retinal layers and foveal IS/OS junction status, correlated with visual acuity following resolution of macular edema in patients with CRVO. Additionally, we looked at the relationship between macular perfusion revealed by fluorescein angiography (FA) and its association with those SD-OCT findings.
Methods
A retrospective chart review was conducted surveying the imaging database for patients with CRVO who underwent both SD-OCT and FA exam during initial clinical evaluation at the Retina Service of The New York Eye and Ear Infirmary, between September 2006 and September 2008. The study was approved by the Institutional Review Board of the New York Eye and Ear Infirmary.
Patients with CRVO, who presented within 1 month of onset of symptoms, were included in the study. Patients had to have at least 6 months of follow-up, and resolution of macular edema on clinical exam, and by the SD-OCT (central foveal thickness <250 μm) at the end of this period. Eyes with poor quality SD-OCT scans or FA images, or patients with macular edema caused by other etiologies such as diabetic retinopathy, postoperative or inflammatory cystoid macular edema, were excluded. In patients with bilateral CRVO, one eye was selected randomly to be included. Medical records of all eligible patients were reviewed, and demographics, systemic comorbidities, and treatments performed were recorded. Best corrected Snellen visual acuity measurements recorded during the initial visit and following resolution of macular edema were collected. Initial best corrected visual acuity (BCVA) was defined as that recorded during initial presentation to our service. Final BCVA was taken as the one recorded at follow-up examination after resolution of macular edema. Based upon the final BCVA, patients were separated into two groups: group 1 (BCVA ≤ 20/200) and group 2 (BCVA > 20/200).
The SD-OCT (Spectral OCT/SLO, OPKO/OTI, Miami, FL) device used in this study had transverse and axial resolutions of 20 and 5–6 μm, respectively. Individual cross-section images covered a field of 29° and came with a paired scanning laser ophthalmoscopy (SLO) image displaying the origin of the slice. Images considered acceptable in quality were evaluated by two masked retina specialists for evidence of predefined macular abnormalities and central retinal thickness. Integrity of the foveal photoreceptor layer was evaluated using high quality raw grayscale SD-OCT scans to determine the condition of the IS/OS junction line. Eyes were classified as having loss of the IS/OS junction when this line was totally absent in the fovea. In all patients, SD-OCT scans to evaluate macular thickness and to assess effectiveness of treatment during follow-up were performed until they met the satisfaction of the operator, an ophthalmologist with extensive imaging experience. Early stage and late stage SD-OCT findings refer to those macular changes recorded in the SD-OCT images taken during the initial visit and following resolution of macular edema, respectively.
FA assessment of macular ischemia was interpreted by one masked observer, and studies were separated into two categories, according to the presence or absence of macular ischemia. The patients with foveal avascular zones (FAZs) ≥1000 μm, or broken perifoveal capillary rings at the borders of the FAZ or distinct areas of capillary nonperfusion within one disk diameter of the foveal center, as judged in FA transit phase frames, were regarded as having macular ischemia.Citation22
Statistical analysis
Chi-square analysis was used for categorical data, and the independent sample student t-test was used for continuous data to determine whether significant differences appeared between groups 1 and 2. Fisher’s exact test was used when one or more of the cells in chi-square analysis had expected values below 5. All clinical manifestations, SD-OCT findings, and presence of macular ischemia on FA were submitted for analysis. A two-tailed P-value of <0.05 was considered statistically significant. Logistic regression model was used to evaluate the risk factors for poorer visual outcome (BCVA ≤ 20/200). Potential risk factors including age, initial visual acuity, and SD-OCT findings that showed differences which were statistically significant between groups were analyzed by backward stepwise regression. Factors with P-value >0.05 were removed from the equation. Spearman’s correlation coefficient was used to analyze the relationship between SD-OCT findings and macular ischemia by FA. All data were analyzed using SPSS Program Package Version 15.0 (SPSS Inc., Chicago, IL). Logistic regression power was calculated using PASS 2008 (NCSS, Kaysville, UT) software.
Results
Twenty-two patients (22 eyes) diagnosed with CRVO were included [9 female and 13 male; mean age of 53.0 ± 15.0 (standard deviation) years]. Co-morbidities included systemic arterial hypertension (45%), dyslipidemia (23%), type 2 diabetes mellitus (9%), and acquired immunodeficiency syndrome (4.5%). Treatment modalities used for macular edema included intravitreal injections of bevacizumab in 10 (45%) eyes and triamcinolone acetonide in four (18%) eyes. Multiple injections had been administered if required for resolution of the macular edema. Five eyes in group 2 had received no treatment for macular edema due to good vision at presentation. Peripheral panretinal photocoagulation was performed in 6 (27%) eyes. Two eyes developed neovascular glaucoma despite laser treatment. The mean follow-up period for all patients was 14.6 ± 8.1 (standard deviation) months (range, 7–42 months). Foveal thickness and central subfield thickness could not be determined on early stage SD-OCT in three patients due to severe macular edema beyond the range of the instrument (2.0 mm maximum depth). FA images of one patient were missing. This patient was excluded from the analysis of the relationship between the macular perfusion status and SD-OCT findings.
Among the 22 eyes included, 10 (45%) eyes had final BCVA ≤ 20/200 (group 1), and 12 (55%) eyes had final BCVA > 20/200 (group 2). summarizes clinical characteristics, SD-OCT findings, and macular perfusion status for each group. There were no statistically significant differences in age, gender, and initial visual acuity between groups. There were also no significant differences in foveal thickness and central subfield thickness between the two groups before and after resolution of macular edema. The main findings analyzed in the SD-OCT scans were retention of hyperreflectivity of the inner layers, presence of intraretinal fluid, presence of serous retinal detachment, loss of foveal IS/OS junction, and loss of inner retinal layers ( and ).
Figure 1 Fluorescein angiography (20.9 seconds) of one patient with recent onset central retinal vein occlusion in the right eye showing no evidence of ischemia in the macula (left). Gray-scale spectral domain optical coherence tomography (SD-OCT) horizontal scan at the initial visit (upper right) demonstrates prominent macular edema with cystoid spaces and serous retinal detachment under the fovea. The Snellen best corrected visual acuity was 20/200 at this point. This patient was treated with multiple intravitreal injections of bevacizumab. Gray-scale SD-OCT horizontal scan at the final visit (lower right) shows that macular edema has resolved completely. The inner segment/outer segment (IS/OS) junction can still be identified in the fovea, and there is a complete preservation of the inner retinal architecture. Visual acuity improved to 20/25 at final visit.
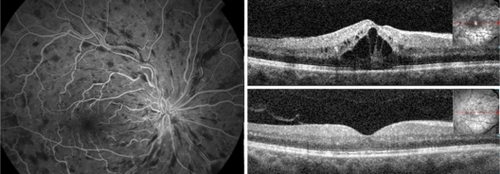
Figure 2 Fluorescein angiography (35.1 seconds) of another patient with recent onset central retinal vein occlusion in the right eye revealing ischemia in the macular area (left). Gray-scale spectral domain optical coherence tomography (SD-OCT) vertical scan at the initial visit (upper right) demonstrates the presence of a discrete amount of subretinal fluid under the fovea and loss of inner retinal layers. Visual acuity was counting fingers at this point. This patient was treated with an intravitreal injection of bevacizumab and panretinal photocoagulation. Gray-scale SD-OCT vertical scan at the final visit (lower right) shows resolution of subretinal fluid under the fovea. The inner segment/outer segment (IS/OS) cannot be identified in the fovea and there is loss of the normal inner retina architecture. Visual acuity was 20/400 at final visit.
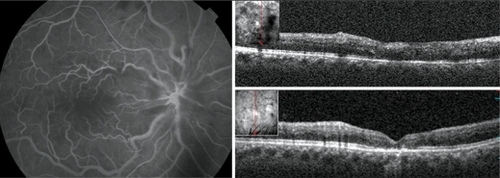
Table 1 Demographic and clinical characteristics of each group of patients with central retinal vein occlusion
Statistical analysis showed that eyes in group 1 had higher rates of residual intraretinal fluid (P = 0.027), loss of foveal IS/OS junction (P = 0.020) and loss of inner retinal layers (P = 0.002) in late stage SD-OCT images compared with those in group 2. To determine the risk factors for poorer visual outcome (BCVA ≤ 20/200), the SD-OCT findings described above, along with age and initial visual acuity, were analyzed using a logistic regression model. Among all findings analyzed, loss of foveal IS/OS junction line (odds ratio [OR] = 13.826; P = 0.098; 95% confidence interval [CI]: 0.616–310.321) and loss of inner retinal layers (OR = 38.908; P = 0.013; 95% CI: 2.169–698.087) in late stage SD-OCT images correlated with poorer visual outcomes. The power of this logistic regression model was 0.703.
Group 1 had more eyes with macular ischemia by FA at initial presentation when compared with group 2 (P = 0.009). summarizes the SD-OCT findings in eyes with and without macular ischemia by FA. Macular ischemia by FA showed significant correlation with the following SD-OCT findings: thinner central subfield thickness (r = −0.54, P = 0.021) and loss of inner retinal layers (r = 0.47, P = 0.031) in early stage SD-OCT images; and presence of residual intraretinal fluid (r = 0.61, P = 0.003) and loss of inner retinal layers (r = 0.71, P < 0.001) in late stage SD-OCT images.
Table 2 Comparison between eyes with and without macular ischemia on FA
Discussion
In this study we found that loss of foveal IS/OS junction line and absence of inner retinal layers in late stage SD-OCT images were significantly correlated with poor visual outcomes in patients with CRVO. Additionally, loss of inner retinal layers in late stage SD-OCT images correlated significantly with macular ischemia diagnosed in early FA studies.
Currently, agents such as intravitreal triamcinolone acetonide or bevacizumab have been shown to be effective for reducing the macular edema associated with CRVO.Citation6–Citation8 In most cases, reduction of macular edema is associated with visual acuity improvement. However, only some patients are able to achieve full recovery of vision following resolution of macular edema, and others experience only limited visual improvement despite “successful” treatment. In fact, the relationship between central retinal thickness and visual acuity has not been well established in cases of CRVO. Scott et alCitation23 demonstrated that the correlation between OCT-measured center point thickness, and visual acuity letter score was statistically significant, but this relationship was, at best, modest in patients with macular edema associated with retinal vein occlusions. In our study, there was a trend, though not significant statistically, for patients with poorer visual outcomes to have had thinner mean foveal thickness and central subfield thickness in both early and late stage SD-OCT imaging when compared with patients achieving better visual outcomes. More importantly, macular ischemia by FA was significantly correlated with thinner central subfield thickness in early stage SD-OCT images. This appeared to go along with atrophic changes in the retina of those patients due to the macular ischemia. Thus, macular thickness alone, in this study, did not appear to be a good predictor of visual outcome in patients with CRVO.
According to histologic reports of eyes with retinal vein occlusions, edema appears at the level of the outer nuclear layer and is associated with liquefaction necrosis which may result in photoreceptor loss and contribute to foveal dysfunction.Citation24 Previous studies using earlier third-generation time domain OCT devices found that IS/OS junction integrity at the fovea was closely associated with visual acuity in eyes with BRVOCitation19–Citation21 and CRVO.Citation10 Most of these studies evaluated the status of the IS/OS junction line following resolution of macular edema as a possible hallmark of integrity of the photoreceptors layer and predictor of function. In the current study, using a faster and higher resolution SD-OCT device, which provided better visualization of the IS/OS junction, we were additionally able to resolve concurrent loss of inner retinal layers, which correlated with poor visual outcomes in these CRVO eyes.
The ability of SD-OCT technology to differentiate changes in individual retinal layers allowed us to correlate poorer visual outcome specifically to loss of inner retinal layers. This goes along with the pathophysiology of CRVO which has its greatest impact on the circulation of the inner retinal layers. Histopathological studies of areas of capillary nonperfusion following retinal vein occlusion have revealed the presence of inner ischemic atrophy with loss of inner plexiform and inner nuclear layers.Citation25–Citation27 These are consistent with the SD-OCT appearance of inner retinal architecture disappearance in patients with more severe macular ischemia and limited visual recovery. It also agrees with the statistically significant correlation between the finding of macular ischemia by FA and the loss of inner retinal layers on SD-OCT.
It is still unclear at what point these retinal structural changes occur in the course of CRVO. We were unable to demonstrate any difference in early stage SD-OCT image findings between groups 1 and 2. This suggests that some time interval is required before structural changes such as loss of IS/OS junction line and loss of inner retinal layers occur. In addition, during acute stages of the disease, visualization of the retinal morphology is often impaired due to scattering blur produced by intraretinal fluid and shadow artifacts caused by hemorrhage. These limitations mirror the difficulties diagnosing macular ischemia by FA in very hemorrhagic occlusions. Given the complementary nature of the information received from the two studies, its clear that SD-OCT and FA exams together provide a more complete clinical assessment for management of patients with CRVO.
In previous reports, initial visual acuity was often found to be the most reliable prognostic factor for predicting visual prognosis in eyes with CRVO.Citation1,Citation2,Citation28 It is, however, occasionally misleading due to transient macular edema or intraretinal hemorrhage. In our study, we similarly found that patients with poorer initial visual acuity were more likely to have worse long-term visual outcomes, but the correlation was not statistically significant, perhaps due to our small sample size.
Using multiple regression analysis, loss of the foveal IS/OS junction line and loss of inner retinal layers came up as risk factors for poorer visual outcome. Macular ischemia was not included in this particular regression model because it was highly correlated with loss of inner retinal layers. Given that our purpose was to focus on SD-OCT abnormal findings in relation to CRVO visual outcomes, we chose inner retinal layer loss instead of macular ischemia by FA to include in the regression analysis.
There were certain limitations to our study. First, it is based upon a relatively small sample size. Second, it is a retrospective chart review. And finally, it included patients treated with a variety of treatment modalities including intravitreal injections of bevacizumab and triamcinolone and panretinal photocoagulation. A small number of patients (5 eyes) did not receive any kind of treatment, and all of them were in group 2. Each of these courses of management could potentially influence visual outcome to different extents. However, at the point of analysis, all patients were free of edema both clinically and by SD-OCT exam.
In summary, loss of the foveal IS/OS junction line and loss of inner retinal layers in late stage SD-OCT images in eyes with CRVO significantly correlated with poorer visual outcomes. In addition, the absence of inner retinal layers strongly correlated with the finding macular ischemia by FA. This suggests that SD-OCT can be an important tool both for the evaluation and management of macular edema as well as helping to predict long-term visual prognosis in patients with CRVO, based on these specific structural changes. Judgment as to whether SD-OCT structural predictions are better than current clinical assessments must be reserved pending larger prospective trials.
Acknowledgements
Tseng Hsiao-Jung, Biostatistical Center for Clinical Research, Chang Gung Memorial Hospital, Taoyuan, Taiwan.
Disclosure
Dr Richard B Rosen is a member of the Scientific Advisory Boards of OTI-OPKO, OD-OS and Clarity Medical.
References
- The Central Vein Occlusion Study GroupNatural history and clinical management of central retinal vein occlusionArch Ophthalmol19971154864919109757
- Glacet-BernardACoscasGChabanelAZourdaniALelongFSamamaMMPrognostic factors for retinal vein occlusion: prospective study of 175 casesOphthalmology19961035515608618752
- The Central Vein Occlusion Study GroupEvaluation of grid pattern photocoagulation for macular edema in central vein occlusion. M reportOphthalmology1995102142514339097788
- BinderSAggermannTBrunnerSLong-term effects of radial optic neurotomy for central retinal vein occlusion consecutive interventional case seriesGraefes Arch Clin Exp Ophthalmol20072451447145217406885
- GhaziNGNoureddineBHaddadRSJurdiFABashshurZFIntravitreal tissue plasminogen activator in the management of central retinal vein occlusionRetina20032378078414707827
- GoffMJJumperJMYangSSIntravitreal triamcinolone acetonide treatment of macular edema associated with central retinal vein occlusionRetina20062689690117031289
- IturraldeDSpaideRFMeyerleCBIntravitreal bevacizumab (Avastin) treatment of macular edema in central retinal vein occlusion: a short-term studyRetina20062627928416508427
- PaiSAShettyRVijayanPBClinical, anatomic, and electrophysiologic evaluation following intravitreal bevacizumab for macular edema in retinal vein occlusionAm J Ophthalmol200714360160617306753
- MohamedQMcIntoshRLSawSMWongTYInterventions for central retinal vein occlusion: an evidence-based systematic reviewOphthalmology200711450751917324695
- OtaMTsujikawaAKitaMIntegrity of foveal photoreceptor layer in central retinal vein occlusionRetina2008281502150818997611
- HuangDSwansonEALinCPOptical coherence tomographyScience1991254117811811957169
- HeeMRIzattJASwansonEAOptical coherence tomography of the human retinaArch Ophthalmol19951133253327887846
- PuliafitoCAHeeMRLinCPImaging of macular diseases with optical coherence tomographyOphthalmology19951022172297862410
- DrexlerWUltrahigh-resolution optical coherence tomographyJ Biomed Opt20049477414715057
- NassifNCenseBParkBHIn vivo human retinal imaging by ultrahigh-speed spectral domain optical coherence tomographyOpt Lett20042948048215005199
- PodoleanuAGRosenRBCombinations of techniques in imaging the retina with high resolutionProg Retin Eye Res20082746449918495519
- SrinivasanVJWojtkowskiMWitkinAJHigh-definition and 3-dimensional imaging of macular pathologies with high-speed ultrahigh-resolution optical coherence tomographyOphthalmology20061132054206517074565
- SakamotoAHangaiMYoshimuraNSpectral-domain optical coherence tomography with multiple B-scan averaging for enhanced imaging of retinal diseasesOphthalmology20081151071107818061270
- MurakamiTTsujikawaAOhtaMPhotoreceptor status after resolved macular edema in branch retinal vein occlusion treated with tissue plasminogen activatorAm J Ophthalmol200714317117317188062
- OtaMTsujikawaAMurakamiTAssociation between integrity of foveal photoreceptor layer and visual acuity in branch retinal vein occlusionBr J Ophthalmol2007911644164917504858
- OtaMTsujikawaAMurakamiTFoveal photoreceptor layer in eyes with persistent cystoid macular edema associated with branch retinal vein occlusionAm J Ophthalmol200814527328018045566
- ChungEJRohMIKwonOWKohHJEffects of macular ischemia on the outcome of intravitreal bevacizumab therapy for diabetic macular edemaRetina20082895796318698297
- ScottIUVanVeldhuisenPCOdenNLSCORE Study Investigator Group. SCORE Study report 1: baseline associations between central retinal thickness and visual acuity in patients with retinal vein occlusionOphthalmology200911650451219167078
- TsoMOPathology of cystoid macular edemaOphthalmology1982899029157133637
- BowersDKFinkelsteinDWolffSMGreenWRBranch retinal vein occlusion. A clinicopathologic case reportRetina198772522592448855
- FrangiehGTGreenWRBarraquer-SomersEFinkelsteinDHistopathologic study of nine branch retinal vein occlusionsArch Ophthalmol1982100113211406178389
- GreenWRChanCCHutchinsGMTerryJMCentral retinal vein occlusion: a prospective histopathologic study of 29 eyes in 28 casesRetina19811275515633406
- The Central Vein Occlusion Study GroupBaseline and early natural history report: the Central Vein Occlusion StudyArch Ophthalmol1993111108710957688950