Abstract
A 61-year-old man presented to the ophthalmology department having developed bilateral branch retinal vein occlusions. Baseline blood tests revealed no abnormality; however, subsequent investigations showed a raised plasma homocysteine (HC) level. The patient has been treated for refractory epilepsy for a number of years. Although antiepileptic medications have been shown to reduce folate levels and result in a raised HC level, this has not previously been shown to be to a level causing a retinal vascular event.
Keywords:
Introduction
Retinal vein occlusions are the second most common retinal vascular disease following diabetic retinopathy. A combination of hypertensive, atherosclerotic, inflammatory, or thrombophilic conditions may lead to retinal endothelial vascular damage. Hyperhomocysteinemia has been implicated as an independent risk factor for systemic vascular events, including retinal vascular disease. We present a case demonstrating the potential biochemical implications of antiepileptic agents and discuss their role in retinal vascular events.
Case history
A 61-year-old man was referred to the ophthalmology clinic by his optician for fundal changes noted at a routine eye examination. He was completely visually asymptomatic, with no past ocular history of note. His medical history included epilepsy, which had been difficult to control, for which he took phenytoin, topiramate, and pregabalin. There was no history of diabetes, hypertension, or cardiovascular disease, nor any family history of note. He smoked occasionally and drank little alcohol.
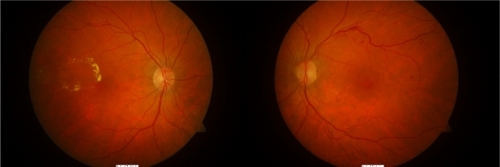
On examination, his visual acuity was 6/4 (20/13) in the right eye and 6/5 (20/15) in the left eye; anterior segment examination was normal with intraocular pressures within the normal range. Dilated fundal examination revealed right macular exudates and subretinal fluid, suggestive of a branch retinal vein occlusion (BRVO). In the left eye he demonstrated a few scattered retinal hemorrhages along the superotemporal arcade ().
Figure 1 Color fundal photos demonstrating signs of branch vein occlusions in both left and right eyes.
The patient’s blood pressure was normal (117/70 mm Hg). He underwent a series of blood tests, revealing a normal full blood count, electrolytes, cholesterol, lipids and triglycerides, fasting glucose, autoantibodies, C3, C4, immunoglobulins, and thrombophilia screen. His only abnormality detected was a high serum homocysteine (HC) level (20 umol/L). He was started on folate therapy, as this was considered the most likely cause of his raised HC level secondary to his antiepileptic medication but was subsequently discontinued as he noticed an increase in his seizure rate.
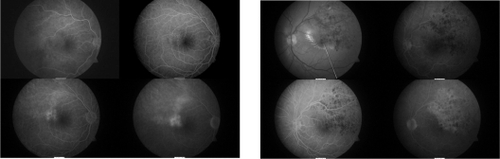
At his review appointment 2 months later, the patient reported a deterioration in the vision in his left eye; examination revealed a visual acuity of 6/24 (20/80), extensive retinal hemorrhages along the superotemporal arcade, and diffuse macular edema. The visual acuity in the right eye remained satisfactory at 6/9 (20/30). His fluorescein angiogram revealed a right superotemporal BRVO with evidence of some macular edema and leakage; the left eye showed evidence of a superotemporal BRVO with extensive retinal hemorrhages and some late leakage around the macular region ().
Figure 2 Fluorescein angiograms demonstrating bilateral branch vein occlusions with left macular edema.
The patient underwent argon macular grid laser therapy to his left eye, which improved his acuity to 6/12 (20/40). He continues to be monitored.
Discussion
Antiepileptic drugs (AEDs) have been shown to be related to atherosclerosis and vascular risk.Citation1 Even in children utilizing AEDs, cytochrome P450 liver enzyme-inducing agents such as carbamezapine, phenytoin, and phenobarbital have caused rises in cholesterol, triglycerides, and low-density lipoprotein levels. The effects may be reversible, as switching to alternative AEDs such as levetiracem or lamotrigine has been shown to correct such biochemical abnormalities.Citation2
The role of plasma HC has been suggested. The use of AEDs such as carbamezapine and sodium valproate have been shown to cause an increase in plasma HC levels,Citation3 most likely due to disruption of folate metabolism. HC itself is well known to be an independent risk factor for vascular events.Citation4 The mechanism of action remains uncertain, but suggestions include oxidative damage of endothelial cells, dysregulation of endothelial function due to endothelial nitric oxide synthase impairment, promotion of endothelial thrombotic functions such as platelet activation, and inflammatory processes.Citation1 The relationship between HC and retinal vascular occlusion has also been well documented, both for central retinal vein occlusionsCitation5–Citation9 and for branch vein occlusions.Citation10,Citation11 Although the false-positive rate for raised serum HC is approximately 5%, making the test unsuitable for screening purposes, the dose-dependent relationship between HC levels and risk of cardiovascular disease is a factor not to be taken lightly in individuals who have had a vascular event.Citation12
Cardiovascular events, including retinal vascular diseases, have a multifactorial causality, combining both occlusive and inflammatory parameters. This case demonstrates a potential causal factor involved that is often overlooked. Although HC levels have been related to AEDs, and raised plasma HC has been linked to vascular events, this is the first report of bilateral branch vein occlusion in a patient utilizing such antiepileptic agents. The potential risks of these AEDs ought to be respected and remembered when considering the choice of agents in patients, both young and old, when managing their seizures.
Disclosure
The authors report no conflicts of interest in this work.
References
- JakubusTMichalska-JakubusMLukawskiKAtherosclerotic risk among children taking antiepileptic drugsPharmacol Rep20096141142319605940
- MintzerSSkidmoreCAbidinCEffects of antiepileptic drugs on lipids, homocysteine, and C-reactive proteinAnn Neurol20096544845619296463
- AslanKBozdemirHUnsalCGuvencBThe effect of antiepileptic drugs on vitamin B12 metabolismInt J Lab Hematol200730263518190464
- KaplanEDAssociation between homocyst(e)ine levels and risk of vascular eventsDrugs Today (Barc)20033917519212730702
- NarayanasamyASubramaniamBKarunakaranCHyperhomocysteinemia and low methionine stress are risk factors for central retinal venous occlusion in an Indian populationInvest Ophthalmol Vis Sci2007481441144617389469
- MarcucciRBertiniLGiustiBThrombophilic risk factors in patients with central retinal vein occlusionThromb Haemost20018677277611583306
- LaheyMTunçMKearneyJLaboratory evaluation of hypercoagulable states in patients with central retinal vein occlusion who are less than 56 years of ageOphthalmology200210912613111772591
- MoghimiSNajmiZFaghihiHHyperhomocysteinemia and central retinal vein occlusion in Iranian populationInt Ophthalmol200828232817636432
- GaoWWangYZhangPWangHHyperhomocysteinemia and low plasma folate as risk factors for central retinal vein occlusion: a case–control study in a Chinese populationGraefes Arch Clin Exp Ophthalmol20062441246124916538453
- SalaunNDelyferM-NRougierM-BKorobelnikJ-FÉvaluation du bilan étiologique des occlusions veineuses rétiniennes du sujet âgé de moins de 60 ansJ Fr Ophtalmol20073091892318046276
- WegerMStangerODeutschmannHHyperhomocyst(e)inemia, but not methylenetetrahydrofolate reductase C677T mutation, as a risk factor in branch retinal vein occlusionOphthalmology20021091105111912045051
- WaldDSLawMMorrisJKThe dose-response relation between serum homocysteine and cardiovascular disease: implications for treatment and screeningEur J Cardiovasc Prev Rehabil20041125025315179109