Abstract
Macular edema (ME) is the most common sight-threatening complication in uveitis. The diagnostic and therapeutic management of the uveitic macular edema (UME) might be challenging due to the complex diagnostic workup and the difficulties physicians face to find the underlying cause, and due to its usually recurrent nature and the fact that it can be refractory to conventional treatment. Some of the mild cases can be treated with topical steroids, which can be combined with non-steroid anti-inflammatory drugs. However, immunomodulators such as methotrexate, tacrolimus, azathioprine, cyclosporine and mycophenolate mofetil together with anti-tumor necrosis factor-α (anti-TNF alpha) monoclonal antibodies such as adalimumab and infliximab, may be required to control the inflammation and the associated ME in refractory cases, or when an underlying disease is present. This review of the literature will focus mostly on the non-infectious UME.
Introduction
Uveitis is the inflammation of the uveal tract, the vascular layer between the sclera and the neuroretina, which can lead to significant visual impairment. Uveal tract consists posteriorly of the choroid, in the middle part of the ciliary body and anteriorly of the iris.
The retina has a double blood supply and each one has a blood-retinal barrier. Choroidal vasculature covers 80% of eye’s blood supply. The inner blood-retina barrier (BRB) is formed by tight junctions between adjacent endothelial cells and the outer BRB by tight junctions between the retinal pigment epithelium (RPE) cells (tight junction proteins include zonula occludens, occludins and VE-cadherins). The outer BRB is essential for maintaining the integrity of the retina and is the one responsible for removal of the metabolic wastes and transportation of nutrients, water and ions. It also separates the neuroretina from the fenestrated choriocapillaris.Citation1
Inflammation to any of the uveal tract structure is called uveitis. Uveitis can be classified further into anterior, intermediate, posterior and panuveitis according to the primary location of the inflammation. The most common form of intraocular inflammation is anterior uveitis (AU), followed by posterior uveitis and panuveitis, while intermediate uveitis is the least common.Citation2,Citation3 Classification of uveitis following the International Uveitis Study Group classification system (SUN)Citation4–Citation6 is depicted in and .
Table 1 Anatomic Classification of uveitis following the International Uveitis Study Group classification system (SUN*).
Table 2 The SUN* Working Group Descriptors of Uveitis.
Pathophysiology of uveitic macular edema (UME)
The main cause leading to the UME is the breakdown of either inner either outer or both BRBs and is a consequence of chronic inflammation. Extracellular fluid is accumulated either in the intraretinal or the subretinal space.Citation7 A UME might complicate an anterior, intermediate or a posterior uveitis.
The UME can be found in the outer nuclear layer or extend more superficially or deep before resulting to affect all retinal layers, and might even present in the form of a serous retinal detachment due to an RPE dysfunction.Citation8,Citation9 In all cases, it appears to result from the sum-up of cytotoxic and vasogenic effects due to the immunological aggression.Citation10
UME occurs when there is compromised equilibrium of water influx and efflux as a result of the inflammation and the overwhelming of compensatory mechanisms. A breach in the BRB will lead to a vasogenic edema due to the increase of oncotic pressure. Sometimes a dysfunction of the RPE pump and transmembrane ionic channels (Na+, K+, Cl-, HCO3-) and aquaporin 1 (AQP1) might be the cause; in this case no evidential leak is visible on the fluorescein angiography but a serous retinal detachment might exist.Citation11,Citation12 Different therapeutic strategies and pathophysiology implicate in the acute phase of inflammation and chronic stages where atrophy and fibrosis occur.Citation13 The inner BRB breakdown can be triggered by many factors, including vascular endothelial growth factor (VEGF), TNF-a, TGF-β, IL-1, angiotensin II (pro-inflammatory cytokines), adenosine, histamine and glucose. The VEGF is a protein greatly produced by Müller cells and cells that promote neovascularization and causes degradation of tight junction proteins by intracellular phosphorylations.Citation14,Citation15
Müller cells are the most important macroglial cells and their role is to ensure the homeostasis of the retinal extracellular milieu, facilitating the transfer of nutrients and evacuating metabolic by-products.Citation16 They ensure structural integrity and provide a link between neural elements and the vascular network. Müller cells consist also an important source of pigment epithelium-derived factor, contributing in the regulation of retinal angiogenesis. In conditions of stress, Müller cells secrete significant amounts of VEGF, which result in an increase in vascular permeability and neovascularization.Citation16 In the presence of inflammation, Müller cells swell, resulting in the formation of edema. This swelling has also been observed in inflammatory ME after surgery and is presumably derived by the presence of arachidonic acid and prostaglandin E2.Citation17,Citation18 The overall synthesis of potassium-rectifying channels (Kir) decreases also in the presence of inflammation. These functional alterations in Müller cells lead to the formation of cytotoxic ME and favor the formation of intracellular edema and accumulation of subretinal fluid, both characteristics of UME.Citation19 This edema lacks leakage on the angiogram despite manifest edema on the optical coherence tomography (OCT) and is more commonly observed in older individuals, probably because there is a progressive loss of Kir channels with age and Müller cells are less able to excrete water and potassium ions.Citation9
In inflammatory conditions, a vasogenic component coexists. Activated Müller cells and microglial cells synthesize VEGF together with pro-inflammatory cytokines and metalloproteases (such MMP-9) that lead to phosphorylation of occludin and VE-cadherin resulting in losing the integrity of the BRB, as desmosomes between capillary endothelial cells and between the cells of RPE are lost.Citation13
The outer BRB is important for maintaining the adhesion between the RPE and photoreceptors. This is achieved by mechanisms of active transportation from trans-epithelial space to the extraretinal space. Inflammatory conditions that involve the choriocapillaris, choroid and sclera could damage the outer BRB and despite the healthy retinal capillary endothelium, a macular edema (ME) might occur.Citation20,Citation21
In uveitic ocular inflammation despite the inflammatory UME, other causes may increase also the macular thickness, such as:
Inflammatory choroidal neovascularization
Inflammatory epiretinal membrane (ERM) formation with associated vitreomacular traction
Central serous chorioretinopathy exacerbated by steroid therapy
Contiguity with papillary swelling.
Etiology of non-infectious UME
Non-infectious known causes of UME are:
HLA-B27 positive uveitis (HLA-B27 associated diseases, including psoriasis, ankylosing spondylitis, inflammatory bowel disease, and reactive arthritis). A chronic AU, intermediate uveitis, a combination of anterior and intermediate uveitis may occur. AU can be also associated with hypopyon.Citation22
Juvenile idiopathic arthritis (JIA). The most common form of uveitis is chronic AU, which is almost always asymptomatic in the initial stages. However, it can be sight-threatening due to complications, such as glaucoma, cataract, band keratopathy and UME.Citation23
Sarcoidosis. Sarcoidosis-related uveitis is often bilateral and associated with numerous, whitish irregularly scattered granulomatous retinal and choroidal lesions.Citation24
Multiple sclerosis (MS). MS patients have ten times higher prevalence of intermediate uveitis which is often associated with retinal vasculitis.Citation25
Pars-planitis. An idiopathic chronic intermediate uveitis which can be associated with AU and retinal vasculitis.Citation26
Adamantiades–Behçet’s disease. Uveitis is bilateral, often no simultaneous and no granulomatous with coexisting focal or multiple retinal lesions.Citation27
Irvine–Gass syndrome and any postoperative ME. Even though the postoperative ME is not considered a typical UME, it should be included in the differential diagnosis of non-infectious UME as most of the time it is related with postoperative inflammation and uveitis.Citation28 Onset is 4–12 weeks with a peak at 4–6 weeks postoperatively. Patients’ typical symptom is deterioration of vision after an initial period of improvement following surgery.Citation29
Uveitis-glaucoma-hyphema syndrome is caused by mechanical trauma due to malpositioned intraocular lens over adjacent structures (iris, ciliary body, iridocorneal angle) and can lead to chronic inflammation, secondary iris neovascularization and ME.Citation30
Drug-induced (or medically induced) uveitis. A number of medications; topical (metipranolol, glucocorticosteroids, brimonidine and prostaglandin analogs), periocular, intraocular (cidofovir, anti-VEGF agents [ranibizumab, bevacizumab, aflibercept] and triamcinolone acetonide), systemic (cidofovir, rifabutin, bisphosphonates, sulfonamides, tumor necrosis factor inhibitors [TNF-a], oral fluoroquinolones and diethylacarbamazine) and vaccines (bacille Calmette–Guérin, measles, mumps and rubella, hepatitis B and varicella) have been associated with uveitis. Mechanisms underlying drug-induced uveitis are unclear but it is suggested that both toxic and inflammatory reactions play a role.Citation31,Citation32
Other collagen diseases including systemic lupus erythematosus (SLE), scleroderma, relapsing polychondritis, necrotizing vasculitis, granulomatosis with polyangiitis (GPA) (formerly known as Wegener’s disease), rheumatoid arthritis, polyarthritis. Non-granulomatous mild AU may occur in SLE patients. However, severe sight-threatening retinal vasculitis with macular involvement is more frequent.Citation33
Birdshot chorioretinopathy (BCR). BCR is strongly associated with HLA-A29 allele and it is believed to be T-cell driven. Typical manifestations include bilateral non- granulomatous uveitis with deep peripapillary or diffuse hypopigmented characteristic multiple cream-colored, irregular choroidal lesions.Citation34
Sympathetic ophthalmia. It is a rare entity, typically presented as a bilateral, granulomatous panuveitis that occurs after surgery or ocular trauma to one eye threatening vision in the other eye.Citation35
Intraocular tumor: primary non-hodgkin oculo-cerebral lymphoma. Typically, it presents as a chronic posterior uveitis with small whitish choroidal lesions, which is the most common masquerade. AU is unusual.Citation36
Vogt–Koyanagi–Harada (VKH) disease. Ocular findings include severe bilateral, chronic granulomatous panuveitis with serous retinal detachment, optic disc swelling and hyalitis.Citation37
Idiopathic uveitis. No cause/extraocular disease is identified.
ME is the main reason for visual loss in patients with uveitis, causing a visual acuity (VA) drop below 20/40 in about 30% of patients with posterior uveitis. VA deteriorates in 45% of the patients with posterior uveitis, in 64% of panuveitis and 28% of intermediate uveitis of which the 28%, 59% and 85%, respectively, were complicated with ME. UME is more frequently found in panuveitis with an incidence of 66%.Citation38
The systemic diseases associated with a poor visual prognosis are juvenile chronic arthritis and sarcoidosis.Citation38
Epidemiology and prevalence of uveitis and UME
Most of the epidemiological data of uveitis have been studied in the developed world.Citation39
The incidence and prevalence of uveitis is between 0.017–0.052% and 0.038–0.714%, respectively, in the population per year.Citation2,Citation3,Citation40,Citation41
Epidemiology changes with geographic location. AU prevalence is low in South Africa, posterior uveitis is more common in Africa, panuveitis is more common in Japan and in India panuveitis is more frequent than posterior uveitis.Citation42–Citation45
The prevalence of non-infectious uveitis has not been thoroughly studied separately from the prevalence of infectious uveitis. A recent original investigation carried out in the US made an effort to study the prevalence of non-infectious uveitis standalone.Citation46 This study reports that non-infectious uveitis affected an estimated 298,801 adults (estimated prevalence 121/100,000) and 21,879 children (estimated prevalence 29/100,000) in the United States in 2015. AU prevalence was 98/100,000 representing the 81% of all non-infectious uveitis cases, followed by non-infectious panuveitis (prevalence 12/100,000), posterior uveitis (prevalence 10/100,000) and intermediate uveitis (prevalence 1/100,000). A smaller study of 927 patients in France studying severe sight-threatening uveitis found that 68% of the cases were non-infectious.Citation47 However, this sample is not representative as it covers only severe cases.
The prevalence mentioned below is the total prevalence of uveitis recorded, unless stated otherwise.
Anterior uveitis
The most common uveitis is AU with prevalence up to 90% of all the cases of uveitis in primary care and 50–60% in tertiary centers. HLA-B27 AU is the most common type of non-infectious uveitis in most of the developed countries (except Japan and Italy).Citation48–Citation50
AU is less frequent in areas with low prevalence of HLA-B27 such as India, South Africa, Japan and Korea.Citation42,Citation51,Citation52
Seronegative spondyloarthropathies (ankylosing spondylitis, psoriatic arthritis, reactive arthritis and Reiter syndrome) are the most usual underlying cause of AU with a prevalence of 5% of all uveitis and 8–12% of acute AU.Citation52–Citation57
Analyzing further, the prevalence of uveitis in systemic autoimmune diseases: 2–9% of patients with inflammatory bowel disease, 7–16% of patients with psoriatic arthritis, 12–37% of patients with reactive arthritis and 20–40% of patients with ankylosing spondylitis will develop AU.Citation48
ME is less common in AU compared to patients with intermediate uveitis, posterior uveitis or panuveitis.Citation15,Citation58,Citation59 Approximately, 11% of patients with isolated AU and 60% of patients with JIA-associated uveitis will develop ME.Citation60,Citation61 The frequency of ME in patients with AU fluctuates between 9% and 28%.Citation38,Citation61–Citation63
Intermediate uveitis
Intermediate uveitis is the least common type of uveitis (15% of all types).Citation64 In most cases of intermediate uveitis, there is no underlying cause identified and they are classified as idiopathic (60–100%). Non-infectious diseases that cause intermediate uveitis include sarcoidosis, MS and intraocular lymphoma (masquerade syndrome).Citation65,Citation66 Despite the fact that intermediate uveitis is the least common type of uveitis, it is the form with the highest frequency of ME, fluctuating between 25% and 70%.Citation38,Citation61–Citation63
Posterior uveitis
It is the second most common uveitis (15–30% of all cases).Citation64 Non-infectious common etiologic factors include sarcoidosis, VKH disease and BCR.Citation43 Sarcoidosis is responsible for 1–13% of uveitis cases in Western World.Citation65,Citation67
According to previous studies, ME rate in posterior uveitis is 19–34%.Citation38,Citation61–Citation63
Panuveitis
The prevalence of panuveitis is greatly variable between geographic locations. It is less common in Europe and the USA and more frequent in Asia, Africa and South America.Citation52,Citation68,Citation69 Japan has a high prevalence of panuveitis due to VKH, Adamantiades–Behçet disease and sarcoidosis.Citation70 VKH panuveitis is rare in Europe with a prevalence of 0–3% and more common in Asia with a prevalence of 11–29%. Adamantiades–Behçet panuveitis has a higher prevalence in Asia and the Mediterranean region (15% in Portugal and 18% in Italy).Citation51
The rate of ME in patients with panuveitis is 18–66%.Citation38,Citation61–Citation63
ME in non-infectious uveitis
In non-infectious uveitis, ME is the most common complication, as it occurs in 8.3% of patients, followed by epiretinal membrane and glaucoma (6.3% and 4.2%, respectively).Citation71
ME in HLA-B27 uveitis ranges between 2% and 32% of cases.Citation72–Citation77 According to a recent study from Turkey, ME in ankylosing spondylitis occurs in about 17.5% of patients and is more frequent in males than in females (18.9% vs 14.3%, respectively),Citation78 while the rate of ME in JIA uveitis is 60%.Citation60,Citation61,Citation79
ME in patients with intermediate uveitis occurs in 60% of cases approximately.Citation61,Citation80–Citation83 The rate of ME in sarcoidosis is 27.3%, while in patients with Admantiades–Behçet’s disease it ranges from 15% to 63%.Citation61,Citation84–Citation86 On the other hand, in BCR uveitis, ME rate is 100%.Citation61
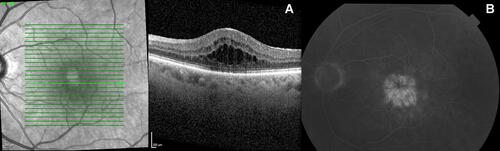
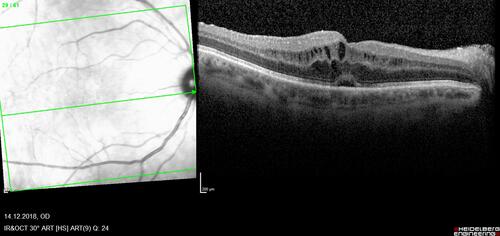
Diagnostic imaging in UME
Diagnosis is usually confirmed using imaging systems, mainly the OCT and fundus fluorescein angiography (FFA).
Usually, a non-infectious UME presents with visual disturbances that are highly variable such as drop in near VA, metamorphopsia, micropsia, blurred vision and positive relative scotomas. In chronic cases where the outer retina has undergone degenerative structural changes, the visual effects can be significant.
The gold standard technique for confirming the diagnosis of UME is the OCT.Citation87,Citation88
Optical coherence tomography (OCT)
OCT provides in vivo near-histological cross-sectional images of the retina. The layers of the retina can be visualized and a detailed analysis of the pathology affecting various structural layers can be done.
Fluid accumulation can be detected in any layer. Furthermore, a quantification of macular thickness can be made, the outer/inner segment line of the photoreceptors can be visualized and examined, intraretinal or subretinal fluid can be seen as well as the presence of ERM or vitreomacular traction. OCT advantages are that it is a non-invasive, reproducible and sensitive imaging system.Citation89,Citation90
Fundus fluorescein angiography (FFA)
FFA despite being more invasive than OCT is a useful tool concerning the inflammatory ME. Dye diffusion can be usually detected in the macular area, which might be associated with pooling in the cystoid spaces. It can help in finding and staging the severity of intraocular inflammation, detecting active choroiditis/retinitis lesions and quantification of retinal vascular (venous, arterial or mixed) leakage. FFA can help to examine the status of macular vasculature which has a direct relationship with the visual morbidity and is the only imaging system that can reveal macular ischemia.Citation87,Citation91
The management of conditions such as posterior uveitis has been revolutionized with the newest ultra-wide field FFA.Citation92,Citation93 Furthermore, with the use of FFA the therapeutic response to a therapeutic intervention can be assessed.
Representative cases with UME on OCT and FFA are depicted in and .
Diagnostic management of UME
When uveitis-related ME is present, physicians need to rule out any infectious or autoimmune underlying disease.
Initial survey should focus on personal medical and surgical history, previous ocular redness, trauma or ocular surgery.
General signs should be researched (fever, sweating and weight loss) and then various organs including skin (herpetic eruption, aphtha, psoriasis or any previous cutaneous eruption or depigmentation), lung (asthma, breathlessness), digestive (abdominal pain, diarrhea, blood stools and hepatitis), joint pain, urinary tract (blood, ulceration) and nervous system (headache, dizziness, sensitive trouble, hypoacusia) should be assessed.
Lifestyle should also be considered, ie alcohol, smoking, toxicomania, and risk of any sexually transmitted disease, presence of pets at home (cat scratch/Lyme disease), risk factors such as raw meat or badly washed salad (toxoplasmosis).
A particular attention should be given to recent traveling and possible administration of immunotherapy, which cause a tremendous increase of ME incidence (ie, Fingolimod, Paclitaxel, Taxane).Citation94
Slit lamp examination should focus on the presence of conjunctival injection, cells in the anterior chamber, the lens status and the presence of cells or floaters in the anterior vitreous. Fundus examination might reveal snowbanking in intermediate uveitis, white cells in the vitreous or inflammatory deposit along the vascular arcade.
During the examination of the fundus, the acuteness or the chronicity of the disease might also be noticed. The presence of exudate will argue for a longstanding edema. The association with an optic nerve swelling could be a sign of worse visual prognosis and therefore should be addressed during the first consultation. Unfortunately, it does not contribute to the etiological orientation.
Bilateral complete peripheral fundus examination is mandatory as it could reveal peripheral ischemia or inflammatory lesions.
As mentioned above, OCT and especially spectral-domain OCT remains the most commonly used imaging technique to assess the patient. It is a useful tool as it allows follow-up. ME should be assessed on focusing on two points: the retinal thickness map and the presence of cyst in the retina. Normal range of central foveal thickness is 182 µm±23. Nevertheless as individual variation might happen, it is always good to have the contralateral eye scanned with OCT to allow comparison, especially in the absence of intraretinal cysts.Citation95
FFA is very useful for the differential diagnosis of ME especially in the young diabetic patient where an ME might be associated with an almost normal appearance of the peripheral fundus, whereas the angiography will reveal extended zone of ischemia and microaneurysms’ leak responsible for the ME.Citation96 Not every retinal leaking is associated with the presence of inflammatory disease and the angiography by its analysis of retinal vascularization is helpful. For example, the scarcity and irregularity of the macular vasculature of a degenerative macular telangiectasia type 2 seen on the FFA would be helpful for the differential diagnosis of other macular cystic degenerations. Finally, FFA could help to exclude a vascular etiology such as vascular occlusion by highlighting tortuous collaterals, delayed filling of vessels or tortuosity of vessels.
Furthermore, FFA might show even late vascular leakage and be very useful in case where there are no intraretinal cysts and only a mild macular thickening is visible on the OCT. On the other hand, the absence of leakage with simultaneous presence of cyst should be suggestive of a different ME cause (ie, X-linked retinoschisis, Goldmann–Favre syndrome, nicotinic retinopathy, Iatrogenic cause such as nab-Paclitaxel, sirolimus).Citation97,Citation98
It is important to mention also that fundus autofluorescence can be helpful in revealing white dot syndromes.Citation99
Once the correct diagnosis of ME is made and no obvious etiology such as Irvine–Gass exists, then blood tests are required.
Some authors suggest that clinical examination might be sufficient to make a diagnosis of an underlying disease (lupus, Adamantiades–Behçet’s disease, cytomegalovirus (CMV)-related retinitis, VKH); nevertheless, one should always keep in mind that an accurate diagnosis is of outmost importance as a mistreatment might be harmful.Citation100
The blood test should be tailored following the local incidence of infectious disease, taking into account possible previous patient’s trip and their phenotype (ie, Caucasians and HLA-B27, Mediterraneans and Adamantiades–Behçet disease, Asians and VKH).Citation49
Classically, a blood test might include the following items:
Electrolytes with renal and liver function, blood glucose, red cells count with platelets and inflammatory parameters
Tailored infectious tests: syphilis, Lyme, cat scratch disease, HIV, herpes simplex virus and herpes zoster virus, CMV, Epstein–Barr virus, toxoplasmosis, human herpes virus-6 (HHV-6), tuberculosis (QuantiferonTB), West Nile virus or other tropical diseases depending on patients trip or demography.
Tailored immunologic tests: lysozyme, angiotensin converting enzyme, plasmatic protein electrophoresis, nuclear antibody (±anti-centromere, anti-dsDNA, anti-histone), ANCA, rheumatoid factor, complement C3, human leukocyte Antigen (HLA) B27, B51, A29.
Radiological exams such as chest computed tomography for sarcoidosis, brain magnetic resonance imaging for lymphoma or positron emission tomography-computed tomography for vasculitis or sinus X-ray for GPA should be done following clinical examination results.
Unfortunately, there are no standard screening tests. It is recommended to exclude the most common infectious causes and especially syphilis as an inadequate immunosuppressive treatment in those patients might have dramatic consequences.Citation101 Also, it is highly recommended to rule out sarcoidosis as it may take various clinical appearances.Citation102
More invasively, in case of unexplained UME, even with a complete clinical and laboratory workup, an anterior chamber tap and a vitreous biopsy might be necessary.Citation103,Citation104
Classically, a high CD4/CD8 ratio will argue for sarcoidosis (sensitivity and specificity up to 100% and 96%, respectively), whereas a high CD8 count and the presence of viral DNA will argue for a viral infection.Citation105 Analysis of CD19 could be helpful to rule out a tumoral etiology.Citation106
Sometimes an intraocular lymphoma might mimic a UME thus ratio of IL-10/IL-6>1 in the aqueous humor will be highly suggestive of this cause.Citation107
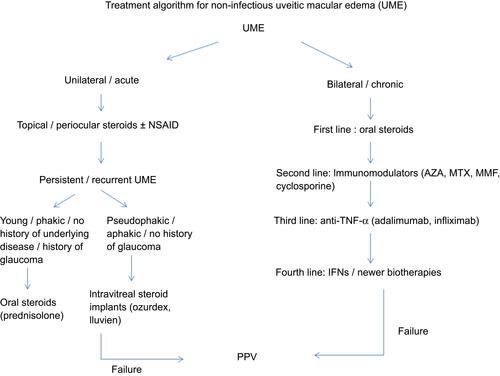
Therapeutic management
Infectious UME should be treated with the appropriate etiological treatment. Herein, we will focus on the various UME of non-infectious causes.
An accurate initial diagnosis of ME etiology is of outmost importance, as even with the right treatment, a possible resistance to it might raise doubts over whether the initial investigations were not properly done.
Irvine–Gass syndrome or pseudophakic ME or postoperative ME
The treatment nowadays is mainly based on the prevention of its occurrence. The European Society of Cataract and Refractive Surgeons has largely modified their recommendations following PREMED studies.Citation108,Citation109
Topical steroidal and non-steroidal anti-inflammatory drops have clearly led to a drop of the incidence of ME. Principle of action is mainly related to the decrease of postoperative blood-aqueous barrier breakdown.Citation110
In case of occurrence of ME, despite topical prevention, it is recommended to associate topical steroids and non-steroids anti-inflammatory drops with oral or topical carbonic anhydrase inhibitors usually for a couple of months. Vitrectomy and grid macular laser were used with some success before the introduction of anti-VEGF injections and intravitreal steroid implants.Citation111,Citation112 Periocular steroid injections remain the first-line treatment after failure of topical or oral therapy, followed by intravitreal anti-VEGF agents, like ranibizumab and bevacizumab, or intravitreal steroids as intravitreal administration of triamcinolone was found to be more efficient compared to periocular administration.Citation113,Citation114 One injection might be sufficient with low recurrence rate but for severe cases, repeated injections are often necessary.Citation115,Citation116
Third-line treatment usually consists of intraocular implants. However, physicians should be cautious with this therapeutic option as there is a risk of ocular hypertension and/or migration of the implant in the anterior chamber which can lead to endothelial cells damage.Citation117–Citation119 In a recent study from France, Ozurdex implant improved VA by at least 15 EDTRS letters, while half of the patients did not need a second injection within the first year.Citation120
In some cases, a combination of the above therapies might be considered (ie, intravitreal anti-VEGF and steroids with topical NSAIDs).Citation121
Rarely, in case of refractory ME in presence of an iris-fixated intraocular lens, even with a previous complete vitrectomy, extraction of the lens and replacement with a scleral-fixated lens might be necessary to resolve the ME.Citation122
Over the last decade, some new therapeutical perspectives are coming out such as oral mineralocorticoid-receptor antagonists or subcutaneous interferon-alpha.Citation123,Citation124
Health care professional’s decision about the most appropriate treatment should be made taking into account patient’s health, comfort and safety profile.
ME related to corneal grafts
MΕ following penetrating keratoplasty is a common complication but recently with the development of new endothelial grafting techniques (Descemet’s stripping endothelial automated keratoplasty and Descemet’s membrane endothelial keratoplasty), which are supposed to be less invasive, their incidence has increased.Citation125,Citation126 Keratoplasty-related ME, usually, resolves spontaneously or with topical anti-inflammatory treatment alone, within a few weeks, without affecting the final visual outcome of patients.Citation125–Citation127
ME related to immunological diseases
This kind of ME can be caused by entities, such as Adamantiades–Behçet’s disease, Sarcoidosis, HLA-B27 spondyloarthritis, VKH, JIA and inflammatory bowel disease.
Initial treatment remains oral and topical steroid and non-steroid anti-inflammatory drugs. In case of unilateral ME, periocular use of steroids is indicated, whereas in bilateral form, systemic steroids are usually preferred.
Immunomodulatory treatment such as methotrexate (a folic acid analog which inhibits leukocyte division),Citation128 tacrolimus and sirolimus (macrolides which inhibit T lymphocyte),Citation129 azathioprine (a purine analog which reduces the peripheral T and B lymphocytes and downregulates interleukin-2 synthesis and IgM production),Citation130 mycophenolate mofetil (an inhibitor of the purine synthesis pathway),Citation131 cyclosporine (which is produced from the fungus Tolipocladium inflatum and inhibits T-cells),Citation132 and Type I interferons (cytokines which play an important role in the regulation of innate and adaptive immune response and in the stabilization of the BRB)Citation133,Citation134 were introduced with the hope that they would be more efficient and reduce the side effects of steroids.Citation135–Citation138 Those corticosteroid-sparing agents are of outmost importance for chronic diseases, nevertheless immunomodulatory treatment has also side effects such as nephrotoxicity, neurotoxicity, gastrointestinal disturbances, flu-like syndrome, leucopenia, thrombocytopenia, hypercholesterolemia, hyperglycemia, potentially increased risk of non-hodgkin lymphoma, and requires frequent clinical observation and lab tests (renal and liver function tests, glucose and lipids profile, full blood count).Citation138 Unfortunately, there is no clear evidence for a standardized protocol and, therefore, the choice of the molecule will depend on the physician’s experience and the patient’s state.Citation139,Citation140
In case of failure (due to ineffectiveness or side effects), the more recent anti-TNF alpha treatment can be used as first line or rescue treatment (etanercept, infliximab, adalimumab) as the pro-inflammatory cytokine TNF-alpha was found to be involved in the pathogenesis of non-infectious uveitis.Citation141–Citation149 Infliximab (a mouse-human chimeric IgG1 monoclonal antibody against TNF-alpha, administered intravenously) and adalimumab (a human IgG1 monoclonal antibody against TNF-alpha administered subcutaneously) have proven their efficiency to reduce steroids dependence even in cases refractory to standard immunosuppressive therapy for sarcoidosis, whereas etanercept seems to be less effective than Infliximab for ocular inflammations.Citation150,Citation151 Systemic administration of anti TNF-alpha agents has been linked with serious adverse events, including malignancies, infections (ie tuberculosis) and autoimmune diseases.Citation152
Intravitreal administration of methotrexate can also be considered according to a British study published in 2009, but this was reported prior to the arrival of the new immunomodulatory agents.Citation153
In cases of persisting UME to conventional pharmacological treatment, pars plana vitrectomy (with or without internal limiting membrane peeling) may be indicated.Citation154 Although the mechanism of UME regression following surgical intervention is not fully understood, there is some evidence that reduction of inflammatory mediators in the vitreous body leads to reduction of antigen presentation.Citation155
ME related to ocular diseases
Retinitis pigmentosa might be associated with uveitis and ME at any stage of the disease.Citation156,Citation157 The pathophysiology of this edema is poorly understood, it might be related to inflammatory reaction due to autoantibodies and abnormal vascular permeability.Citation158 Topical or systemic carbonic anhydrase inhibitors are used as first-line treatment and in case of resistance intravitreal triamcinolone acetonide has shown good results.Citation159,Citation160
Birdshot retinopathy usually responds to systemic steroids, but sometimes resistance even to immunosuppressive agents might threaten the visual outcome.Citation161 More recent anti-TNF alpha agents can be good alternative therapeutic options in those situations.Citation162 However, even these anti -TNF alpha agents might fail to achieve a resolution of ME. Recently, Leclercq et al reported the effectiveness of tocilizumab in refractory birdshot UME cases.Citation163
Medically induced ME
Taxane-induced ME often needs withdrawal of treatment as topical dorzolamide has little effectiveness and anti-VEGF agents do not seem to have better results.Citation164 ME in this condition is probably related to aquaporin interaction rather than inflammatory reactions.Citation165 This might explain the reason that only the first injection of subconjunctival triamcinolone is effective, whereas the second one does not seem to be beneficial.Citation166
Fingolimod, commonly used nowadays in MS, has the particularity to induce ME usually a few months after initiation in approximately 0.5% of patients.Citation167,Citation168 Withdrawal of treatment is not always necessary, as steroid or non-steroid treatment can be effective with continued Fingolimod use.Citation169,Citation170
Patients with UME should be monitored closely initially. It is important to examine them 4–6 weeks after steroid treatment initiation to check intraocular pressure and the effectiveness of the treatment. A collaborative follow-up with a rheumatologist or immunologist is recommended in case of auto-immune disease. OCT monitoring and angiography should be repeated in conjunction with a regular VA assessment and complete slit lamp examination.
A summary of the most important studies and the algorithm involving the treatment of non-infectious UME is depicted in and , respectively.
Table 3 Non-infectious UME. Summary of the most important studies
Prognosis
Uveitis-related ME is considered as a risk factor for severe vision loss.Citation171 The prognosis depends on the etiology of the uveitis and also the severity of the ocular inflammation and the activity of the potentially coexisting systemic disease,Citation172 for example a UME secondary to Adamantiades–Behçet disease will have a poorer prognosis compared to a sarcoidosis related UME. The location of the inflammation and the type of the lesion are also important prognostic factors; for example, coexisting vitreoretinal interface alterations and posterior location of the uveitis are bad prognostic factors.Citation173
The prognosis of pediatric UME has drastically improved over the last decades despite its chronicity and legal blindness decreased by more than 50% with a strict control of the inflammation.Citation174,Citation175 These data highlight the significance and the need for aggressive treatment such as long-lasting intravitreal steroids.Citation176
Impact of UME on VA and quality of life
Regardless of its cause, ME leads to reduced VA which can affect patients’ quality of life.Citation177 Lardenoye et al in a cross-sectional study reported that 43% of patients with UME presented significant visual loss (≤20/60). Factors associated with poor vision were advanced age of the patients, chronic inflammation, and specific uveitis entities with intraocular lymphoma and BCR having the worse visual prognosis among the non-infectious causes, while HLA-B27-related uveitis, sarcoidosis and Adamantiades–Behçet disease seem to have lower proportions of impaired vision secondary to ME.Citation61 The same group had previously demonstrated that 35% of patients with uveitis experienced significant visual reduction.Citation38 In a large retrospective study conducted by Durrani et al, VA <6/18 was found in 47% of patients with UME (27% due to UME alone and 20% UME combined with cataract).Citation178 Taylor et al, in a retrospective study, observed that UME was associated with reduced overall visual field sensitivity, while eyes with cystoid UME had VA almost four lines worse compared to eyes without cystoid UME.Citation179 The proportion of eyes with vision <20/40 was 70% when cystoid UME was present vs 30% in eyes without cystoid UME. In a more recent retrospective study in a pediatric population with JIA, it was found that the impact on vision was more significant when both macular thickening and cysts were present, and that the central macular thickness was correlated with VA, but not with disease activity.Citation60
Systemic treatment for UME is associated with systemic adverse events, such as diabetes, osteoporosis and hypertension affecting the quality of life of these patients. Systemic immunomodulatory treatment is also associated with significant adverse events, such as skin reaction, renal and liver dysfunction.Citation137 On the other hand, local ocular administration of steroids has a high risk of inducing ocular complications. Up to 40% of patients might need surgery to control IOP whereas this rate remains at <10% in case of systemic steroids.Citation180
Conclusion
ME is a common, sight-threatening complication of non-infectious uveitis and can persist or recur despite improvement or resolution of the ocular inflammation. The diagnostic and therapeutic management of non-infectious UME remains one of the biggest challenges in ophthalmology. New pharmaceutical agents such as ACTHAR gel (a repository adrenocorticotropic hormone injection for the treatment of sarcoidosis),Citation181 the selective janus kinase 1 inhibitor filgotinib (for the treatment of rheumatoid arthritis and possibly for active non-infectious uveitis)Citation182,Citation183 and ustekinumab (a monoclonal antibody targeting the p40 subunit of interleukin-12 and interleukin-23 which can be a safe therapeutic option for psoriatic arthritis and Crohn’s disease)Citation184,Citation185 are expected with great interest. Moreover, the role of vitrectomy with or without peeling of the internal limiting membrane should be studied deeper, as the mechanism of UME improvement after vitrectomy is still unclear.Citation183
Disclosure
The authors report no conflicts of interest in this work.
References
- Evans M. Uveitis. In: Yanoff M, Duker J, editors. Ophthalmology. 4th ed. Philadelphia: Elsevier; 2014:687.
- Tran VT, Auer C, Guex-Crosier Y, Pittet N, Herbort CP. Epidemiology of uveitis in Switzerland. Ocul Immunol Inflamm. 1994;2(3):169–176. doi:10.3109/09273949409057073
- Paivonsalo-Hietanen T, Tuominen J, Vaahtoranta-Lehtonen H, Saari KM. Incidence and prevalence of different uveitis entities in Finland. Acta Ophthalmol Scand. 1997;75(1):76–81.
- Bloch-Michel E, Nussenblatt RB. International Uveitis Study Group recommendations for the evaluation of intraocular inflammatory disease. Am J Ophthalmol. 1987;103(2):234–235. doi:10.1016/s0002-9394(14)74235-7
- Jabs DA, Nussenblatt RB, Rosenbaum JT, Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509–516. doi:10.1016/j.ajo.2005.03.057
- Deschenes J, Murray PI, Rao NA, Nussenblatt RB; International Uveitis Study Group. International Uveitis Study Group (IUSG): clinical classification of uveitis. Ocul Immunol Inflamm. 2008;16(1):1–2. doi:10.1080/09273940801899822
- Yhuel Y, Weber M. Physiopathologie de l’oedème maculaire inflammatoire. In: Cohen S, Gaudric A, editors. Rétine. Les Ulis: Médecine Sciences Publications; 2012:184–189.
- Munk MR, Ram R, Rademaker A, et al. Influence of the vitreomacular interface on the efficacy of intravitreal therapy for uveitis-associated cystoid macular oedema. Acta Ophthalmol. 2015;93(7):e561–567. doi:10.1111/aos.12699
- Tran TH, de Smet MD, Bodaghi B, Fardeau C, Cassoux N, Lehoang P. Uveitic macular oedema: correlation between optical coherence tomography patterns with visual acuity and fluorescein angiography. Br J Ophthalmol. 2008;92(7):922–927. doi:10.1136/bjo.2007.136846
- Valentincic NV, de Groot-Mijnes JD, Kraut A, Korosec P, Hawlina M, Rothova A. Intraocular and serum cytokine profiles in patients with intermediate uveitis. Mol Vis. 2011;17:2003–2010.
- Schafer DP, Lehrman EK, Kautzman AG, et al. Microglia sculpt postnatal neural circuits in an activity and complement-dependent manner. Neuron. 2012;74(4):691–705. doi:10.1016/j.neuron.2012.03.026
- Stamer WD, Bok D, Hu J, Jaffe GJ, McKay BS. Aquaporin-1 channels in human retinal pigment epithelium: role in transepithelial water movement. Invest Ophthalmol Vis Sci. 2003;44(6):2803–2808. doi:10.1167/iovs.03-0001
- de Smet MD. Insights into the physiopathology of inflammatory macular edema. Dev Ophthalmol. 2017;58:168–177. doi:10.1159/000455279
- Omri S, Behar-Cohen F, de Kozak Y, et al. Microglia/macrophages migrate through retinal epithelium barrier by a transcellular route in diabetic retinopathy: role of PKCzeta in the Goto Kakizaki rat model. Am J Pathol. 2011;179(2):942–953. doi:10.1016/j.ajpath.2011.04.018
- Fardeau C, Champion E, Massamba N, LeHoang P. Uveitic macular edema. Eye (Lond). 2016;30(10):1277–1292. doi:10.1038/eye.2016.115
- Bringmann A, Pannicke T, Grosche J, et al. Muller cells in the healthy and diseased retina. Prog Retin Eye Res. 2006;25(4):397–424. doi:10.1016/j.preteyeres.2006.05.003
- Pannicke T, Uckermann O, Iandiev I, Wiedemann P, Reichenbach A, Bringmann A. Ocular inflammation alters swelling and membrane characteristics of rat Muller glial cells. J Neuroimmunol. 2005;161(1–2):145–154. doi:10.1016/j.jneuroim.2005.01.003
- Miyake K, Ibaraki N. Prostaglandins and cystoid macular edema. Surv Ophthalmol. 2002;47(Suppl 1):S203–S218.
- Liu XQ, Kobayashi H, Jin ZB, Wada A, Nao IN. Differential expression of Kir4.1 and aquaporin 4 in the retina from endotoxin-induced uveitis rat. Mol Vis. 2007;13:309–317.
- Gaudric A, Privat E. Ischémie choroïdienne aigue. In: CJ P, editor. Pathologies vasculaires oculaires. Paris (France): Société Française d’Ophtalmologie; 2008:555–571.
- Pavesio CE, Meier FM. Systemic disorders associated with episcleritis and scleritis. Curr Opin Ophthalmol. 2001;12(6):471–478.
- Sharma SM, Jackson D. Uveitis and spondyloarthropathies. Best Pract Res Clin Rheumatol. 2017;31(6):846–862. doi:10.1016/j.berh.2018.08.002
- Sen ES, Ramanan AV. Juvenile idiopathic arthritis-associated uveitis. Best Pract Res Clin Rheumatol. 2017;31(4):517–534. doi:10.1016/j.berh.2018.01.002
- Salah S, Abad S, Monnet D, Brezin AP. Sarcoidosis. J Fr Ophtalmol. 2018;41(10):e451–e467. doi:10.1016/j.jfo.2018.10.002
- Stubiger N, Ruprecht K, Pleyer U. [Intraocular inflammation in multiple sclerosis]. Ophthalmologe. 2018;115(6):531–542. doi:10.1007/s00347-018-0673-5
- Chauhan K, Tripathy K. Pars planitis. In: StatPearls. Treasure Island (FL); 2018.
- Bazvand F, Zarei M, Ebrahimiadib N, et al. Ocular manifestations, conventional fundus fluorescein angiographic findings, and relationship between angiographic findings and visual acuity in Behcet’s disease. Semin Ophthalmol. 2017;32(6):764–771. doi:10.1080/08820538.2016.1178310
- Cho H, Madu A. Etiology and treatment of the inflammatory causes of cystoid macular edema. J Inflamm Res. 2009;2:37–43.
- Zur D, Loewenstein A. Postsurgical cystoid macular edema. Dev Ophthalmol. 2017;58:178–190. doi:10.1159/000455280
- Zemba M, Camburu G. Uveitis-glaucoma-hyphaema syndrome. General review. Rom J Ophthalmol. 2017;61(1):11–17.
- Moorthy RS, Moorthy MS, Cunningham ET Jr. Drug-induced uveitis. Curr Opin Ophthalmol. 2018;29(6):588–603. doi:10.1097/ICU.0000000000000530
- London NJ, Garg SJ, Moorthy RS, Cunningham ET. Drug-induced uveitis. J Ophthalmic Inflamm Infect. 2013;3(1):43. doi:10.1186/1869-5760-3-43
- Shoughy SS, Tabbara KF. Ocular findings in systemic lupus erythematosus. Saudi J Ophthalmol. 2016;30(2):117–121. doi:10.1016/j.sjopt.2016.02.001
- Shao EH, Menezo V, Taylor SR. Birdshot chorioretinopathy. Curr Opin Ophthalmol. 2014;25(6):488–494. doi:10.1097/ICU.0000000000000101
- Castiblanco CP, Adelman RA. Sympathetic ophthalmia. Graefes Arch Clin Exp Ophthalmol. 2009;247(3):289–302. doi:10.1007/s00417-008-0939-8
- Choi JY, Kafkala C, Foster CS. Primary intraocular lymphoma: A review. Semin Ophthalmol. 2006;21(3):125–133. doi:10.1080/08820530500350498
- Bonnet C, Daudin JB, Monnet D, Brezin A. [Vogt-Koyanagi-Harada disease]. J Fr Ophtalmol. 2017;40(6):512–519. doi:10.1016/j.jfo.2017.02.006
- Rothova A, Suttorp-van Schulten MS, Frits Treffers W, Kijlstra A. Causes and frequency of blindness in patients with intraocular inflammatory disease. Br J Ophthalmol. 1996;80(4):332–336. doi:10.1136/bjo.80.4.332
- Miserocchi E, Fogliato G, Modorati G, Bandello F. Review on the worldwide epidemiology of uveitis. Eur J Ophthalmol. 2013;23(5):705–717. doi:10.5301/ejo.5000278
- Gritz DC, Wong IG. Incidence and prevalence of uveitis in Northern California; the Northern California Epidemiology of Uveitis Study. Ophthalmology. 2004;111(3):491–500; discussion 500. doi:10.1016/j.ophtha.2003.06.014
- Dandona L, Dandona R, John RK, McCarty CA, Rao GN. Population based assessment of uveitis in an urban population in southern India. Br J Ophthalmol. 2000;84(7):706–709. doi:10.1136/bjo.84.7.706
- Ayanru JO. The problem of uveitis in Bendel State of Nigeria: experience in Benin City. Br J Ophthalmol. 1977;61(10):655–659. doi:10.1136/bjo.61.10.655
- Yang P, Zhang Z, Zhou H, et al. Clinical patterns and characteristics of uveitis in a tertiary center for uveitis in China. Curr Eye Res. 2005;30(11):943–948. doi:10.1080/02713680500263606
- Wakabayashi T, Morimura Y, Miyamoto Y, Okada AA. Changing patterns of intraocular inflammatory disease in Japan. Ocul Immunol Inflamm. 2003;11(4):277–286.
- Khairallah M, Yahia SB, Ladjimi A, et al. Pattern of uveitis in a referral centre in Tunisia, North Africa. Eye (Lond). 2007;21(1):33–39. doi:10.1038/sj.eye.6702111
- Thorne JE, Suhler E, Skup M, et al. Prevalence of noninfectious uveitis in the United States: a claims-based analysis. JAMA Ophthalmol. 2016;134(11):1237–1245. doi:10.1001/jamaophthalmol.2016.3229
- Bodaghi B, Cassoux N, Wechsler B, et al. Chronic severe uveitis: etiology and visual outcome in 927 patients from a single center. Medicine (Baltimore). 2001;80(4):263–270. doi:10.1097/00005792-200107000-00005
- Tsirouki T, Dastiridou A, Symeonidis C, et al. A focus on the epidemiology of uveitis. Ocul Immunol Inflamm. 2018;26(1):2–16. doi:10.1080/09273948.2016.1196713
- Smit RL, Baarsma GS, de Vries J. Classification of 750 consecutive uveitis patients in the Rotterdam Eye Hospital. Int Ophthalmol. 1993;17(2):71–76.
- Mercanti A, Parolini B, Bonora A, Lequaglie Q, Tomazzoli L. Epidemiology of endogenous uveitis in north-eastern Italy. Analysis of 655 new cases. Acta Ophthalmol Scand. 2001;79(1):64–68.
- Chang JH, Wakefield D. Uveitis: a global perspective. Ocul Immunol Inflamm. 2002;10(4):263–279.
- Biswas J, Narain S, Das D, Ganesh SK. Pattern of uveitis in a referral uveitis clinic in India. Int Ophthalmol. 1996;20(4):223–228.
- Perkins ES, Folk J. Uveitis in London and Iowa. Ophthalmologica. 1984;189(1–2):36–40. doi:10.1159/000309382
- Henderly DE, Genstler AJ, Smith RE, Rao NA. Changing patterns of uveitis. Am J Ophthalmol. 1987;103(2):131–136. doi:10.1016/s0002-9394(14)74217-5
- McCannel CA, Holland GN, Helm CJ, Cornell PJ, Winston JV, Rimmer TG; UCLA Community-Based Uveitis Study Group. Causes of uveitis in the general practice of ophthalmology. Am J Ophthalmol. 1996;121(1):35–46. doi:10.1016/s0002-9394(14)70532-x
- Thean LH, Thompson J, Rosenthal AR. A uveitis register at the Leicester Royal Infirmary. Ophthalmic Epidemiol. 1996;3(3):151–158.
- Munoz-Fernandez S, Martin-Mola E. Uveitis. Best Pract Res Clin Rheumatol. 2006;20(3):487–505. doi:10.1016/j.berh.2006.03.008
- Grajewski RS, Boelke AC, Adler W, et al. Spectral-domain optical coherence tomography findings of the macula in 500 consecutive patients with uveitis. Eye (Lond). 2016;30(11):1415–1423. doi:10.1038/eye.2016.133
- de Smet MD, Okada AA. Cystoid macular edema in uveitis. Dev Ophthalmol. 2010;47:136–147. doi:10.1159/000320077
- de Boer J, Steijaert A, van den Bor R, Stellato R, Ossewaarde-van Norel J. Development of macular edema and impact on visual acuity in uveitis associated with juvenile idiopathic arthritis. Ocul Immunol Inflamm. 2015;23(1):67–73. doi:10.3109/09273948.2013.871566
- Lardenoye CW, van Kooij B, Rothova A. Impact of macular edema on visual acuity in uveitis. Ophthalmology. 2006;113(8):1446–1449. doi:10.1016/j.ophtha.2006.03.027
- Levin MH, Pistilli M, Daniel E, et al. Incidence of visual improvement in uveitis cases with visual impairment caused by macular edema. Ophthalmology. 2014;121(2):588–595 e581. doi:10.1016/j.ophtha.2013.09.023
- Pivetti-Pezzi P, Accorinti M, La Cava M, Colabelli Gisoldi RA, Abdulaziz MA. Endogenous uveitis: an analysis of 1,417 cases. Ophthalmologica. 1996;210(4):234–238. doi:10.1159/000310715
- Bajwa A, Osmanzada D, Osmanzada S, et al. Epidemiology of uveitis in the mid-Atlantic United States. Clin Ophthalmol. 2015;9:889–901. doi:10.2147/OPTH.S80972
- Birnbaum AD, French DD, Mirsaeidi M, Wehrli S. Sarcoidosis in the national veteran population: association of ocular inflammation and mortality. Ophthalmology. 2015;122(5):934–938. doi:10.1016/j.ophtha.2015.01.003
- Merle H, Cabre P, Olindo S, Merle S, Smadja D. Ocular lesions in 200 patients infected by the human T-cell lymphotropic virus type 1 in martinique (French West Indies). Am J Ophthalmol. 2002;134(2):190–195. doi:10.1016/s0002-9394(02)01521-0
- Wakefield D, Chang JH. Epidemiology of uveitis. Int Ophthalmol Clin. 2005;45(2):1–13.
- Merrill PT, Kim J, Cox TA, Betor CC, McCallum RM, Jaffe GJ. Uveitis in the southeastern United States. Curr Eye Res. 1997;16(9):865–874.
- Aydin T, Taspinar O, Guneser M, Keskin Y. Association of Vogt Koyanagi Harada syndrome and seronegative rheumatoid arthritis. Ethiop J Health Sci. 2016;26(2):193–196. doi:10.4314/ejhs.v26i2.14
- Nashtaei EM, Soheilian M, Herbort CP, Yaseri M. Patterns of uveitis in the middle East and europe. J Ophthalmic Vis Res. 2011;6(4):233–240.
- Lee JH, Mi H, Lim R, et al. Ocular autoimmune systemic inflammatory infectious study - report 3: posterior and panuveitis. Ocul Immunol Inflamm. 2019;27(1):89–98. doi: 10.1080/09273948.2017.1358377
- Power WJ, Rodriguez A, Pedroza-Seres M, Foster CS. Outcomes in anterior uveitis associated with the HLA-B27 haplotype. Ophthalmology. 1998;105(9):1646–1651. doi:10.1016/S0161-6420(98)99033-9
- Linssen A, Meenken C. Outcomes of HLA-B27-positive and HLA-B27-negative acute anterior uveitis. Am J Ophthalmol. 1995;120(3):351–361. doi:10.1016/s0002-9394(14)72165-8
- Braakenburg AM, de Valk HW, de Boer J, Rothova A. Human leukocyte antigen-B27-associated uveitis: long-term follow-up and gender differences. Am J Ophthalmol. 2008;145(3):472–479. doi:10.1016/j.ajo.2007.11.009
- Hoeksema L, Los LI. Visual prognosis and ocular complications in herpetic versus HLA-B27- or ankylosing spondylitis-associated anterior uveitis. Ocul Immunol Inflamm. 2016;24(3):302–312. doi:10.3109/09273948.2015.1005237
- Accorinti M, Iannetti L, Liverani M, Caggiano C, Gilardi M. Clinical features and prognosis of HLA B27-associated acute anterior uveitis in an Italian patient population. Ocul Immunol Inflamm. 2010;18(2):91–96. doi:10.3109/09273941003597268
- Pathanapitoon K, Suksomboon S, Kunavisarut P, et al. HLA-B27-associated acute anterior uveitis in the University Referral Centre in North Thailand: clinical presentation and visual prognosis. Br J Ophthalmol. 2006;90(12):1448–1450. doi:10.1136/bjo.2006.099788
- Sungur G, Yakin M, Uzman S, Balta O, Orman G, Ornek F. Clinical features and prognosis of uveitis in a Turkish patient population with ankylosing spondylitis: incidence and management of ocular complications. Ocul Immunol Inflamm. 2019;27(4):551–559. doi: 10.1080/09273948.2018.1431290
- Angeles-Han ST, McCracken C, Yeh S, et al. Characteristics of a cohort of children with juvenile idiopathic arthritis and JIA-associated uveitis. Pediatr Rheumatol Online J. 2015;13:19. doi:10.1186/s12969-015-0018-8
- Heinz C, Schoonbrood S, Heiligenhaus A. Intermediate uveitis in children and young adults: differences in clinical course, associations and visual outcome. Br J Ophthalmol. 2014;98(8):1107–1111. doi:10.1136/bjophthalmol-2013-304589
- Paroli MP, Spinucci G, Monte R, Pesci FR, Abicca I, Pivetti Pezzi P. Intermediate uveitis in a pediatric Italian population. Ocul Immunol Inflamm. 2011;19(5):321–326. doi:10.3109/09273948.2011.603878
- de Boer J, Berendschot TT, van der Does P, Rothova A. Long-term follow-up of intermediate uveitis in children. Am J Ophthalmol. 2006;141(4):616–621. doi:10.1016/j.ajo.2005.09.035
- Arellanes-Garcia L, Navarro-Lopez L, Recillas-Gispert C. Pars planitis in the Mexican Mestizo population: ocular findings, treatment, and visual outcome. Ocul Immunol Inflamm. 2003;11(1):53–60.
- Accorinti M, Pesci FR, Pirraglia MP, Abicca I, Pivetti-Pezzi P. Ocular Behcet’s disease: changing patterns over time, complications and long-term visual prognosis. Ocul Immunol Inflamm. 2017;25(1):29–36. doi:10.3109/09273948.2015.1094095
- Tugal-Tutkun I, Onal S, Altan-Yaycioglu R, Huseyin Altunbas H, Urgancioglu M. Uveitis in Behcet disease: an analysis of 880 patients. Am J Ophthalmol. 2004;138(3):373–380. doi:10.1016/j.ajo.2004.03.022
- Accorinti M, Okada AA, Smith JR, Gilardi M. Epidemiology of macular edema in uveitis. Ocul Immunol Inflamm. 2019;27(2):169–180. doi: 10.1080/09273948.2019.1576910
- Gupta V, Al-Dhibi HA, Arevalo JF. Retinal imaging in uveitis. Saudi J Ophthalmol. 2014;28(2):95–103. doi:10.1016/j.sjopt.2014.02.008
- Gaucher D, Tadayoni R, Erginay A, Haouchine B, Gaudric A, Massin P. Optical coherence tomography assessment of the vitreoretinal relationship in diabetic macular edema. Am J Ophthalmol. 2005;139(5):807–813. doi:10.1016/j.ajo.2004.12.084
- Grewal DS, O’Sullivan ML, Kron M, Jaffe GJ. Association of disorganization of retinal inner layers with visual acuity in eyes with uveitic cystoid macular edema. Am J Ophthalmol. 2017;177:116–125. doi:10.1016/j.ajo.2017.02.017
- Roesel M, Henschel A, Heinz C, Dietzel M, Spital G, Heiligenhaus A. Fundus autofluorescence and spectral domain optical coherence tomography in uveitic macular edema. Graefes Arch Clin Exp Ophthalmol. 2009;247(12):1685–1689. doi:10.1007/s00417-009-1149-8
- Thomas AS, Redd T, Campbell JP, et al. The impact and implication of peripheral vascular leakage on ultra-widefield fluorescein angiography in uveitis. Ocul Immunol Inflamm. 2019;27(3):349–355. doi: 10.1080/09273948.2017.1367406
- Karampelas M, Sim DA, Chu C, et al. Quantitative analysis of peripheral vasculitis, ischemia, and vascular leakage in uveitis using ultra-widefield fluorescein angiography. Am J Ophthalmol. 2015;159(6):1161–1168 e1161. doi:10.1016/j.ajo.2015.02.009
- Campbell JP, Leder HA, Sepah YJ, et al. Wide-field retinal imaging in the management of noninfectious posterior uveitis. Am J Ophthalmol. 2012;154(5):908–911 e902. doi:10.1016/j.ajo.2012.05.019
- Willis MA, Cohen JA. Fingolimod therapy for multiple sclerosis. Semin Neurol. 2013;33(1):37–44. doi:10.1055/s-0033-1343794
- Chan A, Duker JS, Ko TH, Fujimoto JG, Schuman JS. Normal macular thickness measurements in healthy eyes using Stratus optical coherence tomography. Arch Ophthalmol. 2006;124(2):193–198. doi:10.1001/archopht.124.2.193
- Kozak I, Morrison VL, Clark TM, et al. Discrepancy between fluorescein angiography and optical coherence tomography in detection of macular disease. Retina. 2008;28(4):538–544. doi:10.1097/IAE.0b013e318167270b
- Rahman HT, Yeh S, Bergstrom CS. Cystoid macular edema without leakage secondary to nab-Paclitaxel (Abraxane): clinical experience with intravitreal bevacizumab. J Ocul Pharmacol Ther. 2013;29(3):360–362. doi:10.1089/jop.2011.0178
- Nayak SK, Jeloka TK, Sreepada SV. Sirolimus-induced pneumonitis, sinusitis and macular oedema. Nephrol Dial Transplant. 2004;19(11):2931. doi:10.1093/ndt/gfh465
- Yeh S, Forooghian F, Wong WT, et al. Fundus autofluorescence imaging of the white dot syndromes. Arch Ophthalmol. 2010;128(1):46–56. doi:10.1001/archophthalmol.2009.368
- de-la-Torre A, Valdes-Camacho J, de Mesa CL, et al. Coinfections and differential diagnosis in immunocompetent patients with uveitis of infectious origin. BMC Infect Dis. 2019;19(1):91. doi:10.1186/s12879-018-3613-8
- Shaikh SI, Biswas J, Rishi P. Nodular syphilitic scleritis masquerading as an ocular tumor. J Ophthalmic Inflamm Infect. 2015;5:8. doi:10.1186/s12348-015-0040-5
- Thorne JE, Brucker AJ. Choroidal white lesions as an early manifestation of sarcoidosis. Retina. 2000;20(1):8–15.
- Margolis R. Diagnostic vitrectomy for the diagnosis and management of posterior uveitis of unknown etiology. Curr Opin Ophthalmol. 2008;19(3):218–224. doi:10.1097/ICU.0b013e3282fc261d
- Rothova A, de Boer JH, Ten Dam-van Loon NH, et al. Usefulness of aqueous humor analysis for the diagnosis of posterior uveitis. Ophthalmology. 2008;115(2):306–311. doi:10.1016/j.ophtha.2007.05.014
- Kojima K, Maruyama K, Inaba T, et al. The CD4/CD8 ratio in vitreous fluid is of high diagnostic value in sarcoidosis. Ophthalmology. 2012;119(11):2386–2392. doi:10.1016/j.ophtha.2012.05.033
- Maruyama K, Inaba T, Sugita S, et al. Comprehensive analysis of vitreous specimens for uveitis classification: a prospective multicentre observational study. BMJ Open. 2017;7(11):e014549.
- Pochat-Cotilloux C, Bienvenu J, Nguyen AM, et al. Use of a threshold of interleukin-10 and Il-10/Il-6 ratio in ocular samples for the screening of vitreoretinal lymphoma. Retina. 2018;38(4):773–781. doi:10.1097/IAE.0000000000001922
- Wielders LHP, Schouten J, Winkens B, et al. European multicenter trial of the prevention of cystoid macular edema after cataract surgery in nondiabetics: ESCRS PREMED study report 1. J Cataract Refract Surg. 2018;44(4):429–439. doi:10.1016/j.jcrs.2018.01.029
- Wielders LHP, Schouten J, Winkens B, et al. Randomized controlled European multicenter trial on the prevention of cystoid macular edema after cataract surgery in diabetics: ESCRS PREMED Study Report 2. J Cataract Refract Surg. 2018;44(7):836–847. doi:10.1016/j.jcrs.2018.05.015
- Sanders DR, Kraff M. Steroidal and nonsteroidal anti-inflammatory agents. Effect on postsurgical inflammation and blood-aqueous humor barrier breakdown. Arch Ophthalmol. 1984;102(10):1453–1456. doi:10.1001/archopht.1984.01040031173012
- Young PW, Shea M. Pars plasma vitrectomy in the management of the Irvine-Gass syndrome. Can J Ophthalmol. 1980;15(4):172–175.
- Lardenoye CW, van Schooneveld MJ, Frits Treffers W, Rothova A. Grid laser photocoagulation for macular oedema in uveitis or the Irvine-Gass syndrome. Br J Ophthalmol. 1998;82(9):1013–1016. doi:10.1136/bjo.82.9.1013
- Loewenstein A, Zur D. Postsurgical cystoid macular edema. Dev Ophthalmol. 2010;47:148–159. doi:10.1159/000320078
- Thorne JE, Sugar EA, Holbrook JT, et al. Periocular triamcinolone vs. intravitreal triamcinolone vs. intravitreal dexamethasone implant for the treatment of uveitic macular edema: the PeriOcular vs. INTravitreal corticosteroids for uveitic macular edema (POINT) trial. Ophthalmology. 2019;126(2):283–295. doi:10.1016/j.ophtha.2018.08.021
- Mitropoulos PG, Chatziralli IP, Peponis VG, Drakos E, Parikakis EA. Intravitreal ranibizumab for the treatment of Irvine-Gass syndrome. Ocul Immunol Inflamm. 2015;23(3):225–231. doi:10.3109/09273948.2014.898775
- Arevalo JF, Maia M, Garcia-Amaris RA, et al. Intravitreal bevacizumab for refractory pseudophakic cystoid macular edema: the Pan-American Collaborative Retina Study Group results. Ophthalmology. 2009;116(8):1481–1487, 1487 e1481. doi:10.1016/j.ophtha.2009.04.006
- Malcles A, Janin-Manificat H, Yhuel Y, et al. [Anterior chamber migration of intravitreal dexamethasone implant (Ozurdex(R)) in pseudophakic eyes: report of three cases]. J Fr Ophtalmol. 2013;36(4):362–367. doi:10.1016/j.jfo.2012.11.003
- Bahadorani S, Krambeer C, Wannamaker K, et al. The effects of repeated Ozurdex injections on ocular hypertension. Clin Ophthalmol. 2018;12:639–642. doi:10.2147/OPTH.S148990
- Massa H, Georgoudis P, Panos GD. Dexamethasone intravitreal implant (OZURDEX((R))) for macular edema secondary to noninfectious uveitis: a review of the literature. Ther Deliv. 2019;10(6):343–351. doi:10.4155/tde-2019-0024
- Bellocq D, Korobelnik JF, Burillon C, et al. Effectiveness and safety of dexamethasone implants for post-surgical macular oedema including Irvine-Gass syndrome: the EPISODIC study. Br J Ophthalmol. 2015;99(7):979–983. doi:10.1136/bjophthalmol-2014-306159
- Warren KA, Bahrani H, Fox JE. NSAIDs in combination therapy for the treatment of chronic pseudophakic cystoid macular edema. Retina. 2010;30(2):260–266.
- Massa HF, Gobej I, Jacquier P, Jonescu-Cuypers C, Le Quoy O. Cystoid macular oedema and iris-fixated intraocular lens treated with intraocular lens exchange: a case series and review. J Int Med Res. 2019;47(1):188–195. doi:10.1177/0300060518799004
- Matet A, Daruich A, Behar-Cohen F. Irvine-Gass macular edema responding to the combination of oral mineralocorticoid-receptor antagonist with dexamethasone drops. Ophthalmic Surg Lasers Imaging Retina. 2017;48(11):936–942. doi:10.3928/23258160-20171030-11
- Deuter CM, Gelisken F, Stubiger N, Zierhut M, Doycheva D. Successful treatment of chronic pseudophakic macular edema (Irvine-Gass syndrome) with interferon alpha: a report of three cases. Ocul Immunol Inflamm. 2011;19(3):216–218. doi:10.3109/09273948.2011.562341
- Nirankari VS, Karesh JW. Cystoid macular edema following penetrating keratoplasty: incidence and prognosis. Ophthalmic Surg. 1986;17(7):404–407.
- Kocaba V, Mouchel R, Fleury J, et al. Incidence of cystoid macular edema after descemet membrane endothelial keratoplasty. Cornea. 2018;37(3):277–282. doi:10.1097/ICO.0000000000001501
- Kitazawa K, Kayukawa K, Wakimasu K, et al. Topical non-steroidal anti-inflammatory drugs for the treatment of cystoid macular edema post Descemet’s stripping automated endothelial keratoplasty. Jpn J Ophthalmol. 2018;62(6):615–620. doi:10.1007/s10384-018-0621-6
- Jabs DA, Rosenbaum JT, Foster CS, et al. Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: recommendations of an expert panel. Am J Ophthalmol. 2000;130(4):492–513. doi:10.1016/s0002-9394(00)00659-0
- Hogan AC, McAvoy CE, Dick AD, Lee RW. Long-term efficacy and tolerance of tacrolimus for the treatment of uveitis. Ophthalmology. 2007;114(5):1000–1006. doi:10.1016/j.ophtha.2007.01.026
- Bacon PA, Salmon M. Modes of action of second-line agents. Scand J Rheumatol Suppl. 1987;64:17–24.
- Thorne JE, Jabs DA, Qazi FA, Nguyen QD, Kempen JH, Dunn JP. Mycophenolate mofetil therapy for inflammatory eye disease. Ophthalmology. 2005;112(8):1472–1477. doi:10.1016/j.ophtha.2005.02.020
- Nussenblatt RB, Palestine AG, Chan CC. Cyclosporin A therapy in the treatment of intraocular inflammatory disease resistant to systemic corticosteroids and cytotoxic agents. Am J Ophthalmol. 1983;96(3):275–282. doi:10.1016/s0002-9394(14)77814-6
- Gillies MC, Su T. Interferon-alpha 2b enhances barrier function of bovine retinal microvascular endothelium in vitro. Microvasc Res. 1995;49(3):277–288. doi:10.1006/mvre.1995.1024
- Feron EJ, Rothova A, van Hagen PM, Baarsma GS, Suttorp-Schulten MS. Interferon-alpha 2b for refractory ocular Behcet’s disease. Lancet. 1994;343(8910):1428. doi:10.1016/S0140-6736(94)92549-6
- Neri P, Mariotti C, Cimino L, Mercanti L, Giovannini A. Long-term control of cystoid macular oedema in noninfectious uveitis with Mycophenolate Mofetil. Int Ophthalmol. 2009;29(3):127–133. doi:10.1007/s10792-008-9200-z
- Ramanan AV, Dick AD, Jones AP, et al. Adalimumab plus methotrexate for uveitis in juvenile idiopathic arthritis. N Engl J Med. 2017;376(17):1637–1646. doi:10.1056/NEJMoa1614160
- Trivedi A, Katelaris C. The use of biologic agents in the management of uveitis. Intern Med J. 2018. doi:10.1111/imj.14215
- Yanai R, Takeda A, Yoshimura T, Sonoda KH. [Pathophysiology and new treatment of uveitis]. Nihon Rinsho Meneki Gakkai Kaishi. 2014;37(2):74–82.
- Tallouzi MO, Mathers JM, Moore DJ, et al. COSUMO: study protocol for the development of a core outcome set for efficacy and effectiveness trials in posterior segment-involving uveitis. Trials. 2017;18(1):576. doi:10.1186/s13063-017-2294-8
- Tallouzi MO, Moore DJ, Calvert M, Murray PI, Bucknall N, Denniston AK. The effectiveness of pharmacological agents for the treatment of uveitic macular oedema (UMO): a systematic review protocol. Syst Rev. 2016;5:29. doi:10.1186/s13643-016-0289-2
- Sharma SM, Nestel AR, Lee RW, Dick AD. Clinical review: anti-TNFalpha therapies in uveitis: perspective on 5 years of clinical experience. Ocul Immunol Inflamm. 2009;17(6):403–414. doi:10.3109/09273940903072443
- Markomichelakis NN, Theodossiadis PG, Pantelia E, Papaefthimiou S, Theodossiadis GP, Sfikakis PP. Infliximab for chronic cystoid macular edema associated with uveitis. Am J Ophthalmol. 2004;138(4):648–650. doi:10.1016/j.ajo.2004.04.066
- Schaap-Fogler M, Amer R, Friling R, Priel E, Kramer M. Anti-TNF-alpha agents for refractory cystoid macular edema associated with noninfectious uveitis. Graefes Arch Clin Exp Ophthalmol. 2014;252(4):633–640. doi:10.1007/s00417-013-2552-8
- Arida A, Fragiadaki K, Giavri E, Sfikakis PP. Anti-TNF agents for Behcet’s disease: analysis of published data on 369 patients. Semin Arthritis Rheum. 2011;41(1):61–70. doi:10.1016/j.semarthrit.2010.09.002
- Vallet H, Seve P, Biard L, et al. Infliximab versus adalimumab in the treatment of refractory inflammatory uveitis: a multicenter study from the french uveitis network. Arthritis Rheumatol. 2016;68(6):1522–1530. doi:10.1002/art.39667
- Diaz-Llopis M, Salom D, Garcia-de-Vicuna C, et al. Treatment of refractory uveitis with adalimumab: a prospective multicenter study of 131 patients. Ophthalmology. 2012;119(8):1575–1581. doi:10.1016/j.ophtha.2012.02.018
- Calvo-Rio V, Blanco R, Beltran E, et al. Anti-TNF-alpha therapy in patients with refractory uveitis due to Behcet’s disease: a 1-year follow-up study of 124 patients. Rheumatology (Oxford). 2014;53(12):2223–2231. doi:10.1093/rheumatology/keu266
- Mesquida M, Molins B, Llorenc V, et al. Twenty-four month follow-up of tocilizumab therapy for refractory uveitis-related macular edema. Retina. 2018;38(7):1361–1370. doi:10.1097/IAE.0000000000001690
- Calvo-Rio V, Blanco R, Santos-Gomez M, et al. Golimumab in refractory uveitis related to spondyloarthritis. Multicenter study of 15 patients. Semin Arthritis Rheum. 2016;46(1):95–101. doi:10.1016/j.semarthrit.2016.03.002
- Riancho-Zarrabeitia L, Calvo-Rio V, Blanco R, et al. Anti-TNF-alpha therapy in refractory uveitis associated with sarcoidosis: multicenter study of 17 patients. Semin Arthritis Rheum. 2015;45(3):361–368. doi:10.1016/j.semarthrit.2015.05.010
- Galor A, Perez VL, Hammel JP, Lowder CY. Differential effectiveness of etanercept and infliximab in the treatment of ocular inflammation. Ophthalmology. 2006;113(12):2317–2323. doi:10.1016/j.ophtha.2006.04.038
- Imrie FR, Dick AD. Biologics in the treatment of uveitis. Curr Opin Ophthalmol. 2007;18(6):481–486. doi:10.1097/ICU.0b013e3282f03d42
- Taylor SR, Habot-Wilner Z, Pacheco P, Lightman SL. Intraocular methotrexate in the treatment of uveitis and uveitic cystoid macular edema. Ophthalmology. 2009;116(4):797–801. doi:10.1016/j.ophtha.2008.10.033
- Golan S, Loewenstein A. Surgical treatment for macular edema. Semin Ophthalmol. 2014;29(4):242–256. doi:10.3109/08820538.2013.796394
- Muhaya M, Calder VL, Towler HM, Jolly G, McLauchlan M, Lightman S. Characterization of phenotype and cytokine profiles of T cell lines derived from vitreous humour in ocular inflammation in man. Clin Exp Immunol. 1999;116(3):410–414. doi:10.1046/j.1365-2249.1999.00921.x
- Liew G, Strong S, Bradley P, et al. Prevalence of cystoid macular oedema, epiretinal membrane and cataract in retinitis pigmentosa. Br J Ophthalmol. 2018. doi:10.1136/bjophthalmol-2018-311964
- Dutta Majumder P, Menia N, Roy R, et al. Uveitis in patients with retinitis pigmentosa: 30 years’ consecutive data. Ocul Immunol Inflamm. 2018;26(8):1283–1288. doi:10.1080/09273948.2017.1348527
- Moldow B, Sander B, Larsen M, et al. The effect of acetazolamide on passive and active transport of fluorescein across the blood-retina barrier in retinitis pigmentosa complicated by macular oedema. Graefes Arch Clin Exp Ophthalmol. 1998;236(12):881–889.
- Grover S, Fishman GA, Fiscella RG, Adelman AE. Efficacy of dorzolamide hydrochloride in the management of chronic cystoid macular edema in patients with retinitis pigmentosa. Retina. 1997;17(3):222–231.
- Saraiva VS, Sallum JM, Farah ME. Treatment of cystoid macular edema related to retinitis pigmentosa with intravitreal triamcinolone acetonide. Ophthalmic Surg Lasers Imaging. 2003;34(5):398–400.
- Menezo V, Taylor SR. Birdshot uveitis: current and emerging treatment options. Clin Ophthalmol. 2014;8:73–81. doi:10.2147/OPTH.S54832
- Jaffe GJ, Dick AD, Brezin AP, et al. Adalimumab in patients with active noninfectious uveitis. N Engl J Med. 2016;375(10):932–943. doi:10.1056/NEJMoa1509852
- Leclercq M, Le Besnerais M, Langlois V, et al. Tocilizumab for the treatment of birdshot uveitis that failed interferon alpha and anti-tumor necrosis factor-alpha therapy: two cases report and literature review. Clin Rheumatol. 2018;37(3):849–853. doi:10.1007/s10067-018-4007-4
- Hassall MM, Andrew NH. Single-eye trial of a topical carbonic anhydrase inhibitor versus intravitreal bevacizumab for the treatment of taxane drug-induced cystoid macula oedema. BMJ Case Rep. 2016;2016. doi:10.1136/bcr-2015-212733
- Kanakis M, Georgalas I, Makatsoris T, Pharmakakis N. Taxane induced cystoid macular edema: case report and integrated pathogenic theory. Curr Drug Saf. 2019;14(1):43–47. doi:10.2174/1574886313666180828163016
- Matsuoka N, Hasebe H, Mayama T, Fukuchi T. Sub-tenon injections of triamcinolone acetonide had limited effect on cystoid macular edema secondary to nanoparticle albumin-bound-paclitaxel (Abraxane). Case Rep Ophthalmol Med. 2015;2015:181269. doi:10.1155/2015/181269
- Turaka K, Bryan JS. Does fingolimod in multiple sclerosis patients cause macular edema? J Neurol. 2012;259(2):386–388. doi:10.1007/s00415-011-6367-4
- Jain N, Bhatti MT. Fingolimod-associated macular edema: incidence, detection, and management. Neurology. 2012;78(9):672–680. doi:10.1212/WNL.0b013e318248deea
- Chui J, Herkes GK, Chang A. Management of fingolimod-associated macular edema. JAMA Ophthalmol. 2013;131(5):694–696. doi:10.1001/jamaophthalmol.2013.47
- Minuk A, Belliveau MJ, Almeida DR, Dorrepaal SJ, Gale JS. Fingolimod-associated macular edema: resolution by sub-tenon injection of triamcinolone with continued fingolimod use. JAMA Ophthalmol. 2013;131(6):802–804. doi:10.1001/jamaophthalmol.2013.2465
- Albaroudi N, Tijani M, Boutimzine N, Cherkaoui O, Laghmari M. [Prognostic factors in uveitis]. J Fr Ophtalmol. 2017;40(9):751–757. doi:10.1016/j.jfo.2017.04.005
- Takeuchi M, Kanda T, Kaburaki T, et al. Real-world evidence of treatment for relapse of noninfectious uveitis in tertiary centers in Japan: a multicenter study. Medicine (Baltimore). 2019;98(9):e14668. doi:10.1097/MD.0000000000014668
- Matas J, Llorenc V, Fonollosa A, et al. Predictors for functional and anatomic outcomes in macular edema secondary to non-infectious uveitis. PLoS One. 2019;14(1):e0210799. doi:10.1371/journal.pone.0210799
- Eiger-Moscovich M, Tomkins-Netzer O, Amer R, et al. Visual and clinical outcome of macular edema complicating pediatric noninfectious uveitis. Am J Ophthalmol. 2019;202:72–78. doi:10.1016/j.ajo.2019.02.011
- Garweg JG. Macular edema in childhood uveitis. Klin Monbl Augenheilkd. 2018;235(4):373–376. doi:10.1055/s-0043-123650
- Leinonen S, Immonen I, Kotaniemi K. Fluocinolone acetonide intravitreal implant (Retisert((R))) in the treatment of sight threatening macular oedema of juvenile idiopathic arthritis-related uveitis. Acta Ophthalmol. 2018;96(6):648–651. doi:10.1111/aos.13744
- Kaleemunnisha S, Sudharshan S, Biswas J. Quality of life in non-infectious uveitis patients on immunosuppressive therapy. Middle East Afr J Ophthalmol. 2014;21(3):225–231. doi:10.4103/0974-9233.134675
- Durrani OM, Tehrani NN, Marr JE, Moradi P, Stavrou P, Murray PI. Degree, duration, and causes of visual loss in uveitis. Br J Ophthalmol. 2004;88(9):1159–1162. doi:10.1136/bjo.2003.037226
- Taylor SR, Lightman SL, Sugar EA, et al. The impact of macular edema on visual function in intermediate, posterior, and panuveitis. Ocul Immunol Inflamm. 2012;20(3):171–181. doi:10.3109/09273948.2012.658467
- Multicenter Uveitis Steroid Treatment Trial Follow-up Study Research G. Quality of life and risks associated with systemic anti-inflammatory therapy versus fluocinolone acetonide intraocular implant for intermediate uveitis, posterior uveitis, or panuveitis: fifty-four-month results of the multicenter uveitis steroid treatment trial and follow-up study. Ophthalmology. 2015;122(10):1976–1986. doi:10.1016/j.ophtha.2015.06.043
- Baughman RP, Barney JB, O’Hare L, Lower EE. A retrospective pilot study examining the use of Acthar gel in sarcoidosis patients. Respir Med. 2016;110:66–72. doi:10.1016/j.rmed.2015.11.007
- Taylor PC, Abdul Azeez M, Kiriakidis S. Filgotinib for the treatment of rheumatoid arthritis. Expert Opin Investig Drugs. 2017;26(10):1181–1187. doi:10.1080/13543784.2017.1372422
- Koronis S, Stavrakas P, Balidis M, Kozeis N, Tranos PG. Update in treatment of uveitic macular edema. Drug Des Devel Ther. 2019;13:667–680. doi:10.2147/DDDT.S166092
- Feagan BG, Sandborn WJ, Gasink C, et al. Ustekinumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2016;375(20):1946–1960. doi:10.1056/NEJMoa1602773
- Lopez-Ferrer A, Laiz A, Puig L. The safety of ustekinumab for the treatment of psoriatic arthritis. Expert Opin Drug Saf. 2017;16(6):733–742. doi:10.1080/14740338.2017.1323864