Abstract
Knobloch syndrome is an autosomal recessive disorder associated with early-onset ocular abnormalities and central nervous system malformations. Ocular abnormalities are usually severe, and include high myopia, vitreoretinal degeneration, retinal detachment, macular abnormalities, and cataract. The most frequent systemic changes are midline malformations of the brain, ventricular dilation, and occipital encephalocele. Cognitive delay may occur. We report a case of cataract in a child with Knobloch syndrome. Cataract surgery and follow-up are described.
Case report
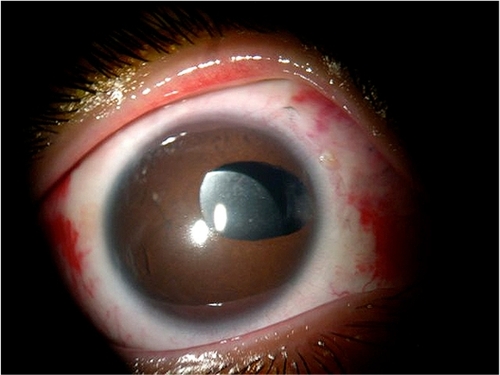
The proband, a 12-year-old Caucasian male, was referred to the Congenital Cataract Section of the Federal University of Sao Paulo, Brazil, complaining of progressive loss of vision. External observation showed bilateral leukocoria and right exotropia. The best corrected visual acuity was counting fingers at 0.5 m in each eye.
Slit-lamp examination revealed a total cataract in the right eye, and a nuclear and posterior subcapsular cataract in the left eye. Goldmann tonometry was 11 mmHg and 10 mmHg, respectively, in the right and left eyes. Right eye fundus examination was not feasible due to total cataract. Fundus examination of the left eye showed a myopic fundus with vitreous detachment and myopic macular scarring.
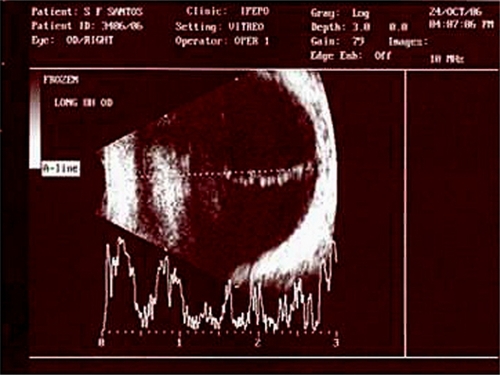
Thin lenses and a probable posterior staphyloma in both eyes were identified by ultrasonography. Vitreous opacities resembling the presence of posterior fetal vasculature were detected in the right eye (). The axial length was 27.8 mm and 27.5 mm, respectively, in the right and left eyes. The patient had no systemic changes or delay in neuropsychomotor development.
Figure 1 Retinal echography showing vitreous opacities resembling a persistence of fetal vasculature.
The proband’s brother was blind secondary to bilateral retinal detachment and aphakia. Consanguinity was detected in their parents, who were first cousins. A prior familial genetic study had been performed at another institution before the referral of the proband to our service. The familial genetic diagnosis was Knobloch syndrome type I. The parents and one proband’s sister had a normal eye examination without systemic features. The proband, as part of the present examination, also underwent a genetic study, which disclosed the same genetic diagnosis (Knobloch syndrome type I).
Phacoemulsification in the right eye was performed under general anesthesia, given the patient’s age. A limbal incision, anterior capsulorhexis, and nucleus fragmentation were performed. A peroperative posterior capsular rupture occurred. There was no vitreous prolapse and it was possible to implant an intraocular lens within the capsular bag.
On the first day of follow-up, findings were unremarkable. At one-week follow-up, slit-lamp examination showed an inflammatory reaction in the anterior vitreous and anterior chamber, despite use of topical and systemic steroids. Two months after surgery, visual acuity had improved to 20/200 in the right eye, and the patient switched to a left exotropia. A progressive posterior capsular opacity was detected in the visual axis, and a neodymium YAG laser capsulotomy was performed in the right eye. One year after surgery, dislocation of the intraocular lens was observed by slit-lamp examination. Ultrasound biomicroscopy showed a displaced intraocular lens behind the ciliary body at 7–8 clock hours. The intraocular lens haptic was dislocated to the inferior temporal quadrant (). A scleral intraocular lens fixation and anterior vitrectomy were performed to reposition the intraocular lens.
One year later, a phacoemulsification was performed in the patient’s left eye due to considerable progression of the pre-existing lens opacity to a total cataract. A limbal incision, anterior capsulorhexis, and nucleus fragmentation were done. A peroperative posterior capsular rupture occurred, as had previously happened during the patient’s right eye surgery. At this time, there was no capsular support to perform a safe intraocular lens implantation, and the left eye was left aphakic. Visual acuity with best corrected refraction improved from counting fingers to 20/200 in the left eye. The visual axis remained clear in both eyes, with final best corrected visual acuity of 20/200, leading to a better quality of life for the patient.
Discussion
This case report describes the outcomes of cataract surgery in a patient with Knobloch syndrome type I, an autosomal recessive disease affecting collagen XVIII. It was first described by Knobloch and Layer in 1971.Citation1 The pattern of inheritance is related to consanguinity. There are ocular and systemic clinical features.Citation2,Citation3 Ocular abnormalities include high myopia, vitreoretinal degeneration and opacities, retinal detachment, macular abnormalities, and cataract.Citation4
Ocular abnormalities are present in all cases reported in the literature, with great variability of clinical manifestations, due to the large number of mutations that occur in the gene. There are reports of cases of Knobloch syndrome associated with the persistence of primary vitreous.Citation1,Citation5 There is no previous report of cataract surgery in Knobloch syndrome, according to a recent PubMed search using “Knobloch syndrome” and “cataract” as keywords.
Collagen XVII is responsible for a proteoglycan component of basement membranes, including those of the iris, retina, and vitreous. It plays a role in eye development and maintenance of visual function.Citation6,Citation7
Planning cataract surgery in patients with Knobloch syndrome requires attention to the modified structure of the collagen, probably causing alterations and weakness of the zonula and lens capsule.Citation5 An intense inflammatory response may also occur after surgery, especially in children.Citation8
Knobloch syndrome should be monitored due to the risk of complications during or after phacoemulsification surgery. It is very important to consider the risk of retinal detachment in these patients. Genetic analysis in a specialized laboratory is necessary to confirm the diagnosis of Knobloch syndrome.
Disclosure
The authors declare no financial support or relationships that may pose a conflict of interest in this work.
References
- KnoblochWHLayerJMPersistence of fetal vasculature in a patient with Knobloch syndrome, potential role for endostatin in fetal vascular remodeling of the eye, retinal detachment and encephaloceleJ Pediatr Opthalmol19718181184
- Passos-BuenoMRSuzukiOTArmelin-CorreaLMMutations in collagen 18A1 and their relevance to the human phenotypeAn Acad Bras Cienc200678112313116532212
- Passos-BuenoMRMarieSKMonteiroMKnobloch syndrome in a large Brazilian consanguinous family: Confirmation of autosomal recessive inheritanceAm J Med Genet19945221701737802003
- SertieALQuimbyMMoreiraESA gene which causes severe ocular alterations and occipital encephalocele (Knobloch syndrome) is mapped to 21q22.3Hum Mol Genet1996568438478776601
- DuhEJYaoYGDagliMGoldbergMFPersistence of fetal vasculature in a patient with Knobloch syndrome: Potential role for endostatin in fetal vascular remodeling of the eyeOphthalmology2004111101885188815465551
- SertieALSossiVCamargoAAZatzMBraheCPassos-BuenoMRCollagen XVIII, containing an endogenous inhibitor of angiogenesis and tumor growth, plays a critical role in the maintenance of retinal structure and in neural tube closure (Knobloch syndrome)Hum Mol Genet20009132051205810942434
- MahajanVBOlneyAHGarrettPCharyADraganELernerGCollagen XVIII mutation in Knobloch syndrome with acute lymphoblastic leukemiaAm J Med Genet Part A2010152A112875287920799329
- TartarellaMBVerçosaITécnicas cirúrgicas da catarata na criança [Surgical techniques for cataract in children]VerçosaITartarellaMBCatarata na Criança [Cataract in Children].Fortaleza, BrazilEditora Celigráfica2008