Abstract
Aim
To evaluate the influence of optic disc size on the diagnostic accuracy of macular ganglion cell complex (GCC) and conventional peripapillary retinal nerve fiber layer (pRNFL) analyses provided by spectral domain optical coherence tomography (SD-OCT) in glaucoma.
Methods
Eighty-two glaucoma patients and 30 healthy subjects were included. All patients underwent GCC (7 × 7 mm macular grid, consisting of RNFL, ganglion cell and inner plexiform layers) and pRNFL thickness measurement (3.45 mm circular scan) by SD-OCT. One eye was randomly selected for analysis. Initially, receiver operating characteristic (ROC) curves were generated for different GCC and pRNFL parameters. The effect of disc area on the diagnostic accuracy of these parameters was evaluated using a logistic ROC regression model. Subsequently, 1.5, 2.0, and 2.5 mm2 disc sizes were arbitrarily chosen (based on data distribution) and the predicted areas under the ROC curves (AUCs) and sensitivities were compared at fixed specificities for each.
Results
Average mean deviation index for glaucomatous eyes was −5.3 ± 5.2 dB. Similar AUCs were found for the best pRNFL (average thickness = 0.872) and GCC parameters (average thickness = 0.824; P = 0.19). The coefficient representing disc area in the ROC regression model was not statistically significant for average pRNFL thickness (−0.176) or average GCC thickness (0.088; P ≥ 0.56). AUCs for fixed disc areas (1.5, 2.0, and 2.5 mm2) were 0.904, 0.891, and 0.875 for average pRNFL thickness and 0.834, 0.842, and 0.851 for average GCC thickness, respectively. The highest sensitivities – at 80% specificity for average pRNFL (84.5%) and GCC thicknesses (74.5%) – were found with disc sizes fixed at 1.5 mm2 and 2.5 mm2.
Conclusion
Diagnostic accuracy was similar between pRNFL and GCC thickness parameters. Although not statistically significant, there was a trend for a better diagnostic accuracy of pRNFL thickness measurement in cases of smaller discs. For GCC analysis, an inverse effect was observed.
Introduction
Morphological changes of the optic nerve head (ONH) and peripapillary retinal nerve fiber layer (pRNFL) often precede the development of visual field (VF) loss in glaucoma. Therefore, a precise structural evaluation is essential for early diagnosis of the disease.Citation1,Citation2 Clinical examination combined with stereophotograph evaluation is still the most commonly used method to assess structural damage in glaucoma. However, several objective imaging devices have become available over the past few years, improving diagnosis of the disease and disease follow-up.Citation3,Citation4
Since the introduction of time-domain optical coherence tomography (TD-OCT), studies have consistently shown the usefulness of pRNFL thickness measurement for glaucoma diagnosis.Citation5–Citation7 However, as a diagnostic parameter, total macular thickness measurement using TD-OCT has not been nearly as accurate as pRNFL.Citation8,Citation9 With the advent of spectral-domain optical coherence tomography (SD-OCT), a significant improvement in imaging resolution was achieved, allowing segmentation of the macular region and better identification of each layer.Citation10–Citation12 The RTVue-100 OCT (Optovue Inc, Fremont, CA) is one of the commercially available SD-OCT devices. With an axial resolution of 5 μm in tissue and a scan speed of 26,000 A-scans/second (compared with an axial resolution of 8 to 10 μm and a scan speed of 400 A-scans/second from TD-OCT), the RTVue- 100 OCT provides a segmented evaluation of the macular inner retinal layers (MIRL).Citation13 This specific analysis is called ganglion cell complex (GCC) scan, and consists of three layers: the RNFL, ganglion cell layer, and inner plexiform layer.Citation13 Recent studies have demonstrated GCC thickness as a useful parameter for glaucoma diagnosis.Citation14,Citation15
While measuring MIRL thickness, the GCC protocol uses a 7 × 7 mm macular grid centered 1 mm temporal to the fovea.Citation14–Citation16 Based on a different method, the pRNFL protocol uses a circular scan (3.45 mm in diameter) concentric to the ONH to provide regional and global thickness measurements.Citation2,Citation3 For all patients, a fixed disc diameter is adopted. A well-centered image is essential for accurate and reproducible pRNFL thickness measurements.Citation3,Citation4 However, it is generally recognized that the optic disc area shows a high interindividual variability in normal and glaucomatous eyes, ranging between 0.8 and 6.0 mm2.Citation1, Citation13 Using the same circular scan diameter for all eyes may result in pRNFL thickness measurements performed at different distances from the ONH margin.Citation3 Consequently, this would lead to over- or underestimated pRNFL measurements in eyes with small or large optic disc sizes, as it is well known that the pRNFL is thicker closer to the disc margin compared with more distant regions. It could be hypothesized that these altered pRNFL thickness measurements could affect the OCT’s ability to discriminate between glaucomatous and healthy eyes.
In the present study, the influence of optic disc area on the diagnostic accuracy of pRNFL and GCC scan protocols provided by SD-OCT for glaucoma diagnosis were evaluated and compared.
Methods
This prospective study followed the tenets of the Declaration of Helsinki and was approved by the institutional review board. Written informed consent was obtained from all participating patients.
Patients
Glaucoma patients (glaucomatous optic neuropathy [GON] and reproducible VF loss) and healthy subjects were prospectively enrolled. Initially, all participants underwent a thorough ophthalmological examination. Exclusion criteria were: previous ocular surgery or trauma; spherical equivalent > ±4.0 D; history of using oral or topical steroids; and any ocular disease other than glaucoma (for glaucomatous patients), including moderate or advanced cataract. All controls needed a normal ophthalmological examination, with intraocular pressure (IOP) <21 mmHg, normal VF testing and absence of GON on fundoscopy and stereophotographic evaluation.
Characteristic GON was defined as a vertical cup:disc ratio (CDR) ≥0.6, asymmetry of CDR ≥0.2 between eyes, presence of localized RNFL defects, and/or neuroretinal rim defects in the absence of any other abnormalities that could explain such findings. A glaucomatous VF defect in the standard automated perimetry (Humphrey SITA – Standard 24–2, Carl Zeiss Meditec, Dublin, CA) was defined as three or more points in clusters with a probability of <5% (excluding those on the edge of the field or directly above and below the blind spot) on the pattern deviation plot, a pattern standard deviation index with a probability of <5%, or a glaucoma hemifield test with results outside the normal limits.
Procedures
Baseline data assessed were age, gender, self-described race, best-corrected visual acuity, VF mean deviation (MD) index, and Goldmann applanation tonometry (IOP). Initially, ONH area for each patient was determined by confocal scanning laser ophthalmoscopy using the Heidelberg Retina Tomograph III (HRT III) (Heidelberg Engineering, Heidelberg, Germany). In all cases, ONH was delineated manually by an experienced glaucomatologist, masked to patient condition. The mean value of three consecutive scans was considered for analysis. Then all patients underwent MIRL thickness measurement (GCC scan protocol) and pRNFL thickness measurement (using the RNFL 3.45 mm scan) with the RTVue-100 OCT. Differently from TD-OCT, which accumulates the information along the longitudinal direction over the course of the scan time (using a mechanical moving part to perform the A-scan), SD-OCT acquires the information simultaneously (in an entire A-scan) by a CCD camera. Due to the nature of the mechanical moving speed, the scan time in TD-OCT is very slow, limiting its application in cases that require high repeatability and data-sampling rates. In SD-OCT, the A-scan acquisition rate is only limited by the CCD camera frame transfer rate and the computer calculation time to perform the Fourier transform of the CCD-acquired raw data into A-scan information. Because of the fast CCD camera frame transfer rate and fast Fourier transform algorithm, SD-OCT, like the RTVue, can perform 26,000 A-scans/second (65 times faster than TD-OCT).Citation13
Global (average thickness) and regional (superior and inferior thicknesses) parameters of the two scan protocols (MIRL and pRNFL) were used for analysis. Images that had a signal strength index <40 or that were not well centered (subjective assessment) were excluded from the analysis. All images were acquired by the same experienced operator, who was masked for patient clinical data.
Statistical analysis
Initially, receiver operating characteristic (ROC) curves were generated for different GCC and pRNFL parameters. Then a ROC logistic regression model was built to evaluate the effect of disc size on the diagnostic performance of each parameter. This model has been described in detail elsewhere;Citation17,Citation18 briefly, the modeling technique allows the evaluation of the effect of covariates on the whole ROC curve. Also, it is possible to calculate areas under ROC for arbitrary levels of the covariate. Subsequently, 1.5, 2.0, and 2.5 mm2 disc sizes were arbitrarily chosen (based on the distribution of the data) and the predicted areas under the ROC curves (AUCs) and sensitivities at fixed specificities for each of them were compared. Whenever both eyes were eligible, one was randomly selected for analysis. Statistical significance was set at P < 0.05.
Results
A total of 82 glaucoma patients (mean age 67.5 ± 10.4 years) and 30 healthy subjects (mean age 60.5 ± 11.3 years) were included. Average MD for glaucomatous eyes was −5.3 ± 5.2 dB. Baseline characteristics of study patients are summarized in .
Table 1 Baseline characteristics of study patients
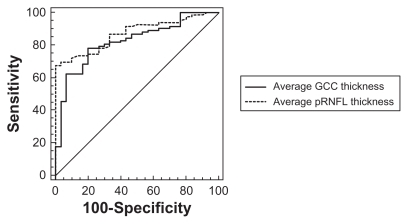
The AUCs for average, superior, and inferior GCC thickness were not significantly different at 0.824, 0.823, and 0.791, respectively (P ≥ 0.13). The AUCs for average, superior, and inferior pRNFL thickness were also similar at 0.872, 0.816, and 0.845, respectively (P ≥ 0.09). Finally, similar AUCs were found for the best pRNFL (average thickness = 0.872) and GCC parameters (average thickness = 0.824; P = 0.19) ().
Figure 1 ROC curves for SD-OCT thickness parameters. Similar AUCs were found for average pRNFL thickness (0.872) and average GCC thickness (0.824; P = 0.19).
Regarding the influence of optic disc size on the diagnostic accuracy of the SD-OCT parameters analyzed, the coefficient representing disc area in the ROC regression model was not statistically significant for average pRNFL thickness (−0.176) or average GCC thickness (0.088; P ≥ 0.56). However, a trend for a better diagnostic accuracy of pRNFL thickness and a worse performance of GCC thickness measurement was observed in smaller disc cases, based on the comparisons of AUCs and sensitivities at 80% specificity. AUCs for fixed disc areas (1.5, 2.0, and 2.5 mm2) were 0.904, 0.891, and 0.875 for average pRNFL thickness, and 0.834, 0.842, and 0.851 for average GCC thickness, respectively. The highest sensitivities at 80% specificity for average pRNFL (84.5%) and average GCC thicknesses (74.5%) were found with disc sizes fixed at 1.5 mm2 and 2.5 mm2, respectively. All sensitivity values according to each fixed disc area are provided in .
Table 2 Sensitivities at 80% specificity according to each fixed optic disc size
Discussion
The use of OCT for glaucoma detection and follow-up has been well established as a useful tool for the management of the disease. Understanding possible factors that could affect the diagnostic performance of the device is important while interpreting its results. Evaluating the influence of optic disc size on the discrimination ability of the conventional pRNFL analysis and on the relatively new GCC scan protocol provided by SD-OCT, slightly different diagnostic performances were found depending on the optic disc size. Interestingly, opposite effects were observed for the two different protocols analyzed.
In this study, it was demonstrated that the diagnostic accuracy was similar between pRNFL and GCC thickness parameters. Few studies have investigated the usefulness of the different parameters provided by the RTVue-100 SD-OCT in glaucoma patients; the findings of the present study are in agreement with all of these. In these studies, in which patients with different disease stages were evaluated, macular GCC thickness and pRNFL thickness also showed similar diagnostic performance for glaucoma detection.Citation13–Citation15
Evaluating the influence of optic disc size on the diagnostic performance of GCC and pRNFL scans, a trend for a better diagnostic performance of the pRNFL protocol in cases of smaller discs and better performance of the macular GCC protocol in cases of larger discs was observed, based on the comparisons of AUCS and sensitivities at fixed specificities (the coefficient representing disc area in the ROC regression model was not statistically significant). Although these findings might not be important for patients with optic disc sizes within the normal range, they are probably relevant for those with small or large optic discs and should be considered when evaluating these patients. There is scant information in the literature about this topic. Rao et al,Citation19 conducting a similar study, found no correlation between optic disc size and sensitivity and specificity values provided by SD-OCT. In that study, disease severity was included as a covariate, and significantly influenced the diagnostic accuracies of RTVue scanning protocols. This fact might partially explain the different outcomes observed in these two studies.
It is important to stress some specific characteristics and limitations of this study. First, the control group had a relatively small average disc size (and also a limited range), which may have influenced the results. Second, not all SD-OCT parameters available in the RTVue-100 were investigated, such as global loss volume and focal loss volume. Finally, the correlation between disease severity and SD-OCT diagnostic performance was not investigated, as the study population had a narrow range of disease severity (based on functional loss), and only a small percentage of patients with advanced damage. A study with a wider range of disease severity would be able to investigate this association more appropriately.
Conclusion
In summary, diagnostic accuracies were similar between conventional pRNFL and macular GCC protocols. Although not statistically significant, there was a trend for a better diagnostic performance of pRNFL thickness measurements in cases of smaller discs. For the GCC analysis, an inverse effect was observed. These findings should be taken into consideration while interpreting SD-OCT results for glaucoma diagnosis.
Prior publication
This paper was presented in part at the Annual Meeting of the Association for Research in Vision and Ophthalmology, Fort Lauderdale, FL, May 2010.
Disclosure
The authors report no conflicts of interest in this work.
References
- MedeirosFAZangwillLMBowdCWeinrebRNComparision of the GDxVCC scanning laser polarimeter, HRT II confocal scanning laser ophthalmoscope and stratus OCT optical coherence tomograph for detection of glaucomaArch Ophthalmol2004122682783715197057
- BrusiniPSalvetatMLZeppieriMTosoniCParisiLFelettiMlComparison between GDxVcc scanning laser polarimetry and stratus OCT optical coherence tomograph in the diagnosis of chronic glaucomaActa Ophthalmol Scand200684565065516965496
- SaviniGZaniniMCarelliVSadenAARoss–CisnerosFNBarboniPCorrelation between retinal nerve fiber layer thickness and optic nerve head size: an optical coherence tomography studyBr J Ophthalmol200589448949215774930
- MedeirosFAZangwillLMBowdCSamplePAWeinrebRNInfluence of disease severity and optic disc size on the diagnostic performance of imaging instruments in glaucomaInvest Ophthalmol Vis Sci20064731008101516505035
- LeungCKChanWMYungWHComparison of macular and peripapillary measurements for the detection of glaucoma: an optical coherence tomography studyOphthalmology2005112339140015745764
- KanamoriANakamuraMEscanoMFSeyaRMaedaHNegiAEvaluation of the glaucomatous damage on retinal nerve fiber layer thickness measured by optical coherence tomographyAm J Ophthalmol2003135451352012654369
- HuangDSwansonEALinCPOptical coherence tomographyScience19912545035117811811957169
- WollsteinGSchumanJSPriceLLOptical coherence tomography (OCT) macular and peripapillary retinal nerve fiber layer measurements and automated visual fieldsAm J Ophthalmol2004138221822515289130
- LedererDESchumanJSHertzmarkEAnalysis of macular volume in normal and glaucomatous eyes using optical coherence tomographyAm J Ophthalmol2003135683884312788124
- WojtkowskiMKowalczykALeitgebRFercherAFFull range complex spectral optical coherence tomography technique in eye imagingOpt Lett200227161415141718026464
- de BoerJFCenseBParkBHPierceMCTearneyGJBoumaBEImproved signal-to-noise ratio in spectral-domain compared with time-domain optical coherence tomographyOpt Lett200328212067206914587817
- ChenTCCenseBPierceMCSpectral domain optical coherence tomography: ultra-high speed, ultra-high resolution ophthalmic imagingArch Ophthalmol2005123121715172016344444
- SeongMSungKRChoiEHMacular and peripapillary retinal nerve fiber layer measurements by spectral domain optical coherence tomography in normal-tension glaucomaInvest Ophthalmol Vis Sci20105131446155219834029
- GarasAVarghaPHollóGDiagnostic accuracy of nerve fiber layer, macular thickness and optic disc measurements made with the RTVue- 100 optical coherence tomograph to detect glaucomaEye (Lond)2011251576520930859
- KimNRLeeESSeongGJKimJHAnHGKimCYStructure-function relationship and diagnostic value of macular ganglion cell complex measurement using Fourier-domain OCT in glaucomaInvest Ophthalmol Vis Sci20105194646465120435603
- TanOChopraVLuATDetection of macular ganglion cell loss in glaucoma by Fourier-domain optical coherence tomographyOphthalmology2009116122305231419744726
- PepeMSThree approaches to regression analysis of receiver operating characteristic curves for continuous test resultsBiometrics19985411241359544511
- MedeirosFASamplePAZangwillLMLiebmannJMGirkinCAWeinrebRNA statistical approach to the evaluation of covariate effects on the receiver operating characteristic curves of diagnostic tests in glaucomaInvest Ophthalmol Vis Sci20064762520252716723465
- RaoHLLeiteMTWeinrebRNEffect of disease severity and optic disc size on diagnostic accuracy of RTVue spectral domain optical coherence tomograph in glaucomaInvest Ophthalmol Vis Sci20115231290129620811060